Abstract
Background
Hypertension (HTN), characterized by an elevation of blood pressure, is a serious public health chronic condition that significantly raises the risks of heart, brain, kidney, and other diseases. In South Africa, the prevalence of HTN (measured objectively) was reported at 46.0% in females, nonetheless little is known regarding the prevalence and risks factors of self-reported HTN among the same population. Therefore, the aim of this study was to examine determinants of self-reported HTN among women in South Africa.
Methods
The study used data obtained from the 2016 South African Demographic and Health Survey. In total, 6,027 women aged ≥ 20 years were analyzed in this study. Self-reported HTN was defined as a case in which an individual has not been clinically diagnosed with this chronic condition by a medical doctor, nurse, or health worker. Multiple logistic regression models were employed to examine the independent factors of self-reported HTN while considering the complex survey design.
Results
Overall, self-reported HTN was reported in 23.6% (95% confidence interval [CI], 23.1–24.1) of South African women. Being younger (adjusted odds ratio [aOR], 0.04; 95% CI, 0.03–0.06), never married (aOR, 0.69; 95% CI, 0.56–0.85), and not covered by health insurance (aOR, 0.74; 95% CI, 0.58–0.95) reduced the odds of self-reported HTN. On the other hand, being black/African (aOR, 1.73; 95% CI, 1.17–2.54), perception of being overweight (aOR, 1.72; 95% CI, 1.40–2.11), and perception of having poor health status (aOR, 3.53; 95% CI, 2.53–5.21) and the presence of other comorbidities (aOR, 7.92; 95% CI, 3.63–17.29) increased the odds of self-reported HTN.
Conclusions
Self-reported HTN was largely associated with multiple sociodemographic, health, and lifestyle factors and the presence of other chronic conditions. Health promotion and services aiming at reducing the burden of HTN in South Africa should consider the associated factors reported in this study to ensure healthy aging and quality of life among women.
Similar content being viewed by others
Background
Hypertension (HTN) characterized by persistently high blood pressure is a serious public health chronic condition that significantly increases the risks of cardiovascular diseases (CVDs), renal failure, blindness, and other diseases [1, 2]. Globally, it is estimated that about 1.3 billion adults aged 30 years and above were diagnosed with HTN where two-thirds of those cases are reported in low-income and middle-income countries [3]. Furthermore, even though it is simple to diagnose HTN and reasonably easy to manage with low-cost drugs, approximately 580 million people with HTN (46%) are unaware of their condition because they were never diagnosed [4]. Globally, HTN is a leading cause of premature death and as part of global targets for noncommunicable diseases, the prevalence of HTN is set to be reduced by 33% between 2010 and 2030 [1, 5].
While the causes of HTN remain a mystery, it is certain that numerous factors may contribute to the pathogenesis of this chronic condition; nonetheless, it is thought that HTN is a result of an interaction of several genetic and environmental factors [6,7,8]. The World Health Organization (WHO) stated that modifiable risk factors such as unhealthy diets, physical inactivity, tobacco smoking, consumption of a huge amount of alcohol, and being overweight/obese were the risk factors of HTN [9, 10]. Furthermore, WHO stated that nonmodifiable risk factors including genetics, age over 65 years, and comorbidities of other chronic diseases such as diabetes or kidney disease [9, 10] were also the contributing risk factors for HTN. In reaction to the WHO report, a preponderance of previous researchers have reported that age of the respondents [11,12,13,14], educational level [13, 15, 16], ethnicity [13, 17], occupation [17], not having health insurance [16], being overweight/obese [11,12,13, 17, 18], higher waist circumference [19], physical activity [17], smoking status [13], presence of other comorbidities [12, 13, 17, 18, 20], geographical region [11, 20], were significant factors positively associated with HTN. However, most of the studies that were conducted in South Africa, had considered localized areas such as towns and municipalities as well as had focused on the objectively measured HTN (systolic blood pressure level of 140 mmHg or above or a diastolic blood pressure level of 90 mmHg or above) [11, 12, 18, 20]. Nonetheless, there is no study that had addressed the self-reported HTN as an outcome measure in South Africa.
Generally, self-reported HTN is habitually employed in research settings to evaluate the magnitude of this condition in the general population [21,22,23]. Self-reporting of the specific condition is a simple and low-cost technique that focuses on an individual’s own behaviors, beliefs, attitudes, or intentions [24]. Thus, due to its simplicity and low cost in obtaining health information from individuals, self-reporting has become an integral approach for continuous population monitoring to inform policies aimed to reduce the burden of various diseases [25, 26]. Studies have also reported the validity of self-reports against the objective measurement of the disease. For example, an Iranian study reported a prevalence of 16.8% and 15.7% for self-reported HTN, and HTN based on verified medical history and measurements, respectively [27]. It was, therefore, concluded that self-reported HTN is acceptable, and its method can be used for public health initiatives in the absence of countrywide HTN control and detection programs.
In South Africa, the prevalence of uncontrolled HTN has been estimated at 13.5% to 75.5% [18], while statistics for the controlled HTN ranged from 19.0% to 56.0% [28]. The recent data obtained from the South Africa Demographic and Health Survey (SADHS) indicated that the prevalence of HTN (objectively measured) has nearly doubled since 1998, from 25 to 46% among women [29]. The percentage of women aged 15 years and above with self-reported HTN was reported at 23% in 2016 [29]. These statistics are relatively high and call for urgent attention to reduce the burden of this condition in the general population. HTN is a precursor of stroke and ischemic heart disease, which were the second and fourth leading causes of mortality, respectively, in 2012 in South Africa [30]. Therefore, the objective of this study was to examine the determinants of self-reported HTN among women in South Africa. Such empirical evidence might be required by health policymakers to create targeted strategies for the control of HTN.
Methods
Ethical statements
This study was approved by the South Africa Medical Research Council and the Institutional Review Board of International Classification of Functioning (ICF). All methods were conducted in accordance with the Declaration of Helsinki principles. The data were de-identified to prevent the respondents’ identity from being revealed. All individuals who agreed to take part in the survey were asked to provide either written or verbal consent for the interview. Particularly, verbal consent was sought from participants who could not write or read. The Centre for Disease Control and Prevention granted a waiver of written consent per 45CFR46 for respondents who were unable to provide written consent but consented verbally.
Study design and data sources
The study used cross-sectional data from SADHS 2016. The SADHS 2016 was conducted to provide up-to-date estimates of basic demographic and measures of population health such as fertility levels, awareness and use of contraceptives, childhood and maternal mortality, immunization coverage, and prevalence and treatment of acute respiratory infection, fever, diarrhea, nutrition, etc. [29]. Additionally, the survey was also conducted to provide estimates of health and behavior measures for adults aged 15 years and older.
Sampling design
The sample for the SADHS 2016 was designed to produce estimates of vital measures of the country as a whole: urban and nonurban areas. Administratively, South Africa is divided into nine provinces namely Eastern Cape, Free State, Gauteng, KwaZulu-Natal, Limpopo, Mpumalanga, Northern Cape, North West, and Western Cape, which vary considerable in size. The Statistics South Africa Master Sample Frame was created using Census 2011 data. Enumeration areas (EAs) was used as the sampling frame for the SADHS 2016. In the Master Sample Frame, EAs of manageable size were treated as primary sampling units (PSUs), whereas small neighboring EAs were combined to form new PSUs, and large EAs were split into conceptual PSUs. Using a two-stage stratified sampling design with a probability proportional to size, PSUs were selected at the first stage while the systematic sampling of residential dwelling units (DUs) was performed at the second stage. Thus, a total of 750 PSUs were selected from the 26 sampling strata. From each PSU, a fixed number of 20 residential DUs were selected using a systematic sampling technique. Of the 15,292 households selected, 13,288 households were occupied, and interviews were successfully conducted in 83% of the occupied households.
Data collection
Data collection was conducted between June 2016 and November 2016 at the request of the National Department of Health. Data were collected using questionnaires administered by conducting face-to-face interviews. All households were eligible for interviews using the Household Questionnaire where basic demographic indicators on the characteristics of each person listed were collected, including age, sex, marital status, education, and relationship to the head of the household were collected. Further, information on characteristics of the household’s DU, such as the source of drinking water, type of sanitation facility, materials used for the floor, walls, and roof of the DU, and ownership of various durable goods were also collected. Secondly, the woman’s questionnaire was used to collect information from all eligible women aged 15 years and older on background characteristics such as age, education, media, exposure, etc. Additionally, the woman’s questionnaires also included a module on adult health where information on the use of tobacco, alcohol, consumption of fat, salt, sugar, fruit, and vegetables, health care-seeking behaviors, and self-reported prevalence of a variety of noncommunicable diseases including HTN were captured.
Measures
Outcome of interest
The present study considered self-reported HTN (high blood pressure) as the dependent variable. Specifically, respondents were asked, “Has a medical doctor, nurse, or health professional told you that you have high blood pressure?” If the response was “yes” then respondents were classified as having self-rated HTN, and if the response was “no,” then the respondents were considered having no self-reported HTN.
Independent variables
Independent variables of this study were selected after a review of the relevant literature and their availability in the SADHS 2016 dataset [11, 17, 31]. In total, 10 sociodemographic variables, seven health and lifestyle-related factors, and three other comorbidities of chronic diseases were included.
Sociodemographic variables included the age of the respondents, education level, ethnicity, household wealth, marital status, employment status, exposure to mass media, place of residence, and geographical region. Lifestyle-related factors included self-reported body mass index (BMI) and perception of own health, type of fruits eaten yesterday, type of vegetables eaten yesterday, frequency of eating processed meat, frequency of eating fried foods, and sugar-sweetened drinks in the last 24 h. Other chronic diseases included comorbidities of self-reported HTN, comorbidities of self-reported diabetes, and comorbidities of self-reported hypercholesterolemia. These variables were categorized as follows: age of the respondents in years (20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50 + years), educational level (no education/primary, secondary, tertiary education), ethnicity (black/African, white, colored and other), household wealth (poorest, poorer, middle, richer, richest), marital status (never married, currently married, divorced/widowed), current employment (not employed or employed), covered by health insurance (yes or no), the amount of mass media exposure (0, 1, 2, 3), place of residence (urban or rural), and geographical region (Western Cape, Eastern Cape, Northern Cape, Free State, KwaZulu-Natal, North West, Gauteng, Mpumalanga, Limpopo). Household wealth was calculated using household items such as such as televisions and bicycles, materials used for housing construction, and types of water access and sanitation facilities and principal component analysis was used to create scores and these were further divided into quintiles.
Health and lifestyle-related factors included perception of own weight—BMI (underweight, normal weight, overweight/obese), perception of own health, also known as self-rated health status (SRHS) was measured using a single question: “In general, how do would you rate your health?” with the following response options: excellent, good, moderate, or poor; type of fruits eaten yesterday (none, one type, two or more types); type of vegetables eaten yesterday (none, one type, two or more types); frequency of eating processed meat (never, every day, at least once a week, occasionally); frequency of eating fried foods (never, every day, at least once a week, occasionally); and sugar-sweetened drinks yesterday (no or yes). Objectively BMI is calculated by dividing the person’s weight in kilograms by their height in meters squared (kg/m2) [32]. For adults over 20 years old, BMI falls into one of the following categories: underweight (below 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obesity (30 kg/m2 and above).
Comorbidities for self-reported HTN included self-reported diabetes and self-reported hypercholesterolemia. Particularly, respondents were asked; “Has a medical doctor, nurse, or health provider told you that you have high blood pressure?” If the response was “yes” then respondents were classified as having self-reported diabetes/blood sugar or high blood cholesterol/fats in the blood (hypercholesterolemia), and if the response was “no”, then the respondents were considered having no self-reported diabetes or hypercholesterolemia.
Statistical analysis
All data analyses were conducted using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA). Characteristics of the study population were presented with numbers and percentages. Group comparisons between respondents that reported to have HTN and those that did not have HTN were made with Rao-Scott chi-square test. To assess the relationship between the selected variables and self-reported HTN, multivariate logistic analyses were constructed using a generalized estimating equation. The generalized estimating equation models accounted for the clustering effects of the hierarchical SADHS data. The results of the multivariate analysis were reported as adjusted odds ratios (aORs) with their P-values and 95% confidence intervals (CIs). A P-value of less than 0.05 was considered statistically significant.
Results
Baseline characteristics
Table 1 displays the baseline characteristics of the study sample. Of the 6,027 respondents analyzed in this study, self-reported HTN occurred in 23.6% of women (95% CI, 23.1–24.1). Regarding sociodemographic factors, the average age of respondents was 40.7 years, with about 23.4% of them aged 50 years or older. Levels of education, in general, were low, with 26.4% having received no formal/primary education, about 64.3% attained secondary school education, and a majority of them (84.5%) were black or Africans. About half (50.3%) reported that they had never been married and approximately three-quarters of respondents (71.3%) were not currently employed. A majority of respondents (86.3%) were not covered by health insurance and about 42.4% had access to all three forms of media. More than half of the respondents (55.2%) resided in urban areas. Regarding health and lifestyle factors, a majority of respondents (76.7%), reported normal BMI and 13.0% reported their self-rated health as excellent. Intake of fruits and vegetables in general, was low, with about 51.0% and 40.0% of respondents failing to consume any type of fruits and vegetables in the last 24 h, respectively. About one-third of the participants consumed fried foods and processed meat at least once a week. Similarly, one-third of the respondents had taken sugar-sweetened drinks in the last 24 h before the data collection.
Comparison of the self-reported hypertension rates among the study respondents
Table 2 compares the prevalence of self-reported HTN among women of different characteristics. In terms of sociodemographic characteristics, respondents of different age (χ2 = 1362.1, df = 6, P < 0.001), ethnicity (χ2 = 19.2, df = 2, P < 0.001), education (χ2 = 315.3, df = 2, P < 0.001), household wealth (χ2 = 49.5, df = 4, P < 0.001), marital status (χ2 = 469.9, df = 2, P < 0.001), exposure to mass media (χ2 = 31.1, df = 3, P < 0.0001), type of place of residence (χ2 = 11.0, df = 1, P = 0.001), and geographical region (χ2 = 121.5, df = 1, P < 0.001) had statistically different self-reported hypertensive rates. In terms of health, life styles, and other comorbidities, respondents of different perceived BMI (χ2 = 79.8, df = 2, P < 0.001), perceived health (χ2 = 505.2, df = 3, P < 0.001), frequency of eating processed meat (χ2 = 76.8, df = 3, P < 0.001), frequency of eating fried foods (χ2 = 51.5, df = 3, P < 0.001), sugar-sweetened drinks (χ2 = 24.2, df = 1, P < 0.001), presence of other comorbidities (χ2 = 132.3, df = 1, P < 0.001) had also significantly reported different hypertensive rates.
Factors associated with self-reported hypertension
Table 3 shows factors associated with self-reported HTN among women in South Africa. In this study, the significant predictors of self-reported HTN were the category of the respondent’s age, ethnicity, levels of education, marital status, insurance coverage, geographical region, self-rated body weight, SRHS, and presence of other comorbidities. Compared to respondents of age group 50 years and above, those aged 20 to 24 years (aOR, 0.04; 95% CI, 0.03–0.06) had reduced odds of self-reported HTN. Respondents who had never been married (aOR, 0.69; 95% CI, 0.56–0.85) had also lower odds of self-reported HTN compared to respondents who were formerly married. Furthermore, respondents who had no insurance coverage (aOR, 0.74; 95% CI, 0.58–0.95) had reduced odds of self-reported HTN compared to their counterparts who had insurance coverage. On the other hand, increased odds of self-reported HTN were observed in respondents who perceived their body weight to be overweight (aOR, 1.72; 95% CI, and 1.40–2.11), compared to respondents who perceived their body weight as normal. Being black/African (aOR, 1.73; 95% CI, 1.17–2.54), perception of having poor health status (aOR, 3.53; 95% CI, 2.53–5.211), and the presence of other comorbidities (aOR, 7.92; 95% CI, 3.63–17.29) increased the odds of self-reported HTN. Other predictors that increased the odds of self-reporting HTN included being resident of Western Cape (aOR, 2.70; 95% CI, 1.80–4.05), Eastern Cape (aOR, 2.31; 95% CI, 1.67–3.18), Northern Cape (aOR, 3.01; 95% CI, 2.06–4.40), Free State (aOR, aOR, 2.16; 95% CI, 1.52–3.07), North West (aOR, 2.75; 95% CI, 1.97–3.85), Gauteng (aOR, 1.75; 95% CI, 1.20–2.25), and Mpumalanga (aOR, 1.70; 95% CI, 1.21–2.38) compared to being a Limpopo dweller.
Discussion
The present study revealed a considerable high prevalence (23.6%; 95% CI, 23.1–24.1) of self-reported HTN among women in South Africa. Thus, efforts to reduce the burden of HTN can improve the quality of life among women. Even though the present study was exploratory in nature, it has revealed some important factors that may be worthy of the future investigation. The study found that the age of the respondents, ethnicity, education status, marital status, insurance coverage, geographical region, self-rated body weight, SRHS, and presence of other comorbidities were the significant predictors of self-reported HTN.
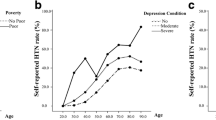
In line with previous studies [11, 12, 33,34,35], the current study revealed that age was associated with the likelihood of the respondents to have a self-reported HTN. The results also revealed a clear dose–response relationship such that the likelihood of respondents having self-reported HTN increased with an increase in age. HTN has been linked with numerous health hazards, and the incidence of this condition is reported to be common among older people [36]. Generally, previous researchers have argued that HTN is a result of arterial stiffness, thickness, loss of elasticity, and stenosis of the aorta and arterial wall, a state that is attributed to aging [37]. Prior researchers have also shown that aging is also associated with inflammation, oxidative stress, and endothelial dysfunction the conditions that jointly influence the health risks of late-life HTN [38,39,40]. Furthermore, empirical evidence has demonstrated that older people tend to have more functional disorders as physical activity declines [41, 42] a phenomenon that increases the likelihood of reporting HTN. Others have also reported that the risk of HTN is high in older people since they pay less attention to their health and are more likely to have financial constraints that hinder them from accessing health care [43].
In line with prior research [44, 45], lower education levels (secondary education and lower) were associated with the likelihood of having self-reported HTN. Education has been reported to play a vital role in guarding against diseases that are influenced by lifestyle such as diabetes [44]. Thus, higher levels of education may enable attainment of social, psychological, and economic positive skills and assets, and may offer insulation from various adverse stimuli [46]. Furthermore, a number of studies have suggested that educational interventions can improve HTN knowledge, health behaviors, and blood pressure control [47]. Additionally, there is clear evidence on the impact of educational level on lifestyle, nutrition, and physical activity [48], of which the three aforementioned characteristics have an impact on HTN [49].
The likelihood of having self-reported HTN was high in blacks or Africans. Our results are in line with finding from Brazil [13, 50], and the United States [51, 52] where high prevalence rates of self-reported HTN was reported in black women than white women. The probable factors related to the higher prevalence of self-reported HTN in the black population are thought to be genetic predisposition [53], poor economic conditions [54], less access to health services, and stress due to racial discrimination [55, 56]. In line with other studies in South Africa, a survey in Cape Town confirmed very high levels of HTN among black South Africans than whites [57]. Similarly, multiple surveys conducted in urban areas of South Africa had documented higher blood pressures in blacks compared to whites [58, 59].
Having a stable health insurance coverage is often related to improved chronic disease outcomes (such as HTN, diabetes, cancer, and CVD) by ensuring reliable access to outpatient services including detection of disease, disease monitoring, and medications [60,61,62]. Generally, patients that have health insurance coverage are reported to have better access to health care [63, 64] and a number of previous studies have reported that patients with health insurance coverage had an increased odds of achieving blood pressure control compared to their counterparts without health insurance [60, 65]. Surprisingly, in this study, respondents who had no health insurance coverage exhibited a lower likelihood of having self-reported HTN. The reasons may be that uninsured individuals might be less likely to receive preventive services for chronic conditions such as diabetes, cancer, and CVD, a phenomenon that might make them unaware of their present health conditions. On the other hand, previously, it was reported that residents of Free State, Mpumalanga, and KwaZulu-Natal [11, 20] had higher odds of HTN in South Africa. However, in this study, it was found that additional provinces namely Western Cape, Eastern Cape, Northern Cape, North West, Gauteng, and Mpumalanga exhibited increased odds of having self-reported HTN. Thus, forthcoming studies should consider the probable causes for higher odds of self-reported HTN in those additional provinces.
Consistent with previous studies [66, 67], the current study also revealed that marital status was associated with HTN. In particular, those that were never married had a reduced likelihood of having self-reported HTN. In previous cross-section studies, it was reported that those that were not married (divorced, separated, or widowed) and never married individuals were found to have a higher prevalence of HTN compared to their married counterparts [68]. Furthermore, longitudinal studies have reported somewhat inconsistent results where no associations were found between marital status and change in marital status and HTN [69]. The mechanisms by which marital status influences HTN are poorly understood. However, previous researchers have suggested some reasons for the influences of marital status that include psychopathological factors, health behaviors including physical activities and diet adherence, neuroendocrine pathways, and biological mediators and immune pathways [69]. It is believed that married people have less stress, better sleep, better moods, and have a more healthy diet compared to the never married counterparts [66]. Thus, the results of the current study need further investigation.
In this study, overweight/obesity emerged as a significant predictor associated with self-reported HTN among women. These results are in line with the findings from some of the previous work in different parts of the world i.e., that reported on the HTN which was measured objectively [70,71,72,73]. Generally, the specific mechanisms through which overweight/obesity result in HTN are complex and poorly understood. However, previous researchers have documented that neuroendocrine mechanisms and, lately, factors derived from adipose are believed to play a major role [74, 75]. On the other hand, overweight/obesity might induce HTN and other CVD by activating the renin–angiotensin–aldosterone system, increasing sympathetic activity, promoting insulin resistance and leptin resistance, increased procoagulatory activity, and endothelial dysfunction [75]. Additionally, other mechanisms involve an increased renal sodium reabsorption that causes a shift of the pressure natriuresis; thus, causing extracellular fluid volume expansion [76]. Furthermore, overweight/obesity may increase the risk of HTN through subclinical inflammation.
As with previous studies [77,78,79], the current study found an association between poor SRHS and the likelihood of self-reported HTN. Previous researchers have used this simple and relatively subjective SRHS to predict chronic disease morbidity including CVD [80,81,82], cardiovascular mortality [83,84,85], and all‐cause mortality [86,87,88,89]. In line with prior research [80, 81], respondents who reported having poor SRHS had high chances of having self-reported HTN in this study. The mechanisms through which SRHS induces HTN are not clearly stated. However, SRHS in previous studies has been reported to be closely associated with social integration and adaptability to psychosocial stress [90, 91]. The probable clarifications for the observed relationship between SRHS and the occurrence of severe HTN may comprise the stated association between poor SRHS and associated negative psychosocial variable gathering to the metabolic syndrome [92], increased markers of inflammation and insulin resistance that result in increasing blood sugar [93, 94], sleep apnea and disordered sleep [95], and elevated levels of cortisol and low levels and adrenal androgen.
In this study, the presence of other chronic comorbidities of diabetes and hypocholesteremia had a high likelihood of having self-reported HTN. Our results are in agreement with similar findings from previous studies [96,97,98,99], where dyslipidemia, obesity, and impaired fasting glucose were reported to be the most common comorbidities of hypertensive patients. However, in this study we only considered self-reported diabetes and self-reported hypocholesteremia as comorbidities of self-reported HTN due to the availability of data. Another study reported that seven of the eight chronic conditions were more prevalent in hypertensive patients than in adults without HTN [96]. Generally, HTN, diabetes, and hypercholesterolemia share common pathways and are interrelated [100]. It is established that hypercholesterolemia facilitates HTN by decreasing coronary blood flow reserve and capillary density; and inducing apoptosis of capillary endothelial cells and eventually resulting in impaired left ventricular function [101]. Furthermore, it is believed that hypercholesterolemia may alter membrane lipid bilayer [102], and may alter the regulation of intracellular calcium ions; thus, excess calcium uptake could directly contribute to atherogenesis [103] and eventually, that may lead to the development of atherosclerosis.
Similarly, there is a significant overlap between diabetes and HTN in the causes and disease pathophysiology [104]. It is established that renal sodium control differs in diabetes since there is an upregulation of sodium transporters in the kidneys [105]. Thus, the renin–angiotensin–aldosterone system may be upregulated in diabetes, resulting in increased blood pressure through a direct effect mediated by angiotensin II [106], as well as indirectly through upregulation of sympathetic activity [107]. Another essential connection between HTN and diabetes is the occurrence as well as the progression of diabetic kidney disease [108], the pathophysiology of which is mediated through several pathways including endothelial dysfunction and advanced glycation end-products [109]. Furthermore, obesity and metabolic syndrome, through their effects on various hormones and inflammation pathways, may also influence the occurrence of HTN and diabetes [107].
This study has several strengths. Firstly, the use of a nationally representative sample makes the results of the current study generalizable to the specified population. Secondly, the analysis controlled for a wide range of characteristics, thus strengthening the observed associations. However, we are aware of the potential limitations of the current study. Firstly, this study utilized a cross-sectional design. Therefore, the temporal relationship between self-reported HTN and its associated factors could not be established in this study. Secondly, the outcome measure and other independent variables were self-reported diagnoses; thus, our results are prone to recall bias. Thirdly, it should be noted that chronic conditions such as HTN are frequently under-reported or incorrectly reported by patients, and therefore, the results should be interpreted with caution.
Conclusions
Self-reported HTN was largely associated with multiple sociodemographic, health, and lifestyle factors as well the presence of other chronic conditions. Health education, promotion, and services aiming at reducing the burden of HTN in South Africa should consider self-reported HTN and the associated factors reported in this study to ensure healthy aging and quality of life among women.
Availability of data and materials
The datasets generated and/or analyzed during the present study are available in the DHS Program repository: https://dhsprogram.com/data/dataset/South-Africa_Standard-DHS_2016.cfm?flag=1.
Abbreviations
- aOR:
-
Adjusted odds ratio
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- DU:
-
Dwelling unit
- EA:
-
Enumeration area
- HTN:
-
Hypertension
- PSU:
-
Primary sampling unit
- SADHS:
-
South Africa Demographic and Health Survey
- SRHS:
-
Self-rated health status
- WHO:
-
World Health Organization
References
World Health Organization (WHO). Hypertension. Geneva: WHO; 2022. (https://www.who.int/news-room/fact-sheets/detail/hypertension Available from [cited 2022 Feb 19]).
Iqbal AM, Jamal SF. Essential hypertension. Treasure Island: StatPearls; 2022.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–50.
United Nations. High blood pressure now more common in low and middle-income countries, new report finds. New York: United Nations; 2021. (https://news.un.org/en/story/2021/08/1098342 Available from[cited 2022 Feb 19]).
Kulkarni S. Hypertension management in 2030: a kaleidoscopic view. J Hum Hypertens. 2021;35:812–7.
Kunes J, Zicha J. The interaction of genetic and environmental factors in the etiology of hypertension. Physiol Res. 2009;58(Suppl 2):S33-42.
Wu T, Snieder H, Li L, Cao W, Zhan S, Lv J, et al. Genetic and environmental influences on blood pressure and body mass index in Han Chinese: a twin study. Hypertens Res. 2011;34:173–9.
Biino G, Parati G, Concas MP, Adamo M, Angius A, Vaccargiu S, et al. Environmental and genetic contribution to hypertension prevalence: data from an epidemiological survey on Sardinian genetic isolates. PLoS ONE. 2013;8:e59612.
World Health Organization (WHO). Noncommunicable diseases. Geneva: WHO; 2021. (https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases Available from[cited 2022 Feb 19]).
Brandão MP, Sa-Couto P, Gomes G, Beça P, Reis J. Factors associated with cardiovascular disease risk among employees at a Portuguese higher education institution. Int J Environ Res Public Health. 2022;19:848.
Gupta RD, Talukder A, Hossain M, Akonde M, Kibria A, Muhammed G. Prevalence and associated factors of hypertension among South African adults: findings from the Demographic and Health Survey 2016. J Public Health. 2021. https://doi.org/10.1007/s10389-021-01607-w.
Sharma JR, Mabhida SE, Myers B, Apalata T, Nicol E, Benjeddou M, et al. Prevalence of hypertension and its associated risk factors in a rural Black population of Mthatha town, South Africa. Int J Environ Res Public Health. 2021;18:1215.
Malta DC, Bernal RT, Andrade SS, Silva MM, Velasquez-Melendez G. Prevalence of and factors associated with self-reported high blood pressure in Brazilian adults. Rev Saude Publica. 2017;51(suppl 1):11s.
Ekholuenetale M, Barrow A. Prevalence and determinants of self-reported high blood pressure among women of reproductive age in Benin: a population-based study. Clin Hypertens. 2020;26:12.
Dyer AR, Stamler J, Shekelle RB, Schoenberger J. The relationship of education to blood pressure: findings on 40,000 employed Chicagoans. Circulation. 1976;54:987–92.
Jones HJ, Ibemere S, Gaillard T, Harris A, Anthony J, Shambley-Ebron D. Factors associated with self-reported hypertension among Black women. J Natl Black Nurses Assoc. 2020;31:32–8.
Ab Majid NL, Rodzlan Hasani WS, Mat Rifin H, Robert Lourdes TG, Jane Ling MY, Saminanthan TA, et al. Self-reported diabetes, hypertension and hypercholesterolemia among older persons in Malaysia. Geriatr Gerontol Int. 2020;20(Suppl 2):79–84.
Masilela C, Pearce B, Ongole JJ, Adeniyi OV, Benjeddou M. Cross-sectional study of prevalence and determinants of uncontrolled hypertension among South African adult residents of Mkhondo municipality. BMC Public Health. 2020;20:1069.
Khanam R, Ahmed S, Rahman S, Kibria GM, Syed JR, Khan AM, et al. Prevalence and factors associated with hypertension among adults in rural Sylhet district of Bangladesh: a cross-sectional study. BMJ Open. 2019;9:e026722.
Kandala NB, Nnanatu CC, Dukhi N, Sewpaul R, Davids A, Reddy SP. Mapping the burden of hypertension in South Africa: a comparative analysis of the National 2012 SANHANES and the 2016 Demographic and Health Survey. Int J Environ Res Public Health. 2021;18:5445.
Gonçalves VS, Andrade KR, Carvalho KM, Silva MT, Pereira MG, Galvao TF. Accuracy of self-reported hypertension: a systematic review and meta-analysis. J Hypertens. 2018;36:970–8.
de Andrade SS, Stopa SR, Brito AS, Chueri PS, Szwarcwald CL, Malta DC. Self-reported hypertension prevalence in the Brazilian population: analysis of the National Health Survey, 2013. Epidemiol Serv Saude. 2015;24:297–304.
Cheraghian B, Asadi-Lari M, Mansournia MA, Majdzadeh R, Mohammad K, Nedjat S, et al. Prevalence and associated factors of self-reported hypertension among Tehran adults in 2011: a population-based study (Urban HEART-2). Med J Islam Repub Iran. 2014;28:105.
Lavrakas PJ. Encyclopedia of survey research methods. Thousand Oaks: SAGE; 2008.
Andrade SS, Malta DC, Iser BM, Sampaio PC, de Moura L. Prevalence of self-reported arterial hypertension in Brazilian capitals in 2011 and analysis of its trends in the period between 2006 and 2011. Rev Bras Epidemiol. 2014;17(Suppl 1):215–26.
Dwyer-Lindgren L, Mackenbach JP, van Lenthe FJ, Mokdad AH. Self-reported general health, physical distress, mental distress, and activity limitation by US county, 1995–2012. Popul Health Metr. 2017;15:16.
Najafi F, Pasdar Y, Shakiba E, Hamzeh B, Darbandi M, Moradinazar M, et al. Validity of self-reported hypertension and factors related to discordance between self-reported and objectively measured hypertension: evidence from a cohort study in Iran. J Prev Med Public Health. 2019;52:131–9.
Jongen VW, Lalla-Edward ST, Vos AG, Godijk NG, Tempelman H, Grobbee DE, et al. Hypertension in a rural community in South Africa: what they know, what they think they know and what they recommend. BMC Public Health. 2019;19:341.
National Department of Health (NDoH), Statistics South Africa (Stats SA), South African Medical Research Council (SAMRC), ICF. South Africa demographic and health survey 2016. Pretoria: NDoH; 2019.
Pillay-van Wyk V, Msemburi W, Laubscher R, Dorrington RE, Groenewald P, Glass T, et al. Mortality trends and differentials in South Africa from 1997 to 2012: second National Burden of Disease Study. Lancet Glob Health. 2016;4:e642–53.
Chun H, Kim IH, Min KD. Accuracy of self-reported hypertension, diabetes, and hypercholesterolemia: analysis of a representative sample of Korean older adults. Osong Public Health Res Perspect. 2016;7:108–15.
World Health Organization. A healthy lifestyle: WHO recommendations. Geneva: WHO; 2022. (https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations Available from[cited 2022 Feb 6]).
The China PEACE Collaborative Group. Association of age and blood pressure among 3.3 million adults: insights from China PEACE million persons project. J Hypertens. 2021;39:1143–54.
Muli S, Meisinger C, Heier M, Thorand B, Peters A, Amann U. Prevalence, awareness, treatment, and control of hypertension in older people: results from the population-based KORA-age 1 study. BMC Public Health. 2020;20:1049.
Chiwandire N, Zungu N, Mabaso M, Chasela C. Trends, prevalence and factors associated with hypertension and diabetes among South African adults living with HIV, 2005–2017. BMC Public Health. 2021;21:462.
Buford TW. Hypertension and aging. Ageing Res Rev. 2016;26:96–111.
Sun Z. Aging, arterial stiffness, and hypertension. Hypertension. 2015;65:252–6.
Liguori I, Russo G, Curcio F, Bulli G, Aran L, Della-Morte D, et al. Oxidative stress, aging, and diseases. Clin Interv Aging. 2018;13:757–72.
Guzik TJ, Touyz RM. Oxidative stress, inflammation, and vascular aging in hypertension. Hypertension. 2017;70:660–7.
Higashi Y, Kihara Y, Noma K. Endothelial dysfunction and hypertension in aging. Hypertens Res. 2012;35:1039–47.
Donat Tuna H, Ozcan Edeer A, Malkoc M, Aksakoglu G. Effect of age and physical activity level on functional fitness in older adults. Eur Rev Aging Phys Act. 2009;6:99–106.
Ntenda PAM, Kazambwe JF. A multilevel analysis of overweight and obesity among non-pregnant women of reproductive age in Malawi: evidence from the 2015–16 Malawi Demographic and Health Survey. Int Health. 2019;11:496–506.
Fitzpatrick AL, Powe NR, Cooper LS, Ives DG, Robbins JA. Barriers to health care access among the elderly and who perceives them. Am J Public Health. 2004;94:1788–94.
Tedesco MA, Di Salvo G, Caputo S, Natale F, Ratti G, Iarussi D, et al. Educational level and hypertension: how socioeconomic differences condition health care. J Hum Hypertens. 2001;15:727–31.
Vargas CM, Ingram DD, Gillum RF. Incidence of hypertension and educational attainment: the NHANES I epidemiologic followup study: first National Health and Nutrition Examination Survey. Am J Epidemiol. 2000;152:272–8.
Liberatos P, Link BG, Kelsey JL. The measurement of social class in epidemiology. Epidemiol Rev. 1988;10:87–121.
Dawes MG, Kaczorowski J, Swanson G, Hickey J, Karwalajtys T. The effect of a patient education booklet and BP ‘tracker’ on knowledge about hypertension: a randomized controlled trial. Fam Pract. 2010;27:472–8.
Kautzky-Willer A, Dorner T, Jensby A, Rieder A. Women show a closer association between educational level and hypertension or diabetes mellitus than males: a secondary analysis from the Austrian HIS. BMC Public Health. 2012;12:392.
Jurik R, Stastny P. Role of nutrition and exercise programs in reducing blood pressure: a systematic review. J Clin Med. 2019;8:1393.
Lessa Í. Epidemiology of systemic arterial hypertension and heart failure in Brazil. Rev Bras Hipertens. 2001;8:383–92.
Samanic CM, Barbour KE, Liu Y, Fang J, Lu H, Schieb L, et al. Prevalence of self-reported hypertension and antihypertensive medication use among adults: United States, 2017. MMWR Morb Mortal Wkly Rep. 2020;69:393–8.
Yoon SS, Carroll MD, Fryar CD. Hypertension prevalence and control among adults: United States, 2011–2014. NCHS Data Brief. 2015;220:1–8.
Zilbermint M, Hannah-Shmouni F, Stratakis CA. Genetics of hypertension in African Americans and others of African descent. Int J Mol Sci. 2019;20:1081.
Cooper RS, Forrester TE, Plange-Rhule J, Bovet P, Lambert EV, Dugas LR, et al. Elevated hypertension risk for African-origin populations in biracial societies: modeling the Epidemiologic Transition Study. J Hypertens. 2015;33:473–81.
Deere BP, Ferdinand KC. Hypertension and race/ethnicity. Curr Opin Cardiol. 2020;35:342–50.
Forde AT, Sims M, Muntner P, Lewis T, Onwuka A, Moore K, et al. Discrimination and hypertension risk among African Americans in the Jackson Heart Study. Hypertension. 2020;76:715–23.
Steyn K, Levitt NS, Hoffman M, Marais AD, Fourie JM, Lambert EV, et al. The global cardiovascular diseases risk pattern in a peri-urban working-class community in South Africa: the Mamre Study. Ethn Dis. 2004;14:233–42.
Steyn K, Gaziano TA, Bradshaw D, Laubscher R, Fourie J, South African Demographic and Health Coordinating Team. Hypertension in South African adults: results from the Demographic and Health Survey, 1998. J Hypertens. 2001;19:1717–25.
Seedat YK, Seedat MA, Hackland DB. Prevalence of hypertension in the urban and rural Zulu. J Epidemiol Community Health. 1982;36:256–61.
Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–9.
Schoen C, DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health Serv Res. 2000;35(1 Pt 2):187–206.
Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. Hypertension, diabetes, and elevated cholesterol among insured and uninsured U.S. adults. Health Aff (Millwood). 2009;28:w1151-9.
Schober SE, Makuc DM, Zhang C, Kennedy-Stephenson J, Burt V. Health insurance affects diagnosis and control of hypercholesterolemia and hypertension among adults aged 20–64: United States, 2005–2008. NCHS Data Brief. 2011;57:1–8.
Duru OK, Vargas RB, Kermah D, Pan D, Norris KC. Health insurance status and hypertension monitoring and control in the United States. Am J Hypertens. 2007;20:348–53.
Oso AA, Adefurin A, Benneman MM, Oso OO, Taiwo MA, Adebiyi OO, et al. Health insurance status affects hypertension control in a hospital based internal medicine clinic. Int J Cardiol Hypertens. 2019;1:100003.
Ramezankhani A, Azizi F, Hadaegh F. Associations of marital status with diabetes, hypertension, cardiovascular disease and all-cause mortality: a long term follow-up study. PLoS ONE. 2019;14:e0215593.
Lipowicz A, Lopuszanska M. Marital differences in blood pressure and the risk of hypertension among Polish men. Eur J Epidemiol. 2005;20:421–7.
Tuoyire DA, Ayetey H. Gender differences in the association between marital status and hypertension in Ghana. J Biosoc Sci. 2019;51:313–34.
Schwandt HM, Coresh J, Hindin MJ. Marital status, hypertension, coronary heart disease, diabetes, and death among African American women and men: incidence and prevalence in the Atherosclerosis Risk in Communities (ARIC) Study participants. J Fam Issues. 2010;31:1211–29.
Dua S, Bhuker M, Sharma P, Dhall M, Kapoor S. Body mass index relates to blood pressure among adults. N Am J Med Sci. 2014;6:89–95.
van de Vijver SJ, Oti SO, Agyemang C, Gomez GB, Kyobutungi C. Prevalence, awareness, treatment and control of hypertension among slum dwellers in Nairobi. Kenya J Hypertens. 2013;31:1018–24.
Basu S, Millett C. Social epidemiology of hypertension in middle-income countries: determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension. 2013;62:18–26.
Hasan M, Sutradhar I, Akter T, Das Gupta R, Joshi H, Haider MR, et al. Prevalence and determinants of hypertension among adult population in Nepal: data from Nepal Demographic and Health Survey 2016. PLoS ONE. 2018;13:e0198028.
Engeli S, Sharma AM. Role of adipose tissue for cardiovascular-renal regulation in health and disease. Horm Metab Res. 2000;32:485–99.
Wiecek A, Kokot F, Chudek J, Adamczak M. The adipose tissue: a novel endocrine organ of interest to the nephrologist. Nephrol Dial Transplant. 2002;17:191–5.
Wofford MR, Hall JE. Pathophysiology and treatment of obesity hypertension. Curr Pharm Des. 2004;10:3621–37.
Shankar A, Wang JJ, Rochtchina E, Mitchell P. Association between self-rated health and incident severe hypertension among men: a population-based cohort study. Singapore Med J. 2008;49:860–7.
Barger SD, Muldoon MF. Hypertension labelling was associated with poorer self-rated health in the Third US National Health and Nutrition Examination Survey. J Hum Hypertens. 2006;20:117–23.
Dong W, Pan XF, Yu C, Lv J, Guo Y, Bian Z, et al. Self-rated health status and risk of ischemic heart disease in the China Kadoorie Biobank Study: a population-based cohort study. J Am Heart Assoc. 2017;6:e006595.
van der Linde RM, Mavaddat N, Luben R, Brayne C, Simmons RK, Khaw KT, et al. Self-rated health and cardiovascular disease incidence: results from a longitudinal population-based cohort in Norfolk. UK PLoS One. 2013;8:e65290.
Bao X, Borné Y, Yin S, Niu K, Orho-Melander M, Nilsson J, et al. The associations of self-rated health with cardiovascular risk proteins: a proteomics approach. Clin Proteomics. 2019;16:40.
Kaplan GA, Goldberg DE, Everson SA, Cohen RD, Salonen R, Tuomilehto J, et al. Perceived health status and morbidity and mortality: evidence from the Kuopio ischaemic heart disease risk factor study. Int J Epidemiol. 1996;25:259–65.
Appels A, Bosma H, Grabauskas V, Gostautas A, Sturmans F. Self-rated health and mortality in a Lithuanian and a Dutch population. Soc Sci Med. 1996;42:681–9.
Benjamins MR, Hummer RA, Eberstein IW, Nam CB. Self-reported health and adult mortality risk: an analysis of cause-specific mortality. Soc Sci Med. 2004;59:1297–306.
Barger SD, Cribbet MR, Muldoon MF. Participant-reported health status predicts cardiovascular and all-cause mortality independent of established and nontraditional biomarkers: evidence from a representative US sample. J Am Heart Assoc. 2016;5:e003741.
Ganna A, Ingelsson E. 5 year mortality predictors in 498,103 UK Biobank participants: a prospective population-based study. Lancet. 2015;386:533–40.
Fernández-Ruiz M, Guerra-Vales JM, Trincado R, Fernández R, Medrano MJ, Villarejo A, et al. The ability of self-rated health to predict mortality among community-dwelling elderly individuals differs according to the specific cause of death: data from the NEDICES cohort. Gerontology. 2013;59:368–77.
Feng Q, Zhu H, Zhen Z, Gu D. Self-rated health, interviewer-rated health, and their predictive powers on mortality in old age. J Gerontol B Psychol Sci Soc Sci. 2016;71:538–50.
Sargent-Cox KA, Anstey KJ, Luszcz MA. The choice of self-rated health measures matter when predicting mortality: evidence from 10 years follow-up of the Australian longitudinal study of ageing. BMC Geriatr. 2010;10:18.
Kristenson M, Olsson AG, Kucinskiene Z. Good self-rated health is related to psychosocial resources and a strong cortisol response to acute stress: the LiVicordia study of middle-aged men. Int J Behav Med. 2005;12:153–60.
Barger SD. Do psychological characteristics explain socioeconomic stratification of self-rated health? J Health Psychol. 2006;11:21–35.
Meyer JM, Nasrallah HA, McEvoy JP, Goff DC, Davis SM, Chakos M, et al. The Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Schizophrenia Trial: clinical comparison of subgroups with and without the metabolic syndrome. Schizophr Res. 2005;80:9–18.
Janszky I, Lekander M, Blom M, Georgiades A, Ahnve S. Self-rated health and vital exhaustion, but not depression, is related to inflammation in women with coronary heart disease. Brain Behav Immun. 2005;19:555–63.
Lekander M, Elofsson S, Neve IM, Hansson LO, Undén AL. Self-rated health is related to levels of circulating cytokines. Psychosom Med. 2004;66:559–63.
Akashiba T, Kawahara S, Akahoshi T, Omori C, Saito O, Majima T, et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest. 2002;122:861–5.
Noh J, Kim HC, Shin A, Yeom H, Jang SY, Lee JH, et al. Prevalence of comorbidity among people with hypertension: the Korea National Health and Nutrition Examination Survey 2007–2013. Korean Circ J. 2016;46:672–80.
Steinman MA, Lee SJ, John Boscardin W, Miao Y, Fung KZ, Moore KL, et al. Patterns of multimorbidity in elderly veterans. J Am Geriatr Soc. 2012;60:1872–80.
Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in U.S. adults, 1999–2006. NCHS Data Brief. 2010;(36):1–8.
Davila EP, Hlaing WM. Co-morbidities of emergency department patients admitted with essential hypertension in Florida. Ann Epidemiol. 2007;17:726–7.
Abdel-Zaher AO, Farghaly HS, El-Refaiy AE, Abd-Eldayem AM. Effect of hypercholesterolemia on hypertension-induced renal injury in rats: insights in the possible mechanisms. J Cardiovasc Med Cardiol. 2020;7:39–46.
Yao YS, Li TD, Zeng ZH. Mechanisms underlying direct actions of hyperlipidemia on myocardium: an updated review. Lipids Health Dis. 2020;19:23.
Subczynski WK, Pasenkiewicz-Gierula M, Widomska J, Mainali L, Raguz M. High cholesterol/low cholesterol: effects in biological membranes: a review. Cell Biochem Biophys. 2017;75:369–85.
Gleason MM, Medow MS, Tulenko TN. Excess membrane cholesterol alters calcium movements, cytosolic calcium levels, and membrane fluidity in arterial smooth muscle cells. Circ Res. 1991;69:216–27.
Cheung BM, Li C. Diabetes and hypertension: is there a common metabolic pathway? Curr Atheroscler Rep. 2012;14:160–6.
Poudel RR. Renal glucose handling in diabetes and sodium glucose cotransporter 2 inhibition. Indian J Endocrinol Metab. 2013;17:588–93.
Chawla T, Sharma D, Singh A. Role of the renin angiotensin system in diabetic nephropathy. World J Diabetes. 2010;1:141–5.
Libianto R, Batu D, MacIsaac RJ, Cooper ME, Ekinci EI. Pathophysiological links between diabetes and blood pressure. Can J Cardiol. 2018;34:585–94.
Van Buren PN, Toto R. Hypertension in diabetic nephropathy: epidemiology, mechanisms, and management. Adv Chronic Kidney Dis. 2011;18:28–41.
Alvarez E, Paradela-Dobarro B, González-Peteiro M, González-Juanatey JR. Impact of advanced glycation end products on endothelial function and their potential link to atherosclerosis. In: Lenasi H, editor. Endothelial dysfunction: old concepts new challenges. London: IntechOpen; 2018. p. 211–30.
Acknowledgements
We are sincerely grateful to the Monitoring and Evaluation to Assess and Use Results (MEASURE) Demographic and Health Surveys for allowing us to analyze the population-based datasets, which can be accessed through their archive repository (http://dhsprogram.com/data/available-datasets.cfm).
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. PAMN acquired the data and conducted the analysis. GCC, MPSM, and WME interpreted the results. PAMN, ON, and FNT drafted the first manuscript. GCC, MPSM, AK, and JN revised the draft for important intellectual content. All authors reviewed the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The data were de-identified to prevent the respondents’ identity from being revealed. All individuals who agreed to take part in the survey were asked to provide either written or verbal consent for the interview. Particularly, verbal consent was sought from participants who could not write or read. The Centre for Disease Control and Prevention granted a waiver of written consent per 45CFR46 for respondents who were unable to provide written consent but consented verbally. Ethical approval for the survey was obtained from the South Africa Medical Research Council and the Institutional Review Board of ICF. The Statistics South Africa implemented the data collection. All methods were conducted in accordance with the Declaration of Helsinki principles.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Questionnaire.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ntenda, P.A.M., El-Meidany, W.M.R., Tiruneh, F.N. et al. Determinants of self-reported hypertension among women in South Africa: evidence from the population-based survey. Clin Hypertens 28, 39 (2022). https://doi.org/10.1186/s40885-022-00222-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40885-022-00222-5