Abstract
Background
We report a rare and unusual case of intravesical migration of an intrauterine device with stone formation. The intrauterine device (IUD) is the most common method of reversible contraception in women. However, its insertion is not without risk, it can cause early or late complications. IUD can perforate the uterus wall and migrate into adjacent structures.
Case presentation
A 35 year-old female 5 gravid, 4 para has been benefited from intrauterine contraceptive device (IUCD) 5 years ago, she was presented to gynecological consultation for chronic pelvic pain with urinary symptoms. There was history of a good IUD insertion 5 years ago, considered expelled after one month of its pose. Physical examination was normal, but a pelvic ultrasound and a plain abdominal radiography allowed the detection of an IUD outside the uterine cavity, but inside bladder. A diagnostic and therapeutic cystoscopy was performed, and the IUD with calculus was successfully removed. There were no postoperative complications.
Conclusion
This case is reported to highlight and to reiterate the need to think about one of the rare complication of IUD insertion, which every practitioner must know, it’s the transuterovesical migration, before concluding wrongly to its expulsion. It’s a consequence of, non-compliance with the rules for inserting an IUD and poor monitoring. The evolution towards calcification is a certain consequence; its screening involves rigorous clinical monitoring.
Similar content being viewed by others
Introduction
The intrauterine device (IUD), is an effective, safe and practical contraceptive choice for many women with some 100 million users, it is currently the most popular reversible contraceptive method in the world [1].
Inserting the IUD is a simple medical procedure. However, it is not devoid of risk, especially when insertion techniques are not followed up. It can cause early or late complications, such as bleeding, gynecological infections, expulsion or perforation with migration to adjacent structures, which is both rare and serious [2]. Approximately 1–3 of 1000 IUD insertions result in migration, and the bladder remains the most common destination of IUD migration. Various localization are reported in the literature such omentum, the broad ligament, pouch of Douglas (45%), colon, mesentery and sigmoid [1, 3].
We report a new case of bladder migration of IUD complicated by calculus formation.
Case
Mrs. K.B, 35 year old of rural origin, illiterate, 5 gravida, 4 para (3 vaginal deliveries and one cesarean section), one spontaneous abortion and 4 living children, presented to a gynecological consultation for chronic pelvic pain with burning micturition, pollakiuria, dysuria but without hematuria, resistant to usual therapies for 5 years ago.
The careful questioning of Mrs. K.B discerned in her medical history the notion of contraception by IUD, implemented 5 years ago on day 40th postpartum by a nurse known as a certified and trained health care provider.
The preinsertion counseling have been carried out, the patient didn’t have any contraindication to using IUD. The vaginal examination didn’t show any abnormalities, the uterus was in an anteversed and anteflexed position with normal size,
There was no doubt at the time of insertion, and the immediately check up after insertion was good; the IUD strings was visible in the vagina, and the IUD was at the right place in the uterus after ultrasound control.
The patient reported a pelvic pain for three days after the IUD insertion which subsided with simple analgesic treatment, without abnormal bleeding or urinary complaints. One month later, in the routine control, the nurse did not find any intravaginal IUD strings. Thus, the diagnosis of IUD expulsion was accepted and oral contraception was newly prescribed.
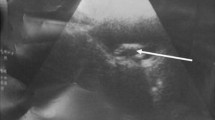
Since that time, the patient complained of pelvic pain with burning micturition, exacerbated in the 3rd trimester of the last pregnancy (delivery by cesarean section) but which was attributed to the pregnancy. Specialized urogenital examination is completely normal, but pelvic ultrasound allowed the detection of an IUD outside the uterine cavity, but inside bladder (Fig. 1).
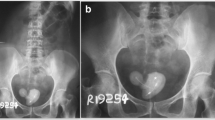
Additionally, Plain abdominal radiography showed the IUD projecting onto the bladder area (Fig. 2). The notion of expulsion of the IUD wrongly retained 5 years ago is eliminated and the diagnosis of secondary perforation of the uterus with migration of the IUD is admitted. The cytobacteriological examination of urine was negative and removal of the IUD under cystoscopy was indicated.
Cystoscopic exploration reveals the IUD firmly embedded in the bladder wall with calcifications (Fig. 3). Its removal was carried out without any incident and the post-operative follow up was simple.
The follow-up gynecological consultation, carried out 1 month after the removal of the IUD, noted the disappearance of the aforementioned symptoms. However, the patient was willing to use contraception such as tubal ligation.
Discussion
The IUD is one of the highly effective reversible methods of contraception. There are two types of products available: copper-coated IUDs or levonorgestrel-releasing IUDs. In the absence of contraindications, the IUD can be used in all women seeking a reliable reversible method of contraception with long-term contraceptive effectiveness that is less demanding in terms of compliance [2].
Patients with contraindications to estrogen or those are breastfeeding may be good candidates. The IUD is also used as morning-after contraception in women who have had unprotected sex for up to 7 days.
The intrauterine device has multiple mechanisms of action; it prevents both fertilization and implantation. The biochemical and morphological modifications produced by the IUD, and more particularly its inflammatory action on the endometrium, lead to a significant accumulation of lysosomal enzymes promoting endometrial destruction and migration [4].
Despite the wide use of IUD in recent years, there are still limitations for adolescents and nulliparous, but recent studies show that the IUD is safe for both of them to use [5].
Untrained Healthcare providers may constitute a danger for women wishing to use IUD. These women are significantly more likely to experience complications, which in turn can decrease demand for IUD services [6]. Therefore, it is imperative to stay up-to-date on guidelines for improving the quality of IUD services. Clinical follow-up is recommended after 4 to 12 weeks, if the IUD threads are not visible or in cases of atypical symptoms, an ultrasound examination should be performed. It can easily confirm whether the IUD is correctly positioned and often to highlight if there is any complications related to the IUD. Moreover, performing an ultrasound before placement to check up uterus measures and position can help for a successful placement [2]. A preinsertion informed consent is mandatory and requires that women understand benefits, technique, and possible complications.
Uterine perforation is a complication rarely observed following IUD insertion; its incidence varies from 1/350 to 1/2,500 insertions [7]. This incidence may be largely underestimated taking into account asymptomatic forms.
Uterine perforation ; partial or complete; usually occurs in the insertion moment of the IUD, Migration to the bladder and development of symptoms are long processes, its real etiology remains unknown. The risk factors for this perforation are essentially the insertion of an IUD in the postpartum or post abortum period, an inexperienced practitioner, multiparity, nulliparirty, scarred and immobile uterus and extremely anteverted or extremely retroverted uterus, the relationship between the size of the IUD and that of the uterine cavity, insertion technique, the use of force more than necessary, atrophic uterus [2, 7]. In our case, it seems that uterine perforation was probably happened at the time of forced insertion, as evidenced by the pain felt by the patient after insertion.
Therefore, it seems important after insertion of an IUD to check its correct positioning with a control ultrasound.
The transuterine migration of the IUD can take several directions to locate anywhere in the abdomen, a recent review illustrates that the bowel is the most affected organ in cases of perforated and migrated IUD (intestine 32%, colon 4%, appendix 1%, ileum 5%, rectum 12%, sigmoid 9%), the second most affected organ is the bladder (24%), often associated with lithiasis formation and urinary complaints [2].Vascular damage is exceptional; However, Ibghi described stenosis of the external iliac vein by an IUD [8].
The bladder location of an IUD is not always synonymous with trans utero-bladder migration. In some patients, a technical fault in the insertion of the IUD has been blamed, which can be accidentally placed in bladder via the transurethral route by inexperienced medical or paramedical profesionnals [9].
Uterine perforation by the IUD is often asymptomatic; most authors do not report any noisy symptoms during these perforations [3]. The disappearance of the reference threads is the first sign of migration (35%) [8], which must always be present in mind, before concluding in an unknown expulsion. It is only at the complication stage that the symptoms appear. Abdominal pain is the second revelatory signe (30%), followed by the occurrence of pregnancy (25%) and self-detection of IUD migration (11%) [10].
The bladder location of the IUD may be responsible for urinary symptoms consisting of Pollakiuria, burning micturition and dysuria, or even terminal hematuria, wrongly suggesting banal cystitis, as the case of our patient. The diagnosis is often mentioned on the plain abdominal radiography which shows the IUD with its metallic tone encompassed in an opacity of calcium tone because the stones are often radiopaque [11], but this is not constant. The diagnosis remains difficult if the IUD is not associated with bladder calculus.
Abdominal ultrasound confirms the bladder location of the IUD with or without stone formation. However, endovaginal ultrasound is more effective for studying the uterus (emptiness and/or possible partial perforation of the uterine wall by one of the arms of the IUD). This examination is more useful before insertion of the IUD because it allows the uterine anatomy to be clarified (anteverted or retroverted, dimensions, submucosal leiomyoma, congenital uterine anomalies). It must be repeated immediately afterwards and 4 to 12 weeks later to ensure the absence of uterine perforation [2].
Cystoscopy examination remains the most reliable diagnosis method, it’s the first stage of an endoscopic treatment. The use of computed tomography (CT), or even pelvic magnetic resonance imaging (MRI), is indicated in some cases, for better topographical characterization, and particularly in the case of associated pregnancy [12].
The IUD perforation of the uterine wall as well as its migration can be responsible in 0.1 to 0.9% of cases for serious complications such as pelvic abscesses, intestinal perforation and vesicoureteral fistula [7]. Furthermore, pelvic actinomycosis can develop, but the formation of bladder stones remains the most common possibility [13]. Indeed, bladder calculus in women is not common; it is 7 to 10 times less common than in men [14]. This is for anatomical and hormonal reasons. The formation of bladder calculus in women is favored by a local cause, a foreign body which may be an IUD.
The urinary infection and chronic inflammation which are almost always associated, plays a large part in calculus formation through ureolysis and the formation of struvite crystals. The migrated device act like foreign body over years and provides a bed for stone formation [11, 15].
Stone formation would be independent of the duration of presence of the IUD as a foreign body in the bladder. Vecsey reported the formation of a stone very early in 6 months after migration [16], while Kiilholma reported the non-formation of a stone on a Nova T type IUD that had migrated into the bladder for 3 years ago [17].
Extraction of the IUD can be done either endoscopically as we did in our case, or via laparotomy and bladder section. [18]. In the event of partial perforation of the bladder wall, laparoscopic extraction was described [19]. In cases of vesicouterine fistula, surgical treatment is often the rule. Conservative treatment by prolonged bladder drainage is rarely effective. In the case of associated actinomycosis, treatment is often dual, combining surgical excision and prolonged antibiotic therapy based on penicillin. The duration of treatment varies from 3 to 12 months. The outcome is often favorable without recurrence [9, 20].
Conclusion
This case is reported to highlight and to reiterate the need to think about one of the rare complication of IUD insertion, wich every practitioner must know, it’s transuterovesical migration, before concluding wrongly to its expulsion. It’s a consequence of, non-compliance with the rules for inserting an IUD and poor monitoring. The evolution towards calcification is a certain consequence; its screening involves rigorous clinical monitoring.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- IUD:
-
Intrauterine device
- IUCD:
-
Intrauterine contraceptive device
- MRI:
-
Magnetic resonance imaging
References
Aljohani A, Alzarea AA, Alnafee R, Aljadaani KS, Sairafi R, Alzahrani A. Migrated intrauterine device: case series report. Int J Surg Case Rep. 2023;111:108631.
Verstraeten V, Vossaert K, Van den Bosch T. Migration of intra-uterine devices. Open Access J Contracept. 2024;12:15.
Rasyid N, Nainggolan HJ, Jonardi PA, Raharja PAR, Wiweko B, Atmoko W, et al. Early-onset complete spontaneous migration of contraceptive intrauterine device to the bladder in a post C-section patient: a case report. Int J Surg Case Rep. 2021;82:105850.
Bahamondes L, Fernandes A, Monteiro I, Bahamondes MV. Long-acting reversible contraceptive (LARCs) methods. Best Pract Res Clin Obstet Gynaecol. 2020;66:28–40.
ACOG Committee Opinion No. 735: adolescents and long-acting reversible contraception: implants and Intrauterine devices. Obstet Gynecol. 2018;131(5):e130–9.
Gehani M, Pal M, Arya A, Singh S, O’Connell SK, Cagatay KA, Sengupta L, Singal S. Potential for improving intrauterine device (IUD) service delivery quality: results from a secondary data analysis. Gates Open Res. 2020;3:1473.
Yahsi S, Aktas BK, Erbay G, Salar R, Gokkaya CS. Intravesical migration of intrauterine device mimicking bladder stone on radiologic imaging: a case report. Indian J Surg. 2015;77(Suppl 1):97–9.
Ibghi W, Batt M, Bongain A, Declemy S, Proton A, Hassen- Kodhja R, Lepas P, Gillet JY. Iliac vein stenosis caused by intrauterine device migration. J Gynecol Obstet Biol Reprod. 1995;24:273–5.
Bacha K, ben amna M, Ben Hassine L, Ghaddab S, Ayed M. Intrauterine device migrating to the bladder. Prog Urol. 2001;11:1289–91.
Kassab B, Audra P. The migrating intrauterine device. Case report and review of the literature. Contracept Fertil Sex. 1999;27:696–700.
Bakri S, Azis A, Nusraya A, Putra MZDA, Natsir AS, Pattimura MIF. Intrauterine device (IUD) migration into the bladder with stone formation: a case report. Urol Case Rep. 2023;15:49102439.
Benaguida H, Kiram H, Ely Cheikh Telmoudi EC, Ouafidi B, Benhessou M, Ennachit M, Elkarroum M. Intraperitoneal migration of an intrauterine device (IUD): a case report. Annals Med Surg. 2021;68:102547.
Bakri S, Azis A, Nusraya A, Putra MZDA, Natsir AS, Pattimura MIF. Intrauterine device (IUD) migration into the bladder with stone formation: a case report. Urol Case Rep. 2023;49:102439.
Vidhyarthy AK, Hameed T, Lal R, Kumar A, Sahni S, Mendoza N. Giant bladder Calculus in an Adult- A persistent problem in the developing world: a Case Report. Clin Pract Cases Emerg Med. 2020;4(4):544–7.
Mhiri MN, Bayondh H, Mhiri CH, Rekik S, Smida L. Le Calcul vésical Chez La Femme à propos de 10 cas. J Gynécol Obst Reprod. 1990;19(8):979–82.
Vecsey D. Intrauterine device a rare foreign body in the urinary bladder. Med klin. 1988;83(17):575–6.
Kiilholma P, Makinen J, Vuori J. Bladder perforation: uncommon complication with a misplaced IUD. Adv Contracept. 1989;5:47.
Nouioui MA, Taktak T, Mokadem S, Mediouni H, Khiari R, Ghozzi S. A mislocated intrauterine device migrating to the urinary bladder: an uncommon complication leading to stone formation. Case Rep Urol. 2020; 2020:2091915.
Rowlands S, Oloto E, Horwell DH. Intrauterine devices and risk of uterine perforation: current perspectives. Open Access J Contracept. 2016;7:19.
Agil A, Tjahjodjati T, Atik N, Rachmadi N, Zahrina D. TT. Case Report: iatrogenic trauma of the bladder due to long-term unidentified intrauterine device malposition inside the bladder with rectovesical fistula. F1000Res 2024 Jan 5:121390.
Funding
The research did not receive a grant or any form of support from funding agents or authorities.
Author information
Authors and Affiliations
Contributions
H.H. conceptualized the case study and took the lead in drafting the manuscript. K.H. and B.F. provided the clinical details of the case study, conducted a literature review and participated in drafting the manuscript. A.B, L.B, A.A. and H.A. reviewed the literature and critically reviewed the manuscript. A.S. conceptualized the case study, provided supervision, participated in the literature review and in drafting the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Houmaid, H., Harou, K., Fakhir, B. et al. Migration of an intrauterine contraceptive device into the bladder complicated by stone formation an exceptional complication: case report and literature review. Contracept Reprod Med 9, 42 (2024). https://doi.org/10.1186/s40834-024-00302-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40834-024-00302-x