Abstract
Background
Despite significant advances in synthetic medicine, medicinal plants are still widely utilized to treat peptic ulcer disease. This study synthesized evidence on commonly used medicinal plants to manage peptic ulcer disease in Ethiopia.
Methods
The evidence was synthesized using electronic databases such as PubMed/Medline, Web of Science, Science Direct, Hinari, and Google Scholar. This review considers all controlled in vivo and ex vivo anti-ulcer studies evaluating Ethiopian medicinal plants with regards to phytochemistry, efficacy, and safety. The search technique covered all published papers using descriptors like Ethiopia, medicinal plants, and anti-ulcer until January 30, 2022. The percentage of ulcer reduction was used to measure the success of the treatment.
Results
Anti-ulcer properties were investigated in 13 papers. Twelve in vivo and one ex vivo study were retrieved. Osyris quadripartita, Plantago lanceolata, Ensete ventricosum, Taverniera abyssinicia, Crotonmacrostachyus Persea Americana and Moringa stenopetala showed effect close to a standard control in difference ulcer induced model. Osyris quadripartite in the dose of 200 mg/kg, Ficus thonningii in dose of 200 and 400 mg/kg, Plantago lanceolata in dose of 400 mg/kg, Trigonella feonum-gracum in dose of 500 and 1000 mg/kg, Linum ussitatissimum in dose of 1000 and 1500 mg/kg, Urtica simensis 400 mg/kg have higher activity compared with standard control in difference different models. Phytochemistry studies revealed presence of numerous components, including flavonoids, phenols, tannins, and saponins, which may be responsible for the anti-ulcer activity.
Conclusion
This study revealed that there are some promising medicinal plant extracts that have been used in Ethiopia for centuries that could be used as anti-ulcer agents. The most effective anti-ulcer agents in animal models are Indigofera spicata Forssk, Thymus schimperi, and Urtica simensis. Identification of most active pharmacological agents and clinical evaluation of Ethiopian medicinal plants used to treat peptic ulcers are worthy of further investigation.
Similar content being viewed by others
Introduction
Peptic ulcer disease (PUD) is acid-induced lesions in the stomach and duodenum characterized by denuded mucosa. Inflammatory or necrotizing disorders that affect the esophagus, stomach, and duodenum mucous membranes and are produced by an imbalance between destructive(acid and pepsin secretion) and defensive factors (mucus secretion, mucosal barrier, blood flow, cellular regeneration, blood flow, cell renewal and migration, non-enzymatic and enzymatic antioxidants, and some growth factors and endogenous protective chemicals) in the stomach usually aggravates peptic ulcers [5, 7, 11].
Endogenous and exogenous damaging factors that cause mucosal and submucosal erosion can contribute to the etiology of gastric and duodenal ulcers. Endogenous damaging factors in the stomach include HCl, pepsin, biliary reflux, lipid peroxidation, and the generation of reactive oxygen species (ROS). On the other hand, exogenous variables include excessive alcoholic consumption, indiscriminate use of nonsteroidal anti-inflammatory drugs(NSAID), immunosuppressive medications, serotonin reuptake inhibitors, alcohol consumption, stress, smoking, and Helicobacter pylori infection (H. pylori) [6, 11, 12, 19].
The majority of peptic ulcer disease occurrences are now most linked to H. pylori infection, the use of NSAIDs, or both. H. pylori colonizes the gastrointestinal mucosa, causing gastritis, peptic ulcer disease, and possibly gastric cancer [22].
PUD is one of the most common gastrointestinal disorders in the world which affects about 10% of the world population globally [9]. Around 4 million people are affected by these lesions worldwide, and 10–20% of cases develop complications, with a 10–40% mortality rate [2].. PUD affects over 4.5 million people in the United States alone each year, with a lifetime prevalence of about 8.4% [17, 22].
Conventional drugs currently used in the treatment of PUD (antacids, PPIs, H2 antagonists, anticholinergic, mucosal protective agents, and antimicrobials for H. pylori-induced PUD) have no long-term curative effect, and relapse is common after prolonged treatment. Moreover, these conventional drugs produce severe adverse reactions [25, 47]. As much as 50% of the western population uses herbal medicines as a therapy alternative, and about 10% use them to treat or prevent digestive issues [4]. Herbal medicine is used as a primary source of health treatment by an estimated 80 to 90% of Ethiopians [36]. Medicinal plants are one of the most often used drugs in the treatment of peptic ulcers, owing to their low cost, cultural acceptability, accessibility to people of lower socioeconomic position, and lesser side effects [13]. Many rural communities continue to rely on it [8]. Preliminary investigations on the scientific evidence of commonly used medicinal plants for peptic ulcer disease in Ethiopia have been conducted, but no evidence has yet been synthesized. This study was aimed to synthesize evidence on phytochemistry, effectiveness, and safety of medicinal plants used in Ethiopia in the management of peptic ulcers.
Methods
This study is a systematic review that followed the Preferred Reporting Items for Systematic Review and Meta-Analysis and the reporting [37]. PRISMA 2020. It looked at pre-clinical research on the anti-ulcer properties of Ethiopian medicinal herbs.
Information sources, searching, and selection of studies
The search engines used were electronic databases such as Hinari, PubMed/Medline, Web of Science, Medline, Science Direct, and Google Scholar as information sources. The review included published articles and thesis until Jan 2022; all available articles having descriptors were used in the search.
Eligibility criteria
Inclusion criteria
The following studies were included;
Studies conducted in laboratory animals or cell lines as disease models or in an in-vitro and in vivo study. These studies should use medicinal plants as a whole or parts in the experimental groups, with seed, root, flower, bud, and leaf extracts or single or complex medicinal plants, plant extracts, and plant preparations independent of how they were prepared (maceration, decoctions, tablets, capsules, pills, powders, injections, or other types of preparations), but no synthetic compounds were included.
The above studies should be published in English, including articles, thesis, essays, and proceedings, dealing with an anti-ulcer activity in vivo or in vitro research up to January 30, 2022.
Exclusion criteria
Previous reviews are excluded.
Data extraction
Three reviewers (AM and DH) independently conducted a literature search and examined relevant studies, screening their titles and abstracts for eligibility in a sequential manner. The full texts of studies that were considered to be potentially eligible were obtained. Disagreements were resolved after a discussion with other authors (SD and AN). The data were extracted using a pre-designed format. The data extracted includes the first author, study area, scientific, family, and local names, study model, animal type, extraction process, a component of the extract used, treatment time, and change in percentage of protection (from negative control and standard control) A study is included if the effect on negative control is mentioned; otherwise, it is eliminated.
Results
Characteristics of included studies
The electronic database search resulted in the discovery of 2678 articles. The total number of articles was decreased to 1648 after de-duplication. After screening the titles and abstracts, 13 papers remained. Eleven peer-reviewed articles and 2 M.sc theses were selected for inclusion (Fig. 1).
As shown in Table 1, 12 of the investigations were in vivo, while one was both in vitro and ex vivo. Study plants were collected from different regions of Ethiopia, and seven plants were collected from Amhara, five in Addis Ababa, and one in Oromia. The most obtained in-vivo anti-ulcer model was pylorus ligation anti-ulcer models and ethanol-induced.
Phytochemistry
All medicinal plant tested contained flavonoids, phenols, and saponins. Tannins present in all plant except in Trigonella feonum-gracum and Linum ussitatissimum. All except Cordia Africana have alkaloids and terpenoids, whereas Ficus thonningii exclusively has anthraquinones. Ficus thonningii, Urtica simensis, Solanum incanum L., and Rumex nepalensis contain glycosides (Table 2).
In vivo studies
In vivo trials varied significantly in treatment duration, ranging from 1 hour to 20 days. Studies were done using different animals and mice were utilized in four tests, rats in seven, and mice and rat were employed in two investigations. The plant was extracted using methanol in eight experiments, ethanol in one, and aqueous in the remaining four. Ensete ventricosum at a dose of 400 mg/kg provided notable ulcer control in pyloric-ligation ulcer induced rats with better ulcer reduction than the negative control. Osyris quadripartita, Plantago lanceolata, Ensete ventricosum, Taverniera abyssinicia, Crotonmacrostachyus Persea Americana and Moringa stenopetala showed effect close to a standard control in difference ulcer induced model. Osyris quadripartite in the dose of 200 mg/kg, Ficus thonningii in the dose of 200 and 400 mg/kg, Plantago lanceolata in the dose of 400 mg/kg, Trigonella feonum-gracum in the dose of 500 and 1000 mg/kg, Linum ussitatissimum in the dose of 1000 and 1500 mg/kg, Urtica simensis 400 mg/kg have higher activity compared with standard control in difference model (Table 3).
Ex vivo studies
The aqueous extract of Linum usitatissimum seed was found to dramatically reduce the contractile responses of both histamine and carbachol on isolated guinea ileum. With the lengthening of the soaking period, the extract’s potency increased significantly. Histamine and carbachol produced reproducible contractions quickly after removing the extract by washing the preparation [26].
Safety
The plant extracts utilized in this study were shown to be quite safe in acute toxicity tests in animals. Eleven plants, including Osyris quadripartite, Urtica simesis,Solanum incanum, Encete ventricosum,Crotonmacrostachyus hocsht, Plantago laceolata, Trigonella feonum, Linum ussitatissimum, Rumex nepalensis and Cordia Africana, had LD50 values greater than 2000 mg/kg [1, 3, 9, 20, 27,28,, 28, 29, 44, 45, 50]. Taverniera abyssinica has a median lethal dose (LD50) of 1409 mg/ml [35] (Table 4).
Discussion
This study reviewed 13 articles on medicinal plants of Ethiopia that have anti-ulcer properties. The majority of studies were carried out in animal model (12), with only one ex vivo study. Ensete ventricosum provided notable ulcer protection over 14 days compared to negative control and lower ulcer reduction compared to the standard control. Osyris quadripartita, Plantago lanceolata, Ensete ventricosum, Taverniera abyssinicia, Crotonmacrostachyus Persea Americana and Moringa stenopetala showed effect close to a standard control in difference ulcer induced model. Osyris quadripartite in the dose of 200 mg/kg, Ficus thonningii at dose of 200 and 400 mg/kg, Plantago lanceolata at dose of 400 mg/kg, Trigonella feonum-gracum at dose of 500 and 1000 mg/kg, Linum ussitatissimum at dose of 1000 and 1500 mg/kg, Urtica simensis 400 mg/kg have higher activity compared with standard control in different models.
The variation between the two studies on Urtica simensis could be owing to the geographical locations (Debra tebor versus Addis Ababa), solvents used, soil, or climatic factors.
Compared to studies conducted in India, the number of investigations on the anti-ulcer activity of Ethiopian medicinal herbs was smaller. In India, for example, a review revealed 40 and 64 plants with anti-ulcer efficacy [39, 49] and 58 from America [18]. This is maybe due lower availability of research centers in Ethiopia due to socioeconomic hurdles.
Several medicinal plants have long been utilized in Ethiopia to cure peptic ulcers; however, the number of plants investigated is low. This review evaluated previous research while emphasizing the need for more research. In the old idea, acid secretion was supposed to be the sole cause of ulcer formation, and lowering acid secretion was thought to be the main therapeutic method. However, recent research has led to a shift in this belief. The potentiation of the defensive system and the reduction of acid secretion are now the key goals of ulcer treatment. The world’s oldest medicinal systems can lead to the discovery of therapeutically effective plant remedies [39].
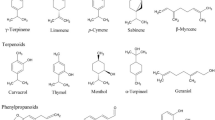
The finding of the study done on preliminary phytochemical analysis of selected medicinal plants revealed the presence of secondary phytochemicals. Flavonoids, Phenols, and Saponins were found in Osyris quadripartite, Ficus thonningii, Urtica simensis, Solanum incanum, Trigonella feonum, Linum usitatissimum, Rumex nepalensis, and Cordia Africana. Tannins was found in Osyris quadripartite, Ficus thonningii, Urtica simensis, Solanum incanum, Rumex nepalensis, and Cordia Africana. Anti-ulcer activities of these medicinal plants could be attributed to one or more of these secondary metabolites.
Medicinal plants are rich in bioactive compounds and have a wide range of pharmacological effects, including anti-ulcer activity. The activity could be attributed to a single phytochemical or a combination of phytochemicals. Alkaloids, phenolics, flavonoids, saponins, and tannins are some of the phytochemicals that could exert anti-ulcer activities [31, 38, 40].
Flavonoids are hypothesized to raise mucosal prostaglandin content, limit H. pylori growth, function as free radical scavengers, and inhibit H+/K + -ATPase, as well as decrease histamine production from mast cells by inhibition of histidine decarboxylase [10, 41].
Saponins may activate mucous membrane protective factors, while tannins make the mucosa’s outermost layer less receptive to chemical irritants [10]. Furthermore, terpenoids and alkaloid compounds have been shown to have powerful anti-ulcer action [24, 30].
To isolate, define, and standardize the active ingredients from herbal sources, ethno-medical knowledge supplemented by modern research is required. By combining traditional and current knowledge, improved anti-ulcer medications with fewer adverse effects can be developed. Although the experimental evaluation of herbal medications for peptic ulcers is excellent, there is no clinical trial on Ethiopian medicinal plants for anti-ulcer activity. This demonstrates that the advantages of study are not reaching the individuals who are the focus of medical research, so time, energy, and resources are being wasted. As a result, pharmacologists must devote more time to investigating herbal medications for possible anti-ulcer action and standardizing such herbal drugs for them to be clinically efficacious and globally competitive.
Numerous therapeutic plants can be found worldwide, but less than one-third of them have had their medical properties determined. More thorough and trustworthy scientific investigations are still required to assess and guarantee the efficacy of medicinal plants and their potential metabolites in the treatment of ulcers. The research included in this paper was conducted entirely using crude plant extract. Future research can use the findings of this study to isolate the active components and turn them into conventional drugs.
Conclusions
According to the findings of this study, some medicinal plants that have been used in Ethiopia for centuries were found to be a promising compound as anti-ulcer agents. The most effective anti-ulcer agents in animal models were Indigofera spicata Forssk, Thymus schimperi, and Urtica simensis. This study found that medicinal plants used in Ethiopia to treat peptic ulcers are worthy of additional research into pharmacologically active components and clinical trials. To collaborate the stated effectiveness of commonly used medicinal plant species, more in vitro, in vivo, and clinical research are needed.
Availability of data and materials
The data supporting the conclusions of this article are included within the article and its supplementary files.
Abbreviations
- ARRIVE:
-
Animal Research: Reporting of In vivo Experiments
- H.Pylori :
-
Heliobacter pylori
- LD50 :
-
Median lethal dose
- NSAID:
-
Nonsteroidal anti-inflammatory drug
- PPI:
-
Proton pump inhibitors
- PRISMA:
-
Preferred Reporting Items for Systematic Review and
Meta-Analysis
- PUD:
-
Peptic ulcer disease
- SYRCLE’s:
-
Systematic Review Centre for Laboratory Animal Experimentation
References
Abebaw M, et al. Evaluation of anti-ulcer activity of the leaf extract of Osyris quadripartita Decne.(Santalaceae) in rats. Dove Medical Press. 2017;9:1.
Adane H, et al. Evaluation of in vivo antiulcer activity of hydro-methanol extract and solvent fractions of the stem bark of Ficus thonningii (Moraceae) on rodent models. Bio Med Res Int. 2021;2021:6685395.
Ahmed O. Evaluation of anti-gastric ulcer activity of aqueous and 80% methanol leaf extracts of Urtica simensis in rats. University. University repository; 2019.
Akinbo F, Eze GJE. Combined effects of medicinal plants on induced upper gastrointestinal tract injury in wistar rats. Ethiop J Health Sci. 2016;26(6):573–80.
Al Batran R, et al. In vivo antioxidant and antiulcer activity of Parkia speciosa ethanolic leaf extract against ethanol-induced gastric ulcer in rats. PLoS One. 2013;8(5):e64751.
Alqasoumi S, et al. Rocket “Eruca sativa”: a salad herb with potential gastric anti-ulcer activity. World J Gastroenterol: WJG. 2009;15(16):1958.
AlRashdi AS, et al. Mechanisms of gastroprotective effects of ethanolic leaf extract of Jasminum sambac against HCl/ethanol-induced gastric mucosal injury in rats. Evid-Based Complement Alter Med. 2012;2012 https://doi.org/10.1155/2012/786426.
Belayneh A, et al. Medicinal plants potential and use by pastoral and agro-pastoral communities in Erer Valley of Babile Wereda, eastern Ethiopia. J Ethnobiol Ethnomed. 2012;8(1):1–11.
Belayneh YM, et al. Evaluation of the antiulcerogenic activity of hydromethanol extracts of Solanum incanum L.(Solanaceae) leaves and roots in mice; single and repeated dose study. Metabolism Open. 2021;11:100119.
Borrelli F, Izzo AA. The plant kingdom as a source of anti-ulcer remedies. Phytother Res. 2000;14(8):581–91.
Brito SA, et al. Antiulcer activity and potential mechanism of action of the leaves of Spondias mombin L. Oxidative Med Cell Longev. 2018;2018 https://doi.org/10.1155/2018/1731459.
Calam J, Baron J. Pathophysiology of duodenal and gastric ulcer and gastric cancer. Br Med J. 2001;323(7319):980–2.
Carrasco V, et al. Antiulcer activities of the hydroethanolic extract of Sedum dendroideum Moc et Sessé ex DC. (balsam). J Ethnopharmacol. 2014;158:345–51.
de Jesus NZ, et al. Tannins, peptic ulcers and related mechanisms. Int J Mol Sci. 2012;13(3):3203–28.
de Sousa Falcão H, et al. Gastric and duodenal antiulcer activity of alkaloids: a review. Molecules. 2008;13(12):3198–223.
Demarque DP, et al. The role of tannins as antiulcer agents: a fluorescence-imaging based study. Rev Bras. 2018;28(4):425–32.
Dunlap JJ, Patterson S. Peptic ulcer disease. Gastroenterol Nurs. 2019;42(5)
Falcão HS, et al. Plants of the American continent with antiulcer activity. Phytomedicine. 2008;15(1):132–46.
Gasparetto M, et al. Helicobacter pylori eradication therapy: current availabilities. Int Scholar Res Notice. 2012;2012 https://doi.org/10.5402/2012/186734.
Hailu D. Anti-ulcer activity of aqueous root extract of Ensete ventricosum (Welw.) Cheesman (Musaceae) in experimental rats. a. a. university. University Repository; 2021.
Jain PJNPR. Secondary metabolites for antiulcer activity. Nat Prod Res. 2016;30(6):640–56.
Kavitt RT, et al. Diagnosis and treatment of peptic ulcer disease. Am J Med. 2019;132(4):447–56.
Khan MSA, et al. Fruit-derived polysaccharides and Terpenoids: recent update on the Gastroprotective effects and mechanisms. Front Pharmacol. 2018;9:569.
Klein-Júnior LC, et al. The therapeutic lead potential of metabolites obtained from natural sources for the treatment of peptic ulcer. Phytochem Rev. 2012;11(4):567–616.
Kumar R. Glacier pothole. In: Singh VP, Singh P, Haritashya UK, editors. Encyclopedia of snow, ice and glaciers. Netherlands: Dordrecht, Springer; 2011. p. 414–5.
Makonnen EJEJ. Is linum usitatissimum seed a potential medicine in the therapy of peptic ulcer? Ethiop J Health Dev. 1996;10(2)
Mekonnen AN, et al. Evaluation of Antiulcer Activity of 80% Methanol Extract and Solvent Fractions of the Root of Croton macrostachyus Hocsht: Ex Del. (Euphorbiaceae) in Rodents. Evid Based Complement Alternat Med. 2020;2020:2809270. https://doi.org/10.1155/2020/2809270.
Melese E, et al. Evaluation of the Antipeptic ulcer activity of the leaf extract of Plantago lanceolata L. in rodents. Phytother Res. 2011a;25(8):1174–80.
Mequanente S, et al. Gastroprotective effect of aqueous trigonella feonum-gracum and linumussitatissimum seed extracts in mice. Pharmacologyonline. 2006;2:324–34.
Mitra P, et al. Anti gastric ulcer activity of Amaranthus spinosus Linn. Leaves in aspirin induced gastric ulcer in rats and the underlying mechanism. SMU Med J. 2014;1(2):313–28.
Mohod SM, et al. Evaluation of antiulcer activity of methanolic extract of leaves of madhuca indica j.f. gmel in rats. Pharmacologyonline. 3:203–213.
Morikawa T, et al. Triterpene Saponins with Gastroprotective effects from tea seed (the seeds of Camellia sinensis). J Nat Prod. 2006;69(2):185–90.
Mota KS, et al. Flavonoids with gastroprotective activity. Molecules. 2009;14(3):979–1012.
Nascimento R, et al. Activity of alkaloids on peptic ulcer: What’s new? Molecules. 2015;20:929–50.
Noamesi BK, et al. Antiulcerative properties and acute toxicity profile of some African medicinal plant extracts. J Ethnopharmacol. 1994;42(1):13–8.
World Health Organization. WHO congress on traditional medicine 2008. Beijing declaration, WHO; 2011.
Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 2021;372
Paguigan ND, et al. Anti-ulcer activity of leguminosae plants. Arq Gastroenterol. 2014;51:64–7.
Rambhai PA, Sisodia S. Indian medicinal plants for treatment of ulcer: systematic review. Pharmac Biosci J. 2018:38–44. https://doi.org/10.20510/ukjpb/6/i6/179237.
Reddy VP, et al. Evaluation of anti-ulcer activity of Citrullus colocynthis fruit against pylorus ligation induced ulcers in male wistar rats. Int J Pharm Pharm Sci. 2012;4(2):446–51.
Repetto M, Llesuy S. Antioxidant properties of natural compounds used in popular medicine for gastric ulcers. Braz J Med Biol Res. 2002;35:523–34.
Serafim C, et al. A review of the role of flavonoids in peptic ulcer (2010–2020). Molecules. 2020;25(22):5431.
Sharifi-Rad M, et al. Antiulcer Agents: From Plant Extracts to Phytochemicals in Healing Promotion. Molecules. 2018;23(7):1751.
Sisay W, et al. Hydromethanolic crude extract of the leaf of Urtica simensis Hochst. Ex. A. Rich.(Urticaceae) acquires appreciable antiulcer effect: validation for in vivo antiulcer activity. Evid-Based Complement Alter Med. 2021;2021 https://doi.org/10.1155/2021/6591070.
Sisay Zewdu W, Jemere Aragaw T. Evaluation of the anti-ulcer activity of Hydromethanolic crude extract and solvent fractions of the root of Rumex nepalensis in rats. J Exp Pharmacol. 2020;12:325–37.
Sumbul S, et al. Role of phenolic compounds in peptic ulcer: an overview. J Pharm Bioallied Sci. 2011;3(3):361–7.
Toth-Manikowski SM, Grams ME. Proton pump inhibitors and kidney disease—GI upset for the nephrologist? Kidney Int Rep. 2017;2(3):297–301.
Vieira Júnior GM, et al. New steroidal saponins and antiulcer activity from Solanum paniculatum L. Food Chem. 2015;186:160–7.
Vimala G, Gricilda Shoba F. A review on antiulcer activity of few Indian medicinal plants. Int J Microbiol. 2014;2014:519590.
Yismaw YE, et al. Phytochemical and antiulcer activity screening of seed extract of Cordia africana lam (Boraginaceae) in pyloric ligated rats. Clin Pharmacol. 2020;12:67–73.
Acknowledgments
Not applicable.
Disclosure
The authors declare no competing interests.
Funding
There is no funding.
Author information
Authors and Affiliations
Contributions
AM was the one who came up with the concept and designed the study. SD, AN, and DH conducted literature searches, gathered data, and drafted the manuscript. The manuscript was written by AM. The final text was reviewed and approved by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they don’t have competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mustefa, A., Nardos, A., Hailu, D. et al. Phytochemistry, efficacy, and safety of medicinal plants used traditionally for the management of peptic ulcer diseases in Ethiopia: a systematic review. Clin Phytosci 9, 9 (2023). https://doi.org/10.1186/s40816-023-00362-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40816-023-00362-7