Abstract
Introduction
In patients treated for cardiac disease, loneliness is known to contribute negatively to health behavior, health outcome, and increase risk of cardiac and all-cause mortality. Even so, in health care research, social support interventional studies targeting patients who experience loneliness are lacking.
Aim
To determine the feasibility of an individually structured social support intervention targeting patients treated for cardiac disease who experience loneliness.
Design
A feasibility study based on randomized clinical trial design with 1:1 randomization to a 6-month social support program, plus usual care (intervention) versus usual care, (i.e., regular guidelines-based follow-up). Intervention: Patients classified as high risk lonely according to the High Risk Loneliness tool will be provided with an informal caregiver in the 6 months rehabilitation phase following cardiac disease treatment. The informal caregiver will be designated by the patient from the existing social network or a peer, depending on patients’ preferences. The core content of the intervention is through nurse consultations at baseline and 1, 3, and 6 months, to enhance and reinforce the informal caregiver’s competences to be a social support resource. The theoretical framework of the nurse consultations will be based on middle-range theory of self-care.
Outcome
Feasibility will be evaluated in terms of acceptability and adherence according to predefined feasibility criteria. The preliminary effect of the intervention on patient-reported outcomes, health behaviors, and health outcomes will be evaluated in the intervention and the control group at baseline and 1, 3, 6, and 12 months.
Discussion
The present study will contribute with knowledge on how to implement a feasible social support intervention targeting patients treated for cardiac disease who experience loneliness and, furthermore, investigate the preliminary effect on health behavior and health outcome in the early rehabilitation period.
Trial registration
The trial is registered on clinicaltrials.gov (NCT05503810) 18.08.2022.
Similar content being viewed by others
Introduction
Cardiac disease is a major cause of impaired quality of life and the leading cause of mortality worldwide [1]. In Denmark, approximately 27,000 people are treated for cardiac disease, i.e., ischemic heart disease with coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI), valve disease with transcatheter aortic valve replacement (TAVR) or surgical aortic valve replacement (SAVR), and arrhythmia with implantable cardioverter defibrillator (ICD), pacemaker implantation, or ablation [2]. One of the psychosocial factors that is known to contribute negatively to cardiac patients’ health behavior [3, 4], health outcome [5, 6], and cardiac and all-cause mortality [7,8,9,10] is loneliness. To illustrate, in a national study including 14,000 patients across cardiac diagnosis, it was found that feeling alone doubled 1-year mortality in analyses adjusted for baseline health status [9].
Loneliness can be defined as follows: “A distressing feeling that accompanies the perception that one’s social needs are not being met by the quantity or especially the quality of one’s social relationships” [11].
The link between loneliness and health outcomes is explained by two main hypotheses: (1) social support increases the feeling of trust and safety which helps to “buffer” the potentially harmful influences of stress-induced cardiovascular reactivity and (2) social support increases the motivation to make healthier choices [12, 13]. Besides, the impact of loneliness on health behaviors and health outcomes, and of similar importance, is that patients experience social support from network members as vital in order to handle the physical and psychological aftermath from in-hospital cardiac disease treatment [14,15,16]. This increased need for social support places patients with inadequate or sparse social support in a vulnerable situation in the early rehabilitation period.
Overall, the evidence on the link between loneliness and health has led to an elevated interest in intervening in this matter. Also, the European guidelines on cardiovascular disease prevention recommend the inclusion of a lack of social support as one of the core psychosocial risk factors in clinical practice [17]. However, in health care research, social support interventional studies targeting patients who experience loneliness is lacking. Therefore, it has yet to be demonstrated how to provide a feasible social support intervention and if improvement in perceived social support leads to improvements in health outcomes [18].
In the social integration literature [19,20,21,22], it is argued that interventions should be underpinned by a theoretical framework to increase the likelihood of achieving success. In this matter, social support interventions involving informal caregivers from patients existing social network have shown positive results. Also, caregiver-oriented strategies and psychological counseling have shown promising results on decreasing loneliness [23].
When structuring a social support intervention, evidence points that the intervention should be fitted to the needs and characteristics of the target population and, therefore, that it is advantageous to involve the target population in the design of the intervention [21]. In our own previous research, we have used patient involvement to illuminate potential preferences and barriers toward a social support intervention in patients with cardiac disease who experiences loneliness [24]. In this study, it was revealed that the intervention must meet the patient's individual preferences in relation to, e.g., the type of informal caregiver that provides the social support needed and intervention start-up time, frequency, and duration, in order to be an attractive proposition.
Based on findings from the patient involvement sessions, alongside the existing literature on loneliness and social support interventions, a study protocol for an intervention study targeting patients treated for cardiac disease who experience loneliness has been developed. As no previous studies have investigated an individually tailored social support intervention in this patient population, this initial study will be conducted as a feasibility trial [25]. Feasibility as a research method is chosen because it will provide valuable knowledge on acceptability, adherence, and attrition, as well as monitor potential deficiencies in the structure of the intervention.
Study hypothesis
We hypothesize that an individually structured social support intervention targeting patients with cardiac disease who experience loneliness has the potential to decrease loneliness which in turn decreases stress-induced cardiovascular reactivity and promotes health behaviors which altogether will be reflected in patients’ wellbeing and in health outcomes.
Study aims and objectives
The primary aim of the study is to determine the feasibility of an individually structured social support intervention targeting patients treated for cardiac disease who experience loneliness.
The secondary aim is to explore the preliminary evidence on the effect of the intervention on health behaviors and health outcomes. The results will be used to perform a sample size calculation in a potential future larger trial [26].
Trial design
A feasibility study based on randomized clinical trial (RCT) design. The RCT design with 1:1 randomization to a 6-month social support program, plus usual care (intervention) versus usual care, (i.e., regular guidelines-based follow-up [29], will provide preliminary evidence on the effect of the intervention on patient-reported outcomes, health behaviors, and health outcomes. To investigate the sustainability of a potential long-term effect of the intervention, the follow-up period will be 1 year.
Sample size
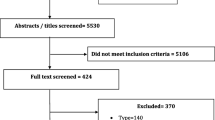
As the primary aim of this study is to test feasibility, there is no requirement for a formal power calculation [30]. Considerations about the sample size are related to the fact that no previous studies have investigated a social support intervention targeting patients with cardiac disease who experience loneliness and, therefore, no data exists on acceptability to the intervention. A sample size of 40 was chosen as it seems reasonable to exploratory investigate the feasibility, in particular acceptability, in a small sample and at the same time have a sample size big enough to investigate the additional aspects that are being assessed for feasibility [31]. Consequently, the study will include 20 patients and 20 informal caregivers in the intervention group and 20 patients in the control group. A flowchart of the trial is presented in Fig. 1.
Trial population, eligibility criteria, and randomization
Patients
Inclusion criteria: Three treatment groups, IHD (CABG or PCI), valve disease (TAVR, SAVR, surgical mitral valve procedures), and arrhythmia (ICD, pacemaker implantation or ablation) treated at Rigshospitalet and classified as high risk lonely according to the High Risk Loneliness (HiRL) tool [10], are given oral and written information about the study design and asked for permission to be contacted within 1 week from discharge to home. The HiRL screening tool has not yet been validated, but previous research suggest that the tool has a prognostic value for 1-year mortality, i.e., sensitivity 19.9% and specificity 89.5%, in patients treated for IHD. The HiRL screening tool is presented in Table 1. The final decision on participation must be taken by the patient within one week of discharge and patients will sign informed consent.
Exclusion criteria: Patients who are unable to provide written consent; thus, patients with severe cognitive or physical dysfunction will not be approached.
Randomization: Patients will be identified and screened consecutively. Randomization is completed using the web-based tool Randomizer for Clinical Trials. Patients will be stratified according to gender.
Patients who accept participation and who are included in the intervention group will receive further oral and written information about the intervention structure and sign informed content. In relation to this, they will be asked about their preference for the choice of an informal caregiver and for the structure of the intervention.
Informal caregivers
The informal caregiver is identified by the patient from two of the following options:
Social network member: This type of informal caregiver will be designated by the patient from the existing social network (e.g., a partner, friend, or neighbor), and the patient will be asked to initiate the contact with the social network member. If he/she accepts to be an informal caregiver, the intervention staff will contact the informal caregiver and give oral and written information, and if acceptance is confirmed, an inclusion-consultation will be performed subsequently. The consultation can be performed in-person or remote (phone or virtually). This consultation aims at investigating the potential caregiver’s prerequisites, resources, and motivation to participate with minimal risk of suffering from caregiver burden.
Exclusion criteria: Potential informal caregivers who are assessed as not having the necessary prerequisites or do not speak or understand Danish.
If the social network member does not accept to be an informal caregiver or if he/she is deemed to be at risk of caregiver burden, the patient will be given the opportunity to point out an alternative social network member to be an informal caregiver or to choose a peer as an informal caregiver.
Peer: This type of informal caregiver is defined as a person with similar disease as the recipient. The peer will be recruited by the Danish Heart Foundation from among volunteers in the existing peer support program.
Overall intervention structure
The core content of the intervention is through nurse consultations to enhance and reinforce the informal caregiver’s competences to be a social support resource. The intervention structure is based on the evidence on the positive impact of support provided by a peer (a person with similar disease as the recipient) [18, 32] or by a network member [23, 33] and the findings from patient involvement interview sessions performed by the project group [24]. Therefore, the patient will be provided with an informal caregiver in the long-term (6 months) rehabilitation phase following cardiac disease treatment. The role of the informal caregiver as a social support resource will be the same independent of which type of caregiver (social network member or peer) the patient has chosen. After choosing the type of informal caregiver, the patient will be asked about preferred frequency and form of contact with the informal caregiver. The patient and the informal caregiver are encouraged to be in contact a minimum of once a week in-person or remote (phone or virtually). The intervention staff will contact the informal caregiver and ask for acceptance of the suggested structure. If a need for adjustment of frequency or form occurs in the intervention period, patients and informal caregivers may arrange this together or in consultation with the intervention staff.
Furthermore, the patients will receive motivational text messages intended to enhance the supportive environment [34]. The text messages will be formulated by the research group and will be sent automatically to the patient on Mondays between 1 and 3 pm by a text message gateway “cpsms.” The wording of the text messages can, for example, be “The choices you make today shape the life you live tomorrow” or “Success is the sum of small efforts repeated.”
At enrollment, 1 month, and 3 and 6 months, an intervention nurse will contact the informal caregiver and provide guidance and counseling based on a theoretical framework derived from complementary fields, i.e., psychology with the theory of dyadic processes [12, 35] and nursing with self-care theory [36, 37]. These theoretical frames will inform the intervention nurse on which domains to focus on when guiding the informal caregiver. An intervention guide for the nurse is used in all nurse consultations. A description of the aim and method for each consultation described in the intervention guide is shown in Table 2.
The central themes are furthermore described in an easy-to-read langue, to be handed out to the informal caregiver as a pamphlet “Guide to HeartBuddy.”
Both patient and informal caregiver will be provided with the possibility of contacting an intervention nurse through an open hotline (workdays, daytime) if any additional questions arise during the intervention period.
Outcomes
Feasibility
The outcomes of the feasibility study will inform the design of a potential upcoming randomized control trial (RCT). The feasibility will be evaluated in terms of acceptability and adherence [38, 39]. Feasibility criteria are based on the balance between the financial and logistical resources of the intervention and the expected effect.
The feasibility criterion for acceptability in patients is supported if 25% of patients who are screened as lonely agree to participate in the trial.
The feasibility criteria for acceptability in social network members is supported if 50% of invited social network members accept participation and are assessed to have the prerequisites to be an informal caregiver.
The feasibility criteria for adherence in patients is supported if 75% adhere to the intervention, i.e., have contact with the informal caregiver once a week for a minimum of 8 out of 12 weeks.
The feasibility criteria for adherence in informal caregivers (social network member or peer) is supported if 75% participate in three out of four consultations. An overview of the feasibility criteria is presented in Table 3.
In feasibility and pilot testing, it is furthermore recommended that the resources used to complete the study is monitored [30]. This will be done by keeping a record of time resources used to include study participants and to complete the four nurse consultations (enrollment, 1 month, 3 and 6 months) and also frequency and time used on the additional questions from patients and informal caregivers to the open hotline.
Health behaviors and health outcomes
All outcomes will be measured in the intervention and control groups at baseline and 1, 3, 6, and 12 months. Demographic characteristics (age, gender) and treatment group (IHD, valve disease or arrhythmia) will be obtained from medical record.
Other outcomes will be obtained patient reported in REDCap. The primary outcome of interest, loneliness, is measured with HiRL tool [10]. The secondary outcome of interest is measured with the following questionnaires: Self-care: Self Care Self-Efficacy scale (Cronbach’s alpha 0.93) [40], health-related quality of life (HeartQoL) (Cronbach's alpha ≥ 0.80) [41], and Hospital Anxiety and Depression scale (HADS) [42] (in cardiac patients: Cronbach’s alpha 0.87 for HADS-A and 0.82 for HADS-D) [43]. Measures on health behaviors, i.e., smoking, alcohol consumption, weight, physical activity, and participation in cardiac rehabilitation, will be patient reported. An overview of outcome measurements and related measurement tools is presented in Fig. 2.
Data analysis
As recommended for the analysis of pilot studies [44], descriptive statistics will be presented as mean and standard deviations (SD) for continuous variables and frequencies and percentages for categorical variables at baseline and follow-ups (1, 3, 6, and 12 months).
To examine the comparability of the intervention group and the control group, baseline characteristics of the groups will be compared using Pearson’s chi-square or Fisher’s exact test for categorical variables and a t-test or Mann–Whitney test for continuous variables. Similar descriptive comparison of health outcome variables by group will be performed at follow-ups. The primary analyses will be performed according to the intention-to-treat principle.
To improve statistical efficiency, the primary outcome, i.e., loneliness, will be analyzed with a regression model adjusted for the stratification variables and the baseline variables, as recommended by the American Medical Association [45] and the European Medicines Agency [46].
Note, we do not aim to investigate statistically significant differences between groups as this is a feasibility trial. Therefore, no power calculation will be conducted. Rather, the measurement of health behaviors and health outcomes aims to give an indication of the potential variability in the outcome measures, which will be used to inform the power calculation for a future RCT.
A lost to follow-up analysis will be conducted for gender, age (higher or lower than mean), treatment procedure, and type of informal caregiver.
All statistical analyses will be performed using SAS Enterprise 7.1.
Discussion
A social support intervention targeting patients treated for cardiac disease who experience loneliness has the potential to decrease the negative impact on health from cardiovascular reactivity and to promote condition management in the early rehabilitation period. Consequently, a social support intervention may diminish the inequality in health behavior and health outcomes we see in patients who experience loneliness. To date, the type of support, with the intensity and the duration of the intervention needed to bring about changes in the experience of loneliness and the process that mediates health behavior and health outcomes, is scarce. The present study will contribute with new knowledge on how to implement a feasible social support intervention and, furthermore, investigate the preliminary evidence on the effect on health behaviors and health outcomes. The added knowledge will inform the design of a potential upcoming RCT.
Trial registration
The trial is registered on ClinicalTrials.gov (NCT05503810) 18.08.2022.
Positive, negative, and neutral results will be published in anonymized form.
Availability of data and materials
Data material can be requested upon reasonable request.
References
Khan MA, Hashim MJ, Mustafa H, Baniyas MY, Al Suwaidi S, AlKatheeri R, et al. Global epidemiology of ischemic heart disease: results from the global burden of disease study. Cureus. 2020;12(7):e9349 Available from: https://www.ncbi.nlm.nih.gov/pubmed/32742886.
Hjertetal.dk. https://hjerteforeningen.dk/alt-om-dit-hjerte/hjertetal/hjertetaldk/.
Pedersen M, Egerod I, Overgaard D, Baastrup M, Andersen I. Social inequality in phase II cardiac rehabilitation attendance: the impact of potential mediators. Eur J Cardiovasc Nurs. 2018;17(4):345–55 Available from: https://www.ncbi.nlm.nih.gov/pubmed/29185799.
Magrin ME, D’Addario M, Greco A, Miglioretti M, Sarini M, Scrignaro M, et al. Social support and adherence to treatment in hypertensive patients: a meta-analysis. Ann Behav Med. 2015;49(3):307–18 Available from: https://www.ncbi.nlm.nih.gov/pubmed/25341642.
Leifheit-Limson EC, Reid KJ, Kasl SV, Lin H, Jones PG, Buchanan DM, et al. The role of social support in health status and depressive symptoms after acute myocardial infarction: evidence for a stronger relationship among women. Circ Cardiovasc Qual Outcomes. 2010;3(2):143–50 Available from: https://www.ncbi.nlm.nih.gov/pubmed/20160162.
Murphy BM, Elliott PC, Le Grande MR, Higgins RO, Ernest CS, Goble AJ, et al. Living alone predicts 30-day hospital readmission after coronary artery bypass graft surgery. Eur J Cardiovasc Prev Rehabil. 2008;15(2):210–5 Available from: https://www.ncbi.nlm.nih.gov/pubmed/18391650.
Barth J, Schneider S, von Kanel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosom Med. 2010;72(3):229–38 Available from: https://www.ncbi.nlm.nih.gov/pubmed/20223926.
Welin C, Lappas G, Wilhelmsen L. Independent importance of psychosocial factors for prognosis after myocardial infarction. J Intern Med. 2000;247(6):629–39 Available from: https://www.ncbi.nlm.nih.gov/pubmed/10886484.
Christensen AV, Juel K, Ekholm O, Thrysoe L, Thorup CB, Borregaard B, et al. Significantly increased risk of all-cause mortality among cardiac patients feeling lonely. Heart. 2019; Available from: https://www.ncbi.nlm.nih.gov/pubmed/31685646.
Blakoe M, Christensen AV, Palm P, Højskov IE, Thrysoee L, Thorup CB, et al. Prognostic value of a brief loneliness questionnaire for patients with coronary heart disease: proposal for a prediction model. J Clin Nurs. 2022;31(11–12):1686–96 Available from: https://pubmed.ncbi.nlm.nih.gov/34473870/. Cited 2022 Dec 20.
Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–27 Available from: https://www.ncbi.nlm.nih.gov/pubmed/20652462.
Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29(4):377–87 Available from: https://www.ncbi.nlm.nih.gov/pubmed/16758315.
Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–57 Available from: https://www.ncbi.nlm.nih.gov/pubmed/3901065.
Mead H, Andres E, Ramos C, Siegel B, Regenstein M. Barriers to effective self-management in cardiac patients: the patient’s experience. Patient Educ Couns. 2010;79(1):69–76 Available from: https://www.ncbi.nlm.nih.gov/pubmed/19748205.
Blakoe M, Berg SK, Hojskov IE, Palm P, Bernild C. Who cares? Perception of loneliness in patients treated for coronary heart disease. Hvem bekymrer sig? Oplevelsen af ensomhed hos patienter med iskaemisk hjertesygdom. Glob Qual Nurs Res. 2022;9:23333936211073612 Available from: https://www.ncbi.nlm.nih.gov/pubmed/35083373.
Junehag L, Asplund K, Svedlund M. A qualitative study: perceptions of the psychosocial consequences and access to support after an acute myocardial infarction. Intensive Crit Care Nurs. 2014;30(1):22–30 Available from: https://www.ncbi.nlm.nih.gov/pubmed/23958430.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Back M, et al. ESC guidelines on cardiovascular disease prevention in clinical practice. Eur J Prev Cardiol. 2021; Available from: https://www.ncbi.nlm.nih.gov/pubmed/34558602.
Parry M, Watt-Watson J. Peer support intervention trials for individuals with heart disease: a systematic review. Eur J Cardiovasc Nurs. 2010;9(1):57–67 Available from: https://www.ncbi.nlm.nih.gov/pubmed/19926339.
Cohen S, Janicki-Deverts D. Can we improve our physical health by altering our social networks? Perspect Psychol Sci. 2009;4(4):375–8 Available from: https://www.ncbi.nlm.nih.gov/pubmed/20161087.
Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238–49.
Poscia A, Stojanovic J, La Milia DI, Duplaga M, Grysztar M, Moscato U, et al. Interventions targeting loneliness and social isolation among the older people: an update systematic review. Exp Gerontol. 2018;102:133–44 Available from: https://www.ncbi.nlm.nih.gov/pubmed/29199121.
Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Personal Soc Psychol Rev. 2011;15(3):219–66.
Clayton C, Motley C, Sakakibara B. Enhancing social support among people with cardiovascular disease: a systematic scoping review. Curr Cardiol Rep. 2019;21(10):123 Available from: https://www.ncbi.nlm.nih.gov/pubmed/31485908.
Blakoe M, Berg SK, Højskov IE, Palm P, Bernild C. One size does not fit all: a qualitative study exploring preferences and barriers towards the design of a loneliness reduction intervention in patients with coronary heart disease. Nurs Open. 2022;9(2):1114–25.
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50(5):587–92 Available from: https://www.ncbi.nlm.nih.gov/pubmed/23159157.
Bell ML, Whitehead AL, Julious SA. Guidance for using pilot studies to inform the design of intervention trials with continuous outcomes. Clin Epidemiol. 2018;10:153–7 Available from: https://www.ncbi.nlm.nih.gov/pubmed/29403314.
Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Chin J Evid Based Med. 2013;13(12):1501–7.
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016;2(1):1–32. https://doi.org/10.1186/s40814-016-0105-8.
Sundhedsstyrelsen. National klinisk retningslinje for hjerterehabilitering. 2015
Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10:1 Available from: https://www.ncbi.nlm.nih.gov/pubmed/20053272.
Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180–91.
Isaksen AS, Gjengedal E. Significance of fellow patients for patients with myocardial infarction. Scand J Caring Sci. 2006;20(4):403–11 Available from: https://www.ncbi.nlm.nih.gov/pubmed/17116149.
Vassilev I, Rogers A, Kennedy A, Koetsenruijter J. The influence of social networks on self-management support: a metasynthesis. BMC Public Health. 2014;14:719 Available from: https://www.ncbi.nlm.nih.gov/pubmed/25023948.
Head KJ, Noar SM, Iannarino NT, Grant HN. Efficacy of text messaging-based interventions for health promotion: a meta-analysis. Soc Sci Med. 2013;97:41–8 Available from: https://www.ncbi.nlm.nih.gov/pubmed/24161087.
Pietromonaco PR, Collins NL. Interpersonal mechanisms linking close relationships to health. Am Psychol. 2017;72(6):531–42 Available from: https://www.ncbi.nlm.nih.gov/pubmed/28880100.
Riegel B, Jaarsma T, Stromberg A. A middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci. 2012;35(3):194–204 Available from: https://www.ncbi.nlm.nih.gov/pubmed/22739426.
Reeves D, Blickem C, Vassilev I, Brooks H, Kennedy A, Richardson G, et al. The contribution of social networks to the health and self-management of patients with long-term conditions: a longitudinal study. PLoS One. 2014;9(6):e98340 Available from: https://www.ncbi.nlm.nih.gov/pubmed/24887107.
Craig P, Dieppe P, Macintyre S, Mitchie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337(7676):979–83. https://doi.org/10.1136/bmj.a1655.
Thabane L, Lancaster G. A guide to the reporting of protocols of pilot and feasibility trials. Pilot Feasibility Stud. 2019;5:37 Available from: https://www.ncbi.nlm.nih.gov/pubmed/30858987.
Yu DSF, De Maria M, Barbaranelli C, Vellone E, Matarese M, Ausili D, et al. Cross-cultural applicability of the Self-Care Self-Efficacy Scale in a multi-national study. J Adv Nurs. 2021;77(2):681–92.
Oldridge N, Hofer S, McGee H, Conroy R, Doyle F, Saner H. The HeartQoL: part II. Validation of a new core health-related quality of life questionnaire for patients with ischemic heart disease. Eur J Prev Cardiol. 2014;21(1):98–106 Available from: https://www.ncbi.nlm.nih.gov/pubmed/22822180.
Snaith RP, Zigmond AS. The hospital anxiety and depression scale. Br Med J (Clin Res Ed). 1986;292(6516):344 Available from: https://www.ncbi.nlm.nih.gov/pubmed/3080166.
Christensen AV, Dixon JK, Juel K, Ekholm O, Rasmussen TB, Borregaard B, et al. Psychometric properties of the Danish Hospital Anxiety and Depression Scale in patients with cardiac disease: results from the DenHeart survey. Health Qual Life Outcomes. 2020;18(1) Available from: https://pubmed.ncbi.nlm.nih.gov/31910859/. Cited 2022 Dec 27.
Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract. 2004;10(2):307–12 Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/j.2002.384.doc.x. Cited 2022 Dec 27.
Holmberg MJ, Andersen LW. Adjustment for baseline characteristics in randomized clinical trials. JAMA. 2022;328(21):2155–6 Available from: https://jamanetwork.com/journals/jama/fullarticle/2798955. Cited 2023 Jan 2.
European Medicines Agency. Guidelines on adjustment for baseline covariates in clinical trials. 2013. Accessed 6 Jan 2023.
The World Medical Association I. Declaration of Helsinki: ethical principles for medical research involving human subjects. October 2008. Korea: WMA Gen Assem Seoul; 2008.
Funding
The trial has been funded by Helsefonden (grant number 20-B-0064) and Snedkermester Sophus Jacobsen og hustru Astrid Jacobsens Fond and The Heart Centre Rigshospitalet.
Author information
Authors and Affiliations
Contributions
Study design: all authors (MB, AVC, PP, IEH, SKB) have contributed to the study design. Manuscript writing: MB has made the first draft of the manuscript. All authors (MB, AVC, PP, IEH, CB, SKB) have contributed and approved the manuscript in its final form.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The project has been approved by The Danish Data Protection Agency (P-2022-135) and the regional ethics committee (Journal-nr.:H-18057178). Informed consent will be obtained from each patient and informal caregiver. The study conforms to the Declaration of Helsinki [47].
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Blakø, M., Christensen, A.V., Højskov, I.E. et al. Protocol for a feasibility randomized trial of a social support intervention plus usual care versus usual care, targeting patients treated for cardiac disease who experience loneliness. Pilot Feasibility Stud 9, 22 (2023). https://doi.org/10.1186/s40814-023-01255-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-023-01255-9