Abstract
Background
To our knowledge, there is no intervention which includes personalised exercise therapy and self-management support for people with multimorbidity, although these interventions may be as effective as for people with single chronic conditions. Therefore, we developed a novel intervention, including personalised exercise therapy and self-management support for people with multimorbidity.
Methods
We followed the Medical Research Council framework and conducted one scoping review, five systematic reviews, two registry-based studies, one qualitative interview study and a mixed-methods feasibility study. Following an iterative approach, together with feedback from people with multimorbidity and relevant stakeholders, we developed the MOBILIZE intervention.
Results
The intervention included 24 (60 minutes) sessions of personalised exercise therapy and 24 (30 minutes) sessions of self-management support twice a week for 12 weeks, delivered in small groups by specifically trained physiotherapists. The intervention targets physiological, psychosocial, behavioural, and contextual factors to improve health-related quality of life and physical function in people living with multimorbidity.
Conclusions
We developed a personalised exercise therapy and self-management support programme for people with multimorbidity. The intervention will be tested for its safety and effectiveness in a randomised controlled trial.
Similar content being viewed by others
Key findings
-
We developed a novel intervention for people with multimorbidity through an iterative and comprehensive process following the Medical Research Council framework. This included several reviews, cohort studies and interviews with people with multimorbidity and several stakeholders.
-
The detailed reporting of the development of the intervention can serve as a model for future development papers to increase transparency and reduce research waste.
-
We focused on people with specific combinations of long-term chronic conditions (i.e., multimorbidity), therefore, this intervention is tailored for this population.
-
The intervention has been developed to be delivered in person, therefore, delivering this intervention using other delivery modalities (e.g., digitally) may require amendments.
Background
Living with two or more chronic conditions (i.e., multimorbidity) is common among people of all ages [1, 2]. Worldwide, approximately one-third of the population lives with one or more chronic conditions [3]. People living with multimorbidity have poorer physical and psychosocial health, a higher risk of hospitalisation and of dying prematurely [4,5,6,7]. The complexity of multimorbidity challenges the single-disease approach generally used by healthcare sectors, where patients use several healthcare services to manage each of their long-term conditions separately [8, 9], which is inefficient and burdensome for the patient [10]. Furthermore, available evidence for effective interventions of multimorbidity is limited [11]. A possible solution to deal with the complexity of managing multimorbidity is to focus on specific combinations of conditions, linked by common risk factors [12,13,14]. This approach may also help improve care and treatment effects for this population [11].
Osteoarthritis (of the knee or hip), type 2 diabetes, depression, heart disease (heart failure or ischemic heart disease), hypertension, and chronic obstructive pulmonary disease [15,16,17,18,19,20,21,22], are among the leading causes of global disability, affect hundreds of millions of people around the world [23], and often coexist linked via systemic inflammation and physical inactivity [24, 25]. Treatment guidelines, while encouraging clinicians to recommend a healthy lifestyle (including exercise therapy and self-management) for people with multimorbidity, focus on pharmacology [26]. However, to our knowledge, there is no intervention which includes personalised exercise therapy and self-management support for people with multimorbidity, although these interventions may be as effective as for people with single chronic conditions [27,28,29].
Therefore, the aim of this paper is to describe the development of a novel intervention (MOBILIZE) which includes personalised exercise therapy and self-management for people with multimorbidity.
Methods
The development of the MOBILIZE intervention is reported following the GUIDance for the rEporting of intervention Development (GUIDED) recommendations (S1 Table) [30]. We followed the newest version of the Medical Research Council Framework [31] to develop the intervention supplemented with crucial elements from the Bleijenberg et al. [32] and O'Cathain et al. guidance [33]. This was done to improve the likelihood of developing an intervention feasible to deliver and accepted by patients living with multimorbidity to ultimately enhance the fit with clinical practice [31,32,33]. Overall, the development of the intervention can be summarised in four phases: (I) “evidence synthesis and registry-based studies” where we summarised the available evidence regarding the effect of exercise therapy and self-management for people with multimorbidity and identified predictors of health outcomes in such interventions, (II) “qualitative analyses” where we explored the perspectives of patients living with multimorbidity, health care professionals, relatives, and patient advocates in relation to self-management with a particular focus on exercise behaviour, (III) theories and mechanism of action for developing the intervention, where we hypothesised the potential mechanisms of action and created a logic model, and finally (IV) mixed-methods feasibility testing of the developed intervention. The full results of the feasibility study are reported elsewhere [34].
Patient and Public Involvement
The development of the MOBILIZE intervention included feedback from several stakeholders, that is, people living with multimorbidity and their carers, patient advocates, physiotherapists and occupational therapists who are routinely working with patients with chronic conditions, a dietician, medical doctors specialised in the chronic conditions of interest, researchers with different backgrounds (physiotherapists, an exercise physiologist, and a health psychologist). All the stakeholders were informed about the different stages of the development and asked to provide feedback when deemed relevant. To determine how the body of evidence generated from the four phases of intervention development could be integrated into the intervention, the research team (AB, MJ, and STS) presented an initial program (based on the evidence gathered in phases (I) and (II)), to the physiotherapists (MD, HR, MN, JRP, GZ, and KHA), the patient advocates and carers, and medical doctors. The structure of the programme was discussed, including the exercises proposed, progression/regression levels, and self-management themes. This approach was also used throughout the development of the intervention, including during the feasibility study, and helped inform the final version of the intervention that is being tested in a randomised controlled trial (RCT) (https://clinicaltrials.gov/ct2/show/NCT04645732). This approach strengthens the internal and external validity, minimises research waste, and adds value to health care research [31,32,33]. The following sections describe the development process of the intervention and how the intervention was adapted after qualitative and quantitative data on the feasibility study were gathered.
Results
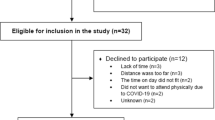
Overall, we performed one scoping review [35], five systematic reviews [27, 36,37,38,39,40], two registry-based studies [41, 42], one qualitative interview study [43], and a mixed-methods feasibility study [34], to identify knowledge gaps and develop an exercise therapy and self-management intervention for people with multimorbidity (Table 1) and Fig. 1.
Evidence synthesis
The reviews performed used the following Population, Intervention, Comparator and Outcome characteristics:
Population
Multimorbidity was defined as people reporting two or more of the following conditions: osteoarthritis (of the knee or hip), type 2 diabetes, depression, heart disease (heart failure or ischemic heart disease), hypertension, and chronic obstructive pulmonary disease. These conditions are linked by a common risk factor (physical inactivity) and pathogenesis (systemic low-grade inflammation), resulting in a cascade of reactions resulting in a ‘vicious cycle’ of chronic diseases and poor outcomes [44, 45]. For two systematic reviews, we included studies reporting at least 80% of the patients with multimorbidity (as defined above) [27, 40]. This pragmatic approach was pre-specified [37], and adopted to capture all the studies which included people with multimorbidity, given the expected inconsistency of reporting of the conditions across trials.
Interventions
Interventions that included exercise therapy and self-management support, either alone or in combination. We did not apply restrictions to the mode of delivery of the interventions (e.g., digitally, face-to-face) and setting (e.g., municipality/community, hospital).
Comparators
Usual care, for instance, advice from their health care provider.
Outcomes
The outcomes of interest included physical (e.g. endurance), psychosocial (e.g. health-related quality of life) and behavioural health (e.g. physical activity). The rationale for including these outcomes follows the guidance of a consensus study [14], which identified outcomes for multimorbidity intervention studies, and the patient partners of MOBILIZE.
Registry-based studies
Additionally, two registry-based studies were conducted to investigate the impact of comorbidities on health outcomes and to identify prognostic factors for health outcomes following an 8-week exercise and education programme in people with knee or hip osteoarthritis [41, 42]. How the results of these studies informed the development of the intervention are summarised in Table 1.
Qualitative analyses
A qualitative approach is particularly useful in capturing how people are affected by a problem and their perspectives on it [33]. Therefore, the qualitative study we conducted aimed to explore the perspectives of people living with multimorbidity, health care professionals, relatives, and patient advocates concerning self-management with a particular focus on exercise behaviour [43]. We conducted 17 interviews (nine focus groups; eight key informants) with 48 informants from four groups (22 people living with multimorbidity, 17 health care professionals, five relatives, and five patient advocates). The interviews were carried out online, informed consent was provided by the participants; the interviews were audio recorded and then transcribed verbatim. For the qualitative and feasibility study [34], patients and relatives were recruited by healthcare professionals from one psychiatric hospital and four hospital departments in Region Zealand (one of five health care regions in Denmark) or via self-referral on the basis of a poster and flyers placed in the hospitals’ waiting rooms or through posts on the hospitals’ and patient organizations’ Facebook pages [43]. The focus groups and interviews were audio-recorded, transcribed verbatim and analysed in an inductive-deductive process using Framework Analysis [46] and the Capability Opportunity and Motivation-Behaviour (COM-B) profile [47]. ,We found that people with multimorbidity identified several barriers related to exercise behaviour (i.e., pain, fatigue, breathlessness, lack of motivation, financial issues, accessibility, transportation, and decreased social support). Relatives' perspectives illustrated an uncertainty concerning their role in supporting self-management while simultaneously showing that they often take over responsibilities, which may represent a burden on their own wellbeing. Therefore, strategies for overcoming barriers to exercise and the participation of relatives in the self-management sessions, as part of usual care, were included in the programme (Table 2). Furthermore, patient advocates emphasised a need for more resources, such as establishing new collaborations and initiatives for people with multimorbidity and the lack of a 'burning platform' for multimorbidity (i.e., lack of urgency and prioritization of multimorbidity in the society) . Hence, this was included in the self-management session by informing the patients about activities, events, and organisations they could join (Table 2). Finally, health care professionals recognised these challenges while sharing their own challenges of empowering people with multimorbidity to change their behaviour given the limited resources. Therefore, this implied we instructed the physiotherapists delivering the intervention to prioritise strategies (i.e., behaviour change techniques) shown to be associated with better health outcomes in people with multimorbidity (Table 1) [38]. Overall, this knowledge, together with the self-management support framework [48], served to identify the core element of the 24 themes of the self-management sessions as well as the specific content of the sessions (Table 2). The core elements of the self-management sessions were proposed by the author team to the patients and physiotherapists delivering the intervention, and this format was deemed acceptable and feasible by them.
Mechanism of action and theory to inform the development of the intervention
In this section, we report the possible mechanisms of action of the MOBILIZE intervention, which are summarised in Fig. 2. Overall, we hypothesised that personalised exercise therapy and self-management support in addition to usual care (for instance, advice from their health care provider or any other treatment prescribed as standard care) will improve health-related quality of life more than usual care alone when measured at 12 months with concurrent positive effects on secondary outcomes. Furthermore, we hypothesised those improvements will occur immediately after the programme with concurrent positive effects on secondary outcomes and that the programme will be cost-effective at 12 months. We, therefore, aimed to develop an intervention that may potentially generate these effects Fig. 2. The knowledge gained from the four phases of intervention development guided us in identifying the core components of the exercise therapy and self-management intervention, as summarised in Table 1.
Anti-inflammatory and physiological factors
The anti-inflammatory effects of exercise therapy at cellular, tissue and organ level [44], as well as its positive physiological effects such as increase in muscle strength, improved blood pressure regulation and insulin sensitivity [49], highlight its potential role in improving health by reducing systemic inflammation.
Psychosocial factors
Providing education about long-term chronic conditions, providing psychological and social support to adjust to life with chronic conditions, encouraging adherence to multiple treatments, and supporting activities of daily living and physical functioning may improve psychosocial wellbeing [50, 51]. This can be achieved both through exercise therapy amd self-management sessions and as result of the psychological and social benefits associated with participation in group-based activities [51].
Contextual factors and expectations
Contextual factors, including the setting of the intervention [52], facilitator, patient and treatment features, as well as the patient-facilitator relationship [53], can influence health outcomes positively or negatively. Therefore, much attention is given to ensuring such factors are addressed when delivering the intervention. The complete list of contextual factors and how they are considered in the MOBILIZE intervention can be found in the S3 Table. Furthermore, expectations are a large determinant of the placebo and nocebo effect [54]. A feasible strategy to increase patients’ realistic expectations is making sure the patients are aware of the health benefits of exercise therapy and self-management. We have therefore instructed the facilitators delivering the intervention to use strategies to set realistic expectations [54]. For instance, via adapting an authentic and empathic communication style when communicating and via educating patients on how to cope with possible adverse effects (e.g. muscle pain, fatigue, and shortness of breath), regularly assess and address patients’ anxieties, concerns, and treatment expectations, and provide adequate information regarding diseases, diagnoses, and treatments [54]. Taken together, the contextual factors and expectations offer an opportunity to integrate strategies which may stimulate placebo effects and prevent nocebo effects [53].
Behavioural factors
Engaging in a healthier lifestyle is associated with up to 6.3 years longer life expectancy for men and 7.6 years for women highlighting the role of a healthy lifestyle as a contributing factor to health [55]. Therefore, we included various Behaviour Change Techniques (BCTs) [56] in the intervention (Table 3). BCTs are defined as observable, replicable, and irreducible components of an intervention designed to alter or redirect causal processes that regulate behaviour. The rationale for using specific BCTs is based on the evidence synthesis results focusing on people with multimorbidity (Table 1) and previous literature investigating this topic given the low-certainty of the evidence for the association between BCTs and people with multimorbidity. For example, BCTs such as ‘Action planning’, ‘Self-monitoring’ and ‘Goal setting’ [56], are strongly associated with improved health behaviours in people without chronic conditions [57], and in people with one condition [55, 58,59,60].
In line with the BCT taxonomy instructions, we have only included the ‘active ingredients of the intervention’. That is, the observable, replicable components aimed at changing a behaviour.
Personalisation of the MOBILIZE intervention
Prescribing the right treatment at the right time to the right patient is key to eliciting benefits and minimising harms. The exercise therapy and self-management content of the intervention has been developed to be personalised. The personalisation of the programme is set during a one-to-one session prior to initiating the programme, lasting 60 minutes between each patient and a physiotherapist. The one-to-one session includes the following phases: (I) Presentation of the exercise therapy programme to the patient and selection of the appropriate starting exercise levels, (II) Presentation of the criteria for progression or regression of the exercises (e.g., the OMNI scale [61], and the Borg scale [62], and how sets and repetitions are progressed are presented so that the patient can indicate the degree of exertion of the exercises) and instructions on how to fill in the intervention diary to record the exertion of the exercises, (III) setting of a Specific, Measurable, Attainable, Relevant, and Timely (SMART) goal (e.g., being able to walk the stairs without discomfort).
Preference and the content of the MOBILIZE intervention
Adherence to treatment is key to its effectiveness [63]. For people with multimorbidity, this is particularly challenging due to the high treatment burden they experience [64]. Having the option to receive treatments based on patient preferences may improve adherence to the treatment and ultimately improve health [65]. Therefore, the MOBILIZE intervention allows patients to choose the type of exercise therapy (aerobic training, strength training, or functional exercises) to perform (Table 4). This decision was supported by the fact that people with multimorbidity seem to benefit from exercise therapy interventions regardless of the type of exercise therapy [27], in line with the WHO guidelines for physical activity for general health [66].
Safety concerns
Behavioural interventions, including exercise therapy, are safe [68]. Although, in general, the risk of non-serious adverse events (according to the FDA definition [69], including short-lasting muscle pain and fatigue) may increase (19%), they do not increase the risk of serious adverse events such as hospitalisation and death [68]. Indeed, in people with multimorbidity they seem to reduce the risk of any serious adverse events by 38% [37]. However, the certainty of these findings in people with multimorbidity is low, mainly due to too few studies investigating this and the heterogeneous reporting of adverse events. Therefore, when developing the intervention, we tried to identify the possible adverse events associated with exercise therapy by looking at systematic reviews of exercise therapy for single chronic conditions [15, 18,19,20, 22, 29, 49, 68], national clinical guidelines [70], and by regular meetings with medical doctors specialised in the single chronic conditions. Overall, in people with one or more stable medical chronic conditions, it is contraindicated to exercise if they experience chest pain, uncontrolled hypertension or diabetes, irregular heartbeat, dizziness or sudden vision change [49]. We have instructed the facilitators delivering the intervention to check these contraindications before initiating any new exercise therapy session.
The prototype of the intervention and amendments
Based on the evidence gathered and feedback from relevant stakeholders (listed in the patient and public involvement paragraph), we developed an intervention consisting of 18 (60 minutes) sessions of personalised, group-based supervised exercise therapy, six sessions of 90 minutes of group-based self-management support and six sessions of home-based unsupervised exercise therapy. The programme was designed to be delivered twice a week for 12 weeks and was tested in a mixed-methods feasibility study [34]. Briefly, the feasibility study showed the intervention was feasible and acceptable in people with multimorbidity in terms of recruitment rate, retention of outcomes at follow-up, outcome burden, adverse events, and qualitative feedback. Adherence to the home-based unsupervised exercise therapy, however, was low and a few barriers were identified in the interviews suggesting that some amendments were needed before proceeding to the RCT. For example, home-based exercise sessions were deemed challenging to complete by the patients, given the lack of supervision. Additionally, we discussed the option of splitting the self-management sessions into shorter but more frequent sessions to facilitate the uptake of the delivered information. Therefore, together with the physiotherapists, patient partners, project managers, and researchers of the MOBILIZE team, we amended the intervention by increasing the number of the group-based supervised exercise therapy sessions to 24 and the number of the group-based self-management sessions to 24.
Overall, each session of the intervention, which will be tested in a randomised controlled trial, lasts 90 minutes and includes 30 minutes of self-management support followed by 60 minutes of supervised group-based exercise therapy delivered by a physiotherapist. The material will be made publicly available in the randomised controlled trial paper. The overall content of the intervention is presented in Table 4 following the Template for the TIDieR (Template for Intervention Description and Replication) [71], incorporating the CERT (Consensus on Exercise Reporting Template) items [67], and S2 Table, including the mechano-biological descriptors of strengthening exercise therapy proposed by Toigo & Boutellier [72].
Discussion
This paper summarises the development of the MOBILIZE intervention, which includes personalised exercise therapy and self-management support for people with multimorbidity. We followed the newest version Medical Research Council framework to develop the intervention [31], which targets people with multimorbidity and can be delivered in different settings at a relatively low cost as it uses material available in most gyms of hospitals, municipalities, and private physiotherapy clinics.
The evidence-based approach used to develop the MOBILIZE intervention together with the input from relevant stakeholders, resulted in an intervention for people with multimorbidity which includes components aimed to elicit physiological, psychosocial, and behavioural effects, considering contextual factors ultimately leading to improved health. This is novel for people with multimorbidity who are usually treated pharmacologically [26].
The iterative process used to develop and feasibility test the intervention helped us identify several challenges that could be addressed before the randomised controlled trial tests the effectiveness of the intervention. This is a key step in reducing waste in research [73].
The continuous interaction with key stakeholders to develop the MOBILZIE intervention in addition to improving the design of the intervention, aims to facilitate its implementation in clinical practice. While this approach has been acknowledged to be time-consuming, it is required when developing complex interventions aiming at improving people’s health behaviours [74].
Limitations
The limited quality of evidence (few studies with inconsistent results) supporting the use of exercise therapy and self-management in people with multimorbidity meant that many decisions taken regarding the type, duration, and intensity of the intervention were taken from evidence of research for people with single chronic conditions. However, the extensive qualitative work conducted as part of the development of the intervention and the constant feedback from the stakeholders helped to adapt this knowledge to people with multimorbidity. This will also improve the translation of our research into clinical practice if the MOBILIZE intervention is shown to be superior to usual care in the randomised controlled trial.
Conclusions
In this paper, we detail the development of a novel intervention for people with multimorbidity. The MOBILIZE intervention, is currently being tested for its safety and effectiveness in a randomised controlled trial. The intervention includes personalised exercise therapy and self-management support to improve health-related quality of life and physical function by eliciting physiological, psychosocial, contextual, and behavioural factors. The development of the MOBILIZE intervention has highlighted the importance of using an iterative process supported by the involvement of several stakeholders to identify solutions to the challenges of developing complex interventions.
Availability of data and materials
The data reported in this paper are available on the Open Science Framework page of the MOBILIZE project https://osf.io/qk6yg/.
Change history
30 December 2022
Additional file 2 was missing in the publised article. The article has been updated to rectify the errors.
Abbreviations
- GUIDED:
-
GUIDance for the rEporting of intervention Development
- MRC:
-
Medical Research Council Framework
- BCt:
-
Behaviour Change Techniques
- OSF:
-
Open Science Framework
References
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43.
Skou ST, Mair FS, Fortin M, Guthrie B, Nunes BP, Miranda JJ, Boyd CM, Pati S, Mtenga S, Smith SM. Multimorbidity. Nat Rev Dis. Primers. 2022;8(1):48. https://doi.org/10.1038/s41572-022-00376-4.
Nguyen H, Manolova G, Daskalopoulou C, Vitoratou S, Prince M, Prina AM. Prevalence of multimorbidity in community settings: A systematic review and meta-analysis of observational studies. J Comorb. 2019;9:2235042X19870934.
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–9.
Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22(Suppl 3):391–5.
Fortin M, Lapointe L, Hudon C, Vanasse A, Ntetu AL, Maltais D. Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes. 2004;2:51.
Condelius A, Edberg AK, Jakobsson U, Hallberg IR. Hospital admissions among people 65+ related to multimorbidity, municipal and outpatient care. Arch Gerontol Geriatr. 2008;46(1):41–55.
Wallace E, Salisbury C, Guthrie B, Lewis C, Fahey T, Smith SM. Managing patients with multimorbidity in primary care. BMJ. 2015;350:h176.
Smith SM, Soubhi H, Fortin M, Hudon C, O'Dowd T. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ. 2012;345:e5205.
Gallacher KMC, Montori VM, Mair FS. Understanding patients’ experiences of treatment burden in chronic heart failure using normalization process theory. Ann Fam Med. 2011;9:235–43.
Smith SM, Wallace E, O'Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Db Syst Rev. 2021;1.
Smith SM, Bayliss EA, Mercer SW, Gunn J, Vestergaard M, Wyke S, et al. How to design and evaluate interventions to improve outcomes for patients with multimorbidity. J Comorb. 2013;3:10–7.
Smith SM, Wallace E, O'Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Db Syst Rev. 2016;3.
Smith SM, Wallace E, Salisbury C, Sasseville M, Bayliss E, Fortin M. A Core Outcome Set for Multimorbidity Research (COSmm). Ann Fam Med. 2018;16(2):132–8.
Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, et al. Exercise for depression. Cochrane Db Syst Rev. 2013;9.
Puhan MA, Gimeno-Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Db Syst Rev. 2016;12.
Lee LL, Mulvaney CA, Wong YK, Chan ESY, Watson MC, Lin HH. Walking for hypertension. Cochrane Db Syst Rev. 2021;2.
Long L, Mordi IR, Bridges C, Sagar VA, Davies EJ, Coats AJS, et al. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Db Syst Rev. 2019;1.
Dibben G, Faulkner J, Oldridge N, Rees K, Thompson DR, Zwisler AD, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Db Syst Rev. 2021;11.
Thomas D, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Db Syst Rev. 2006;3.
Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheum. 2014;66(3):622–36.
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Db Syst Rev. 2015;1.
Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Vetrano DL, Roso-Llorach A, Fernandez S, Guisado-Clavero M, Violan C, Onder G, et al. Twelve-year clinical trajectories of multimorbidity in a population of older adults. Nat Commun. 2020;11(1):3223.
Skou ST, Pedersen BK, Abbott JH, Patterson B, Barton C. Physical Activity and Exercise Therapy Benefit More Than Just Symptoms and Impairments in People With Hip and Knee Osteoarthritis. J Orthop Sports Phys Ther. 2018;48(6):439–47.
Muth C, Blom JW, Smith SM, Johnell K, Gonzalez-Gonzalez AI, Nguyen TS, et al. Evidence supporting the best clinical management of patients with multimorbidity and polypharmacy: a systematic guideline review and expert consensus. J Intern Med. 2019;285(3):272–88.
Bricca A, Harris LK, Jager M, Smith SM, Juhl CB, Skou ST. Benefits and harms of exercise therapy in people with multimorbidity: A systematic review and meta-analysis of randomised controlled trials. Ageing Res Rev. 2020;63:101166.
de Souto BP. Exercise for Multimorbid Patients in Primary Care: One Prescription for All? Sports Med. 2017;47(11):2143–53.
Dekker J, Buurman BM, van der Leeden M. Exercise in people with comorbidity or multimorbidity. Health Psychol. 2019;38(9):822–30.
Duncan E, O'Cathain A, Rousseau N, Croot L, Sworn K, Turner KM, et al. Guidance for reporting intervention development studies in health research (GUIDED): an evidence-based consensus study. BMJ Open. 2020;10(4):e033516.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374:n2061.
Bleijenberg N, de Man-van Ginkel JM, Trappenburg JCA, Ettema RGA, Sino CG, Heim N, et al. Increasing value and reducing waste by optimizing the development of complex interventions: Enriching the development phase of the Medical Research Council (MRC) Framework. Int J Nurs Stud. 2018;79:86–93.
O'Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9(8):e029954.
Skou STBR, Nyberg M, Dideriksen M, Bodtger U, *Bricca A, *Jäger M. *shared senior authorship. Personalised exercise therapy and self-management support for people with multimorbidity: Feasibility of the MOBILIZE intervention. Pilot and Feasability Studies. (Submitted). 2022.
Jäger MZG, Bricca A, Dideriksen M, Smith S, Midtgaard J, Taylor R, et al. Mapping interventional components and behaviour change techniques used to promote self-management in people with multimorbidity: a scoping review. Under. Review. 2022.
Bricca A, Harris LK, Jager M, Smith S, Juhl CB, Skou ST, et al. Benefits and harms of exercise therapy in people with multimorbidity. Br J Sports Med. 2021;55(18):1059–60.
Bricca A, Harris LK, Saracutu M, Smith SM, Juhl CB, Skou ST. The benefits and harms of therapeutic exercise on physical and psychosocial outcomes in people with multimorbidity: Protocol for a systematic review. J Comorb. 2020;10:2235042X20920458.
Bricca A, Jager M, Johnston M, Zangger G, Harris LK, Midtgaard J, et al. Effect of In-Person Delivered Behavioural Interventions in People with Multimorbidity: Systematic Review and Meta-analysis. Int J Behav Med. 2022. https://doi.org/10.1007/s12529-022-10092-8.
Bricca A, Pellegrini A, Zangger G, Ahler J, Jäger M, Skou ST. The Quality of Health Apps and Their Potential to Promote Behavior Change in Patients With a Chronic Condition or Multimorbidity: Systematic Search in App Store and Google Play. JMIR Mhealth Uhealth. 2022;10(2):e33168.
Harris LK, Skou ST, Juhl CB, Jager M, Bricca A. Recruitment and retention rates in randomised controlled trials of exercise therapy in people with multimorbidity: a systematic review and meta-analysis. Trials. 2021;22(1):396.
Pihl K, Roos EM, Taylor RS, Gronne DT, Skou ST. Prognostic factors for health outcomes after exercise therapy and education in people with knee and hip osteoarthritis with or without comorbidities: a study of 37,576 patients treated in primary care. Arthritis Care Res. 2021;74(11):1866–78.
Pihl K, Roos EM, Taylor RS, Grønne DT, Skou ST. Associations between comorbidities and immediate and one-year outcomes following supervised exercise therapy and patient education - A cohort study of 24,513 individuals with knee or hip osteoarthritis. Osteoarthr Cartil. 2021;29(1):39–49. https://doi.org/10.1177/26335565221100172
Jäger MLM, Pedersen JR, Dideriksen M, Nyberg M, Bricca A, Bodtger U, et al. Putting the pieces together: A qualitative study exploring perspectives on self-management and exercise behavior among people living with multimorbidity, healthcare professionals, relatives, and patient advocates. J Multimorb Comorb (Accepted). 2022.
Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11(9):607–15.
Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25(Suppl 3):1–72.
Onwuegbuzie AJ, Dickinson WB, Leech NL, Zoran AG. A Qualitative Framework for Collecting and Analyzing Data in Focus Group Research. Int J Qual Methods. 2009;8(3):1–21.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–75.
Reid H, Ridout AJ, Tomaz SA, Kelly P, Jones N. Physical Activity Risk Consensus g. Benefits outweigh the risks: a consensus statement on the risks of physical activity for people living with long-term conditions. Br J Sports Med. 2022;56(8):427–38.
Allegrante JP, Wells MT, Peterson JC. Interventions to Support Behavioral Self-Management of Chronic Diseases. Annu Rev Public Health. 2019;40:127–46.
Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for adults: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act. 2013;10:135.
Sandal LF, Thorlund JB, Moore AJ, Ulrich RS, Dieppe PA, Roos EM. Room for improvement: a randomised controlled trial with nested qualitative interviews on space, place and treatment delivery. Br J Sports Med. 2019;53(6):359–67.
Rossettini G, Carlino E, Testa M. Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain. BMC Musculoskelet Disord. 2018;19(1):27.
Bingel U. Placebo 2.0: the impact of expectations on analgesic treatment outcome. PAIN. 2020;161.
Chudasama YV, Khunti K, Gillies CL, Dhalwani NN, Davies MJ, Yates T, et al. Healthy lifestyle and life expectancy in people with multimorbidity in the UK Biobank: A longitudinal cohort study. PLoS Med. 2020;17(9):e1003332.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701.
Goodwin L, Ostuzzi G, Khan N, Hotopf MH, Moss-Morris R. Can We Identify the Active Ingredients of Behaviour Change Interventions for Coronary Heart Disease Patients? A Systematic Review and Meta-Analysis. PLoS One. 2016;11(4):e0153271.
Van Rhoon L, Byrne M, Morrissey E, Murphy J, McSharry J. A systematic review of the behaviour change techniques and digital features in technology-driven type 2 diabetes prevention interventions. Digit Health. 2020;6:2055207620914427.
Willett M, Duda J, Fenton S, Gautrey C, Greig C, Rushton A. Effectiveness of behaviour change techniques in physiotherapy interventions to promote physical activity adherence in lower limb osteoarthritis patients: A systematic review. PLoS One. 2019;14(7):e0219482.
Robertson RJ, Goss FL, Rutkowski J, Lenz B, Dixon C, Timmer J, et al. Concurrent validation of the OMNI perceived exertion scale for resistance exercise. Med Sci Sports Exerc. 2003;35(2):333–41.
Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990;16(Suppl 1):55–8.
Horwitz RI, Horwitz SM. Adherence to Treatment and Health Outcomes. Arch Intern Med. 1993;153(16):1863–8.
Kim S, Bennett K, Wallace E, Fahey T, Cahir C. Measuring medication adherence in older community-dwelling patients with multimorbidity. Eur J Clin Pharmacol. 2018;74(3):357–64.
Umar N, Litaker D, Schaarschmidt M-L, Peitsch WK, Schmieder A, Terris DD. Outcomes associated with matching patients' treatment preferences to physicians' recommendations: study methodology. BMC Health Serv Res. 2012;12(1):1.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62.
Slade SC, Dionne CE, Underwood M, Buchbinder R, Beck B, Bennell K, et al. Consensus on Exercise Reporting Template (CERT): Modified Delphi Study. Phys Ther. 2016;96(10):1514–24.
Niemeijer A, Lund H, Stafne SN, Ipsen T, Goldschmidt CL, Jørgensen CT, et al. Adverse events of exercise therapy in randomised controlled trials: a systematic review and meta-analysis. Br J Sports Med. 2020;54(18):1073–80.
Administration. USFD. What is a Serious Adverse Event? Silver Spring, MD2014 [Available from: http://www.fda.gov/Safety/MedWatch/HowToReport/ucm053087.htm accessed 21 Apr 2022.
Pelliccia A, Sharma S, Gati S, Back M, Borjesson M, Caselli S, et al. 2020 ESC Guidelines on Sports Cardiology and Exercise in Patients with Cardiovascular Disease. Rev Esp Cardiol (Engl Ed). 2021;74(6):545.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
Toigo M, Boutellier U. New fundamental resistance exercise determinants of molecular and cellular muscle adaptations. Eur J Appl Physiol. 2006;97(6):643–63.
Glasziou P, Chalmers I. Research waste is still a scandal—an essay by Paul Glasziou and Iain Chalmers. BMJ. 2018;363:k4645.
Eaton S, Roberts S, Turner B. Delivering person centred care in long term conditions. BMJ. 2015;350:h181.
Acknowledgements
We would like to thank Gregers Aagaard and Margit Dybkjær, two people living with long-term chronic conditions, and Tue Dybkjær, a partner of a person with multimorbidity for their feedback on the development of MOBILIZE. We would also like to thank the recruitment centres, clinicians, and people with multimorbidity involved in the study conduct. Finally, we owe gratitude to the MOBILIZE scientific advisory board of Prof. Susan Smith, Prof. Sallie Lamb, Prof. Alan Silman, Prof. Bente Klarlund Pedersen, Prof. Ewa M. Roos, and Prof. Rod Taylor.
Funding
The present study was supported by the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation program (MOBILIZE; grant agreement No 801790), a research program grant from Region Zealand (Exercise First; grant award N/A), Næstved, Slagelse and Ringsted Hospitals’ Research Fund, The Danish Regions and The Danish Health Confederation through the Development and Research Fund (project no. 2703), and The Association of Danish Physiotherapists Research Fund (grant award N/A). Furthermore, STS is the recipient of an ongoing, unrelated grant from the European Union’s Horizon 2020 research and innovation programme (ESCAPE; grant agreement No 945377).
Author information
Authors and Affiliations
Contributions
Study conception and design: Bricca, Jäger, Rasmussen, Nyberg, Dideriksen, Pedersen, Zangger, Andreasson, Skou. Acquisition of data: Bricca, Jäger, Rasmussen, Nyberg, Dideriksen, Pedersen, Zangger, Andreasson, Skou. Analysis and interpretation of data: Bricca, Jäger, Rasmussen, Nyberg, Dideriksen, Pedersen, Zangger, Andreasson, Skou. Drafting the article or revising it critically for important intellectual content: Bricca, Jäger, Rasmussen, Nyberg, Dideriksen, Pedersen, Zangger, Andreasson, Skou. Final approval of the article: Bricca, Jäger, Rasmussen, Nyberg, Dideriksen, Pedersen, Zangger, Andreasson, Skou
Corresponding author
Ethics declarations
Ethics approval and consent to praticipate
This study reports an overview of the studies (already published) that were conducted to develop an intervention including personalised exercise therapy and self-management support. Therefore an Ethical approval is not required. Feasibility study was approved by the Ethics committee of Region Zealand (SJ-857).
Consent for publication
Not applicable
Competing interests
STS is associate editor of the Journal of Orthopaedic & Sports Physical Therapy and has received personal fees from Munksgaard and TrustMe-Ed, all of which are outside the submitted work. He is co-founder of Good Life with Osteoarthritis in Denmark (GLA:D®), a not-for profit initiative hosted at University of Southern Denmark aiming at implementing clinical guidelines for patients with osteoarthritis in clinical practice, no other relationships or activities that could appear to have influenced the submitted work. The funders were not involved in any aspect of the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bricca, A., Jäger, M., Dideriksen, M. et al. Personalised exercise therapy and self-management support for people with multimorbidity: Development of the MOBILIZE intervention. Pilot Feasibility Stud 8, 244 (2022). https://doi.org/10.1186/s40814-022-01204-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-022-01204-y