Abstract
Background
Studies have demonstrated that exercise can mitigate the intensity of menstrual pain in primary dysmenorrhea, but the most effective type of exercise remains unclear. The objective of this systematic review and network meta-analysis was to evaluate the effectiveness of different exercise regimens in reducing pain associated with primary dysmenorrhoea.
Methods
Randomized controlled trials investigating the relationship between menstrual pain and exercise were selected from major electronic databases until February 2, 2024. The primary outcome was the effect of exercise on pain intensity measured by the mean difference on a 10-cm visual analogue scale at 4 and 8 weeks after intervention. The secondary outcome was the difference in risk of dropout at 8 weeks. The study protocol was registered as INPLASY202330050.
Results
This systematic review and network meta-analysis included 29 randomized controlled trials, which involved 1808 participants with primary dysmenorrhea. Exercise interventions included relaxation exercise, strength training, aerobic activity, yoga, mixed exercise, and the Kegel maneuver. Relaxation exercise was the most effective in reducing menstrual pain in 4 weeks (− 3.56; 95% confidence interval: − 5.03 to − 2.08). All exercise interventions were effective in reducing menstrual pain at 8 weeks, with reductions ranging from − 3.87 (95% CI − 5.51 to − 2.22) for relaxation exercise to − 2.75 (95% CI − 4.00 to − 1.51) for yoga, compared to the control group. Relaxation exercises were found to have a significantly lower dropout risk (− 0.11; 95% CI − 0.20 to 0.02), while none of the exercise types was associated with a higher dropout risk than the control group.
Conclusion
All exercise interventions were effective in reducing menstrual pain in primary dysmenorrhea after 8 weeks of intervention. However, relaxation exercise was found to be the most effective intervention at 4 and 8 weeks and had the lowest risk of dropout.
Graphical Abstract

Plain Language Summary
This analysis aimed to see how effective different types of exercise are in reducing pain in women with primary dysmenorrhea. The researchers looked at 29 studies involving 1808 participants and evaluated six different types of exercise. The main outcome was the effect of pain reduction after 4 and 8 weeks of exercise. The researchers found that all types of exercise were effective in reducing menstrual pain after 8 weeks, with relaxation exercises being the most effective at both 4 and 8 weeks. None of the exercise types were associated with higher dropout risks than the control group, and relaxation exercise had a lower dropout risk than the other types of exercise.
Key Points
-
1.
Exercise can be an effective way to reduce menstrual pain in women with primary dysmenorrhea.
-
2.
Different types of exercise, including relaxation exercise, strength training, aerobic activity, yoga, mixed exercise, and the Kegel maneuver, have been found to be effective in reducing menstrual pain after 8 weeks.
-
3.
Relaxation exercises, such as progressive muscle relaxation and self-administered massage, have been found to be the most effective interventions for reducing menstrual pain at both 4 and 8 weeks, and they also have a lower risk of dropout.
Similar content being viewed by others
Introduction
Primary dysmenorrhea, prevalent among women of reproductive age, manifests as menstrual pain and discomfort localized in the lower abdomen. Globally, this condition afflicts a substantial proportion of women, with reported prevalence rates varying from 17 to 90% [1]. Notably, primary dysmenorrhea exerts a considerable impact on the quality of life, often resulting in absenteeism from occupational or educational settings, diminished productivity, and escalated healthcare demands. In the United States alone, the economic burden attributed to this condition is estimated at approximately 600 million working hours lost per year, equating to a financial loss of around US$2 billion annually [2].
Primary dysmenorrhea is postulated to arise from the synthesis of prostaglandins [1, 3] during menstruation, which precipitates potent uterine contractions, diminished uterine blood flow, and subsequent activation of nociceptors. While non-steroidal anti-inflammatory drugs represent the principal therapeutic approach for this condition [1, 3], their efficacy in providing comprehensive relief is not universal, and prolonged usage is associated with potential adverse effects. Consequently, there is an increasing interest in non-pharmacological modalities, such as physical exercise, as potential adjunctive treatments for primary dysmenorrhea.
Owing to the potential of exercise to augment endorphin secretion [4] and attenuate inflammation [5], a multitude of studies have scrutinized its efficacy in the management of primary dysmenorrhea [6,7,8,9,10,11,12]. Despite this extensive investigation, the scholarly discourse remains divided regarding the most effective form of exercise [13, 14]. Various modalities have been examined, encompassing relaxation exercises such as progressive muscle relaxation [12, 15] and self-administered massage [16, 17], alongside strength training [18], aerobic exercises [19], yoga [20], mixed exercise regimes [21], and the Kegel maneuver [22]. Certain studies have documented substantial alleviation in pain following only a 4-week period of exercise intervention [15], whereas others indicate a necessity for up to 8 weeks to discern any tangible benefits [11]. Furthermore, the incidence of participant withdrawal has exhibited variability across these diverse exercise protocols [12, 23].
In contrast to randomized controlled trials and conventional pairwise meta-analyses [24, 25], a meticulously conducted network meta-analysis offers expanded insights into the comparative efficacy and acceptability of various treatments for a specified clinical condition [26]. Moreover, this type of analysis is capable of evaluating the potential superiority of individual interventions in achieving specific outcomes. Such information is pivotal for the formulation of evidence-based clinical guidelines and plays a critical role in informing the design and focus of future clinical research [27, 28].
The objective of this network meta-analysis was to systematically rank and compare the mean differences in pain reduction and the differences in risk of dropout associated with diverse exercise interventions in patients with primary dysmenorrhea. The collation and analysis of these data are intended to furnish more precise and tailored recommendations for individuals contemplating exercise as a strategy for pain management in the context of primary dysmenorrhea.
Methods
This study was conducted adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for network meta-analysis (PRISMA NMA) guidelines [29] (Additional file 1: Table S1). Registration of the study was completed with INPLASY, bearing the registration number INPLASY202330050 [30]. Given the nature of this research, the requirement for ethics review board approval and participant informed consent was deemed unnecessary.
Database Searches and Study Identification
The literature search for this systematic review and network meta-analysis was independently conducted by two authors (Tsai IC and Lei WT). They utilized electronic databases including PubMed, Cochrane Reviews, Cochrane CENTRAL, Web of Science, and ClinicalTrials.gov. The search was structured around a series of keywords: (‘primary dysmenorrhea’ OR ‘dysmenorrhea’ OR ‘menstrual cramps’ OR ‘painful periods’) AND (‘exercise’ OR ‘yoga’ OR ‘aerobic’ OR ‘training’ OR ‘sports’ OR ‘physical activity’ OR ‘workout’ OR ‘fitness’ OR ‘training’) AND (‘randomized’ OR ‘randomised’ OR ‘random’). This search strategy, detailed in Additional file 1: Table S2 of the Supplementary Material, encompassed records from the inception of each database until the final search date of February 2, 2024.
During the preliminary phase of this research, two authors were assigned the responsibility of assessing the relevance of the titles and abstracts of studies identified in the search, employing a consensus-based approach for determining their eligibility. This evaluation was performed using the previously mentioned databases to meticulously review potential trials. In addition to electronic searches, the reference lists of several review articles [13, 14, 31,32,33,34,35,36] were also meticulously perused, and manual searches were conducted to ensure comprehensive coverage. In instances where the initial two reviewers encountered difficulties in achieving a consensus, a third reviewer and co-author of the study (Chang KV) was engaged for arbitration. It is noteworthy that this search process did not impose any language restrictions.
Inclusion and Exclusion Criteria
The network meta-analysis adopted the PICO framework (population, intervention, comparison, outcome) with the following specifications: (1) P: female human participants with primary dysmenorrhea; (2) I: exercise interventions; (3) C: control group without intervention; and (4) O: changes in pain intensity. The diagnosis of primary dysmenorrhea can be established through adherence to the criteria prescribed by the American College of Obstetricians and Gynecologists, as per their recommended guidelines [37].
The study employed the following inclusion criteria: (1) randomized controlled trials that recruited female human participants with primary dysmenorrhea, (2) randomized controlled trials that investigated the quantitative assessment of pain intensity pre- and post-exercise, (3) the control group received no intervention or regular care, and (4) trials that had available data on pain intensity assessment pre- and post-intervention at either 4 weeks or 8 weeks [12, 20, 21, 38].
The selection of the 4-week and 8-week evaluation time points was based on an early stage exploratory literature review. This review revealed that these durations were the most frequently utilized assessment intervals in relevant studies [10,11,12, 16, 18, 20,21,22,23, 38,39,40], typically aligning with the completion of the first or second menstrual cycle post-intervention. By examining outcomes at these two distinct intervals, our analysis aimed to elucidate the requisite duration of each exercise intervention necessary to exert a significant impact on the pain intensity associated with primary dysmenorrhea.
Exclusion criteria for this review and network meta-analysis included: (1) non-randomized controlled trials, (2) studies without comparisons of exercise vs. exercise or exercise vs. regular care comparison, (3) studies lacking quantitative assessments of pain intensity, (4) pain intensity assessment methods that could not be linearly converted to a 10 cm visual analogue scale (VAS), since the VAS is the most convenient method for quantifying pain intensity [41] and is widely used in studies related to primary dysmenorrhea [23, 39, 42], (5) studies that did not separately evaluate pain intensity, but were included this with other attributes such as distress or duration, (6) studies with incomplete or unavailable data, even after attempts to contact the authors via email, and (7) studies enrolling participants that overlapped with a published trial already enrolled in our analysis.
Modeling for Network Meta-analysis
In the execution of this network meta-analysis, specific methodological principles were rigorously observed during the model’s construction. To mitigate the risk of excessive heterogeneity within the analysis, the scope of paired comparisons was deliberately confined to either exercise versus exercise or exercise versus regular care modalities. Consequently, comparisons involving exercise and other treatment options, such as non-steroidal anti-inflammatory drugs, transcutaneous electrical nerve stimulation, or various nutritional supplements, were systematically excluded. The rationale for this exclusion was predicated on the premise that the incorporation of a broader array of treatments could potentially introduce divergent network geometries. This variability, attributable to the differences in the nature of the therapies under consideration, could potentially precipitate inconsistent outcomes within the network meta-analysis [43].
In our study, the categorization of exercise types was meticulously conducted based on the specific content of the exercise prescription [44]. This process entailed a detailed discussion and analysis by two authors (Tsai IC and Lei WT), followed by a validation from a rehabilitation physician (Chang KV). For example, exercises that are conventionally recognized as strength training, such as squats and heel raises, were classified under the strength training category. This classification was upheld even in cases where the original authors of the studies might have referred to these exercises as stretching exercises [42, 45, 46]. The decision to categorize exercises in this manner was grounded in the actual exercise regimen prescribed in the studies, rather than solely on the terminology used by the original study authors.
Methodological Quality Appraisal
In order to evaluate the methodological quality of the studies incorporated into our analysis, we utilized the Cochrane risk of bias tool for randomized trials (RoB 2, version 2, based in London, United Kingdom) [47]. This tool is designed with six fundamental domains that are critical for assessing the integrity and rigor of a study. These domains encompass the randomization process, adherence to the intervention protocol, management of missing outcome data, accuracy of outcome measurement, potential for selective reporting, and the overall assessment of bias risk. Each of these elements plays a pivotal role in determining the reliability and validity of the findings reported in the randomized trials under review.
Primary Outcome: Pain Intensity Reduction, Mean Difference
In this study, the primary outcomes assessed were the changes in pain intensity, quantified using the VAS, subsequent to exercise intervention or regular care. We incorporated data from evaluations conducted at both the 4-week and 8-week time points for comprehensive analysis.
To quantify these primary study outcomes, specifically the changes in pain intensity, we employed the mean difference along with 95% confidence intervals (95% CI). This methodological choice was predicated on the aim of rendering the results more accessible and interpretable for readers. The use of mean difference values facilitates a straightforward visualization of the extent of change, expressed in terms of degrees on a 10 cm VAS scale dedicated to measuring pain intensity. Such an approach enhances the clarity and comprehensibility of the outcome measures, aiding in the practical application and understanding of the study’s findings.
Secondary Outcome: Difference in Risk of Dropout
The secondary outcome measure in our study was the difference in risk of dropout at the 8th week, serving as an intuitive indicator of the sustainability and acceptability of the various exercise interventions. For example, consider a scenario where an individual opts for a particular exercise regimen to alleviate menstrual discomfort and encounters a dropout rate of 12%. In comparison, the control group, which does not receive any specific intervention and might subsequently seek medical assistance or initiate an exercise routine independently, shows a dropout rate of 7%. In this context, the difference in risk of dropout between the two groups would be 5%. This measure effectively reflects the relative adherence to the exercise regimen, offering insights into the feasibility and potential barriers to sustained participation in the prescribed exercise routines for managing primary dysmenorrhea.
Data Extraction, Management and Conversion
The data extraction process from the evaluated studies was meticulously executed by two independent authors (Tsai IC and Lei WT). This comprehensive extraction encompassed various aspects such as demographic data, the study design, specific details of the exercise protocols implemented, and both primary and secondary outcome measures.
In instances where certain data elements were not directly accessible within the published articles, efforts were made to contact the corresponding authors of those studies to acquire the original data.
The process of data extraction, including the conversion and amalgamation of results from different study arms, was conducted in strict adherence to the guidelines outlined in the Cochrane Handbook for Systematic Reviews of Interventions, as well as recommendations from relevant medical literature [26, 48, 49]. This approach ensured a standardized, rigorous, and methodologically sound handling of the data, thereby enhancing the reliability and validity of the results derived from our network meta-analysis.
Statistical Analyses
Due to the inclusion of multiple types of exercises, we employed a random-effects model for this network meta-analysis [50]. The analysis was conducted using MetaInsight (version 4.0.2, Complex Reviews Support Unit, National Institute for Health Research, United Kingdom) under a frequentist framework. MetaInsight is a web-based service for network meta-analysis with the statistical core based on R software, utilizing the netmeta package for frequentist statistical calculations [51].
Initially, a forest plot was generated to display all pairwise comparisons from all individual studies, along with a network plot. Subsequently, forest plots were created for mean differences in pain reduction at 4 and 8 weeks, as well as the differences in risks of dropout at 8 weeks, for each exercise type compared to the control group, to provide an overall summary of the effects. The effect sizes were presented as point estimates (95% CI). The exercise types were ranked, and the numerical values for both direct and indirect comparisons were presented in tables. Inconsistency tests were conducted to detect any data disparities. A two-tailed p value of less than 0.05 was considered statistically significant.
Sensitivity Analysis
To convert baseline and post-intervention pain intensity measurements into mean changes and standard deviations, an assumption regarding the pre-post correlation coefficient is requisite. In this analysis, we adopted a coefficient of 0.8, aligning with the recommendations delineated in the Cochrane Handbook [52]. Notably, there exists a divergence of opinions among scholars regarding the optimal value of this coefficient, with commonly cited figures being 0.5, 0.7, and 0.8 [53].
To assess the potential impact of the selected coefficient on our study’s outcomes, we undertook a sensitivity analysis. This involved recalculating the effect sizes for changes in VAS values at both the 4-week and 8-week intervals, using a coefficient of 0.5 [53]. Subsequently, we scrutinized the direction and magnitude of the effects, their statistical significance, and the relative ranking of the results. This sensitivity analysis was crucial for ensuring the robustness of our findings and their independence from the specific assumption of the correlation coefficient.
Publication Bias
Publication bias assessment adhered to the guidelines outlined in the Cochrane Handbook for Systematic Reviews of Interventions [26]. The generation of a funnel plot was performed concerning the comparison with the control group, utilizing Comprehensive Meta-Analysis software, version 4 (Biostat, Englewood, NJ). In cases where there were ten or more datasets available, an Egger’s regression test was employed.
Results
Study Identification and Selection
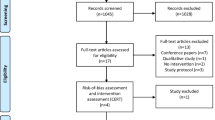
The PRISMA flowchart illustrating the literature search process can be observed in Fig. 1. Additionally, the PRISMA NMA extension’s checklist has been provided in Additional file 1: Table S1. The total number of articles retrieved from various databases is detailed in Additional file 1: Table S2. After the removal of duplicate articles and the exclusion of non-relevant articles through a thorough examination of titles and abstracts, a total of 29 randomized controlled trials were ultimately incorporated [6, 10,11,12, 15,16,17,18,19,20,21,22,23, 38,39,40, 42, 45, 46, 54,55,56,57,58,59,60,61,62,63]. Detailed information regarding the articles excluded during the final stage and the reasons for their exclusion are documented in Additional file 1: Table S3 [7,8,9, 64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109].
In our analysis, the dataset encompassed a total of 1755 individuals at 4 weeks and 1808 individuals at 8 weeks, as extracted from the 29 randomized controlled trials included. The included studies categorized the exercises as follows: relaxation exercises (comprising progressive muscle relaxation and self-administered abdominal massage), strength training, aerobic activity, yoga, and Kegel maneuvers. Exercises that incorporated elements from two or more of these categories were classified as mixed exercises. The network models for the 4-week and 8-week intervals are visually depicted in Fig. 2a, b, respectively.
Among the studies encompassing women of reproductive age, 28 trials recruited participants within the age range of 15–26 years, while only one study [54] included some women beyond the age of 26. Comprehensive details concerning the countries where recruitment took place, the age range of the participants, as well as data regarding pain intensity and dropout rates, can be found in Table 1.
Methodological Quality of the Included Studies
With respect to the overall methodological quality of the included studies, our evaluation revealed that 37.9% of them exhibited a low risk of bias, while 58.6% were associated with some risk of bias. A minor proportion, accounting for 3.4%, exhibited a high risk of bias, as depicted in Additional file 1: Figure S1. Specifically, we identified eighteen studies [10, 12, 17, 22, 39, 40, 42, 45, 46, 55,56,57,58,59,60,61,62,63] that demonstrated some risk of bias in the randomization process due to insufficient details regarding randomization procedures and allocation concealment, or the use of an allocation sequence that could be readily predicted [12, 17]. Moreover, one study [46] received a high-risk rating concerning selective reporting, as it gathered data on pain duration without subsequently reporting them. Detailed information concerning the assessment of the risk of bias is comprehensively documented in Additional file 1: Table S4.
Primary Outcome: Pain Intensity
Following a 4-week intervention period, all exercise modalities demonstrated varying degrees of pain intensity reduction in comparison to the control group, with three of them showing statistically significant reductions, and one exhibiting an effect of borderline significance. Based on the ranking of point estimates, the three exercises that exhibited statistically significant reductions in pain intensity were relaxation exercises (− 3.56; 95% CI − 5.03 to − 2.08), strength training (− 2.29; 95% CI − 3.52 to − 1.07), and aerobic activity (− 1.83; 95% CI − 3.21 to − 0.45), whereas yoga demonstrated an effect of borderline significance (− 1.63; 95% CI − 3.24 to − 0.01), as illustrated in Fig. 3a.
Upon completion of the 8-week intervention period, it is noteworthy that all exercise modalities exhibited effect sizes with 95% CIs that did not intersect with 0, indicating statistically significant reductions in menstrual pain. Based on the point estimates of effect sizes, the interventions were ranked in the following order (as depicted in Fig. 3b): relaxation exercise (− 3.87; 95% CI − 5.51 to − 2.22), mixed exercise (− 3.67; 95% CI − 5.15 to − 2.19), strength training (− 3.17; 95% CI − 4.04 to − 2.30), Kegel maneuvers (− 2.93; 95% CI − 4.62 to − 1.24), aerobic activity (− 2.77; 95% CI − 3.63 to − 1.91), and yoga (− 2.75; 95% CI − 4.00 to − 1.51). These findings suggest that all of the aforementioned exercise interventions were efficacious in reducing menstrual pain by the eighth week.
Table 2 provides a comprehensive overview of the ranking and pairwise comparisons among all intervention groups at both the 4-week and 8-week assessment points, respectively. Moreover, Additional file 1: Figure S2a, b present visual representations of the mean differences observed in the pairwise comparisons for the 4-week and 8-week analyses, respectively.
Secondary Outcome: Difference in Risk of Dropout
Through our analysis of the impact of dropouts at 8 weeks, employing the risk difference metric, we observed that five out of the six types of exercises exhibited 95% CIs that overlapped with 0. This indicates that there was no statistically significant difference in dropout rates when compared to the control group, as illustrated in Fig. 4. The sole exception was relaxation exercise, which displayed a risk difference effect size of − 0.11 (95% CI − 0.20 to − 0.02), signifying an 11% lower risk of dropout in comparison to the control group. These findings suggest that among all the exercises and the control group, relaxation exercise had the lowest risk of dropout.
Additional file 1: Figure S3 presents the differences in risk of dropout between various types of exercises as well as between the exercise groups and the control group for the studies with available data at 8 weeks.
Inconsistency Test
Utilizing the network generated by the interconnected nodes, we conducted both direct and indirect comparisons and subjected them to statistical assessment to ascertain consistency. The outcomes of the pertinent tests for pain intensity at 4 weeks and 8 weeks can be reviewed in Additional file 1: Table S5, while the results for dropout rates at 8 weeks are detailed in Additional file 1: Table S6. Importantly, all available comparisons yielded p values exceeding 0.05, signifying a lack of evidence supporting inconsistency between direct and indirect comparisons.
Sensitivity Analysis
A sensitivity analysis was undertaken by adjusting the pre-post correlation coefficient from 0.8 to 0.5, followed by a recalculation of the network comparisons at both four and 8 weeks, as illustrated in Additional file 1: Figure S4a, b. Encouragingly, our findings revealed that the direction of effect sizes, ranking, and interpretation of the results remained consistent with those obtained using a coefficient of 0.8, as observed in Fig. 3a, b. Additionally, it is worth noting that the actual numerical differences between the two coefficients were all less than 0.05, a value that is considered clinically insignificant on a 10 cm VAS.
Publication Bias
Additional file 1: Figure S5 shows the funnel plot for publication bias. The Egger’s test yielded a p value of 0.20, indicating no significant publication bias.
Discussion
Main Findings and Clinical Implications
Based on the findings of our study, it is evident that all types of exercises were efficacious in reducing menstrual pain when compared to the control group at the 8-week mark. Furthermore, there were no discernible differences in dropout risk between any of the exercise modalities, except for relaxation exercise, when compared to the control group. Relaxation exercises emerged as the most effective approach for pain reduction, as evidenced by a 10-cm VAS score of − 3.56 (95% CI − 5.03 to − 2.08) at 4 weeks and − 3.87 (95% CI − 5.51 to − 2.22) at 8 weeks. Additionally, relaxation exercise exhibited a notably lower dropout rate of − 0.11 (95% CI − 0.20 to − 0.02) in comparison to other exercise modalities and the control group, further underscoring its effectiveness.
This research has significant value for women who are considering exercise as a means to alleviate menstrual pain. It offers valuable insights into the effectiveness of various exercise modalities in reducing menstrual pain and provides information about the expected timeline for experiencing significant improvements. For instance, women interested in strength training can anticipate experiencing relief as early as 4 weeks into the regimen. Conversely, those opting for Kegel exercises should be prepared for a longer timeframe, with noticeable effects potentially taking up to two months to manifest. In cases where there is no specific preference, selecting relaxation exercises is likely to be associated with a lower likelihood of discontinuation and a higher probability of achieving early results.
Significance of the Findings Compared to Existing Literature
The studies by Matthewman et al. [13] and Carroquino-Garcia et al. [14] conducted pairwise meta-analyses to explore the impact of physical activity on primary dysmenorrhea. They both found that exercise could lead to a reduction in pain intensity, with Matthewman et al. reporting a decrease of − 1.89 (95% CI − 2.96 to − 1.09) on a 10 cm VAS scale and Carroquino-Garcia et al. indicating a reduction of − 1.86 (95% CI − 3.17 to − 0.55). However, these studies faced limitations due to grouping all types of exercise together, resulting in high heterogeneity among the included trials.
In contrast, our network meta-analysis addresses this limitation by separately evaluating different types of exercises. This approach allows us to provide a more nuanced understanding of the preferable exercise type and ideal duration for alleviating menstrual pain, which previous traditional meta-analyses [32,33,34, 36] were unable to achieve due to their reliance on traditional meta-analysis methods.
Possible Physiological and Psychological Mechanisms Underlying the Observed Results
Menstrual pain is primarily attributed to the secretion of prostaglandins, which induces uterine contractions, diminishes uterine blood flow, and heightens pain sensitivity [1]. Exercise exerts multiple physiological effects, including enhanced blood circulation to various body regions [110], dilation of blood vessels [111], and an elevation of pain threshold [112, 113]. Additionally, exercise promotes the release of endorphins [4, 5], modulates macrophage polarization, shifting from the production of inflammatory cytokines like IL-1β to anti-inflammatory cytokines such as IL-10 [114], thereby yielding an analgesic effect that contributes to pain alleviation. The psychological aspects of exercise play a crucial role in pain sensation reduction, encompassing mechanisms such as distraction, cognitive focus redirection [115], stress mitigation, mood enhancement [116], and the cultivation of a sense of control and empowerment [117]. These combined physiological and psychological effects may elucidate the varying efficacy of different exercise modalities, particularly when employed in more extended interventions, such as those spanning approximately 8 weeks.
Relaxation exercise emerged as the most efficacious physical activity for pain reduction, displaying significant effectiveness at both the 4 and 8-week points. This intervention encompasses techniques such as progressive muscle relaxation [118] and abdominal massage [119], which are commonly utilized nursing strategies for managing acute post-operative pain [119]. The relaxation effect elicited by these techniques contributes to a reduction in pain sensitivity [120].
Strength training and aerobic activity, ranked as the second and third most effective exercises, respectively, represent moderate to high-intensity exercise modalities that exert a more pronounced influence on pain sensitivity and overall physical well-being. In contrast, mixed exercises may exhibit reduced effectiveness, potentially attributable to the heterogeneity of interventions or challenges associated with adhering to relatively complex protocols. The observed non-significant effect of Kegel exercises at 4 weeks may be attributed to their low-intensity nature.
An intriguing finding in our study was the similarity in dropout rates between the exercise groups and the control group, which could be attributed to two key factors. Firstly, the exercise interventions employed in our study were characterized by their ease of practice [45], minimal time requirements [10], and high tolerability [6], making them well-suited for participants. Secondly, some individuals with primary dysmenorrhea who were allocated to the regular care (no intervention) group may have sought additional measures to alleviate their menstrual pain, leading to protocol violations and subsequent dropout. Among the included studies, certain participants opted to initiate contraceptive pill usage as a means of managing menstrual pain [20], while others explored complementary therapies [12].
Limitations
Our study has certain limitations. The enrolled studies predominantly focused on individuals with regular menstrual cycles, a practical choice to facilitate the organization of exercise programs and follow-up assessments. Regrettably, this approach resulted in the exclusion of women with irregular menstrual cycles, a condition affecting 5.0–35.6% of reproductive-age women [121]. Nevertheless, it should be acknowledged that the inclusion of patients with irregular menstrual cycles in a clinical trial would pose significant technical challenges.
Secondly, our review encompassed 29 studies, with 28 of them enrolling participants within the age range of 15–26 years, while only one study incorporated participants over the age of 26 [54]. This composition may potentially restrict the generalizability of our findings to encompass all women. However, it is essential to note that menstrual pain typically reaches its peak severity in the initial years following menarche and gradually diminishes with advancing age [1]. Consequently, our study outcomes retain relevance and utility within the context of clinical practice.
Conclusion
In summary, our analysis revealed that all forms of exercise yielded noteworthy reductions in pain intensity at the 8-week mark. Notably, relaxation exercise emerged as the most efficacious intervention for pain reduction at both the 4 and 8-week time points, additionally exhibiting a significantly lower dropout risk when compared to the control group.
Availability of Data and Materials
Data are contained within the article and Supplementary Files.
Code Availability
MetaInsight is a service provided by the Complex Reviews Support Unit that utilizes the statistical software R, with a website interface powered by R-shiny. For detailed information regarding the software codes, please contact the corresponding party. Comprehensive Meta-Analysis version 4 is a software package developed by Biostat that is available for commercial use.
References
Ferries-Rowe E, Corey E, Archer JS. Primary dysmenorrhea: diagnosis and therapy. Obstet Gynecol. 2020;136:1047–58. https://doi.org/10.1097/aog.0000000000004096.
Dawood MY. Nonsteroidal anti-inflammatory drugs and changing attitudes toward dysmenorrhea. Am J Med. 1988;84:23–9. https://doi.org/10.1016/0002-9343(88)90473-1.
Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015;2015: Cd001751. https://doi.org/10.1002/14651858.CD001751.pub3.
Saanijoki T, Tuominen L, Tuulari JJ, Nummenmaa L, Arponen E, Kalliokoski K, et al. Opioid release after high-intensity interval training in healthy human subjects. Neuropsychopharmacology. 2018;43:246–54. https://doi.org/10.1038/npp.2017.148.
Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11:607–15. https://doi.org/10.1038/nri3041.
Chen HM, Hu HM. Randomized trial of modified stretching exercise program for menstrual low back pain. West J Nurs Res. 2019;41:238–57. https://doi.org/10.1177/0193945918763817.
Huang WC, Chiu PC, Ho CH. The sprint-interval exercise Using a spinning bike improves physical fitness and ameliorates primary dysmenorrhea symptoms through hormone and inflammation modulations: a randomized controlled trial. J Sports Sci Med. 2022;21:595–607. https://doi.org/10.52082/jssm.2022.595.
Kannan P, Cheung KK, Lau BW, Li L, Chen H, Sun F. A mixed-methods study to evaluate the effectiveness and cost-effectiveness of aerobic exercise for primary dysmenorrhea: a study protocol. PLoS ONE. 2021;16: e0256263. https://doi.org/10.1371/journal.pone.0256263.
Cholbeigi E, Rezaienik S, Safari N, Lissack K, Griffiths MD, Alimoradi Z. Are health promoting lifestyles associated with pain intensity and menstrual distress among Iranian adolescent girls? BMC Pediatr. 2022;22:574. https://doi.org/10.1186/s12887-022-03639-x.
Rakhshaee Z. Effect of three yoga poses (cobra, cat and fish poses) in women with primary dysmenorrhea: a randomized clinical trial. J Pediatr Adolesc Gynecol. 2011;24:192–6. https://doi.org/10.1016/j.jpag.2011.01.059.
Ortiz MI, Cortés-Márquez SK, Romero-Quezada LC, Murguía-Cánovas G, Jaramillo-Díaz AP. Effect of a physiotherapy program in women with primary dysmenorrhea. Eur J Obstet Gynecol Reprod Biol. 2015;194:24–9. https://doi.org/10.1016/j.ejogrb.2015.08.008.
Çelik AS, Apay SE. Effect of progressive relaxation exercises on primary dysmenorrhea in Turkish students: a randomized prospective controlled trial. Complement Ther Clin Pract. 2021;42: 101280. https://doi.org/10.1016/j.ctcp.2020.101280.
Matthewman G, Lee A, Kaur JG, Daley AJ. Physical activity for primary dysmenorrhea: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2018;219:255.e1-255.e20. https://doi.org/10.1016/j.ajog.2018.04.001.
Carroquino-Garcia P, Jiménez-Rejano JJ, Medrano-Sanchez E, de la Casa-Almeida M, Diaz-Mohedo E, Suarez-Serrano C. Therapeutic exercise in the treatment of primary dysmenorrhea: a systematic review and meta-analysis. Phys Ther. 2019;99:1371–80. https://doi.org/10.1093/ptj/pzz101.
Yildiz E, Acaroğlu R. The effect of massage and progressive relaxation exercises on pain intensity and menstrual Symptoms in students with primary dysmenorrhea: a randomized controlled trial. Holist Nurs Pract. 2022;36:284–94. https://doi.org/10.1097/hnp.0000000000000541.
Azima S, Bakhshayesh HR, Kaviani M, Abbasnia K, Sayadi M. Comparison of the effect of massage therapy and isometric exercises on primary dysmenorrhea: a randomized controlled clinical trial. J Pediatr Adolesc Gynecol. 2015;28:486–91. https://doi.org/10.1016/j.jpag.2015.02.003.
Ozturk N, Gerçek Öter E, Kürek EM. The effect of abdominal massage and stretching exercise on pain and dysmenorrhea symptoms in female university students: a single-blind randomized-controlled clinical trial. Health Care Women Int. 2023;44:621–38. https://doi.org/10.1080/07399332.2022.2061973.
Saleh H, Mowafy H. Stretching or core strengthening exercises for managing primary dysmenorrhea. J Womens Health Care. 2016;5:1–6.
Kannan P, Chapple CM, Miller D, Claydon-Mueller L, Baxter GD. Effectiveness of a treadmill-based aerobic exercise intervention on pain, daily functioning, and quality of life in women with primary dysmenorrhea: a randomized controlled trial. Contemp Clin Trials. 2019;81:80–6. https://doi.org/10.1016/j.cct.2019.05.004.
Kirca N, Celik A. The effect of yoga on pain level in primary dysmenorrhea. Health Care Women Int. 2021;44:1–20. https://doi.org/10.1080/07399332.2021.1958818.
Kirmizigil B, Demiralp C. Effectiveness of functional exercises on pain and sleep quality in patients with primary dysmenorrhea: a randomized clinical trial. Arch Gynecol Obstet. 2020;302:153–63. https://doi.org/10.1007/s00404-020-05579-2.
Kaur A, Saxena G, Dhakshinamoorty P. Comparison of effect of fast and slow Kegels exercises in reducing pain in primary dysmenorrhea: experimental design. Physiother Occup Therapy J. 2013;6:135–41.
Yosri MM, Hamada HA, Abd El-Rahman Mohamed M, Yousef AM. Effect of different squatting exercises on menstrual aspects, pelvic mechanics and uterine circulation in primary dysmenorrhoea: a randomised controlled trial. J Obstet Gynaecol. 2022;42:2153021. https://doi.org/10.1080/01443615.2022.2153021.
Tsai IC, Hsu CW, Chang CH, Tseng PT, Chang KV. The effect of curcumin differs on individual cognitive domains across different patient populations: a systematic review and meta-analysis. Pharmaceuticals. 2021;14:1235. https://doi.org/10.3390/ph14121235.
Tsai IC, Hsu CW, Chang CH, Tseng PT, Chang KV. Effectiveness of coenzyme Q10 supplementation for reducing fatigue: a systematic review and meta-analysis of randomized controlled trials. Front Pharmacol. 2022;13: 883251. https://doi.org/10.3389/fphar.2022.883251.
Chaimani A, Caldwell DM, Li A, Higgins JPT, Salanti G. Chapter 11: Undertaking network meta-analyses. In: Cochrane handbook for systematic reviews of interventions version 6.4 (updated August 2023). 2023 [cited Feb 2, 2024]; https://training.cochrane.org/handbook/current/chapter-11.
Hsu PC, Chang KV, Chiu YH, Wu WT, Özçakar L. Comparative effectiveness of botulinum toxin injections and extracorporeal shockwave therapy for post-stroke spasticity: a systematic review and network meta-analysis. eClinicalMedicine. 2022;43: 101222. https://doi.org/10.1016/j.eclinm.2021.101222.
Tseng PT, Chen YW, Zeng BY, Zeng BS, Hung CM, Sun CK, et al. The beneficial effect on cognition of noninvasive brain stimulation intervention in patients with dementia: a network meta-analysis of randomized controlled trials. Alzheimer’s Res Therapy. 2023;15:20. https://doi.org/10.1186/s13195-023-01164-2.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84. https://doi.org/10.7326/M14-2385.
Tsai IC, Chang KV. INPLASY202330050 Comparative effectiveness of different exercises for reducing pain intensity in primary dysmenorrhea: a network meta-analysis of randomized controlled trials. 2023 [cited Feb 2, 2024]. https://doi.org/10.37766/inplasy2023.3.0050.
Daley AJ. Exercise and primary dysmenorrhoea: a comprehensive and critical review of the literature. Sports Med. 2008;38:659–70. https://doi.org/10.2165/00007256-200838080-00004.
Abaraogu UO, Tabansi-Ochiogu CS, Igwe ES. Effectiveness of exercise therapy on pain and quality of life of patients with primary dysmenorrhea: a systematic review with meta-analysis. Turk J Phys Med Rehab. 2016;62:346–54. https://doi.org/10.5606/tftrd.2016.95580.
Armour M, Ee CC, Naidoo D, Ayati Z, Chalmers KJ, Steel KA, et al. Exercise for dysmenorrhoea. Cochrane Database Syst Rev. 2019;9:Cd004142. https://doi.org/10.1002/14651858.CD004142.pub4.
Kim SD. Yoga for menstrual pain in primary dysmenorrhea: a meta-analysis of randomized controlled trials. Complement Ther Clin Pract. 2019;36:94–9. https://doi.org/10.1016/j.ctcp.2019.06.006.
Manouchehri E, Alirezaei S, Roudsari RL. Compliance of published randomized controlled trials on the effect of physical activity on primary dysmenorrhea with the consortium’s integrated report on clinical trials statement: a critical appraisal of the literature. Iran J Nurs Midwifery Res. 2020;25:445–54. https://doi.org/10.4103/ijnmr.IJNMR_223_19.
López-Liria R, Torres-Álamo L, Vega-Ramírez FA, García-Luengo AV, Aguilar-Parra JM, Trigueros-Ramos R, et al. Efficacy of physiotherapy treatment in primary dysmenorrhea: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18:7832. https://doi.org/10.3390/ijerph18157832.
ACOG Committee Opinion No 760. Dysmenorrhea and endometriosis in the adolescent. Obstet Gynecol. 2018;132:e249–58. https://doi.org/10.1097/aog.0000000000002978.
Samy A, Zaki SS, Metwally AA, Mahmoud DSE, Elzahaby IM, Amin AH, et al. The effect of Zumba exercise on reducing menstrual pain in young women with primary dysmenorrhea: a randomized controlled trial. J Pediatr Adolesc Gynecol. 2019;32:541–5. https://doi.org/10.1016/j.jpag.2019.06.001.
Abbaspour Z, Rostami M, Najjar S. The effect of exercise on primary dysmenorrhea. J Res Health Sci. 2004;4:26–31.
Heidarimoghadam R, Abdolmaleki E, Kazemi F, Masoumi SZ, Khodakarami B, Mohammadi Y. The effect of exercise plan based on FITT protocol on primary dysmenorrhea in medical students: a clinical trial study. J Res Health Sci. 2019;19: e00456.
Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15(Suppl 1):S17-24. https://doi.org/10.1007/s00586-005-1044-x.
Gamit KS, Sheth MS, Vyas N. The effect of stretching exercise on primary dysmenorrhea in adult girls. Int J Med Sci Public Health. 2014;3:549–51. https://doi.org/10.5455/ijmsph.2014.210220142.
Zhang J, Yuan Y, Chu H. The impact of excluding trials from network meta-analyses—an empirical study. PLoS ONE. 2016;11: e0165889. https://doi.org/10.1371/journal.pone.0165889.
Kloubec J. Pilates: How does it work and who needs it? Muscles Ligaments Tendons J. 2011;1:61–6.
Shahr-jerdy S, Hosseini RS, Gh ME. Effects of stretching exercises on primary dysmenorrhea in adolescent girls. Biomed Hum Kinet. 2012;4:127–32. https://doi.org/10.2478/v10101-012-0024-y.
Patel NS, Tanna TH, Bhatt S. Effect of active stretching exercises on primary dysmenorrhea in college going female students. Indian J Physiother Occup Therapy Int J. 2015;9:72–6.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898. https://doi.org/10.1136/bmj.l4898.
Deeks JJ, Higgins JPT, Altman DG. Chapter 10: Analysing data and undertaking meta-analyses. In: Cochrane handbook for systematic reviews of interventions. Version 6.4 (updated August 2023). 2023 [cited Feb 2, 2024]. https://training.cochrane.org/handbook/current/chapter-10.
Higgins JPT, Eldridge S, Li T. Chapter 23: Including variants on randomized trials. In: Cochrane handbook for systematic reviews of interventions. Version 6.4 (updated August 2023). 2023 [cited Feb 2, 2024]. https://training.cochrane.org/handbook/current/chapter-23.
Borenstein M, Hedges LV, Rothstein HR. Fixed-effect versus random-effects models. In: Borenstein M, editor. Introduction to meta-analysis. Hoboken: Wiley; 2009. p. 77–86.
Owen RK, Bradbury N, Xin Y, Cooper N, Sutton A. MetaInsight: an interactive web-based tool for analyzing, interrogating, and visualizing network meta-analyses using R-shiny and netmeta. Res Synth Methods. 2019;10:569–81. https://doi.org/10.1002/jrsm.1373.
Higgins JPT, Li T, Deeks JJ. Chapter 6: Choosing effect measures and computing estimates of effect. In: Cochrane handbook for systematic reviews of interventions. Version 6.4 (updated August 2023). 2023 [cited Feb 2, 2024]. https://training.cochrane.org/handbook/current/chapter-06.
Pearson MJ, Smart NA. Reported methods for handling missing change standard deviations in meta-analyses of exercise therapy interventions in patients with heart failure: a systematic review. PLoS ONE. 2018;13: e0205952. https://doi.org/10.1371/journal.pone.0205952.
Sakuma Y, Sasaki-Otomaru A, Ishida S, Kanoya Y, Arakawa C, Mochizuki Y, et al. Effect of a home-based simple yoga program in child-care workers: a randomized controlled trial. J Altern Complement Med. 2012;18:769–76. https://doi.org/10.1089/acm.2011.0080.
Salehi F, Marefati H, Mehrabian H, Sharifi H. Effect of pilates exercise on primary dysmenorrhea. J Res Rehab Sci. 2012;8:248–53.
Reyhani T, Jafarnejad F, Behnam H, Ajam M, Baghaei M. The effect of brisk walking on primary dysmenorrhea in girl students. Iran J Obstet Gynecol Infertility. 2013;16:14–9.
Rezvani S, Taghian F, Valiani M. The effect of aquatic exercises on primary dysmenorrhoea in nonathlete girls. Iran J Nurs Midwifery Res. 2013;18:378–83.
Siahpour T, Nikbakht M, Rahimi E, Rabiee M. The Effect of 8 weeks aerobic exercise and yoga on primary dismenorrhea. Armaghane Danesh Yasuj Univ Med Sci J. 2013;18:475–83.
Heidarianpour A, Zamiri DF. The effects of 8 weeks of moderate intensity aerobic exercise on menstrual cycle disorders and serum levels of sex hormones in non athlete women. Sci J Kurd Univ Med Sci. 2016;21:103–11. https://doi.org/10.22102/21.2.103.
Nasri M, Barati AH, Ramezani A. The effects of aerobic training and pelvic floor muscle exercise on primary dysmenorrhea in adolescent girls. J Clin Nurs Midwifery. 2016;5:53–61.
Shah S, Verma N, Begani P, Nagar H, Mujawar N. Effect of exercises on primary dysmenorrhoea in young females. Int J Physiother Res. 2016;4:1658–62. https://doi.org/10.16965/ijpr.2016.155.
Tharani G, Dharshini E, Rajalaxmi V, Kamatchi K, Vaishnavi G. To compare the effects of stretching exercise versus aerobic dance in primary dysmenorrhea among collegiates. Drug Invent Today. 2018;10(Special Issue 1):2844–8.
Akbas E, Erdem EU. Effectiveness of group aerobic training on menstrual cycle symptoms in primary dysmenorrhea. Med J Bakirkoy. 2019;15:209–16. https://doi.org/10.4274/BTDMJB.galenos.2018.20180621103019.
Monori A, Csakvari T, Karacsony I, Ferenczy M, Fusz K, Olah A, et al. Comparing the effect of progressive relaxation and perineal strengthening interval exercises among women with primary dysmenorrhoea to reduce menstrual cramps. Value Health. 2017;20:A519. https://doi.org/10.1016/j.jval.2017.08.684.
Günebakan Ö, Acar M. The effect of tele-yoga training in healthy women on menstrual symptoms, quality of life, anxiety-depression level, body awareness, and self-esteem during COVID-19 pandemic. Ir J Med Sci. 2023;192:467–79. https://doi.org/10.1007/s11845-022-02985-0.
Fathy FT, Gonied AS, El-Dosoky MM, Mohamed SL, Mohamed NS. Effect of aerobic exercises on intensity of primary dysmenorrhea among nursing students. Neuroquantology. 2022;20:6639–54.
Nag U, Kodali M. Meditation and yoga as alternative therapy for primary dysmenorrhea. Int J Med Pharm Sci. 2013;3:39–44.
Arora A, Yardi S, Gopal S. Effect of 12-weeks of aerobic exercise on primary dysmenorrhea. Indian J Physiother Occup Therapy Int J. 2014;8:130.
Yilmaz-Akyuz E, Aydin-Kartal Y. The effect of diet and aerobic exercise on premenstrual syndrome: randomized controlled trial. Rev Nutr Braz J Nutr. 2019;32: e180246. https://doi.org/10.1590/1678-9865201932e180246.
Yonglitthipagon P, Muansiangsai S, Wongkhumngern W, Donpunha W, Chanavirut R, Siritaratiwat W, et al. Effect of yoga on the menstrual pain, physical fitness, and quality of life of young women with primary dysmenorrhea. J Bodyw Mov Ther. 2017;21:840–6. https://doi.org/10.1016/j.jbmt.2017.01.014.
Yang NY, Kim SD. Effects of a yoga program on menstrual cramps and menstrual distress in undergraduate students with primary dysmenorrhea: a single-blind, randomized controlled trial. J Altern Complement Med. 2016;22:732–8. https://doi.org/10.1089/acm.2016.0058.
Dauneria S, Keswani J. A study on the effect of yoga and naturopathy on dysmenorrhea. Int J Yoga Allied Sci. 2014;3:38–42.
Paithankar DSM, Hande DN. Effectiveness of Pilates over conventional physiotherapeutic treatment in females with primary dysmenorrhea. IOSR J Dental Med Sci. 2016;15:156–63.
Thoke AV, Gawali MH. Effects of Surya Namaskar and Yoga Nidra on physical problems of adolescent girls during their menstruation. GOEIJ 2015;4
Gupta R, Kaur S, Kaur A. Comparison to assess the effectiveness of active exercises and dietary ginger vs. active exercises on primary dysmenorrheal among adolescent girls. Nurs Midwifery Res. 2013;9:168–77.
Shirvani MA, Motahari-Tabari N, Alipour A. Use of ginger versus stretching exercises for the treatment of primary dysmenorrhea: a randomized controlled trial. J Integr Med. 2017;15:295–301. https://doi.org/10.1016/s2095-4964(17)60348-0.
Chaudhuri A, Singh A, Dhaliwal L. A randomised controlled trial of exercise and hot water bottle in the management of dysmenorrhoea in school girls of Chandigarh. India Indian J Physiol Pharmacol. 2013;57:114–22.
Motahari-Tabari N, Shirvani MA, Alipour A. Comparison of the effect of stretching exercises and mefenamic acid on the reduction of pain and menstruation characteristics in primary dysmenorrhea: a randomized clinical trial. Oman Med J. 2017;32:47–53. https://doi.org/10.5001/omj.2017.09.
Kanwal R, Masood T, Awan WA, Babur M, Baig MS. Effectiveness of TENS versus stretching exercises on primary dysmenorrhea in students. Int J Rehab Sci. 2017;5:18–24.
El-Bably EM, Abd El-Aziz KS, El-Bandrawy AM, Abo El-Enein MF. Effect of Pilates exercise on primary dysmenorrhea. Med J Cairo Univ. 2019;87:1187–92.
Mirbagher-Ajorpaz N, Adib-Hajbaghery M, Mosaebi F. The effects of acupressure on primary dysmenorrhea: a randomized controlled trial. Complement Ther Clin Pract. 2011;17:33–6. https://doi.org/10.1016/j.ctcp.2010.06.005.
Özgül S, Üzelpasaci E, Orhan C, Baran E, Beksaç MS, Akbayrak T. Short-term effects of connective tissue manipulation in women with primary dysmenorrhea: a randomized controlled trial. Complement Ther Clin Pract. 2018;33:1–6.
Chantler I, Mitchell D, Fuller A. Diclofenac potassium attenuates dysmenorrhea and restores exercise performance in women with primary dysmenorrhea. J Pain. 2009;10:191–200. https://doi.org/10.1016/j.jpain.2008.08.006.
Gaubeca-Gilarranz A, Fernández-de-Las-Peñas C, Medina-Torres JR, Seoane-Ruiz JM, Company-Palonés A, Cleland JA, et al. Effectiveness of dry needling of rectus abdominis trigger points for the treatment of primary dysmenorrhoea: a randomised parallel-group trial. Acupunct Med. 2018;36:302–10. https://doi.org/10.1136/acupmed-2017-011566.
Keshavarzi F, Mahmoudzadeh F, Brand S, Sadeghi Bahmani D, Akbari F, Khazaie H, et al. Both melatonin and meloxicam improved sleep and pain in females with primary dysmenorrhea-results from a double-blind cross-over intervention pilot study. Arch Womens Ment Health. 2018;21:601–9. https://doi.org/10.1007/s00737-018-0838-x.
Golub LJ, Menduke H, Lang WR. Exercise and dysmenorrhea in young teenagers: a 3-year study. Obstet Gynecol. 1968;32:508–11.
Hubbell JW. Specific and non-specific exercise for the relief of dysmenorrhea. Res Q. 1949;20:378–86.
Lundquist C. Use of the Billig exercise for dysmenorrhea for college women. Res Q. 1947;18:45–53.
Kannan P, Claydon LS, Miller D, Chapple CM. Vigorous exercises in the management of primary dysmenorrhea: a feasibility study. Disabil Rehabil. 2015;37:1334–9. https://doi.org/10.3109/09638288.2014.962108.
Vaziri F, Hoseini A, Kamali F, Abdali K, Hadianfard M, Sayadi M. Comparing the effects of aerobic and stretching exercises on the intensity of primary dysmenorrhea in the students of universities of bushehr. J Family Reprod Health. 2015;9:23–8.
Zainab S, Nithyashree P, Jumanah R, Kamalakannan M, Suganthirababu P, Kumaresan A. A study to compare the effectiveness of core strengthening exercises for phase I and phase II of menstrual cycle in primary dysmenorrhea subjects. Biomedicine. 2021;41:315–7. https://doi.org/10.51248/.v41i2.804.
Nag U, Dip P, Kodali M. Effect of yoga on primary dysmenorrhea and stress in medical students. IOSR J Dental Med Sci. 2013;4:69–73.
Behbahani BM, Ansaripour L, Akbarzadeh M, Zare N, Hadianfard MJ. Comparison of the effects of acupressure and self-care behaviors training on the intensity of primary dysmenorrhea based on McGill pain questionnaire among Shiraz University students. J Res Med Sci. 2016;21:104. https://doi.org/10.4103/1735-1995.193176.
Kannan P, Chapple CM, Miller D, Claydon LS, Baxter GD. Menstrual pain and quality of life in women with primary dysmenorrhea: rationale, design, and interventions of a randomized controlled trial of effects of a treadmill-based exercise intervention. Contemp Clin Trials. 2015;42:81–9. https://doi.org/10.1016/j.cct.2015.03.010.
Maged AM, Abbassy AH, Sakr HRS, Elsawah H, Wagih H, Ogila AI, et al. Effect of swimming exercise on premenstrual syndrome. Arch Gynecol Obstet. 2018;297:951–9. https://doi.org/10.1007/s00404-018-4664-1.
Rani M, Singh U, Agrawal GG, Natu SM, Kala S, Ghildiyal A, et al. Impact of Yoga Nidra on menstrual abnormalities in females of reproductive age. J Altern Complement Med. 2013;19:925–9. https://doi.org/10.1089/acm.2010.0676.
Sandhiya M, Senthil Selvam P, Manoj Abraham M, Palekar TJ, Sundaram MS, Kumari P, et al. A study to compare the effects of aerobic exercise versus core strengthening exercise among college girls with primary dysmenorrhea. Int J Res Pharm Sci. 2020;11:2692–7.
Imtiaz I, Riaz H. Effects of high intensity aerobic training on symptomatology of primary dysmenorrhoea. J Pak Med Assoc. 2022;72:2515–8. https://doi.org/10.47391/JPMA.5158.
Sarhadi S, Ramezani A, Gholami M, Taheri H. The effect of an aerobic training cycle in the morning and evening on primary dysmenorrhea and some physiological variables in matured girls. Iran J Obstet Gynecol Infertility. 2015;18:11–20.
Shavandi N, Taghian F, Soltani V. The effect of isometric exercise on primary dismenorrhea. J Arak Univ Med Sci. 2010;13:71–7.
Lorzadeh N, Kazemirad Y, Kazemirad N. The effect of corrective and therapeutic exercises on bleeding volume and severe menstrual pain in non-athletic women. J Obstet Gynaecol. 2021;41:1121–6. https://doi.org/10.1080/01443615.2020.1839870.
Mahvash N, Eidy A, Mehdi K, Zahra MT, Mani M, Shahla H. The effect of physical activity on primary dysmenorrhea of female university students. World Appl Scs J. 2012;17:1246–52.
Israel RG, Sutton M, O’Brien KF. Effects of aerobic training on primary dysmenorrhea symptomatology in college females. J Am Coll Health. 1985;33:241–4. https://doi.org/10.1080/07448481.1985.9935033.
Gokulakrishnan J, Momin RS. Effectiveness of Kegel’s exercises on reducing pain and menstrual cramps in dysmenorrhea among college hostel girls. Int J Res Publ Rev. 2022;3:340–3.
Sutar A, Paldhikar S, Shikalgar N, Ghodey S. Effect of aerobic exercises on primary dysmenorrhoea in college students. IOSR J Nurs Health Sci. 2016;05:20–4. https://doi.org/10.9790/1959-0505052024.
Aboushady RM-N, El-saidy TMK. Effect of home-based stretching exercises and menstrual care on primary dysmenorrhea and premenstrual symptoms among adolescent Girls. IOSR J Nurs Health Sci. 2016;5:10–7.
Azima S, Rajaei Bakhshayesh H, Abbasnia K, Kaviani M, Sayadi M. The effect of isometric exercises on primary dysmenorrhea: a randomized controlled clinical trial. Galen Med J. 2015;4:26–32. https://doi.org/10.31661/gmj.v4i1.168.
Kovács Z, Hegyi G, Szőke H. The effect of exercise on pulsatility index of uterine arteries and pain in primary dysmenorrhea. J Clin Med. 2023;12:7021. https://doi.org/10.3390/jcm12227021.
Aksu A, Vefikuluçay Yılmaz D. The effect of yoga practice on pain intensity, menstruation symptoms and quality of life of nursing students with primary dysmenorrhea. Health Care Women Int. 2024. https://doi.org/10.1080/07399332.2024.2303526.
Joyner MJ, Casey DP. Regulation of increased blood flow (hyperemia) to muscles during exercise: a hierarchy of competing physiological needs. Physiol Rev. 2015;95:549–601. https://doi.org/10.1152/physrev.00035.2013.
Dinenno FA, Tanaka H, Monahan KD, Clevenger CM, Eskurza I, DeSouza CA, et al. Regular endurance exercise induces expansive arterial remodelling in the trained limbs of healthy men. J Physiol. 2001;534:287–95. https://doi.org/10.1111/j.1469-7793.2001.00287.x.
Sluka KA, O’Donnell JM, Danielson J, Rasmussen LA. Regular physical activity prevents development of chronic pain and activation of central neurons. J Appl Physiol. 1985;2013(114):725–33. https://doi.org/10.1152/japplphysiol.01317.2012.
Rice D, Nijs J, Kosek E, Wideman T, Hasenbring MI, Koltyn K, et al. Exercise-induced hypoalgesia in pain-free and chronic pain populations: state of the art and future directions. J Pain. 2019;20:1249–66.
Sluka KA, Frey-Law L, Hoeger BM. Exercise-induced pain and analgesia? Underlying mechanisms and clinical translation. Pain. 2018;159(Suppl 1):S91–7. https://doi.org/10.1097/j.pain.0000000000001235.
Trottier ED, Doré-Bergeron MJ, Chauvin-Kimoff L, Baerg K, Ali S. Managing pain and distress in children undergoing brief diagnostic and therapeutic procedures. Paediatr Child Health. 2019;24:509–35. https://doi.org/10.1093/pch/pxz026.
Iwon K, Skibinska J, Jasielska D, Kalwarczyk S. Elevating subjective well-being through physical exercises: an Intervention Study. Front Psychol. 2021;12: 702678. https://doi.org/10.3389/fpsyg.2021.702678.
Roditi D, Robinson ME. The role of psychological interventions in the management of patients with chronic pain. Psychol Res Behav Manag. 2011;4:41–9. https://doi.org/10.2147/prbm.S15375.
Ju W, Ren L, Chen J, Du Y. Efficacy of relaxation therapy as an effective nursing intervention for post-operative pain relief in patients undergoing abdominal surgery: a systematic review and meta-analysis. Exp Ther Med. 2019;18:2909–16. https://doi.org/10.3892/etm.2019.7915.
Le Blanc-Louvry I, Costaglioli B, Boulon C, Leroi AM, Ducrotte P. Does mechanical massage of the abdominal wall after colectomy reduce postoperative pain and shorten the duration of ileus? Results of a randomized study. J Gastrointest Surg. 2002;6:43–9. https://doi.org/10.1016/s1091-255x(01)00009-9.
Adams R, White B, Beckett C. The effects of massage therapy on pain management in the acute care setting. Int J Ther Massage Bodywork. 2010;3:4–11.
Kwak Y, Kim Y, Baek KA. Prevalence of irregular menstruation according to socioeconomic status: a population-based nationwide cross-sectional study. PLoS ONE. 2019;14: e0214071. https://doi.org/10.1371/journal.pone.0214071.
Funding
This study was funded by the National Taiwan University Hospital, Bei-Hu Branch; Ministry of Science and Technology, Taiwan (MOST 106-2314-B-002-180-MY3 and MOST 109-2314-B-002-114-MY3 and 111–2314-B-002–161); and the Taiwan Society of Ultrasound in Medicine. APC was funded by the Ministry of Science and Technology of Taiwan and Taiwan Society of Ultrasound in Medicine.
Author information
Authors and Affiliations
Contributions
Data curation, Tsai IC, and Lei WT; formal analysis, Tsai IC and Lei WT; investigation, Hsu CW, Chang CH, Tseng PT, Chang KV; methodology, Hsu CW, Tseng PT, Chang KV; software, Tsai IC and Lei WT; supervision, Chang KV; validation, Hsu CW, Chang CH, Tseng PT, Chang KV; writing the original draft, Tsai IC; writing review and editing, Hsu CW, Chang CH, Lei WT, Tseng PT, Chang KV. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This network meta-analysis did not intervene or interact with humans or collect identifiable private information, and thus does not require institutional review board approval.
Consent to Publication
Not applicable.
Competing Interests
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tsai, IC., Hsu, CW., Chang, CH. et al. Comparative Effectiveness of Different Exercises for Reducing Pain Intensity in Primary Dysmenorrhea: A Systematic Review and Network Meta-analysis of Randomized Controlled Trials. Sports Med - Open 10, 63 (2024). https://doi.org/10.1186/s40798-024-00718-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40798-024-00718-4