Abstract
Purpose
Primary dysmenorrhea is the most common gynecological problem in young women and adolescents. Exercise therapy provides positive effects on women with primary dysmenorrhea. The aim of the study was to investigate the effects of a combined exercise program on pain, sleep and menstrual symptoms in patients with primary dysmenorrhea.
Methods
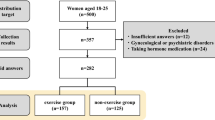
The study is a randomized controlled study. The study included 28 sedentary individuals. The participants were assigned to two groups as the exercise (mean age 22.9 ± 2.0 years) and the control (mean age 23.1 ± 1.8 years) groups. The exercise protocol was carried out with the exercise group three times a week for eight weeks. The Visual Analog Scale (VAS) was used for assessing the intensity of pain. The Menstrual Symptom Questionnaire (MSQ) and Pittsburgh Sleep Quality Index (PSQI) were used for evaluating menstrual symptoms and sleep quality, respectively. The study was registered on the Clinical Trials website by the number NCT03625375.
Results
The comparisons between the groups revealed statistically significant differences in abdominal pain severity, MSQ total score and the subscale scores of negative outcomes and management methods (p < 0.05). The intragroup comparisons of the exercise group demonstrated that the scores of the low back pain and abdominal pain and the MSQ and PSQI scores were found to be significantly different after the 8-week program (p < 0.05).
Conclusion
The combined exercise therapy is an effective way to manage symptoms associated with primary dysmenorrhea.



Similar content being viewed by others
References
Dawood MY (1990) Dysmenorrhea. Clin Obstet Gynecol 33:168–178
DeSanctis V, Soliman AT, Elsedfy H, Soliman NA, Soliman R, ElKholy M (2017) Dysmenorrhea in adolescents and young adults: a review in different country. Acta Biomed 87:233–246
Kannan P, Chapple CM, Miller D, Claydon LS, Baxter GD (2015) Menstrual pain and quality of life in women with primary dysmenorrhea: rationale, design, and interventions of a randomized controlled trial of effects of a treadmill-based exercise intervention. Contemp Clin Trials 42:81–89
Proctor M, Farqhar C (2006) Diagnosis and management of dysmenorrhea. BJM 332:7550
Matthewman G, Lee A, Kaur JG, Daley AJ (2018) Physical activity for primary dysmenorrhea: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2018.04.001
Vaziri F, Hoseini A, Kamali F, Abdali K, Hadianfard M, Sayadi M (2015) Comparing the effects of aerobic and stretching exercises on the intensity of primary dysmenorrhea in the students of universities of Bushehr. J Fam Reprod Health 9:23–28
Rakhshaee Z (2011) Effect of three yoga poses (cobra, cat and fish poses) in women with primary dysmenorrhea: a randomized clinical trial. J Pediatr Adolesc Gynecol 24:192–196
Ortizab MI, Márquezc SKC, Quezadaa LCR, Cánovasb GM, Díazc APJ (2015) Effect of a physiotherapy program in women with primary dysmenorrhea. Eur J Obstet Gynecol Reprod Biol 194:24–29
Kannan P, Chapple CM, Miller D, Claydon LS, Baxter GD (2015) Vigorous exercises in the management of primary dysmenorrhea: a feasibility study. Disabil Rehabil 37:1334–1339
Wong CL, Lai KY, Tse HM (2010) Effects of SP6 acupressure on pain and menstrual distress in young women with dysmenorrhea. Complement Ther Clin Pract 16(2):64–69. https://doi.org/10.1016/j.ctcp.2009.10.002
Huskisson EC (1974) Measurement of pain. Lancet 7889:1127–1131
Güvenç G, Seven M, Akyüz A (2014) Menstrüasyon Semptom Ölçeği’nin Türkçe'ye uyarlanması. TAF Prev Med Bull 13:367–374. https://doi.org/10.5455/pmb1-1378840527
Agargun MY, Kara H, Anlar O (1996) The validity and reliability of the Pittsburgh Sleep Quality Index. Turk Psikiyatri Derg 7:107–115
Rosenthal R (1994) Parametric measures of effect size. In: Cooper H, Hedges LV, Valentine JC (eds) The handbook of research synthesis. Russell Sage Foundation, New York, pp 231–244
Dehnavi ZM, Jafarnejad F, Kamali Z (2018) The Effect of aerobic exercise on primary dysmenorrhea: a clinical trial study. J Educ Health Promot 7:3
Sakuma Y, Sasaki-Otomaru A, Ishida S, Kanoya Y, Arakawa C, Mochizuki Y, Seiishi Y (2012) Effect of a home-based simple yoga program in child-care workers: a randomized controlled trial. J Altern Complement Med 18:769–776
Shirvani MA, Motahari-Tabari N, Alipour A (2017) Use of ginger versus stretching exercises for the treatment of primary dysmenorrhea: a randomized controlled trial. J Integr Med 15:295–301
Dmitrović R (2000) Transvaginal color Doppler study of uterine blood flow in primary dysmenorrhea. Acta Obstetricia Gynecologica Scandinavica 79:1112–1116
Tae YK, Sohee K, In OS, Byeong Seon M, Ju RJ (2017) Effects of stretching and sling exercise on pelvic correction and dysmenorrhea in university students. Res J Pharm Technol 10:3933–3938
Martarelli D, Cocchioni M, Scuri S, Pompei P (2011) Diaphragmatic breathing reduces exercise-induced oxidative stress. Evid Based Complement Altern Med 2011:932430. https://doi.org/10.1093/ecam/nep169
Talasz H, Kofler M, Kalchschmid E et al (2010) Breathing with the pelvic floor? Correlation of pelvic floor muscle function and expiratory flows in healthy young nulliparous women. Int Urogynecol J 21:475
Baker FC, Driver HS (2007) Circadian rhythms, sleep, and the menstrual cycle. Sleep Med 8:613–622
Aktaş D (2015) Prevalence and factors affecting dysmenorrhea in female university students: effect on general comfort level. Pain Manag Nurs 16:534–543
Wang ZY, Liu Z-Z, Jia C-X, Liu X (2019) Age at menarche, menstrual problems, and daytime sleepiness in Chinese adolescent girls. Sleep 42:061
Kelley GA, Kelley KS (2017) Exercise and sleep: a systematic review of previous meta-analyses. J Evid Based Med 10:26–36
Sahin S, Ozdemir K, Unsal A, Arslan R (2015) Review of frequency of dysmenorrhea and some associated factors and evaluation of the relationship between dysmenorrhea and sleep quality in university students. Gynecol Obstet Invest 78:179–185
Driver HS, Taylor SR (2000) Exercise and sleep. Sleep Med Rev 4:387–402
Kovacevic A, Mavros Y, Heisz JJ, Fiatarone Singh MA (2017) The effect of resistance exercise on sleep: a systematic review of randomized controlled trials. Sleep Med Rev 39:52–68
Uchida S, Shioda K, Morita Y, Kubota C, Ganeko M, Takeda N (2012) Exercise effects on sleep physiology. Front Neurol 3:1–5
Latthe P, Mignini L, Gray R, Hills R, Khan K (2006) Factors predisposing women to chronic pelvic pain: systematic review. BMJ 332(7544):749–755
Ju H, Jones M, Mishra GD (2015) A U-shaped relationship between body mass index and dysmenorrhea: a longitudinal study. PLoS ONE 10(7):e0134187. https://doi.org/10.1371/journal.pone.0134187
Ohde S, Tokuda Y, Takahashi O, Yanai H, Hinohara S, Fukui T (2008) Dysmenorrhea among Japanese women. Int J Gynaecol Obstet 100(1):13–17
Sundell G, Milsom I, Andersch B (1990) Factors influencing the prevalence and severity of dysmenorrhoea in young women. Br J Obstet Gynaecol 97(7):588–594
Acknowledgements
The authors would like to thank all participants in the study for their contribution.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
“All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Research and Publication Ethics Board + 2018/52–34) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.”
Informed Consent
Written informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kirmizigil, B., Demiralp, C. Effectiveness of functional exercises on pain and sleep quality in patients with primary dysmenorrhea: a randomized clinical trial. Arch Gynecol Obstet 302, 153–163 (2020). https://doi.org/10.1007/s00404-020-05579-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05579-2