Abstract
Background
India is an attractive destination for travelers. Unfortunately, numerous reports exist on traveler’s diarrhea (TD) and fecal colonization with extended-spectrum beta-lactamase-producing Escherichia coli (ESBL-EC) among international travelers visiting India. Here, we systematically reviewed studies published on the acquisition of ESBL-EC and TD attack rates among international visitors to India.
Methods
Design: Systematic review and meta-analysis.
A systematic search was performed using Google Scholar, PubMed, EMBASE, Web of Science, and gray literature from 2000 to December 2021, for studies containing data for ESBL-EC acquisition or TD experience related to a trip to India. Random effects models were used to compute the prevalence of ESBL-EC acquisition and TD attack.
Results
The literature search yielded a total of 5023 records. Of these, 31 met our inclusion criteria for systematic review and only 17 could be meta-analyzed (9 for TD, and 8 for ESBL-EC). The overall pooled attack rate of TD was 39% (95% confidence interval, CI: 25–53%). In studies where travelers' memory was used to diagnose TD, the pooled attack rate of TD was slightly higher (42%, 95% CI: 21–64%) compared to those where TD was objectively documented (33%, 95% CI: 17–49%). There were significant risks to be colonized with ESBL-EC among the travelers who experienced TD. The pooled rate of ESBL-EC colonization was 72% (CI: 67–78%). Most ESBL-EC produced CTX-M-15 enzyme. Furthermore, most of the travelers who acquired ESBL-EC were from highly industrialized countries recruited from travel clinics: Canada (n = 80), Germany (n = 69), Netherlands (n = 20), Sweden (n = 18), Japan (n = 10), Finland (n = 8), USA (n = 7), Spain (n = 5), and Denmark (n = 3).
Conclusions
TD pooled attack rate and ESBL-EC acquisition among international travelers visiting India were high in this study. However, we cannot make generalizations based upon this TD pooled attack rate for the current situation, due to a lack of current data. Our study highlights that travelers should be advised on TD to ensure that they do not disregard the risk of contracting TD and be better prepared as a result. It also illustrates the importance of international travel in acquiring antibiotic-resistant Escherichia coli.
Similar content being viewed by others
Introduction
Despite rigorous efforts towards the prevention and reduction of travelers’ diarrhea (TD), it remains one of the most common ailments among travelers worldwide [1]. The illness affects 20–40 million travelers per year depending on the destination, traveler characteristics (such as age), and season of travel [2]. TD is primarily caused by consuming food or water contaminated with microorganisms along with poor hand hygiene [3, 4]. Depending on the country, there are diverse microorganisms that can cause TD. Bacteria are the most common pathogen associated with TD responsible for 80% to 90% of cases (such as enterotoxigenic Escherichia coli, enteroaggregative E. coli, Campylobacter jejuni, Shigella species, and Salmonella species). The next most common causes consist of viruses detected in 5% to 10% of incidences (such as norovirus, rotavirus, and astrovirus), and parasites in 10% of incidences (such as Giardia lamblia and Cryptosporidium) [5,6,7]. However, in some cases either the causal agent is unknown or the etiology is revealed as mixed.
The illness is self-limited and short-lived (resolving completely in 1 to 5 days), but it can lead to dehydration [4, 8]. Other sequelae of TD include post-infectious irritable bowel syndrome (PI-IBS), reactive arthritis, and Guillain-Barré syndrome [9, 10]. TD associated with the development of PI-IBS occurs in 3% to 17% of patients [1]. Treatment of TD can have health consequences as well. For instance, treatment of TD with antibiotics while abroad can alter gut microflora and as a consequence can be colonized with extended-spectrum beta-lactamase-producing E. coli (ESBL-EC) [11], which is resistant to common antibiotics such as cephalosporins and fluoroquinolones [12]. This event can further contribute to the spread of antimicrobial resistance that may cause downstream infections [13]. Furthermore, TD can also lead to changes in the host microbiome even without antibiotic treatment [14].
In the past, TD attack rates had been reported to be high in India among travelers [15]. In addition, multiple studies have reported fecal colonization with ESBL-EC among international travelers visiting India [16]. One study estimates that annually about one-third of the 100 million travelers to the tropics acquire extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBL-PE) [17].
Even though there are several published reports on TD and fecal colonization with ESBL-EC related to an international trip to India, no study has systematically synthesized these data. This study aims to summarize the available studies on TD and fecal colonization with ESBL-EC among international travelers to India during the period of 2000 to 2021.
This evidence may help to raise the awareness of both travelers and healthcare professionals about the need for health advisory before travel and educating travelers about preventive measures. We specifically targeted studies carried out in India to understand whether there is any decreasing trend of TD and ESBL-EC acquisition rates as hygiene and improved sanitation has been enhanced in most of the states and union territories (SUTs) by the Swachh Bharat (Clean India) Mission.
Methods
We performed a systematic review and meta-analysis of studies that documented TD and/or fecal colonization with ESBL-EC among international travelers visiting India. In this study, we defined TD as the passage of unformed stools for ≥ 3 times over a span of 24 h with at least one of the following symptoms: nausea; bloody, mucus-containing stool; abdominal cramps; tenesmus; vomiting; fever; or fecal urgency while abroad and/or after returning home [18]. For practical purposes, we considered TD as it was defined in the reviewed studies. This systematic review was undertaken following the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) guidelines [19] and registered in the international prospective register of systematic reviews (registration number CRD42022324904).
Data sources and searches
We ran searches on Google Scholar, PubMed, EMBASE, and Web of Science from January 2000 to December 2021. The last search was conducted on 23 December 2021. The following keywords were used for diarrhea: “Traveler’s diarrhea” OR “Traveller’s diarrhoea” OR “Diarrhoea in travellers” OR “Diarrhea in travelers” OR “Traveler with diarrhea” OR “Traveller with diarrhoea”. Search strings also included “extended-spectrum beta-lactamase-producing Escherichia coli” OR “extended-spectrum beta-lactamase-producing Enterobacteriaceae”. These keywords were combined with “India” OR “Republic of India”. In addition, we also manually searched the reference lists of the selected studies and related key reviews to retrieve additional records. We also searched for gray literature. We did not use any language restrictions. Potentially relevant studies were exported to Endnote software X9 (Clarivate, Philadelphia, USA) and duplicated references were removed.
Study selection and data extraction
First, the titles and abstracts of retrieved studies were independently screened by two investigators (BAM and KK). After that, the full texts of potentially relevant studies were retrieved and screened for inclusion. Data were also extracted independently by two investigators (BAM and KK). Disagreements were resolved by consensus. We included studies meeting the following inclusion criteria: (1) a study must have been carried out on international travelers (population); (2) a study must have described individuals with a history of traveling to India (exposure); a study without a mandatory control group (comparison); a study must have described TD and/or fecal colonization with ESBL-EC during their trip in India or after returning back home (outcome); case reports or series published in full text, cross-sectional and prospective cohort studies describing TD and/or fecal colonization with ESBL-EC related to travel to India (study design). Criteria for exclusion from this study included: cases related to the Indian subcontinent (because in this study our target country was India) and those pre-dating 2000 because we wanted to provide the most recent evidence on TD in India. We also excluded review articles, and those on TD in the locals.
For data extraction, we designed a data extraction sheet using Microsoft Excel 2019 (Version 2204, Microsoft Corp., Albuquerque, NM, USA). For each study, extracted information included: first author, year of publication, year of diagnosis/study period, traveler’s country of origin, number of cases, etiology (if reported), performance of stool analysis or only self-reported TD, CTX-M beta-lactamase group, travel duration, area visited, patient demographics (gender and age) wherever applicable. Reported TD risk factors were also extracted. Reporting quality was not assessed because certainty in evidence from case reports and series is usually deemed to be low [20].
Data synthesis and analysis
Data analysis was performed in Stata version 16 (StataCorp, College Station, TX, USA) using the metaprop command [21]. Descriptive statistics were used to summarize information about the number of cases. The number of cases was grouped by country of origin. For the meta-analysis, the parameters were the number of travelers examined and the proportion of travelers with TD (i.e., TD attack rate) or those with a positive test for ESBL-EC. Studies that did not report the above parameters were excluded from the meta-analysis. Additional analyses were undertaken after stratification by year of diagnosis or study period. Random effects models were used to calculate the pool rates of ESBL-EC acquisition and TD attack. We assessed heterogeneity using I2 statistics. I2 of > 50% were considered to indicate substantial heterogeneity [22].
Results
Literature search and study characteristics
The literature search yielded a total of 5,023 records (Additional file 1), out of which 1,513 duplicates were removed, leaving 3,510 records. We had excluded 3,459 records out of 3,510 after screening their titles and abstracts. Only 51 records were retrieved for full-text screening, of which two were reviews and thus excluded [12, 23]. Another 18 full-texts were excluded mainly due to either a) not being pertinent to this study [13, 24,25,26,27,28,29,30,31], b) referred to the Indian subcontinent [11, 16, 32,33,34,35] or c) were carried out prior to 2000 [15, 36, 37]. Finally, 31 records with 859 cases [38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68] met our inclusion criteria for the qualitative synthesis and only 17 of them could be meta-analyzed (9 for TD and 8 for ESBL-EC).
Only one record was published in French [39]; all the others were published in English. They were published between 2005 and 2021, and the study/ diagnostic period was from 2002 to 2019.
The majority of the studies were conducted in travel clinics from high-income countries (Tables 1 and 2). Specifically, the included studies were conducted in the USA [44, 45, 50, 55,56,57], Canada [66, 67], France [39, 40], Germany [58, 59], India [51, 53], Switzerland [42, 43], Sweden [64, 65], Australia [68], Denmark [62], Finland [54], Japan [61], Korea [38], Netherlands [60], Romania [49], Russia [46], Spain [63], South Africa [48], Thailand [41], and multiple sites (India, UK, and Germany) [47]. Fourteen studies reported on participants who were diagnosed with ESBL-EC after returning from India (Table 2). Of these fourteen studies, ten (71%) clearly reported that ESBL-EC was found to produce CTX-M-15 enzyme [55, 56, 59,60,61, 63,64,65,66,67].
The details of records included in this study are available in the supplementary material (Additional file 2). The majority (850/859; 99%) of the travelers with TD and/or ESBL-EC included in this study were diagnosed between 2002 and 2017. In addition, in 41 cases, information on TD was not specifically described [56, 57, 59, 62, 64, 66]. Moreover, TD diagnosis was based solely on traveler’s memory in seven records [41,42,43,44,45, 52, 53] (which may indicate recall bias). In the remaining studies, TD was diagnosed clinically with direct stool examination or with culture [38,39,40, 46, 48, 49, 51, 68] or polymerase chain reaction (PCR) [47, 50]. ESBL-EC was diagnosed using culture followed by polymerase chain reaction [54, 58, 62, 65] and sequencing [55, 56, 59,60,61, 63, 64, 66, 67]. In one record, ESBL-EC diagnosis method was not specified [57].
Pooled attack rate of TD and rate of colonization with ESBL-producing E. coli
Nine studies (11 data points), which had sufficient data on TD, were used in the meta-analysis [40, 42,43,44,45, 47, 50, 52, 53]. As displayed in Fig. 1A, the overall estimated pooled attack rate of TD was 39% (95% confidence interval, CI: 25–53%). It is important to note that TD was diagnosed between 2002 and 2014 in these studies. Heterogeneity across studies was considerable (I2 = 98%) and statistically significant (p < 0.001).
A Pooled attack rate of traveler’s diarrhea among international travelers visiting India (Studies are grouped by diagnosis period). Studies are represented by the first author, publication year, and the number of cases/number of travelers examined. The studies by Tillet and Steffen had 2 data points each. ES = effect size; CI = confidence interval. B Pooled attack rate of traveler’s diarrhea among international travelers visiting India (Studies are grouped by methods of documenting traveler’s diarrhea). Studies are represented by the first author, publication year, and the number of cases/number of travelers examined. The studies by Tillet and Steffen had 2 data points each. ES = effect size; CI = confidence interval
In the subgroup analysis, the pooled attack rate of TD varied depending upon the method used to document TD: the pooled attack rate of TD was slightly higher [42% (95% CI:21–64%)] in studies where TD was diagnosed solely on traveler’s memory compared to those where TD was objectively documented [33% (95% CI: 17–49%)] (Fig. 1B).
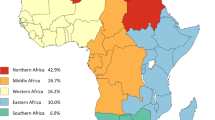
It had been observed that most of the travelers who became colonized with ESBL-EC were more likely to have an history of TD (Table 2). Eight studies were eligible for inclusion in the meta-analysis [58,59,60,61,62, 64, 65, 67]. The overall estimated pooled rate of ESBL-EC acquisition was 72% (CI: 67–78%) (Fig. 2); the rate of ESBL-EC acquisition was quite consistent across the records. Heterogeneity was very low (I2 = 0.00%; p = 0.81). Subgroup analysis revealed that ESBL-EC acquisition was similar in records where the diagnoses were performed less than 10 years ago [71% (95% CI: 65–77%)] compared with ≥ 11 years ago [78% (95% CI: 65–90%)] (Fig. 2). The traveler's country of origin might also play a role in the acquisition of ESBL-EC after visiting India. Most of the travelers were from highly industrialized countries with Canada (80 cases) and Germany (69 cases) reporting the highest number of cases (Fig. 3).
Microorganisms causing TD
The etiology of diarrhea was not reported in most of the travelers with self-reported TD [41,42,43,44,45, 52, 53]. In instances where it was documented, however, the causative agents for TD in travelers to India were: Vibrio cholerae [39, 40, 46, 48, 49], Campylobacter [39, 51, 54], Salmonella Typhi [38], noroviruses [50], and multiple other microorganisms (including Escherichia coli, Giardia lamblia, shigella spp. and Campylobacter species) [47, 51]. Moreover, in some occasions despite thorough stool examination, the pathogen could not be detected. For instance, there was a negative report for the presence of cholera and other pathogens in the stool sample, even though the traveler showed typical diarrhea symptoms [68]. Co-pathogenicity was also common in cases with ESBL-EC, as seen in one traveler from Finland, who was concomitantly infected with enteropathogenic E. coli, Salmonella and Campylobacter [54].
Discussion
This study summarized the available evidence on TD and fecal colonization with ESBL-EC associated with an international travel to India. We also compared rates of ESBL-EC colonization in studies carried out less than 10 years ago compared with more than 10 years ago after 2002.
The overall pooled attack rate of TD in the reviewed studies reveals that an estimated 39% (around one-third) of the international travelers who visit India may experience TD. This estimate confirms that TD is an important health issue among the international travelers who visit India. To be better prepared, travelers should not disregard the potential risk of contracting TD. Furthermore, it is important to note that this estimate stems from calculations using records where data were collected between 2002 and 2014, which is more than seven years ago. Thus, this estimate might not reflect the current situation as hygienic conditions, economy, and public health programs [69] may have substantially improved in India. Similarly, the provision of safe water and adequate sanitation has been enhanced in most states and union territories by the Swachh Bharat (Clean India) Mission [70]. It is also possible that the TD pooled attack rate (39%) may be an underestimate in this study, as either under-reporting of TD is common or because of publication bias. Therefore, it is difficult to extrapolate this estimate to the current situation. Since only a few case reports in this study also provided data collected within the last five years [38, 55], it may be surmised that the COVID-19 pandemic has contributed to the lack of recent data on TD attack rate among international travelers to India.
The pooled attack rate of TD (39%) generated from this study falls within the general range of 30% to 70% as reported by the Centers for Disease Control and Prevention (CDC) [7]. It is also in line with a review by Steffen reporting that in destinations with high TD attack rates such as India, more than 20% of international travelers may experience TD [6]. A similar attack rate of TD (33%) has been reported among international travelers from developed countries visiting Thailand for 28 days [71], among backpackers in Southeast Asia (31%) [72], or again among international climbers in Nepal (36%) [73].
Findings from this review provide evidence that the etiology of TD in visitors to India is heterogenous: bacteria, viruses and parasites, and mixed pathogens have been reported. This suggests that multiple approaches are required for the confirmatory detection of these etiologic agents based on guidelines for TD prevention and treatment [74].
TD will continue to be a challenging health issue for travelers and clinicians. Our findings support the need for clinicians to be aware of the fact that bacteria such as Vibrio cholerae can be the cause of TD in travelers who experience acute watery diarrhea after returning from cholera-endemic countries [39, 40, 48, 49]. Hence, we can argue that not seriously considering this possibility may either delay the diagnosis or lead to misdiagnosis. Nevertheless, it is important to note that Vibrio cholerae is not a traditional etiology of TD [4, 8, 75].
A key finding of our review shows that the prevalence of ESBL-EC acquisition among visitors to India was 72%. The prevalence was similar between studies performed more than 10 years ago (78%) and less than 10 years ago (71%). This estimated prevalence of 72% is relatively high, but not surprising as ESBL’s endemicity is high in India. To put our observation into context, this may be a common occurrence in India: For instance, Hawser and colleagues have reported high rates of ESBL-EC acquisition among the local population in communities (79%) and hospitals (79%) in India [76]. In comparison with the data from other Asian countries, the rates of ESBL-EC acquisition in local communities vary between 51 to 71% in Southeast Asia (such as Vietnam, Thailand, and Laos) [77].
The ESBL-EC prevalence of 72% found in this study among visitors to India closely mirrors that reported in visitors to Egypt (71%) [78]. Moreover, one study found an ESBL-PE prevalence of 75% among Dutch travelers returning from southern Asia [16].
Our findings provide some evidence that international travel contributes to the acquisition of antimicrobial-resistant ESBL-EC. This has implications in public health because antimicrobial resistance may cause downstream infections [13, 79]. We should also note that some authors consider that because ESBL’s endemicity is wider, the contribution of international travel towards the spread of ESBL is relatively minor when compared with endemicity, which is much wider [80]. Most of the travelers with ESBL-EC colonization developed TD (a frequently reported risk factor of acquiring ESBL-EC). In general, for the international travelers, there are various risk factors for becoming colonized by multiresistant bacteria including ESBLs. These risk factors include travel destination, antibiotic use [11, 81] and TD [82]. Thus, these risk factors serve as a reminder for the judicious use of antibiotics, and suggests that there is a need to improve practices in antibiotic use when treating TD.
ESBL-EC colonization is usually transient in returning travelers but can persist for a year before the patient’s system fully recovers. Before clearance, ESBL-EC can be transmitted to other household members, with a probability of transmission rate at 12% [16]. This is plausible and thus a serious problem because most ESBL producing Enterobacteriaceae can lead to difficult-to-treat infections due to multi-drug resistance.
Although this study provides valuable insights into planning future studies in order to help understand TD and ESBL-EC acquisition among visitors to India, it has several limitations. First, our review was restricted to studies carried out in India. Our approach of only taking into account studies that separately provide rates for India excludes large studies reporting on ESBL-PE rates among travelers to South Asia. Therefore, we are now working on another meta-analysis study in order to reflect a true representation of the Indian subcontinent including only prospective studies.
Second, despite our wide search strategy, we could have missed some records and case reports. Case reports do not report all TD cases or ESBL colonization, and this study may also be vulnerable to publication bias. Lack of data precluded the quantitative analysis of travelers’ behaviors associated with ESBL-EC colonization. Behaviors such as antimicrobials consumption (especially fluoroquinolones) during travel increase the risk of ESBL-PE acquisition [12].
Third, because of caveats in the data stratified by variables, such as the region of India visited (rural or urban) in primary studies, destinations within India were not considered in the sensitivity analysis. These factors may need to be considered in future studies.
Conclusions
In conclusion, TD pooled attack rate and ESBL-EC acquisition among international travelers who experienced TD after visiting India were found to be high in this study. The etiology of TD was heterogeneous which includes a wide variety of bacteria, viruses, parasites, and mixed pathogens and therefore, their detection requires different types of methods. Summarized data provide practical implications in travel medicine. Firstly, our study highlights that travelers should be advised on TD to ensure that they do not disregard the potential risk of contracting TD and, as a result, be better prepared. Thus, pre-travel counseling is justified. Secondly, there is a need to remind health care practitioners that in the case of a returning traveler with multidrug resistant Escherichia coli, some antimicrobials such as cephalosporins and fluoroquinolones may be ineffective and therefore precautions need to be taken.
Availability of data and materials
All relevant data are within the manuscript and its supporting information files.
Abbreviations
- CDC:
-
Centers for Disease Control and Prevention
- COVID 19:
-
Coronavirus disease 2019
- EC:
-
Escherichia coli
- ESBL-EC:
-
Extended-spectrum beta-lactamase-producing Escherichia coli
- ESBL-PE:
-
Extended-spectrum beta-lactamase-producing Enterobacteriaceae
- PI-IBS:
-
Post-infectious irritable bowel syndrome
- PRISMA:
-
Preferred Reporting Items for a Systematic Review and Meta-analysis
- TD:
-
Traveler’s diarrhea
- SUTs:
-
States and union territories
References
Steffen R, Hill DR, DuPont HL. Traveler’s diarrhea: a clinical review. JAMA. 2015;313(1):71–80.
McFarland LV, Goh S. Are probiotics and prebiotics effective in the prevention of travellers’ diarrhea: A systematic review and meta-analysis. Travel Med Infect Dis. 2019;27:11–9.
DuPont HL. New insights and directions in travelers’ diarrhea. Gastroenterol Clin North Am. 2006;35(2):337–53 (viii-ix).
Leung KCA, Leung AMA, Wong HCA, Hon LK. Travelers’ Diarrhea: A Clinical Review. Recent Pat Inflammation Allergy Drug Discovery. 2019;13(1):38–48.
Jiang ZD, DuPont HL. Etiology of travellers’ diarrhea. J Travel Med. 2017;24(suppl_1):S13–6.
Steffen R. Emerging options for the management of travelers’ diarrhea. Gastroenterol Hepatol. 2018, 14(12): Supplement 8. https://www.gastroenterologyandhepatology.net/files/2018/12/gh1218sup8-1.pdf.
Connor BA: Connor BA, 2020. Part 2: traveler’s diarrhea. Brunette GW, Nemhauser JB, eds. CDC–Yellow Book 2020: Health Information for International Travel. Atlanta, GA: Oxford University Press, 114–120. In., edn.; 2020.
Sanders JW, Riddle MS, Taylor DN, DuPont HL: 18 - Epidemiology of Travelers' Diarrhea. In: Travel Medicine (Fourth Edition). edn. Edited by Keystone JS, Kozarsky PE, Connor BA, Nothdurft HD, Mendelson M, Leder K. London: Elsevier; 2019: 187–198.
Connor BA, Riddle MS. Post-infectious sequelae of travelers’ diarrhea. J Travel Med. 2013;20(5):303–12.
Connor BA. Post-Infectious Sequelae of Travelers’ Diarrhea: Reactive Arthritis, Guillain-Barré Syndrome, and Irritable Bowel Syndrome. Current Tropical Medicine Reports. 2016;3(3):102–7.
Kantele A, Laaveri T, Mero S, Vilkman K, Pakkanen SH, Ollgren J, Antikainen J, Kirveskari J. Antimicrobials increase travelers’ risk of colonization by extended-spectrum betalactamase-producing Enterobacteriaceae. Clin Infect Dis. 2015;60(6):837–46.
Wuerz TC, Kassim SS, Atkins K. Acquisition of extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBL-PE) carriage after exposure to systemic antimicrobials during travel: Systematic review and meta-analysis. Travel Med Infect Dis. 2020;37:101823.
Chen LH, Han PV, Wilson ME, Stoney RJ, Jentes ES, Benoit C, Ooi WW, Barnett ED, Hamer DH. Self-reported illness among Boston-area international travelers: A prospective study. Travel Med Infect Dis. 2016;14(6):604–13.
Rasko DA. Changes in microbiome during and after travellers’ diarrhea: what we know and what we do not. J Travel Med. 2017;24(suppl_1):S52-s56.
von Sonnenburg F, Tornieporth N, Waiyaki P, Lowe B, Peruski LF, DuPont HL, Mathewson JJ, Steffen R. Risk and aetiology of diarrhoea at various tourist destinations. Lancet. 2000;356(9224):133–4.
Arcilla MS, van Hattem JM, Haverkate MR, Bootsma MCJ, van Genderen PJJ, Goorhuis A, Grobusch MP, Lashof AMO, Molhoek N, Schultsz C, et al. Import and spread of extended-spectrum beta-lactamase-producing Enterobacteriaceae by international travellers (COMBAT study): a prospective, multicentre cohort study. Lancet Infect Dis. 2017;17(1):78–85.
Kantele A, Laaveri T, Mero S, Hakkinen IMK, Kirveskari J, Johnston BD, Johnson JR. Despite Predominance of Uropathogenic/Extraintestinal Pathotypes Among Travel-acquired Extended-spectrum beta-Lactamase-producing Escherichia coli, the Most Commonly Associated Clinical Manifestation Is Travelers’ Diarrhea. Clin Infect Dis. 2020;70(2):210–8.
Steffen R. Epidemiology of travellers’ diarrhea. J Travel Med. 2017;24(suppl_1):S2–5.
Moher D, Liberati A, Tetzlaff J, Altman DG, Grp P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med. 2009;151(4):264-W264.
Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23(2):60–3.
Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72(1):39.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Karanika S, Karantanos T, Arvanitis M, Grigoras C, Mylonakis E. Fecal Colonization With Extended-spectrum Beta-lactamase-Producing Enterobacteriaceae and Risk Factors Among Healthy Individuals: A Systematic Review and Metaanalysis. Clin Infect Dis. 2016;63(3):310–8.
Nuesch-Inderbinen M, Abgottspon H, Sagesser G, Cernela N, Stephan R. Antimicrobial susceptibility of travel-related Salmonella enterica serovar Typhi isolates detected in Switzerland (2002–2013) and molecular characterization of quinolone resistant isolates. BMC Infect Dis. 2015;15:212.
Kharat VB, Ahmed M, Jiang ZD, Riddle MS, DuPont HL. Colonization Factors in Enterotoxigenic Escherichia coli Strains in Travelers to Mexico, Guatemala, and India Compared with Children in Houston. Texas Am J Trop Med Hyg. 2017;96(1):83–7.
Ingle DJ, Nair S, Hartman H, Ashton PM, Dyson ZA, Day M, Freedman J, Chattaway MA, Holt KE, Dallman TJ. Informal genomic surveillance of regional distribution of Salmonella Typhi genotypes and antimicrobial resistance via returning travellers. PLoS Negl Trop Dis. 2019;13(9):e0007620.
Ouyang-Latimer J, Jafri S, VanTassel A, Jiang ZD, Gurleen K, Rodriguez S, Nandy RK, Ramamurthy T, Chatterjee S, McKenzie R, et al. In vitro antimicrobial susceptibility of bacterial enteropathogens isolated from international travelers to Mexico, Guatemala, and India from 2006 to 2008. Antimicrob Agents Chemother. 2011;55(2):874–8.
Greenwood Z, Black J, Weld L, O’Brien D, Anat D, Leder K, Von Sonnenburg F, Pandey P, Schwartz E, Connor BA, et al. Gastrointestinal infection among international travelers globally. J Travel Med. 2008;15(4):221–8.
Peirano G, Schreckenberger PC, Pitout JD. Characteristics of NDM-1-producing Escherichia coli isolates that belong to the successful and virulent clone ST131. Antimicrob Agents Chemother. 2011;55(6):2986–8.
Freeman JT, McBride SJ, Heffernan H, Bathgate T, Pope C, Ellis-Pegler RB. Community-onset genitourinary tract infection due to CTX-M-15-Producing Escherichia coli among travelers to the Indian subcontinent in New Zealand. Clin Infect Dis. 2008;47(5):689–92.
Tarantola A, Ioos S, Rotureau B, Paquet C, Quilici ML, Fournier JM. Retrospective analysis of the cholera cases imported to France from 1973 to 2005. J Travel Med. 2007;14(4):209–14.
Peirano G, Laupland KB, Gregson DB, Pitout JDD. Colonization of Returning Travelers With CTX-M-Producing Escherichia coli. J Travel Med. 2011;18(5):299–303.
Pitzurra R, Steffen R, Tschopp A, Mutsch M. Diarrhoea in a large prospective cohort of European travellers to resource-limited destinations. BMC Infect Dis. 2010;10:231.
Kennedy K, Collignon P. Colonisation with Escherichia coli resistant to “critically important” antibiotics: a high risk for international travellers. Eur J Clin Microbiol Infect Dis. 2010;29(12):1501–6.
Dhanji H, Patel R, Wall R, Doumith M, Patel B, Hope R, Livermore DM, Woodford N. Variation in the genetic environments of bla(CTX-M-15) in Escherichia coli from the faeces of travellers returning to the United Kingdom. J Antimicrob Chemoth. 2011;66(5):1005–12.
Steffen R, Tornieporth N, Clemens SA, Chatterjee S, Cavalcanti AM, Collard F, De Clercq N, DuPont HL, von Sonnenburg F. Epidemiology of travelers’ diarrhea: details of a global survey. J Travel Med. 2004;11(4):231–7.
Jiang ZD, Lowe B, Verenkar MP, Ashley D, Steffen R, Tornieporth N, von Sonnenburg F, Waiyaki P, DuPont HL. Prevalence of enteric pathogens among international travelers with diarrhea acquired in Kenya (Mombasa), India (Goa), or Jamaica (Montego Bay). J Infect Dis. 2002;185(4):497–502.
Shin E, Park J, Jeong HJ, Park AK, Na K, Lee H, Chun JH, Hwang KJ, Kim CJ, Kim J. Emerging high-level ciprofloxacin-resistant Salmonella enterica serovar typhi haplotype H58 in travelers returning to the Republic of Korea from India. PLoS Negl Trop Dis. 2021;15(3):e0009170.
Pougnet L, Pougnet R, Voarino A, Sapin J, Drouillard I, Quilici ML, Desideri-Vaillant C. Cholera in Brest, France. Ann Biol Clin. 2018;76(1):107–10.
Tarantola A, Vaucel J, Laviolle C, Quilici ML, Thiolet JM, Fournier JM, Grp IM. A cluster of Vibrio cholerae O1 infections in French travelers to Rajasthan (India), May 2006. J Travel Med. 2008;15(4):273–7.
Olanwijitwong J, Piyaphanee W, Poovorawan K, Lawpoolsri S, Chanthavanich P, Wichainprasast P, Tantawichien T. Health problems among Thai tourists returning from India. J Travel Med. 2017;24(4):tax013.
Kuenzli E, Juergensen D, Kling K, Jaeger VK, DeCrom S, Steffen R, Widmer AF, Battegay M, Hatz C, Neumayr A. Previous exposure in a high-risk area for travellers' diarrhoea within the past year is associated with a significant protective effect for travellers' diarrhoea: a prospective observational cohort study in travellers to South Asia. J Travel Med. 2017;24(5):tax056.
Schindler VM, Jaeger VK, Held L, Hatz C, Buhler S. Travel style is a major risk factor for diarrhoea in India: a prospective cohort study. Clin Microbiol Infect. 2015;21(7):676 (e671-674).
Stoney RJ, Han PV, Barnett ED, Wilson ME, Jentes ES, Benoit CM, MacLeod WB, Hamer DH, Chen LH, Network BATM. Travelers’ Diarrhea and Other Gastrointestinal Symptoms among Boston-Area International Travelers. Am J Trop Med Hyg. 2017;96(6):1388–93.
Mackaness CA, Osborne A, Verma D, Templer S, Weiss MJ, Knouse MC. A quality improvement initiative using a novel travel survey to promote patient-centered counseling. J Travel Med. 2013;20(4):237–42.
Kuleshov KV, Vodop’ianov SO, Dedkov VG, Markelov ML, Deviatkin AA, Kruglikov VD, Vodop’ianov AS, Pisanov RV, Mazrukho AB, Titova SV, et al. Travel-Associated Vibrio cholerae O1 El Tor. Russia Emerg Infect Dis. 2016;22(11):2006–8.
Steffen R, Cramer JP, Burchard G, Jelinek T, Schwarz U, Ramdas P, Chatterjee S, Jiang ZD, DuPont HL, Dewasthaly S, et al. Efficacy of a travelers’ diarrhea vaccine system in travelers to India. J Travel Med. 2013;20(6):374–9.
Ismail H, Smith AM, Archer BN, Tau NP, Sooka A, Thomas J, Prinsloo B, Keddy KH. Group for Enteric R, Meningeal Disease Surveillance in South A: Case of imported Vibrio cholerae O1 from India to South Africa. J Infect Dev Ctries. 2012;6(12):897–900.
Neghina R, Neghina AM. A case of imported cholera in Romania in 2009. Infect Dis Clin Pract. 2012;20:148–9.
Koo HL, Ajami NJ, Jiang ZD, Neill FH, Atmar RL, Ericsson CD, Okhuysen PC, Taylor DN, Bourgeois AL, Steffen R, et al. Noroviruses as a cause of diarrhea in travelers to Guatemala, India, and Mexico. J Clin Microbiol. 2010;48(5):1673–6.
Jiang ZD, Dupont HL, Brown EL, Nandy RK, Ramamurthy T, Sinha A, Ghosh S, Guin S, Gurleen K, Rodrigues S, et al. Microbial etiology of travelers’ diarrhea in Mexico, Guatemala, and India: importance of enterotoxigenic Bacteroides fragilis and Arcobacter species. J Clin Microbiol. 2010;48(4):1417–9.
Tillett E, Loosemore M. Setting standards for the prevention and management of travellers’ diarrhoea in elite athletes: an audit of one team during the Youth Commonwealth Games in India. Brit J Sport Med. 2009;43(13):1045–8.
Hillel O, Potasman I. Correlation between adherence to precautions issued by the WHO and diarrhea among long-term travelers to India. J Travel Med. 2005;12(5):243–7.
Kantele A, Laaveri T. Extended-spectrum beta-lactamase-producing strains among diarrheagenic Escherichia coli-prospective traveler study with literature review. J Travel Med. 2022;29(1):taab042. https://doi.org/10.1093/jtm/taab042.
Mellon G, Turbett SE, Worby C, Oliver E, Walker AT, Walters M, Kelly P, Leung DT, Knouse M, Hagmann S, et al. Acquisition of Antibiotic-Resistant Bacteria by U.S. International Travelers N Engl J Med. 2020;382(14):1372–4.
Weisenberg SA, Mediavilla JR, Chen L, Alexander EL, Rhee KY, Kreiswirth BN, Jenkins SG. Extended spectrum beta-lactamase-producing Enterobacteriaceae in international travelers and non-travelers in New York City. PLoS ONE. 2012;7(9):e45141.
Islam S. High Rates of ESBL-producing Escherichia coli in Young Children Who Traveled Recently to India. Pediatr Infect Dis J. 2012;31(10):1103–1103.
Miranda IB, Ignatius R, Pfuller R, Friedrich-Janicke B, Steiner F, Paland M, Dieckmann S, Schaufler K, Wieler LH, Guenther S et al. High carriage rate of ESBL-producing Enterobacteriaceae at presentation and follow-up among travellers with gastrointestinal complaints returning from India and Southeast Asia. J Travel Med. 2016;23(2):tav024.
Lubbert C, Straube L, Stein C, Makarewicz O, Schubert S, Mossner J, Pletz MW, Rodloff AC. Colonization with extended-spectrum beta-lactamase-producing and carbapenemase-producing Enterobacteriaceae in international travelers returning to Germany. Int J Med Microbiol. 2015;305(1):148–56.
Reuland EA, Sonder GJB, Stolte I, al Naiemi N, Koek A, Linde GB, van de Laar TJW, Vandenbroucke-Grauls CMJE, van Dam AP. Travel to Asia and traveller's diarrhoea with antibiotic treatment are independent risk factors for acquiring ciprofloxacin-resistant and extended spectrum beta-lactamase-producing Enterobacteriaceae-a prospective cohort study. Clin Microbiol Infect. 2016;22(8):731.e1–7.
Yaita K, Aoki K, Suzuki T, Nakaharai K, Yoshimura Y, Harada S, Ishii Y, Tachikawa N. Epidemiology of extended-spectrum beta-lactamase producing Escherichia coli in the stools of returning Japanese travelers, and the risk factors for colonization. PLoS ONE. 2014;9(5):e98000.
Lausch KR, Fuursted K, Larsen CS, Storgaard M. Colonisation with multi-resistant Enterobacteriaceae in hospitalised Danish patients with a history of recent travel: A cross-sectional study. Travel Med Infect Di. 2013;11(5):320–3.
Guiral E, Mendez-Arancibia E, Soto SM, Salvador P, Fabrega A, Gascon J, Vila J. CTX-M-15-producing enteroaggregative Escherichia coli as cause of travelers’ diarrhea. Emerg Infect Dis. 2011;17(10):1950–3.
Tangden T, Cars O, Melhus A, Lowdin E. Foreign travel is a major risk factor for colonization with Escherichia coli producing CTX-M-type extended-spectrum beta-lactamases: a prospective study with Swedish volunteers. Antimicrob Agents Chemother. 2010;54(9):3564–8.
Tham J, Odenholt I, Walder M, Brolund A, Ahl J, Melander E. Extended-spectrum beta-lactamase-producing Escherichia coli in patients with travellers’ diarrhoea. Scand J Infect Dis. 2010;42(4):275–80.
Laupland KB, Church DL, Vidakovich J, Mucenski M, Pitout JD. Community-onset extended-spectrum beta-lactamase (ESBL) producing Escherichia coli: importance of international travel. J Infect. 2008;57(6):441–8.
Peirano G, Gregson DB, Kuhn S, Vanderkooi OG, Nobrega DB, Pitout JDD. Rates of colonization with extended-spectrum beta-lactamase-producing Escherichia coli in Canadian travellers returning from South Asia: a cross-sectional assessment. CMAJ Open. 2017;5(4):E850–5.
Zwar NA, Torda A. Investigation of diarrhoea in a traveller just returned from India. BMJ. 2011;342:d2978.
Singh A, Vellakkal S. Impact of public health programs on maternal and child health services and health outcomes in India: A systematic review. Soc Sci Med. 2021;274:113795.
Behera MR, Pradhan HS, Behera D, Jena D, Satpathy SK. Achievements and challenges of India’s sanitation campaign under clean India mission: A commentary. J Educ Health Promot. 2021;10:350.
Sharma C, Poovorawan K, Piyaphanee W, Soonthornworasiri N, Angsuwatcharakon P, Phumratanaprapin W, Leowattana W, Wilairatana P. Incidence of Travelers’ Diarrhea among Adult Foreign Travelers in Thailand: A Prospective Study. Am J Trop Med Hyg. 2020;102(5):1009–15.
Piyaphanee W, Kusolsuk T, Kittitrakul C, Suttithum W, Ponam T, Wilairatana P. Incidence and impact of travelers’ diarrhea among foreign backpackers in Southeast Asia: a result from Khao San road. Bangkok J Travel Med. 2011;18(2):109–14.
Murdoch DR. Symptoms of infection and altitude illness among hikers in the Mount Everest region of Nepal. Aviat Space Environ Med. 1995;66(2):148–51.
Riddle MS, Connor BA, Beeching NJ, DuPont HL, Hamer DH, Kozarsky P, Libman M, Steffen R, Taylor D, Tribble DR, et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report. J Travel Med. 2017;24(suppl_1):S57–74.
Zuckerman JN, Rombo L, Fisch A. The true burden and risk of cholera: implications for prevention and control. Lancet Infect Dis. 2007;7(8):521–30.
Hawser SP, Bouchillon SK, Hoban DJ, Badal RE, Hsueh PR, Paterson DL. Emergence of high levels of extended-spectrum-beta-lactamase-producing gram-negative bacilli in the Asia-Pacific region: data from the Study for Monitoring Antimicrobial Resistance Trends (SMART) program, 2007. Antimicrob Agents Chemother. 2009;53(8):3280–4.
Nakayama T, Ueda S, Huong BT, le Tuyen D, Komalamisra C, Kusolsuk T, Hirai I, Yamamoto Y. Wide dissemination of extended-spectrum beta-lactamase-producing Escherichia coli in community residents in the Indochinese peninsula. Infect Drug Resist. 2015;8:1–5.
Laaveri T, Vlot JA, van Dam AP, Hakkinen HK, Sonder GJB, Visser LG, Kantele A. Extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBL-PE) among travellers to Africa: destination-specific data pooled from three European prospective studies. BMC Infect Dis. 2018;18(1):341.
Angue M, Allou N, Belmonte O, Lefort Y, Lugagne N, Vandroux D, Montravers P, Allyn J. Risk Factors for Colonization With Multidrug-Resistant Bacteria Among Patients Admitted to the Intensive Care Unit After Returning From Abroad. J Travel Med. 2015;22(5):300–5.
Adler A, Katz DE, Marchaim D. The Continuing Plague of Extended-Spectrum beta-Lactamase Producing Enterbacterales Infections: An Update. Infect Dis Clin North Am. 2020;34(4):677–708.
Khawaja T, Kirveskari J, Johansson S, Väisänen J, Djupsjöbacka A, Nevalainen A, Kantele A. Patients hospitalized abroad as importers of multiresistant bacteria-a cross-sectional study. Clin Microbiol Infect. 2017;23(9):673.e671-673.e678.
Kantele A, Mero S, Kirveskari J, Lääveri T. Increased Risk for ESBL-Producing Bacteria from Co-administration of Loperamide and Antimicrobial Drugs for Travelers’ Diarrhea. Emerg Infect Dis. 2016;22(1):117–20.
Acknowledgements
We would like to thank Barnabas Martin and Matthew McLaughlin for editing our manuscript, and Mansongi Biyela Carine for her assistance in preparing this manuscript.
Funding
This study was supported by the Program of the Japan Initiative for Global Research Network on Infectious Diseases (J-GRID), JP22wm0125004, from Ministry of Education, Culture, Sports, Science and Technology in Japan (MEXT), and Japan Agency for Medical Research and Development (AMED). The funders had no role in its study design, data collection and analysis, decision to publish, or preparation of the manuscript. All authors had full access to all the data in the review process, and the corresponding author had the final responsibility in deciding to submit this article for publication.
Author information
Authors and Affiliations
Contributions
BAM and SIM: study conception and its design; BAM and KK: data collection, analysis and interpretation; BAM: wrote the first draft of the manuscript; KK: Commented on an early version of the manuscript; KK, AO, KO and SIM: revised the manuscript for important academic content. SIM: supervised this work. All authors have read and agreed to this version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No ethical approval was necessary for this study because it is a review.
Consent for publication
Not applicable for this study because it is a review.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix Figure 1.
PRISMA diagram summarizing evidence search and study selection.
Additional file 2: Supplementary Table 1.
Characteristics of reviewed records.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Muzembo, B.A., Kitahara, K., Ohno, A. et al. Colonization with extended-spectrum beta-lactamase-producing Escherichia coli and traveler’s diarrhea attack rates among travelers to India: a systematic review and meta-analysis. Trop Dis Travel Med Vaccines 8, 22 (2022). https://doi.org/10.1186/s40794-022-00179-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40794-022-00179-1