Abstract
Background
Typhoid fever is an acute, invasive, and potentially fatal systemic infection caused by Salmonella enterica subspecies enterica serotype Typhi (S. Typhi). Drug resistance to antimicrobials such as ciprofloxacin is emerging in developing countries, threatening the efficacy of treatment of patients in endemic regions as well as of travellers returning from these countries.
Methods
We compared the antimicrobial resistance profiles of 192 S. Typhi isolated from patients over a time span of twelve years. Susceptibility testing was done by the disk diffusion method. A representative selection of isolates (n = 41) was screened by PCR for mutations in the quinolone resistance-determining regions (QRDRs) of the gyrA and parC genes and all 192 isolates were screened for plasmid-mediated quinolone resistance (PMQR) genes. Multilocus sequence typing (MLST) was used to investigate the sequence type of isolates from patients with a known history of international travel.
Results
Resistance rates for nalidixic acid increased from 20 % to 66.7 % between 2002 and 2013. Resistance to ciprofloxacin was detected in 55.6 % of the isolates by 2013. Ciprofloxacin resistance was predominantly associated with the triple substitutions Ser83 → Phe and Asp87 → Asn in GyrA and Ser80 → Ile in ParC. The plasmid-mediated resistance gene qnrS1 was detected in two isolates. Sequence type ST1 was associated with the Indian subcontinent, while ST2 was distributed internationally. Multidrug resistance was noted for 11.5 % of the isolates.
Conclusions
Fluoroquinolone resistant S. Typhi constitute a serious public health concern in endemic areas as well as in industrialized countries. Increased surveillance of global patterns of antimicrobial resistance is necessary and the control of resistant strains is of the utmost importance to maintain treatment options.
Similar content being viewed by others
Background
Salmonella enterica subspecies enterica serovar Typhi (S. Typhi) is a human-specific etiological agent of an acute, invasive, and potentially fatal systemic infection also known as typhoid fever [1]. The disease is a serious public health problem in developing countries with the Indian subcontinent (India, Pakistan, Afghanistan, Nepal and Bangladesh) representing a geographic area of intense disease activity [2]. In industrialized countries typhoid fever is rare and mainly associated with travel to high-risk destinations [3, 4]. In the 1990ies, antimicrobial therapy became problematic in endemic areas due to multi-drug resistant (MDR) S. Typhi, rendering chloramphenicol, trimethoprim and ampicillin, which were the drugs used as first-line treatment ineffective. Currently, fluoroquinolones such as ciprofloxacin are recommended by the WHO [5], as they are the most effective orally active, inexpensive and well-tolerated drugs for the treatment of typhoid fever [6]. Hence, the worrisome signs of increasing resistance to this class of antimicrobials represent a challenge for effective control and management of typhoid fever, especially in endemic countries. Resistance is mainly due to the accumulation of mutations in the quinolone resistance-determining regions (QRDRs) of DNA gyrase and topoisomerase IV genes (target site alterations). Additionally, plasmid-mediated quinolone resistance (PMQR) confer a form of reduced susceptibility which is thought to promote the accumulation of the target site mutations [7]. PMQR include the Qnr families of pentapeptide repeat proteins encoded by qnrA, qnrB, qnrC qnrD and qnrS, [8, 9] and [10]. The majority of mutations in quinolone resistant S. Typhi have been detected within the quinolone resistance-determining region (QRDR) of the DNA gyrase gene gyrA and in the topoisomerase gene parC [11]. Primary mutations in target site genes generate resistance to the quinolone antimicrobial nalidixic acid, making it useful as a surrogate marker of decreased susceptibility to fluoroquinolones [12], as resistance to nalidixic acid correlates with decreased susceptibility to ciprofloxacin and hence to potential treatment failure [13–15].
The aim of this study was to describe the antimicrobial susceptibility profiles of S. Typhi isolated from patients over a time span of twelve years. In a selection of isolates, the presence of point mutations in the genes gyrA and parC that encode the quinolone targets was determined. The clonal relationship of isolates known to be associated with international travel was assessed.
Methods
Clinical isolates
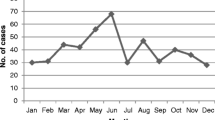
Between 2002 and 2013, 203 S. Typhi isolates were sent to the National Centre for Enteropathogenic Bacteria and Listeria (NENT), Switzerland, for final serological identification and strain collection. All samples had been submitted by hospitals or primary diagnostic laboratories located in Switzerland. The number of collected strains varied from 10 to 24 per annum, with a median of 16. Patients’ data was anonymized. Studies performed with such strains had previously been declared unobjectionable by the ethics commission of the Canton of Zürich, Switzerland (declaration KEK Stv.-Nr. 19/12). For the study, only one isolate per patient was selected. Isolates from family members were considered separate samples (10 samples from 4 families). Of the 203 collected isolates, 192 met these criteria for further analysis.
Antimicrobial susceptibility tests
Susceptibility testing was performed for the 192 isolates using the Kirby Bauer disk diffusion method and the antimicrobials nalidixic acid, ciprofloxacin, ampicillin, amoxicillin/clavulanic acid, cephalotin, cefotaxime, gentamicin, kanamycin, streptomycin, tetracycline, sulfamethoxazole, trimethoprim and chloramphenicol (Becton Dickinson, Heidelberg, Germany). Results were interpreted according to the Clinical and Laboratory Standards Institute (CLSI) [16]. Hereby, breakpoints for ciprofloxacin are ≥31 mm (susceptible), 21–30 mm (intermediate) and ≤20 mm (resistant).
Multidrug-resistance (MDR) was defined as resistance to conventional antityphoid drugs ampicillin, trimethoprim-sulfamethoxazole and chloramphenicol (13).
Molecular characterization of quinolone resistance genes
DNA was extracted using a standard heat lysis protocol. In brief, 5 bacterial colonies were resuspended in 450 μl lysis buffer containing 0.1 M Tris pH 8.5, 0.05 % Tween-20 and 240 μg/ml proteinase K. Samples were incubated at 60 °C for 60′, followed by 97 °C for 15′. Lysates were centrifuged for 10″ at 13,200 rpm and 5 μl of the supernatant were used for PCR.
A subset of 41 isolates eliciting various resistance patterns and representing different years of isolation was subjected to PCR-based detection of mutations in the quinolone resistance-determining regions (QRDRs) of the gyrA and parC genes, using amplification primers described previously [17]. All 192 isolates were screened for plasmid-mediated quinolone resistance (PMQR) genes using primers described previously for qnrA [17, 18], qnrB [19], qnrC [20], qnrD [21], and qnrS [17]. Custom sequencing was performed by Microsynth (Balgach, Switzerland) and nucleotide sequences were analysed with CLC Main Workbench 6.6.1. For database searches the BLASTN program of NCBI (http://www.ncbi.nlm.nih.gov/blast/) was used.
Multilocus sequence typing
Multilocus sequence typing (MLST) [22] was used to investigate the sequence type of 26 isolates from patients with a known history of international travel. These isolates were randomly selected from 83 travel-associated isolates. Internal fragments of the seven housekeeping genes aroC, dnaN, hemD, hisD, purE, sucA and thrA were amplified by PCR. Sequencing of the amplification products was performed by Microsynth (Balgach). Sequence types (ST) were assigned in accordance with the Salmonella enterica MLST Database http://mlst.ucc.ie/mlst/dbs/Senterica.
Results and discussion
A detailed overview of the 192 S. Typhi isolates analysed in this study, together with anamnestic data and any travel information of the patients is given in Additional file 1: Table S1. The majority of the strains (96 %) were isolated from blood or stool. Patient median age was 26 years (range <1–74 years), ninety-five (49.5 %) were female and 21.4 % were children (<16 years). Information on the travel background was availabe for 83 patients. Thereof, the three main countries involved were India with 41 patients (49.4 %), Pakistan with 7 (8.4 %) and Bangladesh with 4 (4.8 %) patients.
The rate of full susceptibility of S. Typhi to the antimicrobials tested in this study declined from 80 % in 2002 to 28 % in 2013. This decrease was mainly due to the emergence of isolates with resistance to nalidixic acid, with resistance rates increasing from 20 to 66.7 % during the same period. Ciprofloxacin resistance rose from 0 to 55.6 %, albeit variably (Table 1). Multidrug-resistance (MDR), and especially resistance to former drugs of first choice ampicillin, trimethoprim-sulfamethoxazole and chloramphenicol [13], was observed variably (0–25 %, Table 1). Resistance to ampicillin-clavulanic acid and cephalotin was found in one and 8 isolates, respectively, while streptomycin and tetracycline resistance was detected in 24 (12.5 %) and 15 (7.8 %) isolates, respectively (Additional file 1: Table S1).
In total, 113 (58.9 %) of the isolates were resistant to nalidixic acid. Of the 36 analysed nalidixic acid-resistant isolates, 35 (97 %) contained a substitution in Ser83 of GyrA, whereby 27 (75 %) contained the amino acid substitution Ser83 → Phe and the remaining 8 carried the mutation Ser83 → Tyr (Table 2). Only one nalidixic acid and ciprofloxacin resistant isolate (N10-1839, see Additional file 1: Table S1) tested negative for substitutions in GyrA. This clearly illustrates the predominance of gyrA mutations in quinolone resistant S. Typhi.
In total, 39 (20.3 %) of the isolates were resistant to ciprofloxacin. The first ciprofloxacin-resistant strain from the collection described in this study was isolated in 2004 from a traveller from Cambodia (isolate 1736–04) and was associated with a Ser83 → Phe in GyrA and a zone diameter of 19 mm in the disk diffusion test for ciprofloxacin (Additional file 1: Table S1 and Table 2). One ciprofloxacin-resistant isolate contained an additional Glu84 → Gly substitution in ParC (isolate 1715–06, see Additional file 1: Table S1). In the disk diffusion test, this substitution was associated with a zone diameter of 14 mm (Table 2). One further isolate (1751–08) contained a Glu84 → Lys substitution in ParC. This substitution has been described previously in two ciprofloxacin-resistant isolates from Bangladesh [23]. However, those isolates both contained the two additional substitutions Trp106 → Gly and Tyr128 → Asp in ParC. Since isolate 1751–08 was categorized as intermediately susceptible to ciprofloxacin (zone diameter 21 mm), the Glu84 → Lys substitution in ParC does not appear to be crucial for ciprofloxacin resistance.
Ciprofloxacin-resistant strains isolated since 2010 (n = 23) all contained the combination of Ser83 → Phe and Asp87 → Asn in GyrA as well as the Ser80 → Ile substitution in ParC and were associated with decreased zone diameters of 6–11 mm in the disk diffusion tests for ciprofloxacin (Table 2). This genotype appears to be becoming more frequent compared to previous reports [11]. Although no gyrB or parE gene mutations were analysed in this study, the data presented here indicate these particular substitutions in GyrA and ParC may be considered a major quinolone resistance mechanism in S. Typhi. Mutations in gyrA are recognized to be predominant in nalidixic acid resistant S. Typhi [24, 25]. Increased efflux pump-mediated mechanisms, which are observed in other fluoroquinolone-resistant Salmonella [26], have very recently been reported to be absent in S. Typhi [27], further highlighting the importance of target-site mutations. Furthermore, a recent study by Baker et al. [24] has shown that mutations in the target genes gyrA and parC correlate with an increase of intrinsic fitness in S. Typhi. This indicates that the quinolone resistance genotypes observed in our study may continue to circulate even in the absence of antimicrobial selective pressure.
The plasmid-mediated quinolone resistance gene qnrS1 was found in a fully susceptible isolate from 2009 and in a ciprofloxacin-resistant isolate from 2010 (isolates N09-2035 and N10-2349, respectively, see Additional file 1: Table S1). No other PMQR genes were detected in any of the isolates. There are few studies that describe PMQR genes in S. Typhi and our findings indicate that they may play a minor role in quinolone resistance of S. Typhi. The qnrS gene has to our knowledge been reported once in an isolate from the Democratic Republic of the Congo [28], whereas in quinolone-resistant S. Typhi isolates from India the qnrB gene predominates [29].
On account of travel histories, 54 isolates (28 %) were demonstrably associated with the Indian subcontinent (Additional file 1: Table S1). However, this number is possibly understated, due to missing travel information for many of the patients. This highlights the need to improve travel history reporting within the healthcare system in order to get a more precise picture of the association of distinct strains with distinct regions worldwide. Multilocus sequence typing of S. Typhi is limited by the fact that it discriminates 2 sequence types only. Nevertheless, typing assigned 15 isolates to ST1, of which 12 (80 %) were associated with the Indian subcontinent. By contrast, the origins of the 14 isolates assigned to ST2 were more widely dispersed and included Southeast Asia (4 isolates; 28.6 %), Africa (3 isolates; 21.4 %), Mexico (4 isolates; 29 %) and South America (1 isolate; 7.1 %). This finding is consistent with observations of Dahiya et al. [30] and indicates that ST2 may be circulating internationally, while ST1 mainly persists in the Indian subcontinent.
Conclusions
This study presents an overview over the development of antimicrobial resistance profiles of S. Typhi over the last 12 years and provides molecular characteristics of nalidixic acid- and ciprofloxacin-resistant S. Typhi isolated in that time span. Since fluoroquinolones are currently the mainstay of the treatment of typhoid fever, resistance in S. Typhi threatens to limit therapeutic options and constitutes a serious public health concern in endemic areas as well as in industrialized countries. Increased surveillance of global patterns of antimicrobial resistance is necessary and the control of resistant strains is of the utmost importance.
This study adds to the current knowledge about the global circulation of quinolone-resistant S. Typhi and their associated mechanisms of resistance.
Ethics statement
The Zurich Cantonal Ethics Commission evaluated the present study, and declared it legally and ethically unobjectionable.
References
Kaur J, Jain SK. Role of antigens and virulence factors of Salmonella enterica serovar Typhi in its pathogenesis. Microbiol Res. 2012;167:199–210.
Kothari A, Pruthi A, Chugh TD. The burden of enteric fever. J Infect Dev Ctries. 2008;2:253–9.
Hassing RJ, Goessens WH, Mevius DJ, van Pelt W, Mouton JW, Verbon A, et al. Decreased ciprofloxacin susceptibility in Salmonella Typhi and Paratyphi infections in ill-returned travellers: the impact on clinical outcome and future treatment options. Eur J Clin Microbiol Infect Dis. 2013;32:1295–301.
Keller A, Frey M, Schmid H, Steffen R, Walker T, Schlagenhauf P. Imported typhoid fever in Switzerland, 1993 to 2004. J Travel Med. 2008;15:248–51.
World Health Organization (WHO). Background document: the diagnosis, treatment, and prevention of typhoid fever. Geneva, Switzerland: WHO; 2003.
Parry CM, Hien TT, Dougan G, White NJ, Farrar JJ. Typhoid fever. N Engl J Med. 2002;347:1770–82.
Strahilevitz J, Jacoby GA, Hooper DC, Robicsek A. Plasmid-mediated quinolone resistance: a multifaceted threat. Clin Microbiol Rev. 2009;22:664–89.
Martínez-Martínez L, Pascual A, Jacoby GA. Quinolone resistance from a transferable plasmid. Lancet. 1998;351:797–9.
Jacoby GA, Walsh KE, Mills DM, Walker VJ, Oh H, Robicsek A, et al. qnrB, another plasmid-mediated gene for quinolone resistance. Antimicrob Agents Chemother. 2006;50:1178–82.
Hata M, Suzuki M, Matsumoto M, Takahashi M, Sato K, Ibe S, et al. Cloning of a novel gene for quinolone resistance from a transferable plasmid in Shigella flexneri 2b. Antimicrob Agents Chemother. 2005;49:801–3.
Parry CM, Thuy CT, Dongol S, Karkey A, Vinh H, Chinh NT, et al. Suitable disk antimicrobial susceptibility breakpoints defining Salmonella enterica serovar Typhi isolates with reduced susceptibility to fluoroquinolones. Antimicrob Agents Chemother. 2010;54:5201–8.
Hakanen A, Kotilainen P, Jalava J, Siitonen A, Huovinen P. Detection of decreased fluoroquinolone susceptibility in Salmonellas and validation of nalidixic acid screening test. J Clin Microbiol. 1999;37:3572–7.
Lynch MF, Blanton EM, Bulens S, Polyak C, Vojdani J, Stevenson J, et al. Typhoid fever in the United States, 1999–2006. JAMA. 2009;302:859–65.
Cooke FJ, Wain J. The emergence of antibiotic resistance in typhoid fever. Travel Med Infect Dis. 2004;2:67–74.
Crump JA, Barrett TJ, Nelson JT, Angulo FJ. Reevaluating fluoroquinolone breakpoints for Salmonella enterica serotype Typhi and for non-Typhi salmonellae. Clin Infect Dis. 2003;37:75–81.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Third Informational Supplement. In: Wayne P, editor. CLSI document M100-S23. 2013.
Karczmarczyk M, Martins M, McCusker M, Mattar S, Amaral L, Leonard N, et al. Characterization of antimicrobial resistance in Salmonella enterica food and animal isolates from Colombia: identification of a qnrB19-mediated quinolone resistance marker in two novel serovars. FEMS Microbiol Lett. 2010;313:10–9.
Robicsek A, Strahilevitz J, Sahm DF, Jacoby GA, Hooper DC. qnr prevalence in ceftazidime-resistant Enterobacteriaceae isolates from the United States. Antimicrob Agents Chemother. 2006;50:2872–4.
Kim HB, Park CH, Kim CJ, Kim E-C, Jacoby GA, Hooper DC. Prevalence of plasmid-mediated quinolone resistance determinants over a 9-year period. Antimicrob Agents Chemother. 2009;53:639–45.
Wang M, Guo Q, Xu X, Wang X, Ye X, Wu S, et al. New plasmid-mediated quinolone resistance gene, qnrC, found in a clinical isolate of Proteus mirabilis. Antimicrob Agents Chemother. 2009;53:1892–7.
Cavaco LM, Hasman H, Xia S, Aarestrup FM. qnrD, a novel gene conferring transferable quinolone resistance in Salmonella enterica serovar Kentucky and Bovismorbificans strains of human origin. Antimicrob Agents Chemother. 2009;53:603–8.
Kidgell C, Reichard U, Wain J, Linz B, Torpdahl M, Dougan G, et al. Salmonella Typhi, the causative agent of typhoid fever, is approximately 50,000 years old. Infect Genet Evol. 2002;2:39–45.
Dimitrov T, Dashti AA, Albaksami O, Udo EE, Jadaon MM, Albert MJ. Ciprofloxacin-resistant Salmonella enterica serovar typhi from Kuwait with novel mutations in gyrA and parC genes. J Clin Microbiol. 2009;47:208–11.
Baker S, Duy PT, Nga TV, Dung TT, Phat VV, Chau TT, et al. Fitness benefits in fluoroquinolone-resistant Salmonella Typhi in the absence of antimicrobial pressure. Elife. 2013;2:e01229.
Holt KE, Dolecek C, Chau TT, Duy PT, La TT, Hoang NV, et al. Temporal fluctuation of multidrug resistant Salmonella typhi haplotypes in the Mekong river delta region of Vietnam. PLoS Negl Trop Dis. 2011;5:e929.
Giraud E, Baucheron S, Cloeckaert A. Resistance to fluoroquinolones in Salmonella: emerging mechanisms and resistance prevention strategies. Microbes Infect. 2006;8:1937–44.
Baucheron S, Monchaux I, Le Hello S, Weill FX, Cloeckaert A. Lack of efflux mediated quinolone resistance in Salmonella enterica serovars Typhi and Paratyphi A. Front Microbiol. 2014;5:12.
Lunguya O, Lejon V, Phoba MF, Bertrand S, Vanhoof R, Verhaegen J, et al. Salmonella typhi in the Democratic Republic of the Congo: fluoroquinolone decreased susceptibility on the rise. PLoS Negl Trop Dis. 2012;6:e1921.
Geetha VK, Yugendran T, Srinivasan R, Harish BN. Plasmid-mediated quinolone resistance in typhoidal Salmonellae: a preliminary report from South India. Indian J Med Microbiol. 2014;32:31–4.
Dahiya S, Kapil A, Kumar R, Das BK, Sood S, Chaudhry R, et al. Multiple locus sequence typing of Salmonella Typhi, isolated in North India - a preliminary study. Indian J Med Res. 2013;137:957–62.
Acknowledgements
This work was partly supported by the Swiss Federal Office of Public Health, Division Communicable Diseases.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MN analysed the data and wrote the manuscript. HA performed the molecular characterization and participated in the analysis of the data. GS: carried out species identification and phenotypic tests. NC performed multilocus sequence typing. RS designed the study, analysed the data and reviewed the manuscript. All authors read and approved the final manuscript.
Additional file
Additional file 1: Table S1.
S. Typhi 2002–2013. Details of the 192 Salmonella Typhi isolated between 2002 and 2013 analysed in this study.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Nüesch-Inderbinen, M., Abgottspon, H., Sägesser, G. et al. Antimicrobial susceptibility of travel-related Salmonella enterica serovar Typhi isolates detected in Switzerland (2002–2013) and molecular characterization of quinolone resistant isolates. BMC Infect Dis 15, 212 (2015). https://doi.org/10.1186/s12879-015-0948-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-015-0948-2