Abstract
Background
The incidence of sterilisation clip migration is reportedly 25%. However, less than 1% of those who experience clip migration will present with pain, an abscess, or spontaneous extrusion. Here we present a rare case of sterilisation clip migration through the entire pelvic floor.
Case presentation
A 66-year-old female was referred from community to the Surgical Emergency Unit with a possible metallic foreign body under the skin following an attempted routine gluteal cyst excision. The patient first noticed a lump under the skin 2 years ago which gradually became more apparent and tender over the previous 2 months. The patient denied recent trauma, had no co-morbidities and had a sterilisation procedure 24 years prior. Examination revealed a non-mobile solid structure just beneath the skin 5 cm laterally from the anal verge. Inflammatory markers were normal and an ultrasound confirmed a 15 × 7 mm foreign body in the subcutaneous tissues. The foreign body was excised easily under local anaesthesia, revealing a closed Filshie sterilisation clip. The wound was closed primarily, and recovery was uncomplicated.
Conclusions
This was a case of sterilisation clip migration to the subcutaneous gluteal region. A literature review revealed 34 case reports of sterilisation clip migration, mostly to the bladder. Patients with a previous sterilisation procedure and suspected subcutaneous foreign body without trauma should elicit a high index of suspicion for migrated sterilisation clips. These clips can migrate through multiple layers of muscle and fascia, including the pelvic floor.
Similar content being viewed by others
Background
The incidence of tubal clip migration is reportedly 25%. However, less than 1% of those who experience clip migration will present with symptoms such as pain, an abscess, or spontaneous extrusion [1]. As we report in this article, clip migration is unpredictable, rare, and the exact mechanisms are not well understood. Here, we present a rare case of sterilisation clip migration through the entire pelvic floor, as well as a literature review of reported sterilisation clip migration.
Case
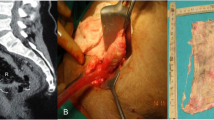
A 66-year-old female was referred from the community to the Surgical Emergency Unit with a possible metallic foreign body under the skin following an attempted routine gluteal cyst excision. The patient first noticed a lump under the skin 2 years ago which gradually became more apparent and tender over the past 2 months. The patient denied recent trauma or procedures in the gluteal region and inflammatory markers were normal. Examination revealed a non-mobile solid pin-like structure just beneath the skin 5 cm laterally from the anal verge (Fig. 1). An ultrasound confirmed a 15 × 7 mm foreign body in the subcutaneous tissue of the posteromedial aspect of the upper thigh (Fig. 2). The foreign body was excised easily under local anaesthesia, revealing a closed Filshie sterilisation clip. The wound was closed primarily, and recovery was uncomplicated. Apart from a laparoscopic sterilisation procedure 24 years prior, the patient was fit and well, with a normal body mass index (BMI).
Illustration of location of foreign body palpated during examination, marked with a cross, on an image adapted from https://theodora.com/anatomy/surface_anatomy_of_the_lower_extremity.html
Discussion
The overall number of sterilisation procedures in NHS hospitals is falling. The latest NHS Digital data suggest a 26% decrease in annual sterilisation procedures over a 10-year period. In the 2018/2019 year, there were 12,918 procedures performed, down from 17,562 in 2008/2009 [2]. However, there is a paucity of population-wide data on the specific type of female sterilisation method used. There have been advances in sterilisation methodology over the last two decades, namely the introduction of transcervical hysteroscopic devices. However, laparoscopic and laparotomic approaches are still utilised particularly in developing countries to achieve the common goal of uterine tubal occlusion [3]. As with all surgical procedures, this operation carries risks. Specific risks include a failed procedure, migration of the clip to other structures, and damage to surrounding anatomy. The latest NICE guidance corroborates a 1 in 200 failure rate of this procedure in achieving sterilisation [4], as reported in a 2001 publication by Mr Marcus Filshie, inventor of the Filshie clip [5]. With regard to clip migration, it appears that slow peritonealisation of the clip(s) results in a higher likelihood of migration. Faster peritonealisation of the clips renders them more likely to remain in situ [5]. Furthermore, while allergic reactions have been reported to cause Hulka clip sterile abscess formation [6], the titanium-silicone basis of Filshie clips makes this less likely, since these materials are commonly implanted elsewhere in the body and are not generally associated with sterile abscess formation [7]. The exact mechanism of migration through the pelvic floor however remains poorly understood. Given the rarity of this pathology, there is limited information on the pathophysiology of this migratory behaviour. Principles of acute and chronic inflammation in Crohn’s disease may help to explain how an abscess from the fallopian tubes could form a fistulous tract through the pelvic floor through neutrophil, macrophage, and fibroblast action, however this is unproven and requires further investigation [8].
We performed a literature review (Table 1) to determine whether this was a unique migration location, as well as to ascertain the incidence of sterilisation clip migration. In June 2023, we searched PubMed from June 1950 to June 2023 with the search terms [(sterilisation) OR (tubal ligation)] AND (clip) AND (migration) to identify other cases of sterilisation clip migration. We also searched the references of each of these papers to further widen our capture. This revealed 34 case reports of sterilisation clip migration, mostly to the bladder and anterior abdominal wall (Fig. 3). Despite an extensive literature search, no similar cases to this were identified. Locations such as the bladder, pelvic peritoneum, inguinal region, femoral region, anterior abdominal wall, spontaneous expulsion through the vagina, and even the liver have all been reported, however none to the gluteal area through the pelvic floor. Interestingly, this complication of tubal sterilisation does not appear to be either an early (< 5 years) or late (> 10 years) event. Figure 4 illustrates how there is a range of when these patients have presented in the acute setting for treatment. However, when exactly the migration occurs is not yet known, as a proportion of these cases may well show migration prior to acute illness presentation; for example, those with asymptomatic migration presenting later with acute sepsis. Furthermore, not all cases of clip migration will have been published in the literature, and there may be further cases not captured by our search strategy, therefore the true prevalence of these instances may be underestimated. Clips placed elsewhere in the body may also migrate. Surgical clip migration after laparoscopic cholecystectomy is another documented occurrence of a different type of clip migration [9]. A case report described a patient who developed cholangitis due to clip migration 10 years after initial laparoscopic cholecystectomy. CT imaging revealed hyperdense material in the dilated common bile duct, retrieved by endoscopic retrograde cholangiopancreatography via balloon trawl.
Patients with a previous sterilisation procedure and suspected subcutaneous foreign body without trauma should elicit a high index of suspicion for migrated sterilisation clips. We show that these clips can migrate through multiple layers of muscle and fascia, including the pelvic floor. Clinicians should be aware of the possibility of clip migration especially when patients present with recurrent abscesses of unknown cause, and thorough history taking may help to guide the working diagnosis. The role of plain film X-radiography is yet to be elucidated, however this may be a simple screening investigation if a radiopaque foreign body is thought to be the underlying cause. Ultimately, the majority of the cases of sterilisation clips were diagnosed on surgical exploration, rather than prior imaging. However, in cases of recurrent abscesses, pre-operative imaging may help reduce the incidence of recurrent abscess formation especially in cases where the sterilisation clip is not excised during the index operation.
Conclusions
Patients with a previous sterilisation procedure and suspected subcutaneous foreign body without trauma should elicit a high index of suspicion for migrated sterilisation clips. These clips can migrate through multiple layers of muscle and fascia, including the pelvic floor.
Availability of data and materials
All data available are presented.
Abbreviations
- BMI:
-
Body mass index
- NHS:
-
National Health Service
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computerised tomography
- I + D:
-
Incision and drainage
- EUA:
-
Examination under anaesthetic
- AXR:
-
Abdominal X-ray
References
Sharma S, Martyniak R, Khokhotva V. Migrated tubal ligation (Filshie) clip as an uncommon cause of chronic abdominal pain. Case Rep Surg. 2020;2020:4809859.
NHS Digital. [cited 2023 Aug 9]. Part 4: Sterilisations and vasectomies. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/sexual-and-reproductive-health-services/2018-19/sterilisations-and-vasectomies.
Gizzo S, Bertocco A, Saccardi C, Di Gangi S, Litta PS, D’antona D, et al. Female sterilization: update on clinical efficacy, side effects and contraindications. Minim Invasive Ther Allied Technol MITAT. 2014;23(5):261–70.
Failure rates | Background information | Contraception—sterilization | CKS | NICE. [cited 2023 Aug 9]. Available from: https://cks.nice.org.uk/topics/contraception-sterilization/background-information/failure-rates/.
Filshie GM. Female sterilisation: medico legal aspects. Rev Gynaecol Pract. 2001;1(2):79–88.
Allergic reaction to Hulka clips—PubMed. [cited 2023 Aug 9]. Available from: https://pubmed.ncbi.nlm.nih.gov/4058833/.
Scales JT. Implants in surgery. Br J Surg. 1974;61(12):987. https://doi.org/10.1002/bjs.1800611217.
Pathogenesis of Fistulating Crohn’s disease: a review—ScienceDirect. [cited 2024 May 4]. Available from: https://www.sciencedirect.com/science/article/pii/S2352345X22002065.
Cookson NE, Mirnezami R, Ziprin P. Acute cholangitis following intraductal migration of surgical clips 10 years after laparoscopic cholecystectomy. Case Rep Gastrointest Med. 2015;2015:e504295.
Frigenza M, Delotte J, Baque P, Trojani C, Mialon O, Chassang M, et al. A recurrent cutaneous fistula secondary to the migration of a clip: report of a complication of tubal sterilization. Gynecol Obstet Fertil. 2012;40(6):379–81.
Poo ZX, Ng G, Siraj SHM. An unusual case of a Filshie clip presenting as a bladder wall abscess 12 years after sterilization. Am J Case Rep. 2020;21: e923661.
Verma A, Oteri OE. An unusual case of migration of Filshie clip. J Fam Plann Reprod Health Care. 2007;33(3):212.
Daucher JA, Weber AM. Chronic abdominal pain after laparoscopic sterilization clip placement. Obstet Gynecol. 2006;108(6):1540–3.
Chronic groin sinus: an unusual complication of sterilisation clips—PMC. [cited 2023 Jun 16]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5696818/.
Dua RS, Dworkin MJ. Extruded Filshie clip presenting as an ischiorectal abscess. Ann R Coll Surg Engl. 2007;89(8):808–9.
Mumme AM, Cham J. Filshie clip migration with multiple groin hernias: a case report. J Med Case Reports. 2015;9:187.
Hasan A, Evgenikos N, Daniel T, Gatongi D. Filshie clip migration with recurrent perianal sepsis and low fistula in ano formation. BJOG Int J Obstet Gynaecol. 2005;112(11):1581.
Konaté A, Rauzy V, Chalon S, Ceballos P, Rivière S, Ciurana AJ, et al. Intraperitoneal migration of Filshie tubal sterilization clips: an uncommon cause of chronic abdominal pain. Gastroenterol Clin Biol. 2002;26(6–7):630–2.
Klumper F, Peters AA. Migrating clips; a complication following sterilization. Ned Tijdschr Geneeskd. 1991;135(6):233–5.
Tan BL, Chong C, Tay EH. Migrating Filshie clip. Aust N Z J Obstet Gynaecol. 2004;44(6):583–4.
Kalu E, Croucher C, Chandra R. Migrating Filshie clip: an unmentioned complication of female sterilisation. J Fam Plann Reprod Health Care. 2006;32(3):188–9.
Kesby GJ, Korda AR. Migration of a Filshie clip into the urinary bladder seven years after laparoscopic sterilisation. Br J Obstet Gynaecol. 1997;104(3):379–82.
Amu O, Husemeyer RP. Migration of sterilisation clips: case report and review. Br J Fam Plann. 1999;25(1):27–8.
Spontaneous Expulsion of Tubal Ligation Clips: A Case Report—ScienceDirect. [cited 2023 Jun 16]. Available from: https://www.sciencedirect.com/science/article/abs/pii/S1701216316325968.
Siew L. Vaginal expulsion of a Hulka clip. A case report. J Reprod Med. 1991;36(9):695–6.
[PDF] Complex inflammatory abdominal mass: a late complication of tubal clip sterilisation? | Semantic Scholar. [cited 2023 Jun 16]. Available from: https://www.semanticscholar.org/paper/Complex-inflammatory-abdominal-mass%3A-a-late-of-clip-Saha-Clausen/06fdebebfbd7027efc21737e62e8ea35598b118e.
Pandit M. Early extrusion of bilateral Filshie clips after laparoscopic sterilisation. BJOG Int J Obstet Gynaecol. 2005;112(5):680.
Loddo A, Botchorishvili R, Mage G. Migration of Filshie clip inside a small peritoneal defect. J Minim Invasive Gynecol. 2008;15(4):394.
Spontaneous urethral extrusion of a Filshie clip—PubMed. [cited 2023 Jun 16]. Available from: https://pubmed.ncbi.nlm.nih.gov/17999315/.
Kale A, Chong YS. Spontaneous vaginal expulsion of a Filshie clip. Ann Acad Med Singapore. 2008;37(5):438–9.
Krishnamoorthy U, Nysenbaum AM. Spontaneous extrusion of a migrating Filshie clip through the anterior abdominal wall. J Obstet Gynaecol. 2004;24(3):328–9.
Miliauskas JR. Migration of a Filshie clip into the urinary bladder with abscess formation. Pathology (Phila). 2003;35(4):356–7.
Gad N, Aziz R, Siwicki K. Filshie clip migration into wall of urinary bladder presenting with acute abdominal pain. Case report and review of English literature: from1990 to April 2009.
Connolly D, Kernohan R. Migrating of Filshie clips. J Obstet Gynaecol J Inst Obstet Gynaecol. 2004;24(8):944.
Lok IH, Lo KWK, Ng JSW, Tsui MHY, Yip SK. Spontaneous expulsion of a Filshie clip through the anterior abdominal wall. Gynecol Obstet Invest. 2003;55(3):183–5.
Garner JP, Toms M, McAdam JG. Filshie clips retrieved from a femoral hernia. J R Army Med Corps. 1998;144(2):107–8.
Filshie Clip Expulsion Through Persistent Groin Sinus After... : Urogynecology. [cited 2023 Jun 16]. Available from: https://journals.lww.com/fpmrs/Abstract/2006/09000/Filshie_Clip_Expulsion_Through_Persistent_Groin.9.aspx.
Denton GW, Schofield JB, Gallagher P. Uncommon complications of laparoscopic sterilisation. Ann R Coll Surg Engl. 1990;72(3):210–1.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
ASL is first-author and was responsible for case report write-up, literature search and review, obtaining radiology images, and submission of the manuscript for publication as corresponding author. AA was responsible for obtaining informed written consent, contributed to the literature search, and manuscript write-up. SMS provided clinical oversight and approval of the final manuscript. CL is lead author with overall case report responsibility, was the operating surgeon, provided clinical oversight, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written consent obtained.
Consent for publication
Written consent obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lakha, A.S., Ang, A., Salih, S.M. et al. Migrated tubal sterilisation clip presenting as a subcutaneous gluteal foreign body 24 years later: a case report and literature review. surg case rep 10, 143 (2024). https://doi.org/10.1186/s40792-024-01937-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-024-01937-3