Abstract
Diabetes occurs more often in individuals with COPD than in the general population, however there are still many issues that need to be clarified about this association. The exact prevalence of the association between diabetes and COPD varies between studies reported, however it is known that diabetes affects 2–37 % of patients with COPD, underlining the need to better understand the link between these two conditions. In this review, we evaluated the epidemiological aspects of the association between diabetes and COPD analyzing potential common issues in the pathological mechanisms underlying the single disease. The close association suggests the occurrence of similar pathophysiological process that leads to the development of overt disease in the presence of conditions such as systemic inflammation, oxidative stress, hypoxemia or hyperglycemia. Another, but not less important, aspect to consider is that related to the influence of the pharmacological treatment used both for the patient affected by COPD and from that affected by diabetes. It is necessary to understand whether the treatment of COPD affect the clinical course of diabetes, it is also essential to learn whether treatment for diabetes can alter the natural history of COPD.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) is a common comorbidity of chronic obstructive pulmonary disease (COPD) [1]. A series of studies have shown that DM is associated with impaired lung function [2]. The chronic complications of diabetes include a number of pathological changes involving different districts and, among these, lung represents a target organ for diabetic microangiopathy in patients with diabetes [3]. The Framingham Heart Study has reported an association between glycemic status and reduced lung function [4]. The diagnosis of DM was associated with lower adjusted mean residual forced expiratory volume in one second (FEV1) and Forced vital capacity (FVC). The Copenhagen City Heart Study, a longitudinal analysis [5], has shown an association between a new diagnosis of diabetes and impaired lung function that was more prominent in diabetic subjects treated with insulin compared with subjects treated with oral hypoglycaemic agents. In a prospective Australian study, the Fremantle Diabetes Study, 125 patients with type 2 diabetes mellitus (T2D) and no history of lung disease was assessed by spirometry at baseline and revaluated seven years later. The key finding was that the average rate of decline in lung function, as measured by FEV1 was 71 ml/year compared to an expected decline in healthy non-smokers of 25–30 ml/year, suggesting that the exposure to blood glucose may be a strong and consistent negative predictor of lung function follow-up after adjustment for baseline and potential confounders [6]. The association between impaired lung function and diabetes is thought to be the result of biochemical changes in the structures of the lung tissue and airways that involves a series of mechanisms likely due to systemic inflammation, oxidative stress, hypoxemia or ultimately to the direct damage caused by chronic hyperglycemia. The lung function decline in patients with diabetes may be a consequence of diabetes itself and diabetic patients seem to have an increased risk of several non-neoplastic lung conditions such as asthma and COPD [3].
In a retrospective study using data collected from the Italian College of General Practitioners Health Search Database it was reported that compared to the non-COPD individuals, patients with COPD exhibit a higher prevalence of DM (10.5 % in the general population vs. 18.7 % in patients with COPD) [7, 8]. This data has been confirmed in another study conducted in Taiwan that reported in COPD patients a higher risk of T2D compared with control subjects after adjusting for confounding factors [9]. However, there are also contrasting data in the literature, such as those reported by Korean researchers who have found no association between COPD and DM perhaps due to differences in race or nutritional factor; or probably simply due to a misclassification when general practitioners use specific diagnostic categories, mainly COPD [10].
In any case, it is not known why patients with COPD are affected by T2D more often than non-T2D subjects. Many conditions, in addition to chronic hyperglycemia, such as inflammation or disease-related inflammation, oxidative stress, hypoxia, reduced physical activity, and smoking habit may contribute to the higher prevalence of diabetes in COPD. In addition to all these conditions, the treatment with corticosteroids is considered to be another cause of the association between these two diseases [11].
Review
Epidemiology
Diabetes occurs more often in people with COPD than in the general population [11], although the exact prevalence varies between studies.
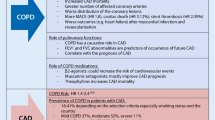
A retrospective analysis examined the relationship between COPD and comorbidities using Health Search Database information obtained from Italian College of General Practitioners, that stores information of nearly 1.5 % of the national population. Compared to the non-COPD individuals, COPD patients were at increased risk of DM, 10.5 % in the general population vs. 18.7 % in COPD patients. Unexpectedly, in this study COPD patients had an increased prevalence of both cardiovascular diseases and T2D and a very low prevalence of the metabolic syndrome, suggesting that COPD is a real risk factor for cardiovascular diseases and diabetes [8].
It has been consistently reported (Table 1) an impaired pulmonary function and glucose intolerance in several cross-sectional and perspective studies. A prospective study conducted in a five years observation period reported that the development of DM was associated with greater rates of decline of pulmonary function suggesting that diabetes may be, in particular at its onset, is associated with a significantly accelerated decline of respiratory function [12]. Lazarus et al within the Normative Aging Study in their perspective analysis reported that FVC was negatively associated with the risk to have higher levels of insulin resistance and a similar associations were found for FEV1 and maximal mid-expiratory flow rate (MMEF), suggesting the possibility that insulin resistance could be the factor correlated with the impairment of pulmonary function [13]. In another prospective study with a median follow up of 13 years, the authors concluded that the risk of developing diabetes is inversely associated with pulmonary function and the longitudinal associations between vital capacity (VC) and diabetes (P = 0.001) and log glucose (P = 0.036) were significant after adjustments for confounders [14].
The Nurses' Health Study, a prospective cohort study, during the 8 years follow-up found that the risk to have T2D was significantly higher in patients with COPD than those without COPD (multivariate relative risk 1.8, 95 % CI 1.1–2.8) nor those with asthma. These data suggest that COPD could be a risk factor for developing T2D, perhaps sharing common inflammatory and cytokine profile [15]. In another Korean study, planned to assess the relationship between lung function and incident T2D, 9,220 men without T2D were prospectively followed for five years. The authors found that impaired lung function is independently associated with the incidence of T2D. FVC and FEV1 were negatively associated with T2D (P < 0.05) independently by confounding factors. It is therefore proposed on the basis of these results, the possibility that the reduced lung function, as measured by FEV1 and FVC, may precede the development of T2D [16].
Differently, in a prospective study conducted in a cohort of 38,570 women with median follow-up of 12.2 years, the hypothesis that asthma or COPD could be involved in the pathogenesis of T2D was tested. Both asthma and COPD were individually and independently associated with an increased risk of T2D in women; this association was independent of cigarette smoking and other diabetes risk factors and also persisted after excluding all COPD cases with asthmatic symptoms. The multivariate RRs were 1.38 (95 % CI, 1.14–1.67) for COPD without asthmatic symptoms [17].
Recently, an increased prevalence of diabetes in non-emphysematous COPD patients (diabetes OR 2.13, p < 0.0001) has been reported in the COPD Gene Study, where patients were classified in emphysema-predominant and non-emphysematous COPD based on CT scan features [18]. Although comorbidities were self-reported, previous studies have shown that it is a reliable source of information [19]. This association persisted also after performing stratified analyses considering obese and non-obese individuals, smoking habit, bronchial obstruction severity divided in GOLD 1– 2 and GOLD 3– 4, ethnicity and age. These results were also confirmed by the ECLIPSE study, where diabetes was reported in 10.6 % of non-emphysema and in 8.2 % of emphysema-predominant COPD [20]. The authors suggested to evaluate for diabetes patients with COPD, especially those defined non-emphysema [18].
In a study conducted in UK using the wide primary care data to quantify the burden of comorbidity among individuals with COPD, it has been shown that COPD is associated with an increased odds of DM. Intriguingly the effect of COPD having DM is higher in current smokers for the younger patients, but after the age of 45 becomes greater in non-smokers, suggesting that this association was independent of smoking status [21].
Mechanisms
DM is a common comorbidity of COPD [7]. What are the mechanisms underlying the increased prevalence of diabetes in COPD still remains unclear, although a number of potential pathways including inflammation, oxidative stress, hypoxia and chronic hyperglycemia may provide some explanation [11, 2].
Systemic inflammation is a common feature to both COPD and to T2D, which drives insulin resistance, atherosclerosis and many systemic expressions of COPD itself. The presence of systemic inflammation is poorly defined in patients with COPD. Most of the studies were cross-sectional and show that not all patients with COPD have a systemic inflammatory response. However systemic inflammation is a risk factor for the development of many chronic diseases, which are COPD co-morbidity [22]. However, we should consider that the persistent systemic inflammation in COPD patients is associated with significantly worse outcomes in terms of mortality and exacerbation rate as demonstrated by the ECLIPSE study. It appears to be mostly independent from the pulmonary component of the disease, raising the possibility that systemic inflammation could be a possible therapeutic target in these patients [23]. The possible development of COPD and T2D could have evidence in the context of a chronic systemic inflammation with the presence of cardiovascular disease or metabolic disorders, known to be related to systemic inflammation, increasing the association between COPD and DM [7]. In any case, systemic inflammation might be increased by the coexistence of these two conditions, COPD and diabetes, worsening both in their clinical manifestations.
There are many evidences that the levels of inflammatory proteins (Table 2), such as cytokines and among these TNF- α, IL-6, or C reactive protein (CRP), are increased in patients with COPD. Systemic inflammation is associated with various complications in COPD, including cardiovascular and metabolic diseases such as diabetes.
TNF-α is a marker of systemic inflammation that appears to be associated with the severity of COPD, increased levels are seen in severe and very severe COPD. On the other hand, high levels of TNF- α may be a risk factor for the development of new-onset T2D, interfering with glucose metabolism and insulin sensitivity [22, 24], suggesting a possible link between COPD and T2D.
Increased levels of IL-6 are independently associated with COPD, in particular serum concentrations of this cytokine were found significantly increased in COPD exacerbation compared to patients in stable phase [25]. Furthermore, IL-6 is a potent stimulator of CRP production by the liver and the increase of CRP that is observed in patients with COPD could represent an explanation. CRP serum is considered the biomarker of systemic inflammation and seems to relate with other inflammatory biomarkers including IL-6 [26, 27]. Many are the associations that have been reported between CRP and the different aspects of COPD. Studies that have explored these aspects have shown contrasting results: a meta-analysis showed a marked difference in the level of serum CRP in COPD compared with controls [28], while in another meta-analysis has not been found any statistically significant difference in CRP levels between COPD and control [29]. Though, a population-based study showed that the increase in CRP was observed in stable COPD compared with controls, even after adjustment for potential confounders [26]. Furthermore cross-sectional studies show that CRP is inversely associated with the FEV1 and PaO2 in patients with COPD [30, 24], confirming the idea that there is a systemic inflammatory response in this disease progressively debilitating [31]; in fact both IL-6 and CRP have been shown to increase the risk of developing new-onset T2D, especially the high levels of CRP may predict the development of the onset of T2D [24].
Oxidative stress is generated by an imbalance between oxidants and antioxidants. In COPD patients, either in stable or during acute exacerbations, oxidative stress is increased mainly by inhalation of oxidants such as those generated by cigarette smoke or pollution, or as a result of inflammatory leukocytes that are activated to release reactive oxygen species. This condition can cause direct damage to the lung targeting lipids and proteins, triggering specific pathways, which could generate increased gene expression, production pro-inflammatory cytokines and ultimately increased inflammation [32]. Finally adiponectin, an adipokin with intrinsic anti-inflammatory property, correlates with COPD; data obtained in case-control studies demonstrated a higher systemic and airway adiponectin concentrations in COPD patients mainly men than controls. Moreover serum adiponectin has a positive correlation with lung function in healthy adults, whereas an inverse correlation has been found in studies conducted in male individuals with COPD [33].
In T2D oxidative stress is present through the activation of specific biochemical pathways, increased production of reactive oxygen species, reduction of antioxidants and furthermore increase lipid peroxidation. Oxidative stress, mainly smoke-induced in COPD patients, could cause in T2D the continuation of the insulin resistance by altering the production of energy. Conversely oxidative stress produced by T2D might worsen COPD activating inflammation and even compromising the response to glucocorticoids [11].
Smoking induces oxidative stress that can trigger local and systemic inflammation, though cigarette smoking is not a link between DM and COPD [34]. This is especially interesting given that exposure to cigarette smoking is crucial for the development of COPD [35] and, at the same time, an independent and modifiable factor for the development of DM [36]. Since cigarette smoking does not appear to be the connection, it is likely that other mechanisms besides systemic inflammation or oxidative stress could define the link between DM and COPD.
Current evidence suggests that COPD, in which hypoxia is one of the typical features, is associated with increased levels of oxidative stress [37], but likewise an excessive oxidative stress may be a risk factor for new-onset T2D it can be also a result of new onset DM [38]. Moreover, the induction of increased levels of reactive oxygen species (ROS), NF-kB and intracellular mediators of inflammation could also lead to chronic hyperglycemia and to an increased synthesis of collagen mediated by higher levels of advanced glycation end products that ultimately would affect negatively lung function [39].
Hypoxia causes significant changes in metabolism, studies conducted in healthy subjects at high altitude showed increased insulin resistance and glucose production in the liver [40, 41] with greater insulin sensitivity at peripheral level and increased uptake of glucose in skeletal muscle [42]. It seems that pancreatic β cells are sensitive to hypoxia-induced damage, regardless of the condition of intermittent hypoxia as that observed in sleep apnea [43], or chronic hypoxia seen in COPD. Indeed, chronic hypoxia has been observed in association with impaired glucose tolerance, reduced insulin sensitivity accompanied by greater lipolysis. In COPD patients, in which the normalization of saturation values has been obtained, it can be observed an improvements of glucose tolerance and insulin sensitivity [44, 45]. It is possible that both of these diseases, COPD and DM, might share common pathophysiological pathways which can be mediated by hypoxia inducible factor (HIF) [46].
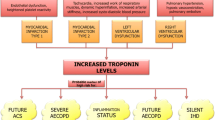
Inflammation, oxidative stress and hyperglycemia in particular, have been shown to induce muscle dysfunction [47]. Lower lung function has also been suggested to be associated with increased serum osmolarity, where blood sugar contributes to the total serum osmolarity [48, 13]. A number of prospective studies have shown that reduced lung function is an independent predictor of T2D [13, 14, 49]. In particular, in a prospective study on lung function in adults with T2D, it has been suggested the idea that alterations in lung function may precede diabetes and then will progress after the onset of diabetes itself [50].
In a study that we conducted on isolated human bronchi, we found that high glucose concentrations lead to enhanced responsiveness of airway smooth muscle cells to contractile agent. The data suggested that the glucose-induced enhancement of bronchial responsiveness is likely to be due to increased activation of a particular intracellular pathway: the Rho-kinase pathway. It seems that the Rho/ROCK pathway plays a role in regulating several biological pathways, including some that affect the level of airway smooth muscle (ASM) tone [2]. The activation of this pathway mediates multiple biological functions involving contractility based on actin-myosin [51]. Moreover, our results suggested that the Rho/ROCK pathway, together with the mobilization of the intracellular calcium and the phosphorylation of MYPT-1, might play a crucial role in the reduced lung function observed in patients with diabetes [2]. It is widely accepted that airway hyperresponsiveness is a risk factor for an accelerated decline in FEV1 and the development of obstructive pulmonary disease such as COPD [50]. As well as pulmonary function impairment that is greater in patients with poorly controlled diabetes, a finding that, however, is not explained by obesity or increasing age [7].
Treatment
The strong association between COPD and diabetes has been explained through evaluation of probable common risk factors, or probable common mechanisms, but it was also explained as a potential consequence of treatment options for COPD. Corticosteroids is considered the main therapeutic approach potentially implicated in the strong association between diabetes and COPD. The use of corticosteroids, in susceptible individuals, may determine states of hyperglycemia. In fact, the use of inhaled corticosteroid (ICS) has been reported to be correlated with an increase in the concentration of plasma glucose in diabetic patients, and this increase seems to be modulated in a dose-response manner [52]. Short-term treatment with oral corticosteroids, used in acute exacerbations, is associated with a five-fold increased risk of acute hyperglycemia and also the long-term use of oral corticosteroids in stable COPD is correlated with increased risk of glucose intolerance [53, 54]. Studies evaluating the actual impact of ICSs on the association between these two pathological conditions, and if ICSs actually increase the risk of DM, have shown contrasting results [18]. In a prospective, crossover study, patients with T2D exhibited small but statistically significant increased glycosylated hemoglobin levels after 6 weeks of treatment with an ICS, fluticasone, although this did not have a clinically significant impact on longterm glycaemic control [55]. Instead, in a more recent retrospective study, double-blind, placebo-controlled, which used the ICS budesonide alone or in combination budesonide/ formoterol in COPD highlighted that the treatment with ICS in COPD patients was not associated with an increased risk of new-onset DM nor hyperglycemia [56]. These studies outline how the association between COPD and T2D might be independent of the use of ICSs [56], although the discrepancy of reported data leave doubts about the real influence of ICSs on diabetes [57].
Beyond everything, it should not be precluded the use of ICSs in COPD patients, where clinical evidence suggests that they may be useful, rather it should be aware that there is a risk of unwanted side effects and it should be considered a use of the lowest possible dose to obtain the optimal management of the disease [57].
Another class of anti-inflammatory treatment is available for severe COPD associated with chronic bronchitis and a history of frequent exacerbations: the phosphodiesterase 4 (PDE4) inhibitor. This treatment has been shown to be related to weight decreased transient and reversible, suggesting a systemic role of this drug possibly impacting on metabolism [58]. In a small randomized, double-blind, placebo-controlled study the effects of a PDE4 inhibitor on the glucose homeostasis and body weight in newly diagnosed T2D without COPD was investigated. Glycated hemoglobin levels and change from baseline in the postmeal for several metabolic parameters were the main outcomes. In patients with T2D a significant reduction in glycated hemoglobin (least square mean: 0.45 %; P: 0.0001) was observed as well as the postmeal rise in glucagon and fasting plasma glucose levels that was lower in the PDE4 inhibitor treatment group compared with in placebo group, suggesting that this antiflammatory drug could help to reduce the postprandial hyperglycemia that characterizes T2D state. The authors concluded that PDE4 inhibitors can lower glucose levels in patients with newly diagnosed T2D without COPD, although the exact mechanism is still unknown [59].
As far as regarding the other class of drugs for the mainstay treatment of COPD, for inhaled bronchodilators there are not much evidences on the association between COPD and diabetes. In a pooled analysis from 19 randomized, doubleblind, placebo-controlled trials with a longacting anticholinergic bronchodilator tiotropium, safety showed that there was no apparent increased risk of DM (RR, 0.99; 95 % CI, 0.41 to 2.37), in patients receiving tiotropium compared to those receiving placebo, however the relative risk of hyperglycemic events was 1.69 [60].
In patients with T2D, metformin is the recommended first-line treatment [61], and this treatment is associated with reduce risk of cardiovascular events and death [62]. Metformin has been, although rarely, associated with lactic acidosis which may be fatal, thus its safety in COPD it has been questioned [63]. The British National Formulary and the US Federal Drug Administration suggested that metformin should be discontinued immediately in any conditions associated with hypoxemia. Hence, the clinical use of metformin in patients with diabetes and coexisting COPD is limited whether it is appropriate or not [64]. Metformin, thanks to its pleiotropic anti-inflammatory and antioxidants actions [65, 66], may have a role in COPD by limiting glucose flux through the epithelium of the airways that is associated also with respiratory infections [67]. A retrospective study, which included patients with COPD and DM, showed that treatment with oral hypoglycemic agents was independently associated with the improvement of FVC [68]. Moreover, a recent open-label study where metformin in patients with COPD has been used, suggested that this drug could improve respiratory muscle strength [69]. Safety of metformin in COPD has been evaluated in a recent retrospective cohort. COPD patients treated with metformin showed an association with lower elevation of lactate concentration of uncertain clinical significance [64]. The authors are currently recruiting patients in the UK in a prospective clinical trial, in order to clarify the use of metformin in COPD (Current Controlled Trials ISRCTN66148745).
Although the Copenhagen City Heart Study has shown an association between a new diagnosis of DM and impaired lung function, a condition that was more prominent in diabetic subjects treated with insulin rather than those treated with oral hypoglycaemic agents [5], insulin may play a role in facilitation of the alveolar-capillary interface conductance [70].
T2D seems to be associated with the reduction of alveolar microvascular reserves and possibly be evidence of deterioration in lung volume, alveolar perfusion and capillary recruitment. This reduction correlates with glycemic control and extrapulmonary microangiopathy [71]. Lung diffusing capacity for carbon monoxide (DLCO) is a known surrogate marker for the alveolar capillary membrane morphological and functional status. A small study on diabetic patients tested the effects of regular insulin on DLCO: insulin improved DLCO in patients with T2D possibly through a facilitation of the alveolar-capillary interface conductance [70]. Based on possible role of insulin in improving pulmonary gas exchange it was attempted inhaled use. However, the use of inhaled insulin has highlighted potential negative effects and among them the presence of cough, and potential reduction in DLCO and FEV1 [72]. More research is needed before inhaled insulin may be recommended in diabetic patients with or without pulmonary disease.
Conclusions
The association between two complex conditions such as COPD and T2D is expressed at different levels: epidemiological, on possible common pathogenic mechanisms and the impact that the treatments used for individual conditions may have on the association itself.
The complexity of this association also stems from the evidence that COPD can be considered a risk factor for the development of T2D, as pointed out by several epidemiological studies that have used national and international databases [8–10, 13].
In our opinion, the lung function may be affected in conditions that precede the onset of T2D, such as in individuals with impaired glucose tolerance or in patients with metabolic syndrome. If this hypothesis is correct, we might state that pulmonary dysfunction precede the onset of T2D, presenting similarities to the pathogenesis of endothelial dysfunction that also usually develops before the onset of T2D, further studies need to be done to clarify this aspect. This close association can lead to the hypothesis that in a part of the population with COPD and with T2D it would be possible to have a similar pathophysiological process that leads to the development of overt disease in the presence of hyperglycemia and/or respiratory failure. Recently, it has been reported that a pro-inflammatory state, that could be a common pathophysiological process for these two conditions, is present in overweight or obese pre-diabetic individuals and early stage of COPD [11]. Indeed, CRP, IL-6 and TNF-α may contribute to an altered metabolic state and insulin resistance. Furthermore, TNF-α is also a key inflammatory mediator in the process of muscle wasting, sometimes associated with cachexia, and this reduces peripheral insulin resistance in skeletal muscle [73]. On the other side, a decrease in adiponectin levels, which usually is present in pre-diabetic conditions, can contributes to the pulmonary and vascular damage [74]. Eventually, it is also possible that COPD may increase the levels of oxidative stress due to a hypoxic state. In this new scenario, COPD can also be considered a metabolic disease with a pathophysiological process similar to T2D. Hence, in this review we have addressed the different aspects of this association, assessing in particular among the hypothesized pathogenetic mechanisms involved the possibility of a new concept of pathogenetic link between COPD and T2D: hyperglycemia. Despite the many data reported in the literature outlining how hyperglycemia and higher levels of insulin-resistance may be associated with the onset and progression of these two conditions, the novelty is that glucose may directly modulate bronchial tone. In fact glucose can directly affect pulmonary bronchial tone and ASM through the regulation of different molecular pathways in smooth muscle cells. Indeed, we demonstrated as higher activation of Rho/ROCK pathway can be a molecular pathway affecting the pulmonary physiology associated to COPD in T2D patients and the modulation of these substrates can potentially represent a novel therapeutic target for the treatment of COPD [2], although this finding should be further explored.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- DM:
-
Diabetes Mellitus
- T2D:
-
Type 2 Diabetes
- FEV1:
-
Forced expiratory volume in one second
- FVC:
-
Forced vital capacity
- MMEF:
-
Maximal mid-expiratory flow rate
- VC:
-
Vital capacity
- CRP:
-
C reactive protein
- ASM:
-
Airway smooth muscle
- PDE4:
-
Phosphodiesterase 4
- ROS:
-
Reactive oxygen species
- HIF:
-
Hypoxia inducible factor
- ICS:
-
Inhaled corticosteroid
- DLCO:
-
Lung diffusing capacity for carbon monoxide
References
Cavailles A, Brinchault-Rabin G, Dixmier A, Goupil F, Gut-Gobert C, Marchand-Adam S, et al. Comorbidities of COPD. Eur Res Rev. 2013;22(130):454–75. doi:10.1183/09059180.00008612.
Cazzola M, Calzetta L, Rogliani P, Lauro D, Novelli L, Page CP, et al. High glucose enhances responsiveness of human airways smooth muscle via the Rho/ROCK pathway. Am J Respir Cell Mol Biol. 2012;47(4):509–16. doi:10.1165/rcmb.2011-0449OC.
Ehrlich SF, Quesenberry Jr CP, Van Den Eeden SK, Shan J, Ferrara A. Patients diagnosed with diabetes are at increased risk for asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, and pneumonia but not lung cancer. Diabetes Care. 2010;33(1):55–60. doi:10.2337/dc09-0880.
Walter RE, Beiser A, Givelber RJ, O'Connor GT, Gottlieb DJ. Association between glycemic state and lung function: the Framingham Heart Study. Am J Respir Crit Care Med. 2003;167(6):911–6. doi:10.1164/rccm.2203022.
Lange P, Groth S, Kastrup J, Mortensen J, Appleyard M, Nyboe J, et al. Diabetes mellitus, plasma glucose and lung function in a cross-sectional population study. Eur Respir J. 1989;2(1):14–9.
Davis WA, Knuiman M, Kendall P, Grange V, Davis TM, Fremantle DS. Glycemic exposure is associated with reduced pulmonary function in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care. 2004;27(3):752–7.
Rogliani P, Calzetta L, Segreti A, Barrile A, Cazzola M. Diabetes mellitus among outpatients with COPD attending a university hospital. Acta Diabetologica. 2014;51(6):933–40. doi:10.1007/s00592-014-0584-0.
Cazzola M, Bettoncelli G, Sessa E, Cricelli C, Biscione G. Prevalence of comorbidities in patients with chronic obstructive pulmonary disease. Respiration. 2010;80(2):112–9. doi:10.1159/000281880.
Lee CT, Mao IC, Lin CH, Lin SH, Hsieh MC. Chronic obstructive pulmonary disease: a risk factor for type 2 diabetes: a nationwide population-based study. Eur J Clin Invest. 2013;43(11):1113–9. doi:10.1111/eci.12147.
Joo H, Park J, Lee SD, Oh YM. Comorbidities of chronic obstructive pulmonary disease in Koreans: a population-based study. J Korean Med Sci. 2012;27(8):901–6. doi:10.3346/jkms.2012.27.8.901.
Wells CE, Baker EH. Metabolic syndrome and European Respiratory Monograph 59: COPD and Comorbidity. Eur Res Monograph. 2013;59:117–34.
Lange P, Groth S, Mortensen J, Appleyard M, Nyboe J, Schnohr P, et al. Diabetes mellitus and ventilatory capacity: a five year follow-up study. Eur Respir J. 1990;3(3):288–92.
Lazarus R, Sparrow D, Weiss ST. Baseline ventilatory function predicts the development of higher levels of fasting insulin and fasting insulin resistance index: the Normative Aging Study. Eur Respir J. 1998;12(3):641–5.
Engstrom G, Janzon L. Risk of developing diabetes is inversely related to lung function: a population-based cohort study. Diab Med. 2002;19(2):167–70.
Rana JS, Mittleman MA, Sheikh J, Hu FB, Manson JE, Colditz GA, et al. Chronic obstructive pulmonary disease, asthma, and risk of type 2 diabetes in women. Diabetes Care. 2004;27(10):2478–84.
Kwon CH, Rhee EJ, Song JU, Kim JT, Kwag HJ, Sung KC. Reduced lung function is independently associated with increased risk of type 2 diabetes in Korean men. Cardiovasc Diabetol. 2012;11:38. doi:10.1186/1475-2840-11-38.
Song Y, Klevak A, Manson JE, Buring JE, Liu S. Asthma, chronic obstructive pulmonary disease, and type 2 diabetes in the Women's Health Study. Diab Res Clin Prac. 2010;90(3):365–71. doi:10.1016/j.diabres.2010.09.010.
Hersh CP, Make BJ, Lynch DA, Barr RG, Bowler RP, Calverley PM, et al. Non-emphysematous chronic obstructive pulmonary disease is associated with diabetes mellitus. BMC Pulmonary Medicine. 2014;14:164. doi:10.1186/1471-2466-14-164.
Oksanen T, Kivimaki M, Pentti J, Virtanen M, Klaukka T, Vahtera J. Self-report as an indicator of incident disease. Ann Epidemiol. 2010;20(7):547–54. doi:10.1016/j.annepidem.2010.03.017.
Agusti A, Calverley PM, Celli B, Coxson HO, Edwards LD, Lomas DA, et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122. doi:10.1186/1465-9921-11-122.
Feary JR, Rodrigues LC, Smith CJ, Hubbard RB, Gibson JE. Prevalence of major comorbidities in subjects with COPD and incidence of myocardial infarction and stroke: a comprehensive analysis using data from primary care. Thorax. 2010;65(11):956–62. doi:10.1136/thx.2009.128082.
MacNee W. Systemic inflammatory biomarkers and co-morbidities of chronic obstructive pulmonary disease. Ann Med. 2013;45(3):291–300. doi:10.3109/07853890.2012.732703.
Miller J, Edwards LD, Agusti A, Bakke P, Calverley PM, Celli B, et al. Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Res Med. 2013;107(9):1376–84. doi:10.1016/j.rmed.2013.05.001.
Mirrakhimov AE. Chronic obstructive pulmonary disease and glucose metabolism: a bitter sweet symphony. Cardiovasc Diabetol. 2012;11:132. doi:10.1186/1475-2840-11-132.
Wedzicha JA, Seemungal TA, MacCallum PK, Paul EA, Donaldson GC, Bhowmik A, et al. Acute exacerbations of chronic obstructive pulmonary disease are accompanied by elevations of plasma fibrinogen and serum IL-6 levels. Thromb Haemost. 2000;84(2):210–5.
Garcia-Rio F, Miravitlles M, Soriano JB, Munoz L, Duran-Tauleria E, Sanchez G, et al. Systemic inflammation in chronic obstructive pulmonary disease: a population-based study. Respir Res. 2010;11:63. doi:10.1186/1465-9921-11-63.
Karadag F, Kirdar S, Karul AB, Ceylan E. The value of C-reactive protein as a marker of systemic inflammation in stable chronic obstructive pulmonary disease. Eur J Int Med. 2008;19(2):104–8. doi:10.1016/j.ejim.2007.04.026.
Gan WQ, Man SF, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax. 2004;59(7):574–80.
Franciosi LG, Page CP, Celli BR, Cazzola M, Walker MJ, Danhof M, et al. Markers of exacerbation severity in chronic obstructive pulmonary disease. Respir Res. 2006;7:74. doi:10.1186/1465-9921-7-74.
Cazzola M, Matera MG, Rogliani P, Page C. Treating systemic effects of COPD. Trends Pharmacol Sci. 2007;28(10):544–50. doi:10.1016/j.tips.2007.09.006.
Agusti A, Faner R. Systemic inflammation and comorbidities in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2012;9(2):43–6. doi:10.1513/pats.201108-050MS.
Anderson D, Macnee W. Targeted treatment in COPD: a multi-system approach for a multi-system disease. Int J Chron Obstruct Pulmon Dis. 2009;4:321–35.
Garcia P, Sood A. Adiponectin in pulmonary disease and critically ill patients. Curr Med Chem. 2012;19(32):5493–500.
Chung KF, Adcock IM. Multifaceted mechanisms in COPD: inflammation, immunity, and tissue repair and destruction. Eur Res J. 2008;31(6):1334–56.
Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007;370(9589):741–50. doi:10.1016/S0140-6736(07)61377-4.
Manson JE, Ajani UA, Liu S, Nathan DM, Hennekens CH. A prospective study of cigarette smoking and the incidence of diabetes mellitus among US male physicians. Am J Med. 2000;109(7):538–42.
MacNee W. Oxidants and COPD. Curr Drug Targets Inflamm Allergy. 2005;4(6):627–41.
Evans JL, Goldfine ID, Maddux BA, Grodsky GM. Oxidative stress and stress-activated signaling pathways: a unifying hypothesis of type 2 diabetes. Endocr Rev. 2002;23(5):599–622. doi:10.1210/er.2001-0039.
Tiengo A, Fadini GP, Avogaro A. The metabolic syndrome, diabetes and lung dysfunction. Diab Metab. 2008;34(5):447–54. doi:10.1016/j.diabet.2008.08.001.
Ge RL, Simonson TS, Cooksey RC, Tanna U, Qin G, Huff CD, et al. Metabolic insight into mechanisms of high-altitude adaptation in Tibetans. Mol Gen Metab. 2012;106(2):244–7. doi:10.1016/j.ymgme.2012.03.003.
Sauerwein HP, Schols AM. Glucose metabolism in chronic lung disease. Clin Nutr. 2002;21(5):367–71.
Gamboa JL, Garcia-Cazarin ML, Andrade FH. Chronic hypoxia increases insulin-stimulated glucose uptake in mouse soleus muscle. Am J Physiol Regul Integr Comp Physiol. 2011;300(1):R85–91. doi:10.1152/ajpregu.00078.2010.
Pallayova M, Lazurova I, Donic V. Hypoxic damage to pancreatic beta cells--the hidden link between sleep apnea and diabetes. Med Hypotheses. 2011;77(5):930–4. doi:10.1016/j.mehy.2011.08.016.
Jakobsson P, Jorfeldt L. Oxygen supplementation increases glucose tolerance during euglycaemic hyperinsulinaemic glucose clamp procedure in patients with severe COPD and chronic hypoxaemia. Clin Physiol Funct Imaging. 2006;26(5):271–4. doi:10.1111/j.1475-097X.2006.00686.x.
Jakobsson P, Jorfeldt L, von Schenck H. Fat metabolism and its response to infusion of insulin and glucose in patients with advanced chronic obstructive pulmonary disease. Clin Physiol. 1995;15(4):319–29.
Semenza GL. Regulation of oxygen homeostasis by hypoxia-inducible factor 1. Physiology. 2009;24:97–106. doi:10.1152/physiol.00045.2008.
Niedowicz DM, Daleke DL. The role of oxidative stress in diabetic complications. Cell Biochem Biophys. 2005;43(2):289–330. doi:10.1385/CBB:43:2:289.
Pogson ZE, McKeever TM, Fogarty A. The association between serum osmolality and lung function among adults. Eur Respir J. 2008;32(1):98–104. doi:10.1183/09031936.00144207.
Yeh HC, Punjabi NM, Wang NY, Pankow JS, Duncan BB, Brancati FL. Vital capacity as a predictor of incident type 2 diabetes: the Atherosclerosis Risk in Communities study. Diabetes Care. 2005;28(6):1472–9.
Yeh HC, Punjabi NM, Wang NY, Pankow JS, Duncan BB, Cox CE, et al. Cross-sectional and prospective study of lung function in adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) study. Diabetes Care. 2008;31(4):741–6. doi:10.2337/dc07-1464.
Fernandes LB, Henry PJ, Goldie RG. Rho kinase as a therapeutic target in the treatment of asthma and chronic obstructive pulmonary disease. Ther Adv Res Disease. 2007;1(1):25–33. doi:10.1177/1753465807080740.
Slatore CG, Bryson CL, Au DH. The association of inhaled corticosteroid use with serum glucose concentration in a large cohort. Am J Med. 2009;122(5):472–8. doi:10.1016/j.amjmed.2008.09.048.
Walters JA, Gibson PG, Wood-Baker R, Hannay M, Walters EH. Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2009;1, CD001288. doi:10.1002/14651858.CD001288.pub3.
Walters JA, Walters EH, Wood-Baker R. Oral corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;3, CD005374. doi:10.1002/14651858.CD005374.
Faul JL, Wilson SR, Chu JW, Canfield J, Kuschner WG. The effect of an inhaled corticosteroid on glucose control in type 2 diabetes. Clin Med Res. 2009;7(1-2):14–20. doi:10.3121/cmr.2009.824.
O'Byrne PM, Rennard S, Gerstein H, Radner F, Peterson S, Lindberg B, et al. Risk of new onset diabetes mellitus in patients with asthma or COPD taking inhaled corticosteroids. Res Med. 2012;106(11):1487–93. doi:10.1016/j.rmed.2012.07.011.
Matera MG, Cardaci V, Cazzola M, Rogliani P. Safety of inhaled corticosteroids for treating chronic obstructive pulmonary disease. Expert Opin Drug Saf. 2015;14(4):533–41.
Fabbri LM, Calverley PM, Izquierdo-Alonso JL, Bundschuh DS, Brose M, Martinez FJ, et al. Roflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with longacting bronchodilators: two randomised clinical trials. Lancet. 2009;374(9691):695–703. doi:10.1016/S0140-6736(09)61252-6.
Wouters EF, Bredenbroker D, Teichmann P, Brose M, Rabe KF, Fabbri LM, et al. Effect of the phosphodiesterase 4 inhibitor roflumilast on glucose metabolism in patients with treatment-naive, newly diagnosed type 2 diabetes mellitus. J Clin Endocrinol Metab. 2012;97(9):E1720–5. doi:10.1210/jc.2011-2886.
Kesten S, Jara M, Wentworth C, Lanes S. Pooled clinical trial analysis of tiotropium safety. Chest. 2006;130(6):1695–703. doi:10.1378/chest.130.6.1695.
American DA. Standards of medical care in diabetes--2013. Diabetes Care. 2013;36 Suppl 1:S11–66. doi:10.2337/dc13-S011.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–89. doi:10.1056/NEJMoa0806470.
Salpeter SR, Greyber E, Pasternak GA, Salpeter EE. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev. 2010;4, CD002967. doi:10.1002/14651858.CD002967.pub4.
Hitchings AW, Archer JR, Srivastava SA, Baker EH. Safety of Metformin in Patients with Chronic Obstructive Pulmonary Disease and Type 2 Diabetes Mellitus. Copd. 2014. doi:10.3109/15412555.2014.898052.
Huang NL, Chiang SH, Hsueh CH, Liang YJ, Chen YJ, Lai LP. Metformin inhibits TNF-alpha-induced IkappaB kinase phosphorylation, IkappaB-alpha degradation and IL-6 production in endothelial cells through PI3K-dependent AMPK phosphorylation. Int J Cardiol. 2009;134(2):169–75. doi:10.1016/j.ijcard.2008.04.010.
Formoso G, De Filippis EA, Michetti N, Di Fulvio P, Pandolfi A, Bucciarelli T, et al. Decreased in vivo oxidative stress and decreased platelet activation following metformin treatment in newly diagnosed type 2 diabetic subjects. Diabetes Metab Res Rev. 2008;24(3):231–7. doi:10.1002/dmrr.794.
Garnett JP, Baker EH, Naik S, Lindsay JA, Knight GM, Gill S, et al. Metformin reduces airway glucose permeability and hyperglycaemia-induced Staphylococcus aureus load independently of effects on blood glucose. Thorax. 2013;68(9):835–45. doi:10.1136/thoraxjnl-2012-203178.
Kim HJ, Lee JY, Jung HS, Kim DK, Lee SM, Yim JJ, et al. The impact of insulin sensitisers on lung function in patients with chronic obstructive pulmonary disease and diabetes. Int J Tuberc Lung Dis. 2010;14(3):362–7.
Sexton P, Metcalf P, Kolbe J. Respiratory effects of insulin sensitisation with metformin: a prospective observational study. COPD. 2014;11(2):133–42. doi:10.3109/15412555.2013.808614.
Guazzi M, Oreglia I, Guazzi MD. Insulin improves alveolar-capillary membrane gas conductance in type 2 diabetes. Diabetes Care. 2002;25(10):1802–6.
Chance WW, Rhee C, Yilmaz C, Dane DM, Pruneda ML, Raskin P, et al. Diminished alveolar microvascular reserves in type 2 diabetes reflect systemic microangiopathy. Diabetes Care. 2008;31(8):1596–601. doi:10.2337/dc07-2323.
Ceglia L, Lau J, Pittas AG. Meta-analysis: efficacy and safety of inhaled insulin therapy in adults with diabetes mellitus. Ann Int Med. 2006;145(9):665–75.
Hotamisligil GS. Mechanisms of TNF-alpha-induced insulin resistance. Exp Clin Endocrinol Diabetes. 1999;107(2):119–25. doi:10.1055/s-0029-1212086.
Mancuso P. Obesity and lung inflammation. J Appl Physiol. 2010;108(3):722–8. doi:10.1152/japplphysiol.00781.2009.
Broekhuizen R, Vernooy JH, Schols AM, Dentener MA, Wouters EF. Leptin as local inflammatory marker in COPD. Res Med. 2005;99(1):70–4.
Bruno A, Chanez P, Chiappara G, Siena L, Giammanco S, Gjomarkaj M, et al. Does leptin play a cytokine-like role within the airways of COPD patients? Eur Respir J. 2005;26(3):398–405. doi:10.1183/09031936.05.00092404.
Yang YM, Sun TY, Liu XM. The role of serum leptin and tumor necrosis factor-alpha in malnutrition of male chronic obstructive pulmonary disease patients. Chinese Med J. 2006;119(8):628–33.
Kythreotis P, Kokkini A, Avgeropoulou S, Hadjioannou A, Anastasakou E, Rasidakis A, et al. Plasma leptin and insulin-like growth factor I levels during acute exacerbations of chronic obstructive pulmonary disease. BMC Pulmonary Medicine. 2009;9:11. doi:10.1186/1471-2466-9-11.
Miller M, Cho JY, Pham A, Ramsdell J, Broide DH. Adiponectin and functional adiponectin receptor 1 are expressed by airway epithelial cells in chronic obstructive pulmonary disease. J Immunol. 2009;182(1):684–91.
Yoon HI, Li Y, Man SF, Tashkin D, Wise RA, Connett JE, et al. The complex relationship of serum adiponectin to COPD outcomes COPD and adiponectin. Chest. 2012;142(4):893–99. doi:10.1378/chest.11-2173.
Barth E, Albuszies G, Baumgart K, Matejovic M, Wachter U, Vogt J, et al. Glucose metabolism and catecholamines. Crit Care Med. 2007;35(9 Suppl):S508–18. doi:10.1097/01.CCM.0000278047.06965.20.
Bratel T, Wennlund A, Carlstrom K. Impact of hypoxaemia on neuroendocrine function and catecholamine secretion in chronic obstructive pulmonary disease (COPD). Effects of long-term oxygen treatment. Res Med. 2000;94(12):1221–8. doi:10.1053/rmed.2000.0953.
Kalupahana NS, Moustaid-Moussa N. The renin-angiotensin system: a link between obesity, inflammation and insulin resistance. Obes Rev. 2012;13(2):136–49. doi:10.1111/j.1467-789X.2011.00942.x.
Karin M, Yamamoto Y, Wang QM. The IKK NF-kappa B system: a treasure trove for drug development. Nat Rev Drug Discov. 2004;3(1):17–26. doi:10.1038/nrd1279.
Agusti A, Morla M, Sauleda J, Saus C, Busquets X. NF-kappaB activation and iNOS upregulation in skeletal muscle of patients with COPD and low body weight. Thorax. 2004;59(6):483–7.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
PR: conceived, carried out and wrote the manuscript. GL: helped to draft and to critically revise the manuscript in particular the tables. DL: helped to conceive and draft the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Rogliani, P., Lucà, G. & Lauro, D. Chronic obstructive pulmonary disease and diabetes. COPD Res Pract 1, 3 (2015). https://doi.org/10.1186/s40749-015-0005-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40749-015-0005-y