Abstract
Purpose
The purpose of the study was to report on the current accuracy measures specific to 1.5-Tesla MRI of the knee in the patient population prone to injuries of the anterior cruciate ligament (ACL), the menisci, and the articular cartilage.
Methods
We accrued patients between January 2018 through August 2021 who underwent a preoperative MRI and were diagnosed with an articular cartilage injury either due to unevenness of articular cartilage in T2-weighted sequences or due to the irregularity of subchondral bone in T1-weighted sequences. All patients were treated arthroscopically. Sensitivity, specificity, and accuracy were calculated for the detection of ACL, meniscus, and cartilage injuries. A P-value of < 0.05 represented statistical significance.
Results
One-hundred and forty-seven cases which included 150 knee joints were enrolled in this study. The mean age at the time of surgery was 42.9 years-old. The sensitivity in the diagnosis of ACL injuries was significantly greater than that in the diagnosis of cartilage injuries (P = 0.0083). The ratios of the equality of operative indication in 6 recipient sites were found to be between 90.0% and 96.0%. The diagnostic critical point was within a 1 cm in diameter.
Conclusion
The diagnostic sensitivity in cartilage injuries was significantly lower than ones of ACL and meniscal injuries. The ratios of the equality of operative indication was determined to be between 90.0% and 96.0%, if we consider the unevenness of articular cartilage or the irregularity of subchondral bone.
Level of evidence
Level III, Prospective diagnostic cohort study.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Osteoarthritis (OA) in the knee is a progressive joint disease characterized by knee pain, disability and articular cartilage loss. Identifying structural features that precede clinically evident disease is critical for the implementation of early interventions to slow the disease trajectory [5]. Currently, plain radiography remains the gold standard for morphological assessment of OA, and radiographic joint space narrowing is used as the criterion for developing disease-modifying drugs. Joint space narrowing is only a crude marker for cartilage thinning and lacks significant sensitivity [15]. Magnetic resonance imaging (MRI), by contrast, enables direct view of cartilage volume. More importantly, MRI provides detailed information about early soft tissue structural changes which are not detectable on radiographs but are crucial for assessment of disease, monitoring the progression, and for treatment planning [8, 14].
Arthroscopy is considered the gold-standard for the diagnosis of internal knee pathologies in addition to being a minimally invasive surgical procedure for the treatment of intra-articular lesions [11]. Yet, as in all surgical procedures, it should be recommended judiciously for appropriate indications. Recently, MRI has become more widely used in the evaluation of intra-articular knee lesions [26], though initial studies were completed nearly 30 years ago [13]. The accuracy of MRI for knee articular cartilage lesions has become more controversial several contemporary studies reporting sensitivity as low as 15% and as high as 60% depending on the characteristics and locations of the lesions [25, 28, 34].
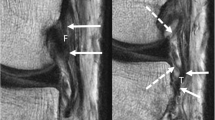
MRI findings consistent with articular cartilage injuries include the unevenness of articular cartilage with inflammatory effusion in T2-weighted sequences or the irregularity of subchondral bone in T1-weighted sequences (Fig. 1). T2-weighted images provide greater contrast between cartilage surfaces and effusions and can detect subtle changes such as fibrillation [17]. The purpose of the current study was to further identify and define measurements specific to 1.5-Tesla MRI of the knee in the patient population presenting with injuries likely to involve the anterior cruciate ligament (ACL), the menisci, and the articular cartilage. We hypothesized that MRI accuracy would lie between 80 to 90% for the menisci and ACL and would lie between 60 to 70% for the articular cartilage. We also hypothesized that the diagnostic critical point of cartilage injuries was at least 1 cm in diameter. This is a clinical study by the orthopaedic surgeons who were specialists of knee surgeries.
a The unevenness of articular cartilage with effusions in T2-weighted sequences in the right medial femoral condyle (arrow). b The arthroscopic view. The arrow showed cartilage injury in MFC. c The irregularity of subchondral bone in T1-weighted sequences in the right medial femoral condyle. d The arthroscopic view
Materials and methods
We enrolled all patients who underwent a diagnostic preoperative MRI followed by arthroscopy of the knee between January 2018 and August 2021 in this study. Inclusion criteria were as follows: (1) patient age older than 9 year, (2) primary knee arthroscopy, (3) MRI performed at the same institution, (4) time interval between the MRI scan and arthroscopy shorter than 3 months. Exclusion criteria were as follows: (1) revision arthroscopy, (2) arthroscopic-assisted fracture reduction surgery, and (3) multi-ligament knee surgery. The status of the ACL, the menisci, and the articular cartilage was collected from the surgical reports and from their respective preoperative MRI reports. Preoperative MRI reports were written by the knee specialist orthopaedic surgeon who examined his patients. All procedures were reviewed and approved by the research ethics committee of our hospital (KMC 13–20).
All MRI images were obtained on a clinical 1.5 T unit (Achieva, Royal Philips, Amsterdam, the Netherlands) using a standard receive-only 8-channel SENSE knee coil. The MRI used a 1.5-Tesla magnet and the standard protocol included the Turbo Spin Echo technique including proton density, T2- and T1-weighted sequences with fat suppression and Short Tau Inversion Recovery sequences with sagittal, coronal, and axial cuts. The MRI criteria used to define pathological lesions of the menisci and ACL were included the following. An intra-meniscal signal extending to an articular surface possibly including distortion of the normal meniscal shape representing a clinically meaningful tear [7], discontinuity of the ACL fibers, wavy appearance, and an angle of less than 45 degree between the distal ACL fibers and the tibia [26] representing a complete tear of ACL; one bruise at the anterior or central lateral femoral condyle and posterolateral tibial plateau with or without countercoup bone contusion at the posteromedial tibial plateau [26] are also secondary signs of an ACL tear.
The MRI criteria used to diagnose articular cartilage injuries included unevenness of articular cartilage with associated effusions in T2-weighted sequences and the irregularity of subchondral bone in T1-weighted sequences (Fig. 1). When evaluating the preoperative MRI, we diagnosed the articular cartilage injury grades in the classification of International Cartilage Repair Society (ICRS) [2], and the recipient area using a ruler in MRI. Six recipient sites were assessed in the following: medial femoral condyle (MFC), lateral femoral condyle (LFC), medial tibia (MT), lateral tibia (LT), trochlea (TR), and patella (P). We compared the preoperative MRI data with the arthroscopic data. We also calculated the simultaneous injuries ratio of cartilage in MFC and medial meniscus, and cartilage in LFC and lateral meniscus.
In ACL, meniscus and cartilage injuries, whether or not they were normal or abnormal, sensitivity {(true positive)/(true positive) + (false negative)}, specificity {(true negative)/(true negative) + (false negative)}, and accuracy {(true positive) + (true negative)/(total)} were calculated. In cartilage injuries, the ratio of diagnosing the same grade in ICRS classification was also calculated. Because the recipient sites with grade 3 or 4 of ICRS required cartilage reconstruction surgery such as autologous chondrocyte implantation or autologous osteochondral grafts [16, 27], we also measured the operative indication ratio which is defined as the diagnostic ratio between less than grade 2 and more than grade 3.
The Mann–Whitney U-test and the chi-square test were used to perform statistical analyses of the various scores. The level of statistical significance was set to a P value of < 0.05.
Results
One-hundred and forty-seven cases including 150 knee joints were enrolled in this study. There were 68 men and 79 women, 70 right knee joints and 80 left ones. The mean operative age was 42.9 years-old (range 9 to 81 years). Diagnosed diseases in this study are presented in Table 1. Normal cases existed 113 knees in medial meniscus, 91 knees in lateral knees and 105 knees in anterior cruciate ligament. The rates of ICRS classification in 6 recipient sites using arthroscopy are presented in Table 2. The most frequent site of abnormal findings in cartilage was the MFC. The most frequent site of injuries rated higher than a grade 3 was also the MFC, and the second site was the TR. The injuries in the medial meniscus were detected in 37 cases (24.7%), and the lateral meniscus injuries were detected in 59 cases (39.3%). The ratio of the cartilage injuries in the LFC was 18.6% in all of the cases of injuries in the lateral meniscus, and the ratio of the cartilage injuries in MFC was 59.5% in all cases of injuries of the medial meniscus.
The sensitivity, specificity, and accuracy of intra-articular structures are presented in Table 3, and those of the 6 recipient sites in articular cartilage are presented in Table 4. The sensitivity in ACL injuries was significantly higher than that in cartilage injuries (P = 0.0083), and the sensitivity in injuries of the medial meniscus (MM) was significantly higher than those in the cartilage injuries of MT (P = 0.0465) and P (P = 0.0233). In cartilage injuries, the sensitivity in MFC (P = 0.0697) and LT (P = 0.0640) were both higher than that in P. There were no significant differences in specificity and accuracy.
The ratios of the ICRS grade equality in 6 recipient sites are presented in Table 5. The ratios were determined to be between 72.7% and 89.3%. The ratios of the equality of operative indication in 6 recipient sites are presented in Table 6. The ratios were found to be between 90.0% and 96.0%. There were no significant differences in the sites of the both of the above ratios. In cartilage injuries, discrepant cases of operative indication were found in 50 recipient sites, and the surgical findings documented an area of injury of less than 1 cm diameter in 45 cases (90%). The recipient sites and areas of injury in another 5 cases were documented as follows: 15 × 20 mm in LFC (MRI grade 0, arthroscopy grade 4), 12 × 20 mm in MT (MRI grade 3, arthroscopy grade 2), 20 × 30 mm in TR (MRI grade 0, arthroscopy grade 3), 11 × 18 mm in TR (MRI grade 0, arthroscopy grade 4), and 15 × 20 mm in TR (MRI grade 2, arthroscopy grade 3). Our findings suggest that the diagnostic critical point of cartilage injuries was 1 cm in diameter, with injuries smaller than 1 cm being inconsistently detected on MRI.
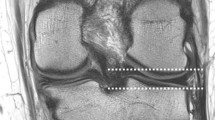
The preoperative oversight case was shown in Fig. 2. This patient was 61 years-old, and was experiencing left knee pain with a catching sensation. We diagnosed a lateral meniscal tear and suspected the cartilage would appear to be normal. His arthroscopy revealed an 11 × 18 mm grade 4 trochlear cartilage injury (Fig. 2a), and a 10 × 10 mm grade 3 cartilage injury on the LFC (Fig. 2b). Retrospective review of his preoperative MRI showed unevenness of the articular cartilage with effusions in T2-weighted sequences in TR (Fig. 2c) and LFC (Fig. 2d). These changes were not read by the original doctor and are considered to be a reading oversight.
The oversight in the preoperative MRI case. a The arthroscopy showed 11 × 18 mm grade 4 cartilage injury in the trochlea. b The arthroscopy showed 10 × 10 mm grade 3 cartilage injury in the lateral femoral condyle. c His preoperative MRI showed the unevenness of articular cartilage with associated effusions in T2-weighted sequences in the trochlea. d His preoperative MRI showed the unevenness of articular cartilage with associated effusions in T2-weighted sequences in the lateral femoral condyle
Discussion
The summary of this study was in the following: 147 cases and 150 knee joints were enrolled in this study. We compared their preoperative MRI to the surgical findings of their knee arthroscopy. Preoperative MRIs found to have unevenness of articular cartilage along with the finding of inflammatory edema and effusions in T2-weighted sequences or irregularity of the subchondral bone in T1-weighted sequences (Fig. 1) were documented to have articular cartilage injuries. The sensitivity of MRI detection of ACL injuries was significantly higher than that in cartilage injuries (P = 0.0083), and the sensitivity in injuries of the MM was significantly higher than those in cartilage injuries of MT (P = 0.0465) and P (P = 0.0233). Regarding cartilage injuries, the sensitivity in MFC (P = 0.0697) and LT (P = 0.0640) were consistently higher than that in P. The ratios of the ICRS grade equality in 6 recipient sites were determined to be between 72.7% and 89.3%. The ratios of the equality of operative indication in these same 6 recipient sites were measured between 90.0% and 96.0%. The critical detection point of cartilage injuries was found to be > = to 1 cm with injuries < 1 cm being more likely to be undetected on MRI.
Articular cartilage defects of the knee are frequently observed in most patient population. Prospective survey of 993 consecutive arthroscopic knee surgeries found articular cartilage pathology in 66% and a localized cartilage defect in 20% of the patients. Most lesions were found to be isolated high-grade lesions located on the femur [1]. Hjelle reported on articular cartilage defects in 1,000 consecutive knee arthroscopies. Focal chondral or osteochondral defects were found in 19% of the patients. The main focal chondral or osteochondral defect was found MFC in 58%, patella in 11%, LT in 11%, LFC in 9%, trochlea in 6%, and MT in 5%. [18]. Jones reported the most frequent lesion location as being the MFC [20]. Souza also reported that the MFC had the highest incidence of cartilage defects, and a high incidence of MM lesions was observed in subjects without MFC lesions [33]. In our study, the articular cartilage pathology existed in 22% of patients, and the most frequent lesion detected involved the MFC, which is consistent with the previous studies.
Fritz reported MRI findings of cartilage derangements in the following [12]: early chondral degeneration, cracks or fissures, chondral defects, the geographic appearance of a loose body, and osteochondral lesions. Early chondral degeneration appears on MRI as low signal intensity or high signal intensity chondral tissue that has lost the normal stratified and layered appearance. Cracks or fissures are commonly seen in the surface of articular cartilage and may be well seen with MRI as well as with arthroscopy. Chondral defects are recognized on MRI as fluid extending into and replacing the articular cartilage. The diagnosis of a chondral defect seen on MRI should prompt a search for associated loose bodies. Osteochondral lesions in the knee can be detected and well characterized with MRI without the need for special pulse sequences. Chang insisted that MRI evaluated the thickness and congruity of the articular surface in suspected articular cartilage injuries [4]. Kijowski reported that higher grades of articular cartilage defects are frequently associated with a greater depth and cross-sectional area of subchondral bone marrow edema [21]. We diagnosed articular cartilage injuries in MRI exhibiting unevenness of articular cartilage and associated inflammatory edema or effusions in T2-weighted sequences or in those exhibiting irregularity of subchondral bone in T1-weighted sequences. Other studies have reported on the diagnosis of cartilage degeneration with MRI. T1 rho and T2 MRI are complementary and reproducible methods for quantitatively and noninvasively monitoring regeneration [19]. T2 values increase with the increasing grade of cartilage damage and have a statistically significant positive correlation with ICRS scores [32].
Comparing the sensitivity of the recipient sites to preoperative MRI findings in diagnosing cartilage injuries, Danieli reported that the sensitivity of MRI was 76.4% (patella), 88.2% (trochlea), 69.7% (MFC), 85.7% (MT), 81.8% (LFC) and 75% (lateral plateau) [6]. Cartilage injuries affecting the MFC or the medial patellar facet were frequently missed by MRI [38]. Svard reported that modulus and T2 weighted images showed significant topographical variation. In the anterior medial condyle the modulus showed a negative association with the presence of an injury [36]. In an ACL-reconstructed knee, T2 values of the cartilage of the central aspect of the MFC at the 2-year follow-up were significantly elevated compared with native control knees [35]. In our study, the sensitivity, specificity and accuracy regarding injuries located on the MFC were higher than for injuries at other sites.
MRI appears to be less accurate than arthroscopy in diagnosing low-grade lesions particularly femorotibial lesions but is nearly equivalent to arthroscopy for high-grade lesions [10, 24]. T2 mapping can be useful for detecting moderate or severe cartilage damage, and the apparent diffusion coefficient can be used to detect early stage cartilage damage [37]. For grade III and IV lesions, 3-T MRI combined with three-dimensional double-echo steady-state cartilage-specific sequences represents an accurate diagnostic tool. For grade II lesions, the technique demonstrates moderate sensitivity, while for grade I lesions, the sensitivity is quite low [23]. MRI accuracy correlated negatively with patient age for articular cartilage damage when compared to arthroscopic findings [22]. MRI underestimated the defect area by an average of 70% compared with arthroscopic visualization [3]. No prior reports have discussed or determined the diagnostic threshold of MRIs for detecting injuries. The ratios for the equality of surgical indications based on surgery versus MRI were calculated to be between 90.0% and 96.0%, when unevenness of articular cartilage with concurrent inflammatory edema or effusions and the irregularity of subchondral bone are considered. The MRI threshold for detecting injuries consistently was 1 cm in longest diameter.
The sensitivity and specificity of MRI were found to be 87% and 93%, respectively, for ACL tears; 89% and 88%, for MM tears, and 78% and 95%, for lateral meniscus tears [29]. In a pediatric adolescent patient, the sensitivity and the specificity of 3 T MRI were 81% and 90.9% for MM injuries, 68.8% and 93% for lateral meniscus injuries, and 97.9% and 98.6% for ACL injuries, respectively [31]. Eijgenraam reported that the strongest correlation between MRI findings and radiographic OA was found in the medial femoral cartilage and the weakest correlation was found in the anterior horn of the MM [9]. Koch insisted that the highest accuracy was observed in MM and in ACL findings [22]. Porter reported that MRI was less accurate than clinical assessment for the diagnosis of lateral meniscal tears [30]. In our study, the sensitivity in MRI detection of ACL injuries was significantly higher than that in MRI detection of any cartilage injuries in any location of the cartilage, and the sensitivity in MRI detection of injuries in the MM was significantly higher than those in the cartilage injuries of MT and P.
One limitation of our study was the modest number of cases (147 cases and 150 knees). A second limitation is that this is a single institution study and a future multi-institutional study is warranted.
In conclusion, the diagnostic sensitivity of MRI in the detection of cartilage injuries was significantly lower than the sensitivity in the detection of ACL and meniscal injuries. The ratios of the equality of operative indication was determined to be between 90.0% and 96.0%, if we consider the unevenness of articular cartilage or the irregularity of subchondral bone. The diagnostic threshold for MRI was 1 cm in longest dimension which makes it effective as a diagnostic tool in clinical practice.
Availability of data and materials
Our findings suggest that the diagnostic critical point of cartilage injuries was 1 cm in diameter, with injuries smaller than 1 cm being inconsistently detected on MRI.
References
Aroen A, Loken S, Heir S et al (2004) Articular cartilage lesions in 993 consecutive knee arthroscopies. Am J Sports Med 32:211–215
Brittberg M, Aglietti A, Gambardella R, et al. (2000) ICRS cartilage injury evaluation package. http://www.cartilage.org/
Campbell AB, Knopp MV, Kolovich GP et al (2013) Preoperative MRI underestimates articular cartilage defect size compared with findings at arthroscopic knee surgery. Am J Sports Med 41(3):590–595
Chang GC, Sherman O, Madelin G, Recht M, Regatte R (2011) MR imaging assessment of articular cartilage repair procedures. Magn Reson Imaging Clin N Am 19(2):323–337
Chu CR, Williams AA, Coyle CH, Bowers ME (2012) Early diagnosis to enable early treatment of pre-osteoarthritis. Arthritis Res Ther 14:212
Danieli MV, Guereiro JPF, Queiroz AO et al (2016) Diagnosis and classification of chondral knee injuries: comparison between magnetic resonance imaging and arthroscopy. Knee Surg Spoerts Traumatol Arthrosc 24(5):1627–1633
De Smet AA (2012) How I diagnose meniscal tears on knee MRI. AJR Am J Roentgenol 199:481–499
Ding C, Cicuttini F, Jones G (2008) How important is MRI for detecting early osteoarthritis? Ccuracy of diagnosies Nat Clin Pract Rheumatol 4:4–5
Eijgenraam SM, Chaudhari AS, Reijman M et al (2020) Time-saving opportunities in knee osteoarthritis: T2 mapping and structural imaging of the knee using a single 5-min MRI scan. Eur Radiol 30:2231–2240
Figueroa D, Calvo R, Vaisman A, Carrasco MA, Moraga C, Delgado I (2007) Knee chondral lesions: incidence and correlation between arthroscopic and magnetic resonance findings. Arthroscopy 23(3):312–315
Fischer SP, Fox JM, Del Pizzo W, Friedman MJ, Snyder SJ, Ferkel RD (1991) Accuracy of diagnoses from magnetic resonance imaging of the knee. A multi-center analysis of one thousand and fourteen patients. J Bone Joint Surg Am 73:2–10
Fritz RC, Chaudhari A, Boutin RD (2020) Preoperative MRI of articular cartilage in the knee: A practical approach. J Knee Surg 33(11):1088–1099
Gelb HJ, Glasgow SG, Sapega AA, Torg JS (1996) Magnetic resonance imaging of knee disorders. Am J Sports Med 24:99–103
Guermazi A, Burstein D, Conaghan P et al (2008) Imaging in osteoarthritis. Rheum Dis Clin N Am 34:645–687
Guermazi A, Roemer FW, Burstein D, Hayashi D (2011) Why radiography should no longer be considered a surrogate outcome measure for longitudinal assessment of cartilage in knee osteoarthritis. Arthritis Res Ther 13:247
Hangody L, Dobos J, Balo E, Panics G, Hangody LR, Berkes I (2010) Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17-year prospective multicenter study. Am J Sport Med 38:1125–1133
Hayashi D, Li X, Murakami AM, Roemer FW, Trattnig S, Guermazi A (2018) Understanding magnetic resonance imaging of knee cartilage repair: A focus on clinical relevance. Cartilage 9(3):223–236
Hjelle K, Solheim E, Strand T, Muri R, Brittberg M (2002) Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy 18(7):730–734
Holtzman DJ, Theologis AA, Carballido-Gamio J, Majumdar S, Li X, Ma CB (2010) T1rho and T2 quantitative magnetic resonance imaging analysis of cartilage regeneration following microfracture and mosaicplasty cartilage resurfacing procedures. J Mgn Reson Imaging 32(4):914–923
Jones KJ, Sheppard WL, Arshi A, Hinckel BB, Sherman SL (2019) Articular cartilage lesion characteristic reporting is highly variable in clinical outcomes studies of the knee. Cartilage 10(3):299–304
Kijowski R, Stanton P, Fine J, Smet AD (2006) Subchondral bone marrow edema in patients with degeneration of the articular cartilage of the knee joint. Radiology 238(3):943–949
Koch JEJ, Ben Elyahu R, Khateeb B et al (2021) Accuracy measures of 1.5 tesla MRI for the diagnosis of ACL, meniscus and articular knee cartilage damage and characteristics of false negative lesions: a level III prognostic study. BMC Musculoskeletal Disorders 22:124. https://doi.org/10.1186/s12891-021-0401-3
Kohl S, Meier S, Ahmad SS et al (2015) Accuracy of cartilage-specific 3-Tesla 3D-DESS magnetic resonance imaging in the diagnosis of chondral lesions: comparison with knee arthroscopy. J Orthop Surg Res 10:191. https://doi.org/10.1186/s13018-015-326-1
Macarini L, Murrone M, Marini S, Mariano M, Zaccheo N, Moretti B (2003) MR in the study of knee cartilage pathologies: influence of location and grade on the effectiveness of the method. Radiol Med 105(4):296–307
Mori R, Ochi M, Sakai Y, Adachi N, Uchio Y (1999) Clinical significance of magnetic resonance imaging (MRI) for focal chondral lesions. Magn Reason Imaging 17:1135–1140
Nacey NC, Geeslin MG, Millar GW, Pierce JL (2017) Magnetic resonance imaging of the knee: an overview and update of conventional and state of the art imaging. J Magn Reason Imaging 45:1257–1275
Nakagawa Y, Mukai S, Nishitani K et al (2022) Autologous osteochondral grafts result in improved clinical outcomes in patients with early knee osteoarthritis. ASMAR 4(2):e713-719
Ochi M, Sumen Y, Kanda T, Ikuta Y, Itoh K (1994) The diagnostic value and limitation of magnetic resonance imaging on chondral lesions in the knee joint. Arthroscopy 10:176–183
Phelan N, Rowland P, Galvin R, O’Byrne JM (2016) A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthrosc 24(5):1525–1539
Porter M, Shadbolt B (2021) Accuracy of standard magnetic resonance imaging sequences for meniscal and chondral lesions versus knee arthroscopy. A prospective case-controlled study of 719 cases. ANZ J Surg 91(6):1284–1289
Schub DL, Altahawi F, Meisel AF, Winalski C, Parker RD, Sluan PM (2012) Accuracy of 3-Tesla magnetic resonance imaging for the diagnosis of intra-articular knee injuries in children and teenagers. J Pediatr Orthop 32(8):765–769
Soellner ST, Goldmann A, Muelheims D, Welsch GH, Pachowsky ML (2017) Intraoperative validation of quantitative T2 mapping in patients with articular cartilage lesions of the knee. Osteoarthritis Cartilage 25:1841–1849
Souza RB, Feeley BT, Zarins ZA, Link TM, Li X, Majumdar S (2013) T1rho MRI relaxation in knee OA subjects with varying sizes of cartilage lesions. Knee 20(2):113–119
Speer KP, Sprinzer CE, Goldner JL, Garrett WE Jr (1991) Magnetic resonance imaging of traumatic knee articular cartilage injuries. Am J Sports Med 19:396–402
Su F, Hilton JF, Nardo L et al (2013) Cartilage morphology and T1rho and T2 quantification in ACL-reconstructed knees: a 2-year follow-up. Osteoarthritis Cartilage 21:1058–1067
Svard T, Lakovaara M, Pkarinen H et al (2018) Quantitative MRI of human cartilage in vitro: relationship with arthroscopic indentation stiffness and defect severity. Cartilage 9(1):46–54
Ukai T, Sato M, Yamashita T et al (2015) Diffusion tensor imaging can detect the early stages of cartilage damage: a comparison study. BMC Musculoskelet Disord 16:35. https://doi.org/10.1186/s12891-015-1499-0
Wong KPL, Han AXY, Wong JLY, Lee DYH (2017) Reliability of magnetic resonance imaging in evaluating meniscal and cartilage injuries in anterior cruciate ligament-deficient knees. Knee Surg Spoerts Traumatol Arthrosc 25(2):411–417
Declarations
This manuscript has not been submitted or is not simultaneously being submitted elsewhere.
Funding
Financial Support of our article is none.
Author information
Authors and Affiliations
Contributions
The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Potential Conflicts of Interest of our article is none.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakagawa, Y., Mukai, S., Sakai, S. et al. Preoperative diagnosis of knee cartilage, meniscal, and ligament injuries by magnetic resonance imaging. J EXP ORTOP 10, 47 (2023). https://doi.org/10.1186/s40634-023-00595-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-023-00595-y