Abstract
Purpose
To determine the diagnostic accuracy of magnetic resonance imaging (MRI) and ultrasound (US) in the diagnosis of anterior cruciate ligament (ACL), medial meniscus and lateral meniscus tears in people with suspected ACL and/or meniscal tears.
Methods
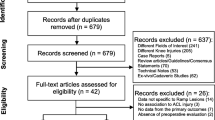
MEDLINE, Web of Science and the Cochrane library were searched from inception to March 2014. All prospective studies of the diagnostic accuracy of MRI or US against arthroscopy as the reference standard were included in the systematic review. Studies with a retrospective design and those with evidence of verification bias were excluded. Methodological quality of included studies was assessed using the QUADAS-2 tool. A meta-analysis of studies evaluating MRI to calculate the pooled sensitivity and specificity for each target condition was performed using a bivariate model with random effects. Sub-group and sensitivity analysis were used to examine the effect of methodological and other study variables.
Results
There were 14 studies included in the meta-analysis of the accuracy of MRI for ACL tears, 19 studies included for medial meniscal tears and 19 studies for lateral meniscal tears. The summary estimates of sensitivity and specificity of MRI were 87 % (95 % CI 77–94 %) and 93 % (95 % CI 91–96 %), respectively, for ACL tears; 89 % (95 % CI 83–94 %) and 88 % (95 % CI 82–93 %), respectively, for medial meniscal tears; and 78 % (95 % CI 66–87 %) and 95 % (95 % CI 91–97 %), respectively, for lateral meniscal tears. Magnetic field strength had no significant effect on accuracy. Most studies had a high or unclear risk of bias. There were an insufficient number of studies that evaluated US to perform a meta-analysis.
Conclusion
This study provides a systematic review and meta-analysis of diagnostic accuracy studies of MRI and applies strict exclusion criteria in relation to the risk of verification bias. The risk of bias in most studies is high or unclear in relation to the reference standard. Concerns regarding the applicability of patient selection are also present in most studies.
Level of evidence
III.





Similar content being viewed by others
References
Adalberth T, Roos H, Lauren M, Akeson P, Sloth M, Jonsson K, Lindstrand A, Lohmander LS (1997) Magnetic resonance imaging, scintigraphy, and arthroscopic evaluation of traumatic hemarthrosis of the knee. Am J Sports Med 25(2):231–237
Alizadeh A, Babaei Jandaghi A, Keshavarz Zirak A, Karimi A, Mardani-Kivi M, Rajabzadeh A (2013) Knee sonography as a diagnostic test for medial meniscal tears in young patients. Eur J Orthop Surg Traumatol 23(8):927–931
Arastu MH, Grange S, Twyman R (2015) Prevalence and consequences of delayed diagnosis of anterior cruciate ligament ruptures. Knee Surg Sports Traumatol Arthrosc 23(4):1201–1205
Arif U, Shah ZA, Khan MA, Ijaz M, Qayum H (2013) Diagnostic accuracy of 1.5 tesla MRI in the diagnosis of meniscal tears of knee joint. Pak J Med Health Sci 7(1):227–230
Behairy NH, Dorgham MA, Khaled SA (2009) Accuracy of routine magnetic resonance imaging in meniscal and ligamentous injuries of the knee: comparison with arthroscopy. Int Orthop 33(4):961–967
Billington J, Fahey T, Galvin R (2012) Diagnostic accuracy of the STRATIFY clinical prediction rule for falls: a systematic review and meta-analysis. BMC Fam Pract 13:76
Bui-Mansfield LT, Youngberg RA, Warme W, Pitcher JD, Nguyen PLL (1997) Potential cost savings of MR imaging obtained before arthroscopy of the knee: evaluation of 50 consecutive patients. Am J Roentgenol 168(4):913–918
Chissell HR, Allum RL, Keightley A (1994) MRI of the knee: its cost-effective use in a district general hospital. Ann R Coll Surg Eng 76(1):26–29
Crawford R, Walley G, Bridgman S, Maffulli N (2007) Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull 84(1):5–23
De Smet AA (2012) How I diagnose meniscal tears on knee MRI. Am J Roentgenol 199(3):181–499
de Vet HCW, Eisinga A, Riphagen II, Aertgeerts B,Pewsner D, Mitchell R (2008) Chapter 7: Searching for studies. In: Deeks JJ, Bossuyt PM, Gatsonis C (eds) Cochrane handbook for systematic reviews of diagnostic test accuracy version 0.4 [Updated Sept 2008] The Cochrane Collaboration
Franklin PD, Lemon RA, Barden HS (1997) Accuracy of imaging the menisci on an in-office, dedicated, magnetic resonance imaging extremity system. Am J Sports Med 25(3):382–388
Glashow JL, Katz R, Schneider M, Scott WN (1989) Double-blind assessment of the value of magnetic resonance imaging in the diagnosis of anterior cruciate and meniscal lesions. J Bone Joint Surg Am 1:113–119
Grevitt MP, Pool CJ, Bodley RN, Savage PE (1992) Magnetic resonance imaging of the knee: initial experience in a district general hospital. Injury 23(6):410–412
Harbord RM, Whiting P (2009) Metandi: meta-analysis of diagnostic accuracy using hierarchical logistic regression. Stata J 9(2):211–229
Health Information and Quality Authority of Ireland (2014) Health Technology Assessment of Scheduled Procedures Knee Arthroscopy. www.hiqa.ie/system/files/Draft-Knee-Arthroplasty.pdf Accessed 13 Jan 2015
Jah AAE, Keyhani S, Zarei R, Moghaddam AK (2005) Accuracy of MRI in comparison with clinical and arthroscopic findings in ligamentous and meniscal injuries of the knee. Acta Orthop Belg 71(2):189–196
Jung JY, Yoon YC, Kwon JW, Ahn JH, Choe B-K (2009) Diagnosis of internal derangement of the knee at 3.0-T MR imaging: 3D isotropic intermediate-weighted versus 2D sequences. Radiology 253(3):780–787
Khan Z, Faruqui Z, Ogyunbiyi O, Rosset G, Iqbal J (2006) Ultrasound assessment of internal derangement of the knee. Acta Orthop Belg 72(1):72–76
Kinnunen J, Bondestam S, Kivioja A, Ahovuo J, Toivakka SK, Tulikoura I, Karjalainen T (1994) Diagnostic performance of low-field MRI in acute knee injuries. Magn Reson Imaging 12(8):1155–1160
Krampla W, Roesel M, Svoboda K, Nachbagauer A, Gschwantler M, Hruby W (2009) MRI of the knee: how do field strength and radiologist’s experience influence diagnostic accuracy and interobserver correlation in assessing chondral and meniscal lesions and the integrity of the anterior cruciate ligament? Eur Radiol 19(6):1519–1528
Mather RC 3rd, Garrett WE, Cole BJ, Hussey K, Bolognesi MP, Lassiter T, Orlando LA (2015) Cost-effectiveness analysis of the diagnosis of meniscus tears. Am J Sports Med 43(1):128–137
McConkey MO, Bonasia DE, Amendola A (2011) Pediatric anterior cruciate ligament reconstruction. Curr Rev Musculoskelet Med 4(2):37–44
Miller GK (1996) A prospective study comparing the accuracy of the clinical diagnosis of meniscus tear with magnetic resonance imaging and its effect on clinical outcome. Arthroscopy 12(4):406–413
Munk B, Madsen F, Lundorf E, Staunstrup H, Schmidt SA, Bolvig L, Hellfritzsch MB, Jensen J (1998) Clinical magnetic resonance imaging and arthroscopic findings in knees: a comparative prospective study of meniscus anterior cruciate ligament and cartilage lesions. Arthroscopy 14(2):171–175
Munshi M, Davidson M, MacDonald PB, Froese W, Sutherland K (2000) The efficacy of magnetic resonance imaging in acute knee injuries. Clin J Sport Med 10(1):34–39
Niitsu M, Anno I, Fukubayashi T, Shimojo H, Kuno S, Akisada M (1991) Tears of cruciate ligaments and menisci: evaluation with cine MR imaging. Radiology 178(3):859–864
Nishikawa H, Imanaka Y, Sekimoto M, Ikai H (2010) Verification bias in assessment of the utility of MRI in the diagnosis of cruciate ligament tears. Am J Roentgenol 195(5):W357–W364
Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Myriam Hunink MG (2003) MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology 226(3):837–848
Perera NS, Joel J, Bunola JA (2013) Anterior cruciate ligament rupture: delay to diagnosis. Injury 44(12):1862–1865
Polly DW Jr, Callaghan JJ, Sikes RA, McCabe JM, McMahon K, Savory CG (1988) The accuracy of selective magnetic resonance imaging compared with the findings of arthroscopy of the knee. J Bone Joint Surg Am 70(2):192–198
Rappeport ED, Wieslander SB, Stephensen S, Lausten GS, Thomsen HS (1997) MRI preferable to diagnostic arthroscopy in knee joint injuries: a double-blind comparison of 47 patients. Acta Orthop Scand 68(3):277–281
Raunest J, Oberle K, Loehnert J, Hoetzinger H (1991) The clinical value of magnetic resonance imaging in the evaluation of meniscal disorders. J Bone Joint Surg Am 73(1):11–16
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58(10):982–990
Richardson ML, Petscavage JM (2011) Verification bias: an under-recognized source of error in assessing the efficacy of MRI of the meniscii. Acad Radiol 18(11):1376–1381
Riel KA, Reinisch M, Kersting-Sommerhoff B, Hof N, Merl T (1999) 0.2-Tesla magnetic resonance imaging of internal lesions of the knee joint: a prospective arthroscopically controlled clinical study. Knee Surg Sports Traumatol Arthrosc 7(1):37–41
Sampson MJ, Jackson MP, Moran CJ, Moran R, Eustace SJ, Shine S (2008) Three Tesla MRI for the diagnosis of meniscal and anterior cruciate ligament pathology: a comparison to arthroscopic findings. Clin Radiol 63(10):1106–1111
Sica GT (2006) Bias in research studies. Radiology 238(3):780–789
Sladjan T, Zoran V, Zoran B (2014) Correlation of clinical examination, ultrasound sonography, and magnetic resonance imaging findings with arthroscopic findings in relation to acute and chronic lateral meniscus injuries. J Orthop Sci 19(1):71–76
Smith TO, Lewis M, Song F, Toms AP, Donell ST, Hing CB (2012) The diagnostic accuracy of anterior cruciate ligament rupture using magnetic resonance imaging: a meta-analysis. Eur J Orthop Surg Traumatol 22(4):315–326
Spiers AS, Meagher T, Ostlere SJ, Wilson DJ, Dodd CA (1993) Can MRI of the knee affect arthroscopic practice? A prospective study of 58 patients. J Bone Joint Surg Br 75(1):49–52
Van Dyck P, Vanhoenacker FM, Lambrecht V, Wouters K, Gielen JL, Dossche L, Parizel PM (2013) Prospective comparison of 1.5 and 3.0-T MRI for evaluating the knee menisci and ACL. J Bone Joint Surg Am 95(10):916–924
von Engelhardt LV, Schmitz A, Pennekamp PH, Schild HH, Wirtz DC, von Falkenhausen F (2008) Diagnostics of degenerative meniscal tears at 3-Tesla MRI compared to arthroscopy as reference standard. Arch Orthop Trauma Surg 128(5):451–456
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536
Yao L, Gentili A, Petrus L, Lee JK (1995) Partial ACL rupture: an MR diagnosis? Skeletal Radiol 24(4):247–251
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Appendices
Appendix 1: Search strategies
MEDLINE (PubMed)
((Ultrasonography [mh] OR ultrasound [56] OR ultrasonograph* [56]) OR (Magnetic Resonance Imaging [mh] | Index tests set |
OR MR imag*[56] OR magnetic resonance imag* [56] OR MRI [56])) OR | |
(Arthroscopy [mh] OR arthroscop* [56]) AND | Reference standard set |
(Menisci, Tibial [mh] OR Medial Meniscus [mh] OR medial menisc* [56] OR Lateral Meniscus [mh] OR lateral menisc* [56] OR meniscal [56] OR Anterior Cruciate Ligament [mh] OR anterior cruciate ligament* [56] OR ‘ACL’ [56]) AND (Knee injuries [mh] OR Cartilage, articular/injuries [mh] OR Cartilage, articular/surgery [mh] OR Rupture [mh:noexp] OR tear [56] OR tears [56] OR torn [56] OR thickness [56] OR repair [56] OR lesion [56] OR lesions [56] OR rupture [56] OR acute knee [56] OR abnormal*[56] OR pain[56] OR painful[56]) | Target conditions set |
EMBASE (Elsevier)
1 ‘echography’/de AND [embase]/lim (157490) | Index tests set |
2 ultrasound:ab,ti OR ultrasonograph*:ab,ti OR sonograp*:ab,ti AND [embase]/lim (264425) | |
3 #1 OR #2 (327246) | |
4 ‘nuclear magnetic resonance imaging’/de AND [embase]/lim (398985) | |
5 ((‘magnetic resonance’ OR mr) NEAR/3 imag*):ab,ti AND [embase]/lim (182022) | |
6 mri:ab,ti AND [embase]/lim (179599) | |
7 #4 OR #5 OR #6 (453055) | |
8 #7 OR #3 (739416) | |
9 arthroscopy/de OR arthroscop*:ab,ti AND [embase]/lim | Reference standard set |
10 #8 OR #9 | |
11 Knee AND meniscus/de AND [embase]/lim | Target condition set |
12 medial menis* AND [embase]/lim (3819) | |
13 lateral menis* AND [embase]/lim (3819) | |
14 meniscal [embase]/lim | |
15 ‘Anterior Cruciate Ligament’ (15713) | |
16 ((anterior adj2 cruciate$ adj2 ligament$) OR ACL) (11589) | |
17 #11 OR #12 OR #13 OR #14 OR #15 OR #16 (22229) | |
18 ‘knee injury’/de AND [embase]/lim | |
19 (acute NEAR/4 knee):ab,ti AND [embase]/lim | |
20 ‘anterior cruciate ligament rupture’/de AND [embase]/lim | |
21 ‘Cartilage injury’/de OR ‘knee meniscus rupture’/de AND [embase]/lim | |
22 tear:ab,ti OR tears:ab,ti OR torn:ab,ti OR thickness:ab,ti OR lesion:ab,ti OR rupture:ab,ti OR ruptured:ab,ti OR ruptures:ab,ti OR injur*:ab,ti OR repair:ab,ti OR abnormal*:ab,ti OR pain:ab,ti OR painful:ab,ti AND [embase]/lim (1316333) |
Appendix 2: QUADAS-2
Modifications underlined.
Phase 1: State the review question:
Patients
Index test(s)
Reference standard and target condition
Phase 2: Draw a flow diagram for the primary study
Phase 3: Risk of bias and applicability judgements
Quadas-2 is structured so that 4 key domains are each rated in terms of the risk of bias and the concern regarding applicability to the research question (as defined above). Each key domain as a set of signalling questions to help reach the judgements regarding bias and applicability.
Domain 1: patient selection
-
(A)
Risk of bias
-
1.
Describe methods of patient selection
-
2.
Was a consecutive or random sample of patients enrolled? (Yes/No/Unclear)
-
3.
Was a case–control design avoided? (Yes/No/Unclear)
-
4.
Did the study avoid inappropriate exclusions? (Yes/No/Unclear)
-
1.
Could the selection of patients have introduced bias? | RISK: LOW/HIGH/UNCLEAR |
-
(B)
Applicability
-
1.
Describe included patients (prior testing, presentation, intended use of index test and setting)
-
2.
Is there concern that the included patients do not match the review question?
-
1.
CONCERN: LOW/HIGH/UNCLEAR
Domain 2: index test (MRI)
-
(A)
Risk of bias
Additional signalling questions underlined in following section.
-
1.
Describe the index test, and how it was conducted and interpreted
-
2.
Were MRI scans performed in the same hospital/centre ? (Yes/No/Unclear)
-
3.
Was the index test interpreted by a single radiologist without consensus opinion ? (Yes/No/Unclear)
-
4.
Were the index test results interpreted without knowledge of the results of the reference standard ? (Yes/No/Unclear)
-
5.
If a threshold was used, was it pre-specified? (Yes/No/Unclear)
-
6.
Could the conduct or interpretation of the index test have introduced bias ?
-
1.
RISK: LOW/HIGH/UNCLEAR
-
(B)
Applicability
-
1.
Is there concern that the index test, its conduct, or interpretation differ from the review question? CONCERN LOW/HIGH/UNCLEAR
-
1.
Domain 3: reference test (arthroscopy)
-
(A)
Risk of bias
Additional signalling question underlined in following section
Question 3. Omitted from assessment of bias
-
1.
Describe the reference standard, and how it was conducted and interpreted:
-
2.
Was the reference standard performed by a single surgeon? (Yes/No/Unclear)
-
3.
Is the reference standard likely to correctly classify the target condition? (Yes/No/Unclear)
-
4.
Were the reference standard results interpreted without knowledge of the results of the index test? (Yes/No/Unclear)
-
1.
Could the reference standard, its conduct, or its interpretation have introduced bias? | RISK: LOW/HIGH/UNCLEAR |
-
(B)
Applicability
-
1.
Are there concerns that the target condition as defined by the reference standard does not match the review question? CONCERN LOW/HIGH/UNCLEAR
-
1.
Domain 4: flow and timing
-
(A)
Risk of bias
-
1.
Describe any patients who did not receive the index test(s) and/or reference standard or who were excluded from the 2 × 2 table (refer to flow diagram)
-
2.
Describe the time interval and any interventions between index test(s) and reference standard:
-
3.
Was there an appropriate interval between index test(s) and reference standard? (Yes/No/Unclear)
-
4.
Did all patients receive a reference standard? (Yes/No/Unclear)
-
5.
Did patients receive the same reference standard? (Yes/No/Unclear)
-
6.
Were all patients included in the analysis? (Yes/No/Unclear)
-
1.
Could the patient flow have introduced Bias? RISK: LOW/HIGH/UNCLEAR
Appendix 3
Rights and permissions
About this article
Cite this article
Phelan, N., Rowland, P., Galvin, R. et al. A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthrosc 24, 1525–1539 (2016). https://doi.org/10.1007/s00167-015-3861-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3861-8