Abstract
Background
Meniscus allograft transplantation (MAT) is a surgical procedure performed in patients complaining post-meniscectomy syndrome. Although the effectiveness of MAT on knee stability has been already demonstrated in cadaveric studies, its biomechanical role has been poorly evaluated in-vivo.
Methods
A narrative review of the biomechanical effect of meniscectomy and MAT was performed. Furthermore, two cases were presented, of one patient who underwent Medial MAT and Anterior Cruciate Ligament (ACL) reconstruction, and one who underwent Lateral MAT. During the surgery, knee laxity was evaluated using a surgical navigation system.
Results
AP laxity and IE rotation were reduced of 25% to 50% at both 30° and 90° of knee flexion after MAT transplantation.
Discussion
In both cases, almost all the tests performed showed a reduction of knee laxity after meniscus transplant, when compared with pre-operative knee laxity. This assessment confirms the insights of previous in-vitro studies and underline a crucial role of MAT in knee biomechanics.
Similar content being viewed by others
Background
Menisci are an important structure of the knee and strongly contribute to different functions, such as load distribution, secondary stabilization of the knee, and tibiofemoral congruity (Ahmed & Burke, 1983; Haut Donahue et al., 2004; Levy et al., 1989; Levy et al., 1982; Markolf et al., 1981) . Meniscal lesions are one of the commonest injury worldwide, with an annual incidence of 60–70 per 100,000 inhabitants (Beals et al., 2016). Despite the common increasing trend of preserving the meniscus through sutures and repair, the meniscectomy is still the treatment of choice (Jacquet et al., 2019). Consequences of meniscectomy have been widely evaluated in the past.
Different studies demonstrated a correlation between meniscectomy and knee degeneration (Allen et al., 1984; Faunø & Nielsen, 1992; Scheller et al., 2001).
In long term follow-up (up to 22 years) 27% of patients who underwent meniscectomy developed symptomatic radiographic knee OA (corresponding to Kellgren/Lawrence grade > or = 2), with a relative risk of 2.6 times higher than the contralateral non-operated knee (Englund & Lohmander, 2004).
A systematic review performed by Petty (Petty & Lubowitz, 2011) found an higher rate of joint degeneration, up to 53%, compared with contralateral uninjured knee.
Meniscectomy is also associated with worse clinical outcomes, such as Lysholm scores, Tegner Activity Level, instability, and removal of lateral meniscus lead to increased instability and poor outcomes (Salata et al., 2010).
Meniscus Allograft Transplantation (MAT) has been proposed as a surgical option to treat patients with symptomatic total or subtotal meniscectomies, with the aim of reducing pain and improving knee function. Its satisfactory clinical results has been demonstrated in more than 40 studies and 1500 patients, (Rosso et al., 2015) often in combination with Anterior Cruciate Ligament (ACL) reconstruction. (Saltzman et al., 2017) Clinical scores confirm the effectiveness of MAT in contrasting the progression of knee osteoarthritis (Young et al., 2017). In patients with significantly arthritic knees, MAT in conjunction with articular cartilage repair may help to delay further surgical treatment by an average of 5 years (Stone et al., 2010).
However, MAT has also been suggested to have a relevant role in controlling knee laxities and thus protecting the ACL (Novaretti & Musahl, 2018). Nevertheless, the biomechanical effect of MAT has been mainly evaluated through cadaveric studies, and there is lack of in-vivo evaluations.
In this study, we first aim to review the biomechanical consequences of meniscectomy and MAT on knee stability. In order to do so, we focused on two main biomechanical parameters: contact stress, since its increase can lead to early OA (Dong et al., 2014); and knee laxity, since it is one of the principal indices of knee instability. Furthermore, we aim to offer an insight about the kinematic effect of either medial or lateral MAT, through an in-vivo kinematic acquisition with a navigation system.
Biomechanical consequence of meniscectomy
Contact stress
The weight-bearing role of the meniscus has been investigated in past (Maher et al., 2017). A greater attention has been focused on the effect of the either partial or total removal of the medial meniscus, since it is the mostly solicited during daily life activities.
Overall, the internal forces acting on the knee after meniscectomy significantly differ from the intact conditions. Knee biomechanics may result in an alteration of contact pressure and contact area. Baratz et al. (Baratz et al., 1986) showed a proportional increase of contact pressure (up to 110%) after partial-to-total meniscectomy in cadaver knees. In addition, contact area has been shown to decrease significantly (up to 75%) relating to the size of the damage. In particular, the peripheral portion of the menisci seems to contribute most to the changes in the knee contact stress (Lee et al., 2006).
As abnormal loading conditions may affect the integrity of the cartilage, meniscectomy is commonly considered as a risk factor for the beginning and the progression of osteoarthritis (Petty & Lubowitz, 2011). The direct contact between the cartilage layers may facilitate the damage of the collagen matrix and prolong the strain recovery. Thus, this may induce vascular invasion, dehydration and endochondral ossification (Song et al., 2008).
Laxity
The menisci have an important role in static and dynamic knee laxity. Numerous in vitro studies highlighted the importance of the menisci in reducing anterior tibial translation in the knee in different ACL conditions. (Allen et al., 2000; Hanley & Warren, 1987; Levy et al., 1989; Levy et al., 1982)
Removal of the medial meniscus has been reported to produce an increase of the strain on the ACL and to contribute to anterior-posterior (AP) laxity, when the ACL is intact (Spang et al., 2010). Compared to the normal condition, removal of almost 50% of the posterior horn of the medial meniscus increases anterior tibial translation and creates a posterior shift of the femur under axial compression (Arno et al., 2013). Through an in-vivo study, Yammine et al. (Yammine, 2013) showed how partial meniscectomy may induce significant immediate post-operative anterior tibial translation (up to 3 mm) even when ACL is not injured.
In an ACL-deficient knee, the effect of medial meniscus injury has been widely studied. A commonly accepted insight is that posterior horn tears (Ahn et al., 2011) or posterior root tears increase AP tibial translation, especially when the knee is flexed 0–60 degrees.
Lorbach et al. (Lorbach et al., 2015) demonstrated that partial or total medial meniscectomy significantly altered AP translation and pivot-shift in the ACL-deficient knee in cadaveric specimens, while meniscal repair effectively restored the intact meniscus status.
A recent study by DePhillipo et al. (DePhillipo et al., 2018) highlighted that ramp lesions increase anterior tibial translation, IE rotation, and Pivot-shift in an ACL-deficient knee. After isolate ACL reconstruction, Pivot shift was not completely restored.
The effect of lateral meniscectomy on AP laxity has been inspected less, and mainly in cadaveric studies: Wieser et al. (Wieser et al., 2012) did not find any statistical difference after meniscus removal in stable knees; using computer navigation, Musahl et al. (Musahl et al., 2010) confirmed the limited effect of the lateral meniscus in resisting anterior tibial translation in the ACL-deficient knee. However, the same authors demonstrated that total lateral meniscectomy in an ACL-deficient knee increased anterior translation of the lateral compartment during the pivot-shift maneuver. A similar effect has also been noted after lateral meniscus posterior root tear (Frank et al., 2017; Shybut et al., 2015) .
The combined effect of ACL replacement and meniscectomy has also been evaluated. Seon et al. (Seon et al., 2009) reported a residual AP laxity (7 mm) after single-bundle ACL reconstruction if subtotal medial meniscectomy was performed, compared with intact menisci. In particular, this was mostly evident at high degrees of knee flexion. In an in vitro study, Papageorgiou et al. (Papageorgiou et al., 2001) reported increased in situ forces in the ACL graft between 30% and 50% after medial meniscectomy in response to a combined anterior ad axial load, which could theoretically increase the risk of graft failure. Moreover, during a mechanized pivot shift, increased anterior translation of the lateral compartment with respect to the intact knee was demonstrated when both menisci were removed during ACL reconstruction (Petrigliano et al., 2011).
Biomechanical effect of MAT
Contact stress
MAT has been reported to be effective in the treatment of meniscus injury, and to partially restore the biomechanical function of the knee after the meniscectomy (Seitz & Dürselen, 2018). An in-vitro study by Kim et al. (Kim et al., 2013) demonstrated that joint contact pressure in meniscectomized knees were significantly higher than pressure after MAT, especially at 30° and 60° of knee flexion. Similarly, McDermott et al. (McDermott et al., 2008) showed that joint contact pressure after MAT are close to the ones in the intact knee, after being significantly risen in knees with medial meniscectomy. These results confirmed the potential chondroprotective effect of MAT in knee osteoarthritis.
Laxity
To the date, the biomechanical effect of MAT on knee laxity has been poorly evaluated (Rosso et al., 2015). An interesting in-vitro assessment of knee stability in presence of meniscal and ACL lesion has been given by Musahl et al. (Musahl et al., 2010): Lachman and Pivot-shift test have been used to evaluate the AP laxity when either medial or lateral meniscus were removed after the simulation of an ACL-deficient condition. A subsequent study from the same authors (Novaretti & Musahl, 2018) demonstrated that, in the same clinical conditions, lateral MAT may partially reduce AP laxity with both a suture-only and a bone-block technique (approximately 50% less than meniscectomized knee). Through another in-vitro study, Spang et al. (Spang et al., 2010) also assessed the effect of MAT in reducing the anterior tibial translation, demonstrating that laxity was statistically restored to the intact conditions. Nevertheless, the stability of the intact knee was not restored. In these studies, a surgical navigation system has been used to evaluate the intra-operative knee kinematics on cadavers. So far, no studies have outlined the in-vivo effect of MAT on knee kinematics.
In-vivo biomechanical evaluation of MAT
Patient 1 – medial MAT
Patient presentation
When the patient came to authors attention, he was a 55 years old male complaining of severe medial compartment pain of the right knee during working, walking and playing sports for 2 years and sensation of knee instability during pivoting movement. The patient was a heavy worker, amateur sportsman, with a Body Mass Index (BMI) of 24 kg/m2, healthy and without relevant comorbidities. The patient had undergone arthroscopic subtotal medial meniscectomy of the right knee 25 years before surgery, due to a traumatic lesion occurred during sport activity. He was asymptomatic until 5 years ago, when he started to complain worsening medial compartment tenderness, however without limiting his normal activities. Pain and swelling became more severe in the last 2 years to preclude him any sport activity such as running and playing tennis. The patient also reported a recent traumatic right knee sprain 6 months before the visit treated conservatively, after which a sense of knee instability and giving way, especially during pivoting activities, made him look for medical attention.
During the visit the patient presented a positive joint line tenderness at palpation, Anterior drawer test 3+ (scale from 0+ to 3+), Lachman test 3+ (scale from 0+ to 3+), Pivot-Shift test 2+ (scale from 0 to 3+), negative Varus and Valgus stress test (Mulligan et al., 2015; Musahl et al., 2012).
Knee radiographs revealed joint space narrowing and small osteophytes of medial femoral condyle and medial tibial plateau (Kellgren-Lawrence grade 3) (Fig. 1) (Kohn et al., 2016).
The Magnetic Resonance Imaging (MRI) showed absence of continuity and dishomeogenous signal of ACL, subtotal medial meniscectomy and subchondral bone edema of medial femoral condyle and tibial plateau, with a chondropathy graded as II according to Yulish Classification (Fig. 2) (Yulish et al., 1987).
Posterior Cruciate Ligament (PCL), lateral meniscus, lateral and patelloframroal compartments did not presented relevant abnormalities.
After counseling, the patient was scheduled for combined ACL reconstruction and medial MAT of the right knee.
Surgical procedure
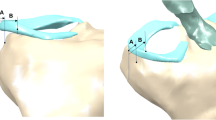
Arthroscopically, chronic ACL lesion with degeneration of the stump was noted. Lateral compartment presented an Outerbridge grade I of the lateral femoral condyle, with no lateral meniscus lesions. The medial compartment presented a subtotal deficit of medial meniscus, an Outerbridge grade II of the medial femoral condyle and a grade III of the medial tibial plateau (Fig. 3a).
Before the MAT and ACL reconstruction, kinematic acquisition was performed using a navigation system (BLU-IGS, Orthokey, Lewes, Delaware, DE, USA) equipped with a dedicated software (KLEE, Orthokey, Lewes, Delaware, DE, USA). Two optical trackers were firmly fixed at femoral and tibial bone through stab incisions, and anatomical landmarks were registered with a third tracker. After the initial set-up, the surgeon manually performed a battery of clinical kinematic tests at maximum manual force (Table 1). The reliability of all the laxity tests performed was evaluated by the research group in previous studies (Lopomo et al., 2009; Martelli et al., 2007).After the tests, arthroscopic meniscal allograft transplantation was performed, according to Marcacci’s technique. (Marcacci et al., 2012) A non-irradiated medial meniscus allograft was prepared without bone plugs. The graft was inserted in the knee joint through arthroscopic portal and the posterior horn was fixed to the anterior tibia through a trans-osseous suture, the periphery was sutured to the capsule with all-inside TRUESPAN (Mitek Sports Medicine, Raynham, Massachusetts, MA, USA), stitches, while the anterior horn was fixed to the remnant of the native meniscus with an all-inside stitch and to the capsule with a free needle (Fig. 3b).
After the transplant, knee laxity was again evaluated with the same tests through surgical navigation system.
Then, ACL reconstruction was performed with a single-bundle Over the top plus lateral plasty technique, using hamstring graft without detaching their tibial insertion (Marcacci et al., 1998).
Finally, the same laxity tests were performed after graft fixation. All the laxity tests were performed by the same experienced surgeon at manual maximum load.
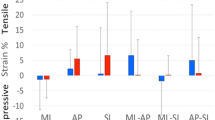
Results
AP displacement at 30° of flexion was 11.5 mm, 9 mm and 4 mm, at the basal state, after MAT and after ACL reconstruction, respectively. AP displacement at 90° of flexion was 10.5 mm, 7 mm and 2 mm, at the basal state, after MAT and after ACL reconstruction, respectively. Varus-Valgus (VV) rotation at 0° of flexion was 5.5°, 2° and 1°, at the basal state, after MAT and after ACL reconstruction, respectively. Internal-External (IE) rotation at 30° of flexion was 10.5°, 11° and 9°, at the basal state, after MAT and after ACL reconstruction, respectively, while the IE rotation at 90° of flexion was 12°, 9° and 7°, at the basal state, after MAT and after ACL reconstruction, respectively VV rotation at 30° of flexion was 7°, 5° and 1.5°, at the basal state, after MAT and after ACL reconstruction, respectively (Fig. 4).
Patient 2 – lateral MAT
Patient presentation
The patient was 30 Years old, amateur sportsman, with BMI 25,3 kg/m2, standing worker, without relevant comorbidities. 12 years before he underwent arthroscopic subtotal lateral meniscectomy of the left knee due to a traumatic meniscal lesion occurred while he was playing basketball. After surgery, he continued playing basketball and other pivoting sports, such as rugby and ski, for several years. In the last 4 years, he started complaining pain in the lateral compartment of the knee, he stopped playing pivoting sports and started bike, swim and running. In the last two years, he stopped playing sports because of pain increase and knee swelling episodes.
During the visit patient presented a tenderness in the lateral joint line of the knee. Laxity tests were negatives for ligamentous lesions.
Knee radiographs showed initial lateral joint space narrowing, graded as I according to Kellgren-Lawrence classification (Fig. 5).
The MRI showed subtotal lateral meniscectomy and a chondropathy graded as II according to Yulish classification. Other structures did not present relevant abnormalities (Fig. 6).
The patient was scheduled for arthroscopic lateral MAT of the left knee.
Surgical procedure
Anteromedial and anterolateral arthroscopic portal were performed. Arthroscopically, the medial compartment, ACL and PCL did not show significant lesions. The lateral compartment presented a subtotal deficit of lateral meniscus and an Outerbridge grade II of the lateral femoral condyle. (Fig. 7a).
Before MAT, kinematic tests were performed and evaluated with navigation system.
Then, arthroscopic lateral meniscal allograft transplantation was performed with a bone plug-free technique, fixing the anterior and posterior horns through two trans-tibial tunnels, while the periphery was sutured to the capsule with all-inside stitches FasT-Fix (Smith & Nephew, Andover, MA, USA) (Zaffagnini et al., 2016) (Fig. 7b).
After graft fixation, new laxity tests were performed and evaluated through surgical navigation system. All the laxity tests were performed by the same experienced surgeon at manual maximum load.
Results
AP displacement at 30° of flexion was 4.5 mm at the basal state and 2.5 mm after MAT while the AP displacement at 90° of flexion was 3 mm at the basal state and 1.5 mm after MAT. IE rotation at 30° of flexion was 21° at the basal state and 13° after MAT while IE rotation at 90° of flexion was 23.5° at the basal state and 17.5° after MAT. VV rotation at 0° of flexion was 2.0° at the basal state and 1° after MAT, while VV rotation at 30° of flexion was 3° at the basal state and 1.8° after MAT (Fig. 8).
Discussion
The aim of the present work was to evaluate the biomechanical role of MAT on knee laxity, through both a narrative review of the literature and two case studies, intraoperatively assessed with surgical navigation system.
Due to the biomechanical effect of both load absorbing and secondary stabilizer, meniscal repair should be the treatment of choice in case of lesions. However, since most of lesions are irreparable and require partial or even subtotal meniscectomies, MAT could be considered a viable and effective treatment for post-meniscectomy syndrome. In fact, MAT demonstrated to be biomechanically effective in improving knee stress distribution and reducing laxities (Nyland et al., 2018). For these reasons, the International Meniscus Reconstruction Experts Forum (IMREF) suggested MAT also in the setting of revision ACL reconstruction when meniscal deficiency is considered responsible of primary reconstruction failure, (Getgood et al., 2017) due to its effect of secondary stabilizer. Case series of primary or revision ACL reconstruction combined with MAT demonstrated satisfactory clinical outcomes and good knee stability (Zaffagnini et al., 2018).
The preliminary results of the in-vivo evaluation of MAT with computer navigation offered some interesting considerations. The MAT was in fact able to decrease knee laxity both in a medial and lateral meniscus-deficient knee, thus suggesting a synergic role with ACL in laxity, especially in resisting anterior tibial translation.
This study has some limitations. The two cases of MAT here described were performed in different settings. The medial MAT, since performed in an ACL and medial meniscus deficient knee, just before ACL reconstruction, is not able to provide information on the contribution of meniscal replacement to an intact-ACL knee. Differently, the lateral MAT was performed in an intact-ACL knee. Thus, it was not possible to compare the results from the two assessments, but we could only evaluate the pure role of the meniscus on the knee laxity. However, the different role on knee laxity of the medial and lateral meniscus would have created a bias in the comparison.
Furthermore, the kinematic evaluation has been performed manually rather than with mechanical devices and standardized forces. However, the senior surgeon has more than 10-year experience with surgical navigation of ACL reconstruction and his high reliability in manual assessment has already been demonstrated (Lopomo et al., 2009; Martelli et al., 2007). Another limitation is represented by the absence of contralateral knee laxity evaluation. This evaluation would have been useful to assess the real side-to-side difference in laxity and thus its relative reduction after MAT. Anyway, even if this practice is commonly performed in cadaveric studies, it would have been unethical in-vivo.
Moreover, these data represent a unique and preliminary experience of in-vivo assessment of MAT, thus they should be confirmed in larger series.
Conclusions
Meniscal Allograft Transplantation represents a valuable solution to improve the overall biomechanics of the knee joint and help to restore a good clinical condition, when associated with ACL replacement. The in-vivo kinematic evaluation here described confirmed the importance of MAT in reducing knee laxity for the two presented cases, particularly regarding the AP translation for the medial MAT and IE rotation for the lateral MAT. Further in-vivo studies may help to better assess the role of MAT in combination with ACL replacement and give insights for a better comprehension of the contribute of meniscal replacement in knee surgery.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACL:
-
Anterior Cruciate Ligament
- AP:
-
anterior-posterior
- BMI:
-
Body Mass Index
- IE:
-
Internal-External
- IMREF:
-
International Meniscus Reconstruction Experts Forum
- MAT:
-
Meniscus allograft transplantation
- MRI:
-
Magnetic Resonance Imaging
- OA:
-
Osteoarthritis
- PCL:
-
Posterior Cruciate Ligament
- VV:
-
Varus-Valgus
References
Ahmed AM, Burke DL (1983) In-vitro measurement of static pressure distribution in synovial joints--part I: Tibial surface of the knee. J Biomech Eng 105:216–225
Ahn JH, Bae TS, Kang K-S, Kang SY, Lee SH (2011) Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med 39:2187–2193. https://doi.org/10.1177/0363546511416597
Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL (2000) Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res Off Publ Orthop Res Soc 18:109–115. https://doi.org/10.1002/jor.1100180116
Allen PR, Denham RA, Swan AV (1984) Late degenerative changes after meniscectomy. Factors affecting the knee after operation. J Bone Joint Surg Br 66:666–671
Arno S, Hadley S, Campbell KA, Bell CP, Hall M, Beltran LS, Recht MP, Sherman OH, Walker PS (2013) The effect of arthroscopic partial medial meniscectomy on tibiofemoral stability. Am J Sports Med 41:73–79. https://doi.org/10.1177/0363546512464482
Baratz ME, Fu FH, Mengato R (1986) Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med 14:270–275. https://doi.org/10.1177/036354658601400405
Beals CT, Magnussen RA, Graham WC, Flanigan DC (2016) The prevalence of meniscal pathology in asymptomatic athletes. Sports Med Auckl NZ 46:1517–1524. https://doi.org/10.1007/s40279-016-0540-y
DePhillipo NN, Moatshe G, Brady A, Chahla J, Aman ZS, Dornan GJ, Nakama GY, Engebretsen L, LaPrade RF (2018) Effect of Meniscocapsular and Meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med 46:2422–2431. https://doi.org/10.1177/0363546518774315
Dong Y, Hu G, Dong Y, Hu Y, Xu Q (2014) The effect of meniscal tears and resultant partial meniscectomies on the knee contact stresses: a finite element analysis. Comput Methods Biomech Biomed Engin 17:1452–1463. https://doi.org/10.1080/10255842.2012.753063
Englund M, Lohmander LS (2004) Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum 50:2811–2819. https://doi.org/10.1002/art.20489
Faunø P, Nielsen AB (1992) Arthroscopic partial meniscectomy: a long-term follow-up. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 8:345–349
Frank JM, Moatshe G, Brady AW, Dornan GJ, Coggins A, Muckenhirn KJ, Slette EL, Mikula JD, LaPrade RF (2017) Lateral meniscus posterior root and Meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: a biomechanical study. Orthop J Sports Med 5:2325967117695756. https://doi.org/10.1177/2325967117695756
Getgood A, LaPrade RF, Verdonk P, Gersoff W, Cole B, Spalding T, the IMREF Group, Amendola A, Amis A, Bin S-I, Bugbee W, Caborn D, Carter T, Chan K-M, Cohen C, Cohen M, Condello V, DeBerardino T, Dirisamer F, Engebretsen L, Farr J, Gomoll A, Harner C, Heard M, Hiemstra L, Kim JG, Kim JM, Kim J-M, Kon E, Laggae K, Lee B-S, Litchfield R, Marcacci M, McCormack R, McDermott I, Monlau JC, Myers P, Noyes F, Patsch C, Robinson J, Rodeo S, Seo S-S, Sherman S, Siebold R, Snow M, Stone K, Tashman S, Thompson P, van Arkel E, van der Merwe W, Verdonk R, Williams A, Zaffagnini S (2017) International meniscus reconstruction experts forum (IMREF) 2015 consensus statement on the practice of meniscal allograft transplantation. Am J Sports Med 45:1195–1205. https://doi.org/10.1177/0363546516660064
Hanley ST, Warren RF (1987) Arthroscopic meniscectomy in the anterior cruciate ligament-deficient knee. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 3:59–65
Haut Donahue TL, Hull ML, Rashid MM, Jacobs CR (2004) The sensitivity of tibiofemoral contact pressure to the size and shape of the lateral and medial menisci. J Orthop Res Off Publ Orthop Res Soc 22:807–814. https://doi.org/10.1016/j.orthres.2003.12.010
Jacquet C, Pujol N, Pauly V, Beaufils P, Ollivier M (2019) Analysis of the trends in arthroscopic meniscectomy and meniscus repair procedures in France from 2005 to 2017. Orthop Traumatol Surg Res OTSR. https://doi.org/10.1016/j.otsr.2019.01.024
Kim JG, Lee YS, Bae TS, Ha JK, Lee DH, Kim YJ, Ra HJ (2013) Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc 21:2121–2125. https://doi.org/10.1007/s00167-012-2182-4
Kohn MD, Sassoon AA, Fernando ND (2016) Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop 474:1886–1893. https://doi.org/10.1007/s11999-016-4732-4
Lee SJ, Aadalen KJ, Malaviya P, Lorenz EP, Hayden JK, Farr J, Kang RW, Cole BJ (2006) Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med 34:1334–1344. https://doi.org/10.1177/0363546506286786
Levy IM, Torzilli PA, Gould JD, Warren RF (1989) The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am 71:401–406
Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 64:883–888
Lopomo N, Bignozzi S, Martelli S, Zaffagnini S, Iacono F, Visani A, Marcacci M (2009) Reliability of a navigation system for intra-operative evaluation of antero-posterior knee joint laxity. Comput Biol Med 39:280–285. https://doi.org/10.1016/j.compbiomed.2009.01.001
Lorbach O, Kieb M, Herbort M, Weyers I, Raschke M, Engelhardt M (2015) The influence of the medial meniscus in different conditions on anterior tibial translation in the anterior cruciate deficient knee. Int Orthop 39:681–687. https://doi.org/10.1007/s00264-014-2581-x
Maher SA, Wang H, Koff MF, Belkin N, Potter HG, Rodeo SA (2017) Clinical platform for understanding the relationship between joint contact mechanics and articular cartilage changes after meniscal surgery. J Orthop Res Off Publ Orthop Res Soc 35:600–611. https://doi.org/10.1002/jor.23365
Marcacci M, Zaffagnini S, Iacono F, Neri MP, Loreti I, Petitto A (1998) Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 6:68–75. https://doi.org/10.1007/s001670050075
Marcacci M, Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, Bonanzinga T, Nitri M, Bondi A, Molinari M, Rimondi E (2012) Meniscal allograft transplantation without bone plugs: a 3-year minimum follow-up study. Am J Sports Med 40:395–403. https://doi.org/10.1177/0363546511424688
Markolf KL, Bargar WL, Shoemaker SC, Amstutz HC (1981) The role of joint load in knee stability. J Bone Joint Surg Am 63:570–585
Martelli S, Lopomo N, Bignozzi S, Zaffagnini S, Visani A (2007) Validation of a new protocol for navigated intraoperative assessment of knee kinematics. Comput Biol Med 37:872–878. https://doi.org/10.1016/j.compbiomed.2006.09.004
McDermott ID, Lie DTT, Edwards A, Bull AMJ, Amis AA (2008) The effects of lateral meniscal allograft transplantation techniques on tibio-femoral contact pressures. Knee Surg Sports Traumatol Arthrosc 16:553–560. https://doi.org/10.1007/s00167-008-0503-4
Mulligan EP, McGuffie DQ, Coyner K, Khazzam M (2015) The reliability and diagnostic accuracy of assessing the translation endpoint during the lachman test. Int J Sports Phys Ther 10:52–61
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38:1591–1597. https://doi.org/10.1177/0363546510364402
Musahl V, Hoshino Y, Ahlden M, Araujo P, Irrgang JJ, Zaffagnini S, Karlsson J, Fu FH (2012) The pivot shift: a global user guide. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 20:724–731. https://doi.org/10.1007/s00167-011-1859-4
Novaretti JV, Musahl V (2018) Lateral meniscal allograft transplantation can partially improve knee stability with bone-block and suture-only fixation techniques. MTSG. LA, New Orleans, p 2018
Nyland J, Campbell K, Kalloub A, Strauss EJ, Kuban K, Caborn DNM (2018) Medial meniscus grafting restores normal tibiofemoral contact pressures. Arch Orthop Trauma Surg 138:361–367. https://doi.org/10.1007/s00402-017-2849-x
Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH (2001) The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med 29:226–231. https://doi.org/10.1177/03635465010290021801
Petrigliano FA, Musahl V, Suero EM, Citak M, Pearle AD (2011) Effect of meniscal loss on knee stability after single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 19(Suppl 1):S86–S93. https://doi.org/10.1007/s00167-011-1537-6
Petty CA, Lubowitz JH (2011) Does arthroscopic partial meniscectomy result in knee osteoarthritis? A systematic review with a minimum of 8 years’ follow-up. Arthrosc J Arthrosc Relat Surg 27:419–424. https://doi.org/10.1016/j.arthro.2010.08.016
Rosso F, Bisicchia S, Bonasia DE, Amendola A (2015) Meniscal allograft transplantation: a systematic review. Am J Sports Med 43:998–1007. https://doi.org/10.1177/0363546514536021
Salata MJ, Gibbs AE, Sekiya JK (2010) A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med 38:1907–1916. https://doi.org/10.1177/0363546510370196
Saltzman BM, Meyer MA, Weber AE, Poland SG, Yanke AB, Cole BJ (2017) Prospective clinical and radiographic outcomes after concomitant anterior cruciate ligament reconstruction and meniscal allograft transplantation at a mean 5-year follow-up. Am J Sports Med 45:550–562. https://doi.org/10.1177/0363546516669934
Scheller G, Sobau C, Bülow JU (2001) Arthroscopic partial lateral meniscectomy in an otherwise normal knee. Clinical, functional, and radiographic results of a long-term follow-up study Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 17:946–952. https://doi.org/10.1053/jars.2001.28952
Seitz AM, Dürselen L (2018) Biomechanical considerations are crucial for the success of tendon and meniscus allograft integration—a systematic review. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5185-y
Seon JK, Gadikota HR, Kozanek M, Oh LS, Gill TJ, Li G (2009) The effect of anterior cruciate ligament reconstruction on kinematics of the knee with combined anterior cruciate ligament injury and subtotal medial meniscectomy: an in vitro robotic investigation. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 25:123–130. https://doi.org/10.1016/j.arthro.2008.09.020
Shybut TB, Vega CE, Haddad J, Alexander JW, Gold JE, Noble PC, Lowe WR (2015) Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 43:905–911. https://doi.org/10.1177/0363546514563910
Song Y, Greve JM, Carter DR, Giori NJ (2008) Meniscectomy alters the dynamic deformational behavior and cumulative strain of tibial articular cartilage in knee joints subjected to cyclic loads. Osteoarthr Cartil 16:1545–1554. https://doi.org/10.1016/j.joca.2008.04.011
Spang JT, Dang ABC, Mazzocca A, Rincon L, Obopilwe E, Beynnon B, Arciero RA (2010) The effect of medial meniscectomy and meniscal allograft transplantation on knee and anterior cruciate ligament biomechanics. Arthrosc J Arthrosc Relat Surg 26:192–201. https://doi.org/10.1016/j.arthro.2009.11.008
Stone KR, Adelson WS, Pelsis JR, Walgenbach AW, Turek TJ (2010) Long-term survival of concurrent meniscus allograft transplantation and repair of the articular cartilage: a PROSPECTIVE TWO- TO 12-YEAR FOLLOW-UP REPORT. J Bone Joint Surg Br 92-B:941–948. https://doi.org/10.1302/0301-620X.92B7.23182
Wieser K, Betz M, Farshad M, Vich M, Fucentese SF, Meyer DC (2012) Experimental loss of menisci, cartilage and subchondral bone gradually increases anteroposterior knee laxity. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 20:2104–2108. https://doi.org/10.1007/s00167-011-1799-z
Yammine K (2013) Effect of partial medial meniscectomy on anterior tibial translation in stable knees: a prospective controlled study on 32 patients. Sports Med Arthrosc Rehabil Ther Technol 5. https://doi.org/10.1186/2052-1847-5-17
Young J, Tudor F, Mahmoud A, Myers P (2017) Meniscal transplantation: procedures, outcomes, and rehabilitation. Orthop Res Rev Volume 9:35–43. https://doi.org/10.2147/ORR.S94378
Yulish BS, Montanez J, Goodfellow DB, Bryan PJ, Mulopulos GP, Modic MT (1987) Chondromalacia patellae: assessment with MR imaging. Radiology 164:763–766. https://doi.org/10.1148/radiology.164.3.3615877
Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Benzi A, Serra M, Rotini M, Bragonzoni L, Marcacci M (2016) Survivorship and clinical outcomes of 147 consecutive isolated or combined arthroscopic bone plug free meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 24:1432–1439. https://doi.org/10.1007/s00167-016-4035-z
Zaffagnini S, Grassi A, Romandini I, Marcacci M, Filardo G (2018) Meniscal allograft transplantation combined with anterior cruciate ligament reconstruction provides good mid-term clinical outcome. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5078-0
Acknowledgements
Not applicable.
Funding
The study was funded by authors.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the enrolled patients signed informed consent forms to undergo surgical procedure, and the research study was approved by the Institutional Review Board (IRB approval: Prot. n° 0000397 of 12/01/2018).
Consent for publication
Consent to publish individual data was obtained by patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zaffagnini, S., Di Paolo, S., Stefanelli, F. et al. The biomechanical role of meniscal allograft transplantation and preliminary in-vivo kinematic evaluation. J EXP ORTOP 6, 27 (2019). https://doi.org/10.1186/s40634-019-0196-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-019-0196-2