Abstract
Background
While 5% of 247 million global malaria cases are reported in Uganda, it is also a top refugee hosting country in Africa, with over 1.36 million refugees. Despite malaria being an emerging challenge for humanitarian response in refugee settlements, little is known about its risk factors. This study aimed to investigate the risk factors for malaria infections among children under 5 years of age in refugee settlements in Uganda.
Methods
We utilized data from Uganda’s Malaria Indicator Survey which was conducted between December 2018 and February 2019 at the peak of malaria season. In this national survey, household level information was obtained using standardized questionnaires and a total of 7787 children under 5 years of age were tested for malaria using mainly the rapid diagnostic test. We focused on 675 malaria tested children under five in refugee settlements located in Yumbe, Arua, Adjumani, Moyo, Lamwo, Kiryadongo, Kyegegwa, Kamwenge and Isingiro districts. The extracted variables included prevalence of malaria, demographic, social-economic and environmental information. Multivariable logistic regression was used to identify and define the malaria associated risk factors.
Results
Overall, malaria prevalence in all refugee settlements across the nine hosting districts was 36.6%. Malaria infections were higher in refugee settlements located in Isingiro (98.7%), Kyegegwa (58.6%) and Arua (57.4%) districts. Several risk factors were significantly associated with acquisition of malaria including fetching water from open water sources [adjusted odds ratio (aOR) = 1.22, 95% CI: 0.08–0.59, P = 0.002], boreholes (aOR = 2.11, 95% CI: 0.91–4.89, P = 0.018) and water tanks (aOR = 4.47, 95% CI: 1.67–11.9, P = 0.002). Other factors included pit-latrines (aOR = 1.48, 95% CI: 1.03–2.13, P = 0.033), open defecation (aOR = 3.29, 95% CI: 1.54–7.05, P = 0.002), lack of insecticide treated bed nets (aOR = 1.15, 95% CI: 0.43–3.13, P = 0.003) and knowledge on the causes of malaria (aOR = 1.09, 95% CI: 0.79–1.51, P = 0.005).
Conclusions
The persistence of the malaria infections were mainly due to open water sources, poor hygiene, and lack of preventive measures that enhanced mosquito survival and infection. Malaria elimination in refugee settlements requires an integrated control approach that combines environmental management with other complementary measures like insecticide treated bed nets, indoor residual spraying and awareness.
Graphical Abstract

Similar content being viewed by others
Background
Malaria is among the major global life-threatening diseases which is spread to humans by bites from infected female Anopheles mosquitoes [1]. Although six Plasmodium parasite species (i.e. P. falciparum, P. vivax, P. malariae, P. ovale curtisi, P. ovale wallikeri and P. knowlesi) are known to cause malaria in humans, P. falciparum is the most prevalent malaria parasite in sub-Saharan Africa (SSA), contributing to most of the malaria cases and deaths [2]. By 2021, there was an estimated 234 million malaria cases and 593,000 deaths within the World Health Organization (WHO) African Region [1]. The malaria burden was further amplified by coronavirus disease 2019 (COVID-19) disruptions which constrained malaria chemoprevention, distribution of insecticide-treated bed nets (ITNs), indoor residual spraying (IRS), malaria testing and treatment [3]. By 2021, an estimated additional 13.4 million cases were attributed to the disruptions during the COVID-19 pandemic [1]. In addition, climate change is adding another layer of complication to the burden considering that the transmission frontiers and the risk for malaria have shifted further to the eastern and southern parts of the African continent especially in highlands and densely populated regions [4, 5].
As the world strives to eliminate malaria [1], the plight of refugees, displaced people, and asylum seekers must not be forgotten. It is widely recognised that human mobility influences the spread of infectious diseases including influenza, cholera, malaria, dengue, schistosomiasis and Ebola among others [6,7,8]. Human mobility is one of determinants of many infectious disease transmission dynamics by either introducing pathogens into susceptible populations or changing the frequency of contacts between infected and susceptible individuals or both [9]. As of late 2021, the United Nations Refugee Agency estimated that globally, there were 89.3 million forcibly displaced people [10], with almost two-thirds of the people affected by humanitarian emergencies inhabiting malaria endemic regions [11].
The high prevalence of malaria among the displaced populations in Africa constitutes an emerging challenge for humanitarian response [12]. Vector borne and other infectious diseases present many challenges in refugee settlements due to inequalities, limited access to healthcare services, and crowded environments which enable rapid disease spread [13]. The risk for malaria infections can increase among refugees especially when immunologically naive individuals with little or no prior malaria exposure move to areas of more intense transmission [11]. Besides, the influx of refugees from endemic countries can be associated with imported malaria [6] which can contribute to secondary transmission and the spread of drug resistance while threatening long-term elimination goals [14].
The population subgroups considered to be at higher risk of contracting malaria include children under 5 years of age [15, 16], pregnant women [17], and patients with HIV/AIDS [18]. Refugees are rendered vulnerable to malaria infections by their lack of protective immunity, increased concentration of people in exposed settings, limited distribution of ITNs, inadequate IRS, insufficient rapid clinical diagnostic and treatment responses [19, 20]. Other risk factors include outdoor night activities, wearing short clothes, residing in unfinished houses, poor drainage [21] and acute malnutrition among children [22].
While 5% of the 247 million global malaria cases are from Uganda [1], the country is also one of the top refugee hosting countries in Africa [23]. Refugee settlements in Uganda are predominantly located in rural areas of hosting districts usually with active malaria transmission. Such areas are typically characterised by overcrowding, inadequate and temporary shelters, limited vector control efforts and poor access to water and sanitation [24]. These conditions make refugee settlements susceptible to high risks of malaria transmission. Elsewhere, it has been documented that malaria is among the leading causes of morbidity and mortality among children under 5 years of age in refugee settlements [16, 21, 25]. Despite these potential risks and challenges, studies on refugees in Uganda have concentrated much on adolescent sexual behaviour [26], psychosocial impact of COVID-19 [27], impact of COVID-19 on food security [28], access to education [29], agroforestry [30], environmental degradation [31] among others, with limited focus on malaria risk factors, treatment and preventive measures [25].
Understanding the key risk factors for malaria infections among children in refugee settlements is crucial for (re)designing humanitarian responses and selecting appropriate intervention strategies for malaria prevention, control, even elimination. This is only possible with adequate research and evidence to support the development of effective and sustainable management strategies. To bridge this knowledge gap, this study utilised data from the 2018–2019 Uganda Malaria Indicator Survey (UMIS) which is the first national wide malaria survey in Uganda to include households and people in refugee settlements [32]. This study aimed at providing an overview the prevalence of malaria infections and local context risk factors for malaria infections among children under 5 years of age in refugee settlements of Uganda.
Methods
Study area
Uganda is the third largest refugee-hosting country in the world after Turkey and Pakistan with over 1.36 million refugees [24]. By 2018, South Sudan made up the largest refugee population in Uganda (985,512), followed by the Democratic Republic of Congo (D.R. Congo) (271,967) and Burundi (36,677) [24]. About 70,988 refugees from Ethiopia, Eritrea, Rwanda, Somalia and Sudan have lived in protracted exile in Uganda for the past three decades [33]. The majority of the refugee population are women and children (82%), with 56% below the age of 15, while 25% are younger than 5 years [34]. This study focused on all refugee settlements located in nine districts of Yumbe, Arua, Adjumani, Moyo, Lamwo, Kiryadongo, Kyegegwa, Kamwenge and Isingiro, as shown in Fig. 1.
Data source
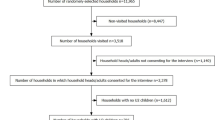
Datasets for this study were obtained from the 2018–2019 UMIS. To link the demographic, social-economic and environmental variables captured in the 2018–2019 UMIS to malaria infections, we conducted a literature review and the variables deemed relevant for the refugee settlements were identified as shown in Additional file 1: Table S1. The 2018–2019 UMIS was obtained from the Demographic and Health Surveys program. The 2018–2019 UMIS was the third malaria survey to be conducted in Uganda (after the 2009 UMIS and 2014–2015 UMIS) focusing on refugee settlements and their hosting districts and included information on malaria parasite prevalence, anemia, and status of key malaria indicators [32]. The survey was based on a nationally representative sample of 320 clusters. Standardised questionnaires were designed to collect the demographic, social, economic and environmental information of the surveyed households. Both rapid diagnostic test (RDT) and the blood smear test (BST) were used to test malaria parasitemia among children under 5 years of age with consent from household heads [32].
Study population, sample size and variable selection
The 2018–2019 UMIS involved a total of 8125 children under 5 years of age of whom, 3481 children were from refugee settlements shown in Fig. 1. In this survey, 7787 children under 5 years of age were tested for malaria country-wide using both RDT and BST methods. In this paper, we only focused on 675 children under 5 years who were tested for malaria in refugee settlements. For quality control, results of the RDT and BST were checked for their completeness. In this study, we used the RDT results because the BST results had significant missing values. The explanatory or independent variables extracted from the survey datasets were those factors which had the ability to potentially influence mosquito survival, biting, feeding, parasite development and breeding (Additional file 1: Table S1). These variables were grouped into risk factors in line with the demographic and social-economic aspects, water, sanitation and housing, malaria prevention practices, knowledge on the causes and prevention of malaria. Variables extracted from the datasets were categorized to perform the analysis. More details are shown in Additional file 1: Table S2.
Data analysis
Data entry and all the analyses were conducted using JMP software, version 13 (JMP Statistical Discovery LLC, North Carolina, USA). Descriptive analysis was performed on all study variables. Univariate logistic regression was used to estimate the unadjusted odds ratio (uOR) of each independent variable to malaria infection. Variables that were significantly associated with malaria infection with a significance level of P < 0.20 were selected for possible inclusion in multivariable logistic regression. We chose P < 0.20 as the threshold for including variables in the multivariable model because this has been suggested elsewhere as an appropriate cut-off. In the multivariable logistic regression, we used a backward stepwise strategy to estimate the adjusted odds ratios (aORs) and corresponding 95% confidence intervals (CI) of the household variables in association with malaria infections with a significance level of P < 0.05. Results of both the descriptive and logistic regression analyses were displayed in a table format.
Results
Prevalence of malaria infections among children in refugee settlements
A total of 675 children below the age of five was used in this study, of which 29.6% were aged 0–15 months, 21.3% aged 16–30 months, 24.9% aged 31–45 months and 24.1% age 46–60 months. Overall, the prevalence of malaria infections in all refugee settlements across the nine hosting districts was 36.6%. Malaria infections were higher in refugee settlements located in Isingiro (98.7%), Kyegegwa (58.6%) and Arua (57.4%) districts. The prevalence of malaria was low in refugee settlements located in Adjumani (19.2%) and Kiryandongo (7.7%) districts.
Determinants of malaria infections among children in refugee settlements
Table 1 depicts the demographic and social-economic risk factors associated with malaria infections. Indeed, significant risk factors included children’s age, age of household head, household wealth status, mother’s level of education, and type of cooking fuel. The results suggest that the odds of contracting malaria were significantly higher in refugee households whose children were aged 31–45 months (aOR = 2.14, 95% CI: 1.32–3.47) and above 45 months (aOR = 2.01, 95% CI: 1.22–3.32) compared to those households whose children were under 31 months. Households whose heads were aged between 15 and 24 years were 1.74 times (aOR = 1.74, 95% CI: 1.08–2.79) more likely to have their children getting malaria infections than those whose heads were 25 years and above. Refugee households with mothers with no education were 1.35 times (aOR = 1.35, 95% CI 0.92–1.96) more likely to have their children contracting malaria compared to households with educated mothers. Poor households were 4.23 times (aOR = 4.23, 95% CI: 1.19–14.9) more likely to have their children at risk of malaria infections compared to rich households. Households which used firewood and straw for cooking were 2.20 (aOR = 2.20, 95% CI: 1.17–4.15) and 2.51 (aOR = 2.51, 95% CI: 0.68–9.25) times more likely to have their children contracting malaria respectively compared to households which used charcoal for cooking (P < 0.05).
Further, Table 1 shows environmental malaria risk factors. Households whose main sources of domestic water were open water sources, boreholes and water tanks, were 1.22 (aOR = 1.22, 95% CI: 0.08–0.59), 2.11 (aOR = 2.11, 95% CI: 0.91–4.89) and 4.47 (aOR = 4.47, 95% CI: 1.67–11.9) times more likely to have their children contracting malaria respectively, compared to households which fetched water from public water taps (P < 0.05). Walk time distance to water sources of 0–15 min was associated with significantly higher odds of getting malaria among children (aOR = 1.68, 95% CI: 1.11–2.56) compared to walk time distance above 15 min. Households which used pit-latrines with slabs and those without any toilet facility or used bushes were 1.48 (aOR = 1.48, 95% CI: 1.03–2.13) and 3.29 (aOR = 3.29, 95% CI: 1.54–7.05) times more likely to have their children obtaining malaria (P < 0.05). Using open pits also increased the risk for malaria infections (aOR = 6.67, 95% CI: 0.47–0.97). From Table 1, it is further indicated that households whose walls were constructed using thatch and cardboard were 4.50 (aOR = 2.50, 95% CI: 0.11–56.0) and 2.30 (aOR = 2.30, 95% CI: 1.39–13.2) times more likely to have their children contracting malaria compared to households whose walls were built with brick and cement or mud (P < 0.05). Additionally, households with thatch roofs were 2.12 (aOR = 2.12, 95% CI: 0.94–4.79) times more likely to have their children contracting malaria compared households with roofs constructed of tarpaulins and iron sheets.
From Table 1, malaria prevention risk factors are presented. It is clearly indicated that households which did not have ITNs or sprayed their households with insecticides, were 1.15 (aOR = 1.15, 95% CI: 0.43–3.13) and 8.04 (aOR = 8.04, 95% CI: 2.47–26.2) times more likely to have their children contracting malaria compared to households which had implemented these preventive interventions. Further, households whose children did not sleep under ITNs were associated with significantly higher risk of malaria infection in children (aOR = 1.30, 95% CI: 0.58–2.49) compared to those households whose children slept under ITNs. Households which did not have access to malaria preventive medicine were 4.84 (aOR = 4.84, 95% CI: 1.82–12.8) more likely to have their children getting malaria compared to those households which had access.
Risk factors associated with knowledge on malaria transmission and prevention are also presented in Table 1. Households which did not know that mosquito bites caused malaria were 1.09 (aOR = 1.09, 95% CI: 0.79–1.51) times more likely to have their children contracting malaria compared to those which knew. Households which indicated that eating maize and mangoes as the causes of malaria were 2.96 (aOR = 2.96, 95% CI: 1.13–7.75) and 1.22 (aOR = 1.22, 95% CI: 0.47–3.19) times more likely to have their children contracting malaria respectively compared to those households which knew the actual causes (P < 0.05). Households which indicated that malaria could not be avoided were 2.14 (aOR = 2.14, 95% CI: 1.29–3.55) times more likely to have their children contracting malaria. The odds of children contracting malaria were high in households which did not know that sleeping under the net (aOR = 1.61, 95% CI: 1.16–2.23) and destroying breeding sites (aOR = 1.99, 95% CI: 1.44–2.76) were the ways of avoiding malaria.
Discussion
The concentration and crowding of refugees in settlements in Uganda is a fertile ground for malaria transmission within these settings and hosting communities. The risk factors discussed below relate to the survival, biting, feeding, parasite development and breeding of mosquitoes.
Demographic and socio-economic risk factors
Age
Although previous studies indicated that infants less than 12 months of age were the most vulnerable groups to malaria infections [35,36,37], the results of this study suggested that households with children aged 31 months and above were more likely to have their children contracting malaria in refugee settlements. There are several potential reasons for the difference. Refugee settlements are distinct and complex with people coming from diverse social-cultural and economic backgrounds. Thus, little is known of the neonatal and infant care practices, social norms, and behavioral patterns adopted by refugees to reduce malaria infections and other diseases. The high risk of malaria infection in children aged 31 months and older could, however, be attributed to the fact that at this age, the children were more active (i.e., crawling, walking, removing clothes, uncovering during sleep, etc.), making them more susceptible to mosquito bites. Moreover, during this age, most of children are weaned when they have not yet acquired natural immunity to manage or fight high parasite density [38]. Other studies have linked malaria risk among children between 24 and 60 months to malnutrition, although the evidence remains inconclusive [39]. The shift in age groups at high risk of malaria as observed from children aged 31 months and above in this study, suggests the need to expand prevention and free treatment strategies for older children in order to cover the peak transmission months in refugee settlements.
The odds for contracting malaria among children were significantly higher among households headed by refugees aged 15–24 years. This is due to the fact that refugees aged 15–24 years were within the category of ‘child and young migrants’ and may not have had adequate knowledge about child care, malaria transmission and prevention and at the same time, may have lacked financial resources and support for malaria prevention measures and treatment. This study further revealed that increase in the age of household head reduced the odds of malaria infections in children. This result is contrary to other studies conducted in Nigeria [40] and SSA which indicate that increase in ages of both male and female heads of households increased the odds of malaria prevalence among children under 5 years of age [41, 42]. This contradiction can be explained by the population variations and age dynamics between refugee and non-refugee settlements. Moreover, such studies never considered refugee settlements yet context specific behavioural and social cultural information are key to understanding the interactions that propel the risks for malaria within these local dynamic settings.
Mother’s educational level
The result of this study shows that lack of education among refugee mothers was significantly associated with a risk of malaria among children compared to those households with educated mothers. This result is consistent with findings from other studies [21, 40,41,42]. Since mothers are at the core of family welfare and wellbeing, their level of education is an essential social determinant of health and influences their ability to make better decisions about the health of children. Since adult literacy programmes for mothers in refugee settlements are rare, larger scale health promotional campaigns focusing on malaria diagnosis, prevention, and treatment are required. Such health education campaigns have worked well in endemic communities where knowledge about malaria and newer interventions are often lacking [43]. For example, a study conducted in Ethiopia indicated that children whose parents received training and awareness about use of ITNs were found to be at a lower risk of malaria infections compared to those who did not have any training [42].
Household wealth status
The findings of this study further suggest that poor refugee households were more likely to have their children contracting malaria. This result is in line with other study findings [36, 43]. The cost of malaria diagnosis, treatment and prevention may seem high for the poor households who face other constraints and daily expenses. Distribution of ITN, conducting IRS and destruction of mosquito breeding sites are options that need to be explored in refugee settlements.
Type of cooking fuel used
Although smoke from biomass cooking is often associated with reduced mosquito abundance and malaria transmission [44], the results of this study indicated that households which used firewood and straw for cooking were more likely to have their children contracting malaria compared to households which used charcoal. This result is consistent with other studies [45]. There are potential reasons to this finding. Women and children in refugee settlements gather much of the firewood used in their households and this exposes them to frequent mosquito bites in the forests and bushes where firewood is obtained. Besides, firewood piles near households serve as daytime hiding place for mosquitoes. Additionally, the shift in mosquito behavior from indoor late-night biting to outdoor early-evening biting [46, 47] coincides well with the major outdoor cooking activities in most refugee homesteads. Some studies in non-refugee settlements, however, indicate no association between outdoor cooking practices and malaria infections among children [48]. Nevertheless, epidemiological modelling [13] is required to better understand the relationships between cooking practices, cooking fuel emissions, mosquito activity and risk of malaria acquisition among children in refugee settlements. Such modelling can be vital in supporting appropriate malaria prevention messaging and evidence-based decision making in this context. Although charcoal use was associated with reduced malaria risk, it is one of the fundamental drivers of deforestation in refugee hosting districts and beyond, thus, its use in malaria control programs is not advisable in both short and long run.
Environmental malaria risk factors
Sources of drinking water
This study found out that refugee households which obtained water from open water sources and water tanks were more likely to have their children contracting malaria. This result is consistent with other studies [41,42,43]. This is likely due to several reasons. First, open water sources like rivers, ponds, lakes, swamps, dams, wells and springs serve as meeting places for humans and mosquitoes. Given the fact that refuge mothers and children fetch most of the water from these sources, the chances of mosquito bites are high. Second, these water sources are potential oviposition sites which are crucial for reproductive success and population dynamics of mosquitoes [49]. Third, these open water sources shorten the gonotrophic cycle [50] especially when located near refugee households. Water tanks as a key malaria risk factor is not surprising because they act as breeding sites for mosquitoes. Households which obtained water from boreholes and public water taps were less likely to have their children contracting malaria, although other studies indicated the opposite [15, 51].
Walk time distance to water sources
This study also revealed short walk time distance (0–15 min) to water sources was one of the risk factors for malaria among children. This result is in line with other studies focusing on malaria infections and distance to water sources [52, 53]. Although distant water sources were associated with reduced malaria risk, this result should not hamper efforts geared to improve water access in refugee settlements. This is because reducing the time to fetch water has been observed to improve child health [54]. Thus, given the land use and land cover changes within refugee settlements, environmental management practices such as draining stagnant water, dredging water channels, clearing vegetation among others, should be applied to water sources to reduce mosquitoes breeding and survival.
Household sanitation
Refugee households which had pit-latrines and those without any toilet facility were more likely to have their children contracting malaria. This result is not surprising because mosquitoes have overtime started changing their breeding preference to contaminated surroundings [55]. Similar findings have been observed in other studies [21, 41, 51, 53]. Based on this finding, interventions need to be strengthened so that pit-latrines which are commonly used within refugee settlements are vector borne free. For example, mosquitoes in pit-latrines can be suppressed when expanded polystyrene beads are used.
Building materials
This study revealed that the odds of malaria infections increased among children living in houses with grass thatch roofs, thatch and cardboard walls. This result is consistent with a systematic review and meta-analysis study on socioeconomic determinants of malaria burden in SSA [42]. Walls made up with thatch and cardboards allow mosquitoes to enter into households with ease [56]. Additionally, thatch provides conducive indoor resting grounds for mosquitoes since there are associated with cool temperatures which can sustain survival of mosquitoes indoors [57]. Thus, the choice of building materials for house construction in refugee settlements should be carefully selected to minimize malaria risk. For example, this study revealed that households with brick walls and iron sheet roofs were less likely to have their children contracting malaria, although the odds were not significant. However, a recent study conducted in SSA [58] revealed that metal-roofed houses contributed to the decline in malaria burden, since they were associated with higher temperatures and lower humidity which reduced survivorship of indoor-resting mosquitoes.
Malaria prevention risk factors
The odds of contracting malaria among children were significantly higher in refugee households which did not have ITNs, sprayed against mosquitoes or lacked access to malaria prevention medicines. Some studies reported similar results [21, 40, 42]. Although our study indicated that ITNs and IRS were effective in reducing the risk for malaria, there are limited in scope and efficacy. For example, IRS interventions apply to mosquitoes which feed and rest indoors, while ITNs prevent night mosquito bites just around the beds. This limitation provides opportunities for outdoor active mosquitoes to multiply while sustaining some level of transmission beyond the reach of ITNs and IRS. Additionally, in some cases, mosquitoes have developed resistance to pyrethroids used in ITNs and IRS [59]. Moreover, their continued use has led to an apparent shift in mosquito behavioural traits (i.e., insecticide avoidance and early-exit behaviours among indoor-feeding vectors) [60]. Despite these protection gaps, promotion of ITNs and IRS should continue in refugee settlements. Moreover, since mothers in refugee settlements engage in various outdoor activities at night [21], provision of nets for outdoor spaces in combination with IRS may be an additional strategy to effectively reduce the incidence of malaria among children. The effectiveness and efficacy of ITNs and IRS can be improved and strengthened by promoting environmentally based interventions which reduce mosquito survival and human-vector contact. However, there is a need for continued formative research and strong collaboration between the scientific community and other stakeholders to coordinate malaria elimination strategies that are adapted to the local social context of refugee settlements.
Knowledge on the causes of malaria
The results of this study suggest that refugee households which did not know the causes and prevention of malaria were more likely to have their children contracting malaria. This result is consistent with a systematic review on studies conducted in Southeast Asia where it was observed that poor knowledge and awareness about malaria transmission were related to some families using nets for reasons other than malaria prevention, such as fishing and for warmth [43]. Similar results are reported from SSA especially among the rural and uneducated individuals [42, 61, 62]. The finding of our study underscores the need for more education, training and communication initiatives to complement delivery of integrated malaria programmes that include mass malaria drug administration in refugee settlements.
Strength and limitations of the study
The utilization of nationally representative data with a high sample size was the study’s main strength. Thus, our results can be used in generalisation to understand malaria risk factors in other refugee settlements with similar demographic and social-economic settings. However, the study had some limitations. We were not able to include other environmental risk factors like rainfall and temperature, since we used secondary data. Finally, the cross-sectional nature of the study design did not allow a causal-effect relationship to be established with certainty among the identified household level risk predictors and malaria infections. Despite these limitations, the study was obviously sufficiently powered to detect several important risk factors for malaria infections which could be given priority in refugee settlements.
Conclusions
Malaria infections among children continue to circulate in many refugee settlements in Uganda. This study identified several malaria risk factors which need special attention within the framework of humanitarian assistance. Refugee households which used firewood and straw for cooking, fetched water from open water sources and water tanks were more likely to have their children contracting malaria. In addition, households which used pit-latrines and open defecation were more likely to have their children getting malaria infections. Malaria among children also increased in households with thatch walls and roofs, and those without preventive measures. To sum up, malaria elimination in refugee settlements requires an integrated control approach that combines environmental management with other complementary measures like insecticide treated bed nets, indoor residual spraying and awareness. Future studies can examine the impact of additional factors on the risk for malaria in refugee settlements that have not been studied here.
Availability of data and materials
The data used in this study can be obtained by sending a request via the DHS Program website and upon approval data can be obtained from https://dhsprogram.com/data/dataset/Uganda_MIS_2018.cfm?flag=1.
Abbreviations
- aOR :
-
Adjusted odds ratio
- BST:
-
Blood Smear Test
- CI :
-
Confidence interval
- COVID-19:
-
Coronavirus disease 2019
- DHS:
-
Demographic and Health Surveys
- IRS:
-
Indoor Residual Spraying
- ITNs:
-
Insecticide-treated bed-nets
- uOR :
-
Unadjusted odds ratio
- RDT:
-
Rapid Diagnostic Test
- UMIS:
-
Uganda Malaria Indicator Survey
- WHO:
-
World Health Organization
References
World Malaria Report. 2022. https://www.who.int/publications/i/item/9789240064898. Accessed 10 Jan 2023.
Ngotho P, Soares A, Hentzschel F, Achcar F, Bertuccini L, Marti M. Revisiting gametocyte biology in malaria parasites. Microbiol Rev. 2019;43:401–14.
Hussein M, Albashir A, Elawad O, Homeida A. Malaria and COVID-19: unmasking their ties. Malar J. 2020;19:1–10.
Semakula H, Song G, Achuu S, Shen M, Chen J, Mukwaya P, et al. Prediction of future malaria hotspots under climate change in sub-saharan Africa. Clim Change. 2017;143:415–28.
Ryan S, Lippi C, Zermoglio F. Shifting transmission risk for malaria in Africa with climate change: a framework for planning and intervention. Malar J. 2020;19:1–14.
Ahmed S, Reithinger R, Kaptoge S, Ngondi J. Travel is a key risk factor for malaria transmission in pre-elimination settings in sub-Saharan Africa: a review of the literature and meta-analysis. Am J Trop Med Hyg. 2020;103:1380–7.
Ciddio M, Mari L, Sokolow S, De-Leo G, Casagrandi R, Gatto M. The spatial spread of schistosomiasis: a multidimensional network model applied to Saint-Louis region, Senegal. Adv Water Resour. 2017;108:406–15.
Mari L, Gatto M, Ciddio M, Dia E, Sokolow S, De-Leo G, et al. Big-data-driven modeling unveils country-wide drivers of endemic schistosomiasis. Sci Rep. 2017;7:1–11.
Wesolowski A, Buckee C, Engø-Monsen K, Metcalf C. Connecting mobility to infectious diseases: the promise and limits of mobile phone data. J Infect Dis. 2016;214:414–20.
Global Trends Report. : Forced Displacement in 2021 https://www.unhcr.org/62a9d1494/global-trends-report-2021. Accessed 12 Jan 2023.
Messenger L, Furnival-Adams J, Pelloquin B, Rowland M. Vector control for malaria prevention during humanitarian emergencies: protocol for a systematic review and meta-analysis. BMJ Open. 2021;11:1–10.
Eshag H, Elnzer E, Nahied E, Talib M, Mussa A, Muhajir A, et al. Molecular epidemiology of malaria parasite amongst patients in a displaced people’s camp in Sudan. Trop Med Health. 2020;48:1–7.
Aylett J, Gilman R, Hall I, Kennedy D, Evers E, Katta A, et al. Epidemiological modelling in refugee and internally displaced people settlements: Challenges and ways forward. BMJ Glob Heal. 2022;7:1–10.
Tatem A, Jia P, Ordanovich D, Falkner M, Huang Z, Howes R, et al. The geography of imported malaria to non-endemic countries: a meta-analysis of nationally reported statistics. Lancet Infect Dis. 2017;17:98–107.
Semakula H, Song G, Achuu S, Zhang S. A bayesian belief network modelling of household factors influencing the risk of malaria: a study of parasitaemia in children under five years of age in sub-saharan Africa. Environ Model Softw. 2016;75:59–67.
Hershey C, Doocy S, Anderson J, Haskew C, Spiegel P, Moss W. Incidence and risk factors for malaria, pneumonia and diarrhea in children under 5 in UNHCR refugee camps: a retrospective study. Confl Health. 2011;5:1–11.
Tegegne Y, Asmelash D, Ambachew S, Eshetie S, Addisu A, Jejaw Zeleke A. The prevalence of malaria among pregnant women in Ethiopia: A systematic review and meta-analysis. J Parasitol Res. 2019;2019:1–9.
Obebe O, Falohun O. Epidemiology of malaria among HIV/AIDS patients in sub-Saharan Africa: a systematic review and meta-analysis of observational studies. Acta Trop. 2021;215:10–39.
Sherrard-Smith E, Griffin J, Winskill P, Corbel V, Pennetier C, Djénontin A, et al. Systematic review of indoor residual spray efficacy and effectiveness against Plasmodium falciparum in Africa. Nat Commun. 2018;9:4982.
Pryce J, Medley N, Choi L. Indoor residual spraying for preventing malaria in communities using insecticide-treated nets. Cochrane Database Syst Rev. 2022;CD0126:1–85.
Takarinda K, Nyadundu S, Govha E, Gombe N, Chadambuka A, Juru T, et al. Factors associated with a malaria outbreak at Tongogara refugee camp in Chipinge District, Zimbabwe: a case-control study. Malar J. 2022;21:1–12.
Tepa A, Abame I, Makamta V, Fongang B, Donkeu J, Ayong L, et al. Nutritional status and humoral immune response to Plasmodium falciparum in children aged 6–59 months. J Trop Med. 2020;2020:1–7.
Ahimbisibwe F. Uganda and the refugee problem: challenges and opportunities. Afr J Polit Sci Int Relations. 2019;13:62–72.
Uganda Country Refugee Response Plan. 2018. https://data.unhcr.org/en/documents/details/63273. Accessed on 28 Dec 2022.
Oboth P, Gavamukulya Y, Barugahare B. Prevalence and clinical outcomes of Plasmodium falciparum and intestinal parasitic infections among children in Kiryandongo refugee camp, mid-western Uganda: a cross sectional study. BMC Infect Dis. 2019;19:1–8.
Bukuluki P, Kisaakye P, Mwenyango H, Palattiyil G. Adolescent sexual behaviour in a refugee setting in Uganda. Reprod Health. 2021;18:1–11.
Bukuluki P, Mwenyango H, Katongole S, Sidhva D, Palattiyil G. The socio-economic and psychosocial impact of COVID-19 pandemic on urban refugees in Uganda. Soc Sci Humanit Open. 2020;2:100045.
The corona pandemic’s impact on the food and nutrition security of refugees in Northern Uganda. https://ruralis.no/wp-content/uploads/2021/05/ny-rapport-1_21-refugee-fsn-corona-pandemic-1.pdf. Accessed on 29 Dec 2022.
Mugerwa M. Increasing access to education for refugees in Uganda. Law Democr Dev. 2021;25:1–29.
Grosrenaud E, Okia C, Adam A, Trenchard L, Agroforestry. Challenges and opportunities in Rhino camp and Imvepi refugee settlements of Arua District, Northern Uganda. Sustain. 2021;13:1–18.
Mwangu A. An assessment of economic and environmental impacts of refugees in Nakivale, Uganda. Migr Dev. 2022;11:433–49.
Uganda Malaria. Indicator Survey 2018–19. https://www.dhsprogram.com/pubs/pdf/MIS34/MIS34.pdf. Accessed on 7 Dec 2022.
An assessment of Uganda’s progressive approach to refugee Management. https://openknowledge.worldbank.org/bitstream/handle/10986/24736/An0assessment00o0refugee0management.pdf?sequence=1&isAllowed=y. Accessed on 9 Dec 2022.
Informing the Refugee Policy Response in Uganda. : Results from the Uganda refugee and host communities household survey 2018. http://hdl.handle.net/10986/32511. Accessed on 5 Dec 2022.
Kamau A, Mtanje G, Mataza C, Mwambingu G, Mturi N, Mohammed S, et al. Malaria infection, disease and mortality among children and adults on the coast of Kenya. Malar J. 2020;19:1–12.
Kwambai T, Mori A, Nevitt S, van Eijk A, Samuels A, Robberstad B, et al. Post-discharge morbidity and mortality in children admitted with severe anaemia and other health conditions in malaria-endemic settings in Africa: a systematic review and meta-analysis. Lancet Child Adolesc Heal. 2022;6:474–83.
Ngari M, Berkley J. Severe anaemia and paediatric mortality after hospital discharge in Africa. Lancet Child Adolesc Heal. 2022;6:447–9.
Tabue R, Njeambosay B, Zeukeng F, Esemu L, Fodjo B, Nyonglema P, et al. Case definitions of clinical malaria in children from three health districts in the north region of Cameroon. Biomed Res Int. 2019;2019:1–8.
Das D, Grais R, Okiro E, Stepniewska K, Mansoor R, Van-Der KS, et al. Complex interactions between malaria and malnutrition: a systematic literature review. BMC Med. 2018;16:1–14.
Ugwu C, Zewotir T. Improving socioeconomic status may reduce the burden of malaria in sub Saharan Africa: a systematic review and meta-analysis. Malar J. 2018;17:1–10.
Boyce M, Katz R, Standley C. Risk factors for infectious diseases in urban environments of sub-Saharan Africa: a systematic review and critical appraisal of evidence. Trop Med Infect Dis. 2019;4:123.
Degarege A, Fennie K, Degarege D, Chennupati S, Madhivanan P. Improving socioeconomic status may reduce the burden of malaria in sub Saharan Africa: a systematic review and meta-analysis. PLoS ONE. 2019;14:1–26.
Cheng B, Htoo S, Mhote N, Davison C. A systematic review of factors influencing participation in two types of malaria prevention intervention in Southeast Asia. Malar J. 2021;20:1–9.
Tamire M, Addissie A, Skovbjerg S, Andersson R, Lärstad M. Socio-cultural reasons and community perceptions regarding indoor cooking using biomass fuel and traditional stoves in rural ethiopia: a qualitative study. Int J Environ Res Public Health. 2018;15:2035.
Mohan I, Kumar Kodali N, Chellappan S, Karuppusamy B, Kumar Behera S, Natarajan G, et al. Socio-economic and household determinants of malaria in adults aged 45 and above: analysis of longitudinal ageing survey in India, 2017–2018. Malar J. 2021;20:306.
Gryseels C, Durnez L, Gerrets R, Uk S, Suon S, Set S, et al. Re-imagining malaria: heterogeneity of human and mosquito behaviour in relation to residual malaria transmission in Cambodia. Malar J. 2015;14:165.
Degefa T, Githeko A, Lee M, Yan G, Yewhalaw D. Patterns of human exposure to early evening and outdoor biting mosquitoes and residual malaria transmission in Ethiopia. Acta Trop. 2021;216:105837.
Woolley K, Bartington S, Pope F, Greenfield S, Tusting L, Price M, et al. Cooking outdoors or with cleaner fuels does not increase malarial risk in children under 5 years: a cross-sectional study of 17 sub-Saharan african countries. Malar J. 2022;21:1–15.
Ignell R, Hill S. Malaria mosquito chemical ecology. Curr Opin Insect Sci. 2020;40:6–10.
Shaw W, Marcenac P, Catteruccia F. Plasmodium development in Anopheles: a tale of shared resources. Trends Parasitol. 2022;8:124–35.
Yang D, He Y, Wu B, Deng Y, Li M, Yang Q, et al. Drinking water and sanitation conditions are associated with the risk of malaria among children under five years old in sub-Saharan Africa: a logistic regression model analysis of national survey data. J Adv Res. 2020;21:1–13.
Mangani C, Frake A, Chipula G, Mkwaila W, Kakota T, Mambo I, et al. Proximity of residence to irrigation determines malaria risk and Anopheles abundance at an irrigated agroecosystem in Malawi. Am J Trop Med Hyg. 2022;106:283–92.
Obasohan P, Walters S, Jacques R, Khatab K. A scoping review of selected studies on predictor variables associated with the malaria status among children under five years in sub-Saharan Africa. Int J Environ Res Public Health. 2021;18:1–21.
Pickering A, Davis J. Freshwater availability and water fetching distance affect child health in sub-Saharan Africa. Environ Sci Technol. 2012;46:2391–7.
De Silva P, Marshall J, Silva P, Marshall J. Factors contributing to urban malaria transmission in sub-Saharan Africa: a systematic review. J Trop Med. 2012;2012:819563.
Furnival J, Olanga E, Napier M, Garner P. Housing interventions for preventing malaria. Cochrane Database Syst Rev. 2019;2019:1–18.
Paaijmans K, Thomas M. The influence of mosquito resting behaviour and associated microclimate for malaria risk. Malar J. 2011;10:183.
Lindsay S, Jawara M, Mwesigwa J, Achan J, Bayoh N, Bradley J, et al. Reduced mosquito survival in metal-roof houses may contribute to a decline in malaria transmission in sub-Saharan Africa. Sci Rep. 2019;9:1–10.
Richards S, Byrd B, Reiskind M, White A. Assessing insecticide resistance in adult mosquitoes: perspectives on current methods. Environ Health Insights. 2020. https://doi.org/10.1177/1178630220952790.
Carrasco D, Lefèvre T, Moiroux N, Pennetier C, Chandre F, Cohuet A. Behavioural adaptations of mosquito vectors to insecticide control. Curr Opin Insect Sci. 2019;34:48–54.
Orok A, Ajibaye O, Aina O, Iboma G, Adagyo Oboshi S, Iwalokun B. Malaria interventions and control programes in sub-Saharan Africa: a narrative review. Cogent Med. 2021;8(1):1940639.
Okumu F, Gyapong M, Casamitjana N, Castro MC, Itoe M, Okonofua F, et al. What Africa can do to accelerate and sustain progress against malaria. PLOS Glob Public Heal. 2022;2(6):262.
Acknowledgements
We would like to thank the DHS program for authorising us to use the data used in this study.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
HMS contributed to conceptualisation, methodology, data acquisition, formal analysis, visualisation, validation, preparation, revision and editing of the original draft. SL participated in conceptualisation, methodology, validation, revision of the original draft and supervision. PIM, FM, MS, DN, HW and PK helped with the conceptualisation, revision of the original draft. All authors approved the final manuscript. All authors read and approved this version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the ethical principles stated in the Helsinki Declaration. The launch of MIS (phase DHS-VII) data collection was conditional on the authorisation of the National Statistical Council and the approval of the National Committee on Health Research Ethics. During data collection, the informed consent of eligible respondents was sought before starting the interviews. The dataset used was fully anonymised.
Consent for publication
Not applicable.
Competing interests
Neither of the authors discloses any potential or actual conflict of interest. No financial or nonfinancial benefits have been or will be received from any party related directly or indirectly to the subject of this article.
Supplementary Information
Additional file 1.
Table S1. Household level risk factors associated with malaria infections among children. Table S2. Selected explanatory variables that were used to predict malaria infections.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Semakula, H.M., Liang, S., Mukwaya, P.I. et al. Determinants of malaria infections among children in refugee settlements in Uganda during 2018–2019. Infect Dis Poverty 12, 31 (2023). https://doi.org/10.1186/s40249-023-01090-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-023-01090-3