Abstract
Background
HER2-positive breast cancer occurs in 15–20% of breast cancer patients and is characterized by poor prognosis. Trastuzumab is considered the key drug for treatment of HER2-positive breast cancer patients. It improves patient survival; however, resistance to trastuzumab remains a challenge in HER2-positive breast cancer patients. Therefore, the prediction of response to trastuzumab is crucial to choose optimal treatment regimens. The aim of the study was to identify genetic variants that could predict response to anti-HER2-targeted therapy (trastuzumab) using next-generation sequencing.
Method
Genetic variants in the hotspot regions of 17 genes were studied in 24 Formalin-Fixed Paraffin-Embedded (FFPE) samples using Ion S5 next-generation sequencing system. FFPE samples were collected from HER2‑positive breast cancer patients previously treated with anti‑HER2‑targeted treatment (Trastuzumab). Patients were divided into two groups; trastuzumab-sensitive group and trastuzumab-resistant group based on their response to targeted therapy.
Results
We identified 29 genetic variants in nine genes that only occurred in trastuzumab-resistant patients and could be associated with resistance to targeted therapy including TP53, ATM, RB1, MLH1, SMARCB1, SMO, GNAS, CDH1, and VHL. Four variants out of these 29 variants were repeated in more than one patient; two variants in TP53, one variant in ATM gene, and the last variant in RB1 gene. In addition, three genes were found to be mutated only in resistant patients; MLH1, SMARCB1 and SMO genes. Moreover, one novel allele (c.407A > G, p. Gln136Arg) was detected within exon 4 of TP53 gene in one resistant patient.
Conclusion
NGS sequencing is a useful tool to detect genetic variants that could predict response to trastuzumab therapy.
Similar content being viewed by others
Introduction
Breast cancer is the most common cancer and the first cause of cancer deaths in females worldwide [1]. In 2020, there were 2.26 million newly diagnosed cases accounting for 24.5% of total new cancer cases, and 684,996 deaths of breast cancer accounting for 15.5% of total cancer deaths globally [1]. In Egypt, breast cancer was responsible for 32.4% of all newly diagnosed cancer cases and 10.3% of all cancer-related fatalities in 2020 [1].
HER2 overexpression occurs in approximately 15–20% of breast cancer cases [2]. HER2-positive breast cancer is characterized by a high histological grade, a high risk for metastasis, and therefore a worse prognosis [3]. However, anti‑HER2‑targeted drugs, such as trastuzumab, pertuzumab, and lapatinib, can block HER2 activity reducing tumor aggressiveness and improving patient survival [4]. They are typically given with chemotherapy as neoadjuvant or adjuvant treatment for HER2-positive breast cancer [5].
The response to anti-HER2-targeted therapy was found to vary among patients with the presence of patients who relapse or develop metastasis during therapy [6]. Therefore, prediction of response to HER2-targeted therapy is crucial to avoid undesirable side effects and for choosing more effective alternatives for patients [7].
HER2-positive breast cancer results from the interplay between genetic and lifestyle/environmental risk factors [8]. Genetic determinants can explain the resistance of some patients to anti-HER2 therapy [9]. Many genetic mutations in HER2 downstream signaling pathways were identified to confer drug resistance as mutations in PI3K, Akt, and PDK genes [10]. Mutations in DNA damage repair pathways were also investigated for association with treatment response such as PTEN, TP53, ATM, STK11, and RB1 [11,12,13,14,15].
Therefore, studying genetic variants in tissue samples of breast cancer patients will aid in individualizing therapy with better outcomes [9]. Next-generation sequencing allows multiple parallel sequencing of several genes at same time [16]. While genome-wide analysis has the most significant role in the classification of breast cancer, targeted sequencing gives deeper coverage through reducing the number of analyzed genes [17, 18]. Targeted sequencing can be used to investigate hotspot cancer-driver mutations in breast cancer and thereafter study mutations that affect signaling pathways conferring anti-HER2 drug resistance [11, 19]. Therefore, we aimed in this study to survey genetic variants in HER2-positive breast cancer patients that may be associated with anti-HER2 drug (trastuzumab) resistance.
Subjects and methods
This study is a retrospective study, in which formalin-fixed paraffin-embedded tissues (FFPE) samples were collected between December 2020 and December 2021 from 24 HER2‑positive breast cancer patients treated with anti‑HER2‑targeted therapy (trastuzumab), after approval of Alexandria Ethics Committee of Faculty of Medicine. The patients were recruited from Clinical Oncology and Nuclear Medicine Department at Alexandria Main University Hospital. Cases were divided into two groups; trastuzumab-sensitive group and trastuzumab-resistant group. Trastuzumab-sensitive group included 12 patients in complete remission for 2 years or more from the start of anti-HER2-targeted therapy. Trastuzumab-resistant group included patients who relapsed or developed metastasis during receiving or within 2 years of the targeted therapy. Patients with metastatic breast cancer at the time of diagnosis were excluded from the study. The positivity of HER-2 neu status was determined using immunohistochemistry (IHC) and fluorescence in situ hybridization. IHC was performed on paraffin-embedded tissue samples to evaluate hormone receptor (HR); estrogen (ER) and progesterone (PR). Informed consents were obtained from all enrolled patients in the study.
DNA extraction
DNA was extracted from FFPE tissue samples using QIAamp DNA FFPE Tissue Kit (QIAGEN, Germany). The concentration of DNA was determined using Qubit™ 1X dsDNA HS (High Sensitivity) Assay with Qubit™ 4 Fluorometer (ThermoFisher Scientific, USA) according to the manufacturer’s recommendations.
Library preparation
DNA libraries were constructed from 10 ng genomic DNA per sample using the Ion AmpliSeq™ Library Kit Plus (ThermoFisher Scientific, USA) according to the manufacturer’s protocol to study approximately 1500 COSMIC mutations from 17 oncogenes and tumor suppressor genes (ATM, RB1, MLH1, NPM1, STK11, CDKN2A, TP53, SMARCB1, VHL, CDH1, EZH2, IDH1, IDH2, GNA11, GNAS, GNAQ, and SMO).
Ion Xpress™ Barcode Adapters Kit (Thermo Fisher Scientific, USA) and Agencourt™ AMPure™ XP Reagent (Beckman Coulter, USA) were used for amplicons adaptors ligation and purification to ensure that each individual sample had a unique ID. The final amplicon libraries were quantified using Ion Library TaqMan™ Quantitation kit (Thermo Fisher Scientific, USA) according to the manufacturer's instructions and were equalized to ~ 100 pM and then combined to form one library pool.
Emulsion PCR and sequencing
The Ion 520™ and Ion 530™ Kit—OT2 (Thermo Fisher Scientific, USA) was first used to prepare enriched, template-positive Ion Sphere™ Particles (ISPs) using the Ion OneTouch™ 2 System (Thermo Fisher Scientific, USA) according to the manufacturer’s protocol. The enriched, template-positive ISPs were then loaded on Ion 520™ Chip (ThermoFisher Scientific, USA) and sequenced using Ion S5™ next generation sequencing system (ThermoFisher Scientific, USA).
Bioinformatic analysis
Torrent Suite™ Software (ThermoFisher Scientific, USA) was used to plan and monitor sequencing runs, view sequencer activity, and analysis of barcode reads, alignment of reads to hg19 reference genome; and generation of run metrics to determine the quality of the run. Ion Reporter™ Software (ThermoFisher Scientific, USA) was used for the annotation of single-nucleotide, insertions, deletions, and splice site alterations. All genetic variants with a minimum depth of coverage of 30 × were included in the study. Allelic frequency ranged from 1.01 to 11.6%.
Statistical analysis of the data
Data were analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using number and percent. Chi-square test was used for categorical variables, to compare between different groups. Fisher’s Exact or Monte Carlo correction for chi-square was used when more than 20% of the cells have an expected count less than 5. The Shapiro–Wilk test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean ± standard deviation. Student t test was used for normally distributed quantitative variables, to compare between two studied groups. Significance of the obtained results was judged at the 5% level.
Results
Patient characteristics
The age of trastuzumab-sensitive HER2-positive breast cancer patients ranged from 35 to 61 years old, while age ranged from 36 to 60 years old in trastuzumab-resistant group. The predominant histopathological subtype of breast cancer was infiltrating ductal carcinoma (100% of patients). Meanwhile, ER−, PR−, HER2+ breast cancer was the most common molecular subtype in both sensitive group and resistant group; representing 50% and 66.7% of patients, respectively. No significant difference was found between both groups as regards age, tumor stage, grade and lines of treatment. All demographic and clinicopathological data are summarized in Table 1.
Genetic variants in HER2-positive breast cancer patients
A total of 107 genetic variants in 11 genes were identified in 19 HER2-positive breast cancer patients. Most of the genetic variants (59.8%) were identified in TP53 gene, followed by VHL (11.2%), and ATM (9.3%) (Fig. 1). No mutations were identified in six genes (NPM1, CDKN2A, EZH2, IDH2, GNA11, and GNAQ). The mutation frequency ranged from 2 to 13 variants per patient with a mean of 5 variants.
The mutational prevalence of the studied genes among patients varied widely from 62.5 to 0%. The most frequently mutated gene was TP53 in 62.5% of the patients, followed by ATM (29.2%), VHL (20.8%), and IDH1 (20.8%) (Fig. 2).
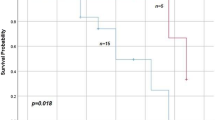
Seven genes were identified to be mutated in both trastuzumab-sensitive and trastuzumab-resistant patients (ATM, CDH1, GNAS, IDH1, RB1, TP53, and VHL). STK11 gene was mutated only in the sensitive group. On the other hand, MLH1, SMARCB1, and SMO genes were only mutated in the resistant group (Fig. 3).
SNV in trastuzumab-sensitive and trastuzumab-resistant patients
A total of 57 genetic variants were identified in eight genes (ATM, CDH1, GNAS, IDH1, RB1, STK11, TP53, and VHL) in ten trastuzumab-sensitive patients (83.3%). While, in trastuzumab-resistant group, a total of 50 genetic variants were identified in ten genes (ATM, CDH1, GNAS, IDH1, MLH1, RB1, SMARCB1, SMO, TP53, and VHL) in nine patients (75%). The most frequently mutated gene was TP53 in both groups followed by VHL in trastuzumab-sensitive patients and ATM in trastuzumab-resistant group (Figs. 4, 5) (Additional file 1: Tables S1, S2).
Missense variants were the most common variant type in both sensitive and resistant groups accounting for 63.2% and 76% of variants, respectively. We also found 77.1% of TP53 variants in the sensitive group were missense variants, followed by nonsense variants (8.6%), synonymous variants (5.7%), frameshift variants (5.7%), and indels (2.9%). TP53 variants were located mainly within exon 6, exon 7, and exon 4, respectively. In trastuzumab-resistant group, 75.9% of TP53 variants were missense variants, followed by frameshift variants (10.4%), splice-site variants (6.9%), synonymous variants (3.4%), and indels (3.4%). They were located mainly within exon 6, exon 7, exon 4, and exon 9, respectively (Additional file 1: Tables S3, S4).
Regarding clinical significance, pathogenic variants were the most common variants in HER2-positive breast cancer patients accounting for 28.1% of variants in the sensitive group and 34% of variants in the resistant group. Meanwhile, likely pathogenic variants accounted for 12.3% of variants in the sensitive group but 20% of variants in the resistant group (Figs. 6, 7). Similarly, TP53 pathogenic and likely pathogenic variants together were the most common variants in TP53 gene in both groups. They accounted together for 34.2% of variants in the sensitive group and almost half of variants (48.3%) in the resistant group (Additional file 1: Tables S5, S6).
SNV associated with targeted therapy response
By comparing the genetic variants in the sensitive group to the resistant group, we identified 29 variants in nine genes (ATM, CDH1, GNAS, MLH1, RB1, SMARCB1, SMO, TP53, and VHL) in nine patients that only occurred in trastuzumab-resistant patients and could be associated with resistance to trastuzumab therapy; nine pathogenic variants, five likely pathogenic variants, seven variants with uncertain significance, four likely benign variants, one benign variant, two with conflicting interpretation with pathogenicity, and one novel variant allele (Table 2). Some of these variants was repeated in more than one patient.
Sixteen variants were identified in TP53 gene (55.2%) in six trastuzumab-resistant patients, these variants were mainly distributed in exons 6, exon 7, and exon 9. Five variants were identified in ATM gene (17.2%) in three resistant patients, they were located mainly in exon 38 and exon 54. In addition, two RB1 variants (6.9%) located in exon 17 and exon 22 were identified in three resistant patients. Four resistant patients were found to harbor the remaining six variants that were identified in CDH1, GNAS, MLH1, SMARCB1, SMO, and VHL genes (20.7%).
Interestingly, four variants were found to be repeated in more than one resistant patient. Two variants were in TP53 gene; a likely pathogenic variant p.Ser241Phe in exon 6 that leads to replacement of serine at codon 241 by phenylalanine [20], this variant was identified in two resistant patients (No. 1 and No. 2). Another splice site variant c.376-2dup, which affects mRNA splicing resulting in abnormal protein. This variant was identified in two resistant patients (No. 2 and No. 6). It was reported to have conflicting interpretations of pathogenicity with mainly uncertain significance [21]. The third variant was in ATM gene; p.Val1941Leu and was identified in two resistant patients (No. 5 and No. 7). It is located in exon 38 with conflicting interpretations of pathogenicity. It results from a G to C substitution at nucleotide position 5821 which replaces valine by leucine at codon 1941 [22]. The last variant is a pathogenic RB1 variant p.Arg556Ter located in exon 17. It was identified in two resistant patients (No. 2 and No. 3). It is a nonsense variant that results from replacing C by T nucleotide at position 1666 leading to a premature stop codon at codon 556 [23].
In addition, we identified three variants in MLH1, SMARCB1, and SMO genes. These genes were only mutated in the resistant group. MLH1 p.Val384Asp is a missense benign variant located in exon 12, where valine is replaced by aspartic acid at codon 384 [24]. It was identified in resistant patient (No. 3) who was diagnosed with Luminal B (ER+, PR+, HER2+) breast cancer in stage IIIA and grade II. This patient underwent surgery and received Adriamycin, Cyclophosphamide, Taxol, Tamoxifen and Herceptin. However, she developed pulmonary metastasis and died later. SMARCB1 p.Arg40Ter is a nonsense pathogenic variant within exon 2 which results in a premature translational stop signal at codon 40 of SMARCB1 gene [25]. It was identified in resistant patient (No. 9). Lastly, SMO p.Trp535Leu is also a pathogenic but missense variant located in exon 9 [26] which was identified in resistant patient (No. 5).
Furthermore, a novel allele (c.407A > G, p.Gln136Arg) within exon 4 in TP53 (rs1567554216) was identified in resistant patient (No. 1). TP53 p.Gln136Arg is a missense variant where amino acid glutamine is replaced by arginine at codon 136 (Q [CAA] > R [CGA]) of the TP53 protein due to A to G substitution at nucleotide position 407. Resistant patient (No. 1) was diagnosed with HER2-enriched breast cancer (ER−, PR−, HER2+) in stage IIIA and grade II. She was first diagnosed with a right breast mass lesion and right axillary lymph node metastasis to which she underwent radical mastectomy and treatment with Adriamycin/ Cyclophosphamide, Taxotere, and Herceptin. However, 1 year later she developed a local recurrence with skin infiltration. Genetic analysis of this patient identified seven TP53 variants (p.Ser241Phe, p.Thr211=, p.Cys135Gly, p.Arg248Leu, p.Arg249Ser, p.Gly302ArgfsTer4, and p.Gln136Arg), four ATM variants (p.Gly2709Ser, p.Pro2699Leu, p.Pro3050Leu, and p.Lys1692Asn), CDH1 p.Val85Ala and IDH1 p.Arg132His.
Resistant patient (No. 2) was diagnosed with HER2-enriched left breast cancer (ER−, PR−, HER2+) in stage III and grade III. She received systematic treatment. Unfortunately, 10 months later, she complained of neurological symptoms (numbness and tingling), MRI Brain with GAD revealed metastatic deposits, and additionally, CT chest revealed pulmonary metastatic nodules. The genetic analysis revealed five TP53 variants (p.Cys135Gly, p.Ser241Phe, p.Arg249Ser, p.Arg248Leu, and a splice site variant c.376-2dup), ATM p.Arg3008Cys, IDH1 p.Arg132His, and RB1 p.Arg556Ter. Most identified variants were pathogenic and likely pathogenic (75%) and three variants (TP53 p.Ser241Phe, TP53 c.376-2dup and RB1 c.1666C > T) of which were only repeated in other resistant patients.
Discussion
HER2-positive breast cancers account 15–20% of all breast cancer cases and show aggressive course and a poor prognosis [2, 3]. Currently, there are many FDA-approved HER2-targeted therapies including monoclonal antibodies (e.g., trastuzumab and pertuzumab), antibody–drug conjugates (e.g., T-DM1 and DS-8201), and small-molecule HER1/2 TKIs (e.g., lapatinib, neratinib, and tucatinib) [27]. Trastuzumab (Herceptin) is the first FDA-approved and is key for treatment of HER2-positive breast cancer [28]. Although trastuzumab significantly improves disease-free survival (DFS), about 25% of patients with early-stage HER2-positive breast cancer disease will relapse after trastuzumab treatment. It may be attributed to the mutation of the target itself after anti-HER2 treatment with down-regulation or loss of HER2 expression, which leads to changes in drug binding or mutations in the HER2 downstream intracellular signaling pathways which when activated, promote tumorigenesis such as PI3K/ AKT/mTOR pathway [27, 29].
In the era of individualized precision medicine, the application of NGS allows the detection of genetic aberrations, which could serve as potential biomarkers for predicting trastuzumab resistance. Consequently, these markers can separate patients who would benefit only from monotherapy from high-risk patients who require combination therapy with adjustment of treatment plans, to ensure favorable prognosis and effectively reduce the treatment cost and side effects [11, 30, 31]. A number of adverse events have been linked to the use of trastuzumab, including acute cardiac toxicity, minor hematologic deficiencies, gastrointestinal symptoms, and pulmonary symptoms [32]. In case of trastuzumab resistance, other drugs can be used such as small molecule TKIs either alone or with monoclonal antibodies, or an ADCs. The second-generation monoclonal antibody margetuximab has been also approved by the FDA for use with chemotherapy for the treatment of previously treated metastatic HER2-positive breast cancer [27].
NGS platform was used in the current study to survey genetic mutations in selected genes that could confer resistance to trastuzumab therapy using FFPE samples. Genetic analysis revealed the presence of 107 genetic variants in HER2-positive breast cancer patients. The most frequent genetic variants were found in TP53 gene, followed by VHL and ATM genes.
By comparing the genetic variants in the sensitive group to the resistant group, 29 variants were identified in nine genes (ATM, CDH1, GNAS, MLH1, RB1, SMARCB1, SMO, TP53, and VHL) in nine patients that only occurred in trastuzumab-resistant patients and could be associated with resistance to anti-HER2-targeted therapy. The most frequent variants were identified in TP53. Pathogenic and likely pathogenic TP53 variants were found to be more frequent in the resistant group compared to the sensitive group.
Similarly, Ye et al. studied the response to trastuzumab using 24 cfDNA samples from 20 patients with HER2‑positive metastatic breast cancer. They reported that genetic variants in TP53 gene were among the most frequent genetic variants in their study [33]. p53 signaling pathway is activated when cells are under stress such as DNA damage. Upon activation, p53 protein works as a transcription factor that transactivates multiple target genes that initiate cell cycle arrest, apoptosis, DNA repair and inhibit metastasis [34, 35]. Breast cancer is actually reported to be the most common cancer (25.5%) in women with pathogenic TP53 mutations [36, 37]. Moreover, the percentage TP53 mutations could reach 70% of HER2-positive breast cancer patients both correlating with a poor prognosis [38,39,40]. TP53 loss of function mutations were found to be associated with resistance to cytotoxic anticancer drugs in breast cancer patients [41]. However, Fountzilas et al. reported that p53-mutated tumors had longer disease-free survival in patients treated with trastuzumab compared to patients not treated with the drug [42]. Therefore, they suggested that the combination of HER2-targeted drugs with anti-mutp53 therapy could provide a synergistic effect in treatment of HER2-positive breast cancer patients [40].
Interestingly, two variants in TP53 gene were found to be present in more than one resistant patient; p.Ser241Phe and c.376-2dup. p.Ser241Phe is a likely pathogenic variant located in exon 6, it was identified in two resistant patients. It was previously reported by Chang et al. in breast cancer patients [43]. c.376-2dup is a splice site variant that was previously reported by Hauke et al. in breast cancer [44]. It was found in two resistant patients in our study. However, the implication of these two variants in treatment response is not clear.
We also identified a novel allele (c.407A > G, p.Gln136Arg) within exon 4 in TP53 variant (rs1567554216) in one resistant patient. The variant rs1567554216 was reported in Li–Fraumeni syndrome but with allele (c.407A > C, p.Gln136Pro) where glutamine is replaced by proline at codon 136. The latter variant TP53 p.Gln136Pro is considered of uncertain significance [45,46,47].
Our results showed that ATM mutations were more frequent in resistant patients compared to sensitive patients. ATM variant p.Val1941Leu in exon 38 was found in two resistant patients. It was reported to cause reduced ATM protein level and kinase activity [48]. ATM works as a tumor suppressor gene with a central role in DNA damage response due to double-stranded breaks [14]. ATM mutations were found to be associated with an increased risk of breast cancer and ATM loss of function was reported in familial breast cancer patients [22, 49, 50]. Stagni et al., reported that ATM protein activity could enhance HER2-dependent tumorigenicity and ATM works as a novel modulator of HER2 protein stability by preventing HER2 degradation. They also reported that ATM inhibition or loss of function could induce trastuzumab resistance [14].
Moreover, a pathogenic variant RB1 p.Arg556Ter in exon 17 was found also in two resistant patients. However, this variant was mainly reported in retinoblastoma [51, 52]. RB1 is a tumor suppressor gene that is mutated in several types of cancer [53]. RB1 gene under-expression was actually reported to promote breast carcinogenesis [54]. Moreover, RB pathway is frequently altered in HER2+ tumors [55]. Risi et al. [15] suggested that RB1 loss of function gene signature (RBsig) could predict response to neoadjuvant chemotherapy in combination with trastuzumab, lapatinib or both in breast cancer.
In addition, we found three genes MLH1, SMARCB1, and SMO that were only mutated in the resistant group. p.Val384Asp in MLH1 gene is a benign variant, however, Lee et al. [56] reported that this variant has high prevalence in HER2-positive luminal B breast cancer which is correlated with breast cancer molecular subtype in our patient harboring this variant. Chiu et al. [24] also stated that MLH1 p.Val384Asp is associated with poor response to EGFR tyrosine kinase inhibitors but in patients with lung adenocarcinoma. Qing Ye et al. reported MLH1 as Herceptin resistance-associated gene. They identified four MLH1 variants (p.Phe155Ser, p.Gln168Lys, p.Val143Asp, and p.Ser160Asn) only present in Herceptin-resistant HER2-positive breast cancer patients [33]. The activity of the mismatch repair system is crucial for removal of several polymerase errors, including base substitution and insertion-deletion mismatches that can form during the replication [57]. Loss of function of MLH1 gene was reported to be associated with resistance to anticancer drugs and poor disease-free survival [58].p.Arg40Ter variant in SMARCB1gene is a pathogenic variant that was reported to have a predisposition to various cancers but mainly rhabdoid tumors [25]. SMO p.Trp535Leu is a missense pathogenic variant, it was reported by Xie et al. [26] but in basal cell carcinoma. SMO gene is one of the genes in Hedgehog (HH) signaling pathway whose expression correlates with tumor size, metastasis, and recurrence. Thus, it can be targeted by SMO inhibitors which are investigated for treatment of breast, liver, and colon cancer. However, SMO mutations can cause resistance to these inhibitors [59, 60].p.Arg201His variant was detected in GNAS gene in one resistant patient. It is a pathogenic variant that was previously reported in breast cancer [43]. GNAS gene was one of the anti‑HER2 therapy resistance‑associated genes reported by Qing et al. who detected seven GNAS variants (p.Arg186His, p.Asp181Gly, p.Asn203Ser, p.Arg216Leu, p.Met206Val, p.Arg216Cys, and p.Asp214Asn) only present in Herceptin-resistant breast cancer patients [33]. GNAS was found to induce breast cancer cell proliferation and metastasis through the PI3K/AKT/Snail1/E-cadherin signaling pathway [61].
We also identified some other variants (TP53 p.Pro3050Leu, TP53 p.Val272Met, TP53 p.Phe270Leu, TP53 p.Arg337Pro, and TP53 p.Ile254Va) in the resistant group that have been previously reported in breast cancer [43, 62, 63]. However no association with treatment was found.
Moreover, 11 common genetic variants were identified in four genes (TP53, IDH1, ATM, and GNAS) in both sensitive and resistant groups. Eight variants were in TP53 gene (p.Cys135Gly, p.Glu349fs, p.Arg248Leu, p.Pro278Ser, p.Asp281Ala, p.Arg249Ser, p.Ser127Phe, and p.Arg280Gly), three variants in IDH1 gene (p.Arg132His), ATM gene (p.Arg3008Cys), and GNAS gene (p.Arg201Cys). Interestingly, Chang et al. [43] reported the same seven variants (TP53 p.Cys135Gly, TP53 p.Arg248Leu, TP53 p.Pro278Ser, TP53 p.Asp281Ala, TP53 p.Arg280Gly, IDH1 p.Arg132His, and GNAS p.Arg201Cys) in breast neoplasm in their study. The similarity of results could highlight the pathogenic contribution of these variants in breast cancer specifically TP53 variants that cause dysregulated p53 signaling pathway which is an early incident in breast tumorigenesis [35]. In addition, TP53 variant p.Glu349fs was reported to be associated with response to PARP inhibitors but in prostate cancer [64].
The main limitations of this study were the small number of cases included, and lack of study of the underlying molecular mechanisms by which the detected variants can cause trastuzumab resistance. Therefore, we recommended future studies with a larger sample size to confirm the association between the detected genetic variants and trastuzumab response and to study the mechanisms by which the detected variants could affect trastuzumab response in order to discover new therapeutic targets. In addition, we recommend to study the association between genetic variants and other anti-HER2 drugs.
Based on previous findings, we concluded that targeted next-generation sequencing is a useful tool to detect DNA mutations that could have clinical utility in predicting response to anti-HER2-targeted therapy allowing individualized treatment regimens for HER2-positive breast cancer patients.
Availability of data and materials
The data supporting the conclusions are included within the article.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Cho N. Molecular subtypes and imaging phenotypes of breast cancer. Ultrasonography. 2016;35(4):281.
Feng Y, Spezia M, Huang S, Yuan C, Zeng Z, Zhang L, et al. Breast cancer development and progression: risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis. Genes Dis. 2018;5(2):77–106.
Llombart-Cussac A, Cortés J, Paré L, Galván P, Bermejo B, Martínez N, et al. HER2-enriched subtype as a predictor of pathological complete response following trastuzumab and lapatinib without chemotherapy in early-stage HER2-positive breast cancer (PAMELA): an open-label, single-group, multicentre, phase 2 trial. Lancet Oncol. 2017;18(4):545–54.
Harbeck N. Neoadjuvant and adjuvant treatment of patients with HER2-positive early breast cancer. Breast. 2022;62(Suppl 1):S12–6.
Vogel CL, Cobleigh MA, Tripathy D, Gutheil JC, Harris LN, Fehrenbacher L, et al. Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol. 2002;20(3):719–26.
Pernas S, Tolaney SM. HER2-positive breast cancer: new therapeutic frontiers and overcoming resistance. Ther Adv Med. 2019;11:1758835919833519.
Mbemi A, Khanna S, Njiki S, Yedjou CG, Tchounwou PB. Impact of gene-environment interactions on cancer development. Int J Environ Res Public Health. 2020;17(21):8089.
Smith AE, Ferraro E, Safonov A, Morales CB, Lahuerta EJA, Li Q, Kulick A, Ross D, Solit DB, de Stanchina E, Reis-Filho J, Rosen N, Arribas J, Razavi P, Chandarlapaty S. HER2+ breast cancers evade anti-HER2 therapy via a switch in driver pathway. Nat Commun. 2021;12(1):6667.
Esteva FJ, Guo H, Zhang S, Santa-Maria C, Stone S, Lanchbury JS, et al. PTEN, PIK3CA, p-AKT, and p-p70S6K status: association with trastuzumab response and survival in patients with HER2-positive metastatic breast cancer. Am J Pathol. 2010;177(4):1647–56.
Mardis ER. The impact of next-generation sequencing on cancer genomics: from discovery to clinic. Cold Spring Harb Perspect Med. 2019;9(9): a036269.
Loi S, Michiels S, Lambrechts D, Fumagalli D, Claes B, Kellokumpu-Lehtinen P-L, et al. Somatic mutation profiling and associations with prognosis and trastuzumab benefit in early breast cancer. J Natl Cancer Inst. 2013;105(13):960–7.
Glück S, Ross JS, Royce M, McKenna EF, Perou CM, Avisar E, et al. TP53 genomics predict higher clinical and pathologic tumor response in operable early-stage breast cancer treated with docetaxel-capecitabine±trastuzumab. Breast Cancer Res Treat. 2012;132(3):781–91.
Stagni V, Manni I, Oropallo V, Mottolese M, Di Benedetto A, Piaggio G, et al. ATM kinase sustains HER2 tumorigenicity in breast cancer. Nat Commun. 2015;6(1):1–10.
Risi E, Biagioni C, Benelli M, Migliaccio I, McCartney A, Bonechi M, et al. An RB-1 loss of function gene signature as a tool to predict response to neoadjuvant chemotherapy plus anti-HER2 agents: a substudy of the NeoALTTO trial (BIG 1-06). Ther Adv Med Oncol. 2019;11:1758835919891608.
Nguyen HT, Le HT, Nguyen LT, Lou H, LaFramboise T. The applications of massive parallel sequencing (next-generation sequencing) in research and molecular diagnosis of human genetic diseases. VJSTE. 2018;60(2):30–43.
Han S-W, Kim H-P, Shin J-Y, Jeong E-G, Lee W-C, Lee K-H, et al. Targeted sequencing of cancer-related genes in colorectal cancer using next-generation sequencing. PLoS ONE. 2013;8(5): e64271.
Zhang H, Ahearn TU, Lecarpentier J, Barnes D, Beesley J, Qi G, et al. Genome-wide association study identifies 32 novel breast cancer susceptibility loci from overall and subtype-specific analyses. Nat Genet. 2020;52(6):572–81.
Grada A, Weinbrecht K. Next-generation sequencing: methodology and application. J Investig Dermatol. 2013;133(8): e11.
Kato S, Han S-Y, Liu W, Otsuka K, Shibata H, Kanamaru R, et al. Understanding the function–structure and function–mutation relationships of p53 tumor suppressor protein by high-resolution missense mutation analysis. Proc Nat Acad Sci U S A. 2003;100(14):8424–9.
Tsaousis GN, Papadopoulou E, Apessos A, Agiannitopoulos K, Pepe G, Kampouri S, et al. Analysis of hereditary cancer syndromes by using a panel of genes: novel and multiple pathogenic mutations. BMC Cancer. 2019;19(1):1–19.
Renwick A, Thompson D, Seal S, Kelly P, Chagtai T, Ahmed M, et al. ATM mutations that cause ataxia-telangiectasia are breast cancer susceptibility alleles. Nat Genet. 2006;38(8):873–5.
Sampieri K, Hadjistilianou T, Mari F, Speciale C, Mencarelli MA, Cetta F, et al. Mutational screening of the RB1 gene in Italian patients with retinoblastoma reveals 11 novel mutations. J Hum Genet. 2006;51(3):209–16.
Chiu C-H, Ho H-L, Doong H, Yeh Y-C, Chen M-Y, Chou T-Y, et al. MLH1 V384D polymorphism associates with poor response to EGFR tyrosine kinase inhibitors in patients with EGFR L858R-positive lung adenocarcinoma. Oncotarget. 2015;6(10):8407.
Sévenet N, Sheridan E, Amram D, Schneider P, Handgretinger R, Delattre O. Constitutional mutations of the hSNF5/INI1 gene predispose to a variety of cancers. Am J Hum Genet. 1999;65(5):1342–8.
Xie J, Murone M, Luoh S-M, Ryan A, Gu Q, Zhang C, et al. Activating smoothened mutations in sporadic basal-cell carcinoma. Nature. 1998;391(6662):90–2.
Wu X, Yang H, Yu X, Qin J-J. Drug-resistant HER2-positive breast cancer: molecular mechanisms and overcoming strategies. Front Pharmacol. 2022;13:3952.
Wang Z-H, Zheng Z-Q, Liu S-N, Xiao X-F, Chen G-Y, Liang W-Q, et al. Trastuzumab resistance in HER2-positive breast cancer: mechanisms, emerging biomarkers and targeting agents. Front Oncol. 2022;12:1006429.
Shi W, Jiang T, Nuciforo P, Hatzis C, Holmes E, Harbeck N, et al. Pathway level alterations rather than mutations in single genes predict response to HER2-targeted therapies in the neo-ALTTO trial. Ann Oncol. 2017;28(1):128–35.
Heather JM, Chain B. The sequence of sequencers: the history of sequencing DNA. Genomics. 2016;107(1):1–8.
Hayes DN, Kim WY. The next steps in next-gen sequencing of cancer genomes. J Clin Investig. 2015;125(2):462–8.
Wang J, Xu B. Targeted therapeutic options and future perspectives for HER2-positive breast cancer. Signal Transduct Targeted Ther. 2019;4(1):34.
Ye Q, Qi F, Bian L, Zhang S-H, Wang T, Jiang Z-F. Circulating-free DNA mutation associated with response of targeted therapy in human epidermal growth factor receptor 2-positive metastatic breast cancer. Chin Med J. 2017;130(05):522–9.
Shahbandi A, Nguyen HD, Jackson JG. TP53 mutations and outcomes in breast cancer: reading beyond the headlines. Trends Cancer. 2020;6(2):98–110.
Børresen-Dale AL. TP53 and breast cancer. Hum Mutat. 2003;21(3):292–300.
Palmero EI, Achatz MI, Ashton-Prolla P, Olivier M, Hainaut P. Tumor protein 53 mutations and inherited cancer: beyond Li-Fraumeni syndrome. Curr Opin Oncol. 2010;22(1):64–9.
Janavičius R, Andrėkutė K, Mickys U, Rudaitis V, Brasiūnienė B, Griškevičius L. Apparently, “BRCA-related” breast and ovarian cancer patient with germline TP53 mutation. Breast J. 2011;17(4):409–15.
Nik-Zainal S, Davies H, Staaf J, Ramakrishna M, Glodzik D, Zou X, et al. Landscape of somatic mutations in 560 breast cancer whole-genome sequences. Nature. 2016;534(7605):47–54.
Silwal-Pandit L, Vollan HKM, Chin S-F, Rueda OM, McKinney S, Osako T, et al. TP53 mutation spectrum in breast cancer is subtype specific and has distinct prognostic relevanceTP53 in breast cancer. Clin Cancer Res. 2014;20(13):3569–80.
Fedorova O, Daks A, Shuvalov O, Kizenko A, Petukhov A, Gnennaya Y, et al. Attenuation of p53 mutant as an approach for treatment Her2-positive cancer. Cell Death Discov. 2020;6(1):100.
Chang EH, Pirollo KF, Bouker KB. Tp53 gene therapy: a key to modulating resistance to anticancer therapies? Mol Med Today. 2000;6(9):358–65.
Fountzilas G, Giannoulatou E, Alexopoulou Z, Zagouri F, Timotheadou E, Papadopoulou K, et al. TP53 mutations and protein immunopositivity may predict for poor outcome but also for trastuzumab benefit in patients with early breast cancer treated in the adjuvant setting. Oncotarget. 2016;7(22):32731.
Chang MT, Asthana S, Gao SP, Lee BH, Chapman JS, Kandoth C, et al. Identifying recurrent mutations in cancer reveals widespread lineage diversity and mutational specificity. Nat Biotechnol. 2016;34(2):155–63.
Hauke J, Horvath J, Groß E, Gehrig A, Honisch E, Hackmann K, et al. Gene panel testing of 5589 BRCA 1/2-negative index patients with breast cancer in a routine diagnostic setting: results of the German Consortium for Hereditary Breast and Ovarian Cancer. Cancer Med. 2018;7(4):1349–58.
Nykamp K, Anderson M, Powers M, Garcia J, Herrera B, Ho Y-Y, et al. Sherloc: a comprehensive refinement of the ACMG–AMP variant classification criteria. Genet Med. 2017;19(10):1105–17.
Giacomelli AO, Yang X, Lintner RE, McFarland JM, Duby M, Kim J, et al. Mutational processes shape the landscape of TP53 mutations in human cancer. Nat Genet. 2018;50(10):1381–7.
Kotler E, Shani O, Goldfeld G, Lotan-Pompan M, Tarcic O, Gershoni A, et al. A systematic p53 mutation library links differential functional impact to cancer mutation pattern and evolutionary conservation. Mol Cell. 2018;71(1):178-90.e8.
Barone G, Groom A, Reiman A, Srinivasan V, Byrd PJ, Taylor AMR. Modeling ATM mutant proteins from missense changes confirms retained kinase activity. Hum Mutat. 2009;30(8):1222–30.
Goldgar DE, Healey S, Dowty JG, Da Silva L, Chen X, Spurdle AB, et al. Rare variants in the ATMgene and risk of breast cancer. Breast Cancer Res. 2011;13(4):1–9.
Stredrick DL, Garcia-Closas M, Pineda MA, Bhatti P, Alexander BH, Doody MM, et al. The ATM missense mutation p. Ser49Cys (c. 146C> G) and the risk of breast cancer. Hum Mutat. 2006;27(6):538–44.
Ayari-Jeridi H, Moran K, Chebbi A, Bouguila H, Abbes I, Charradi K, et al. Mutation spectrum of RB1 gene in unilateral retinoblastoma cases from Tunisia and correlations with clinical features. PLoS ONE. 2015;10(1): e0116615.
Dommering CJ, Mol BM, Moll AC, Burton M, Cloos J, Dorsman JC, et al. RB1 mutation spectrum in a comprehensive nationwide cohort of retinoblastoma patients. J Med Genet. 2014;51(6):366–74.
Dyson NJ. RB1: a prototype tumor suppressor and an enigma. Genes Dev. 2016;30(13):1492–502.
Bièche I, Lidereau R. Loss of heterozygosity at 13q14 correlates with RB1 gene underexpression in human breast cancer. Mol Carcinog: Published in cooperation with the University of Texas MD Anderson Cancer Center. 2000;29(3):151–8.
Cancer Genome Atlas N. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490(7418):61–70.
Lee SE, Lee HS, Kim K-Y, Park J-H, Roh H, Park HY, et al. High prevalence of the MLH1 V384D germline mutation in patients with HER2-positive luminal B breast cancer. Sci Rep. 2019;9(1):1–10.
Plotz G, Welsch C, Giron-Monzon L, Friedhoff P, Albrecht M, Piiper A, et al. Mutations in the MutSα interaction interface of MLH1 can abolish DNA mismatch repair. Nucleic Acids Res. 2006;34(22):6574–86.
Mackay H, Cameron D, Rahilly M, Mackean M, Paul J, Kaye S, et al. Reduced MLH1 expression in breast tumors after primary chemotherapy predicts disease-free survival. J Clin Oncol. 2000;18(1):87.
Bhateja P, Cherian M, Majumder S, Ramaswamy B. The Hedgehog signaling pathway: a viable target in breast cancer? Cancers. 2019;11(8):1126.
Jeng K-S, Sheen I-S, Leu C-M, Tseng P-H, Chang C-F. The role of smoothened in cancer. Int J Mol Sci. 2020;21(18):6863.
Jin X, Zhu L, Cui Z, Tang J, Xie M, Ren G. Elevated expression of GNAS promotes breast cancer cell proliferation and migration via the PI3K/AKT/Snail1/E-cadherin axis. Clin Transl Oncol. 2019;21:1207–19.
Dorling L, Carvalho S, Allen J, Gonzalez-Neira A, Luccarini C, Wahlström C, et al. Breast cancer risk genes-association analysis in more than 113,000 women. N Engl J Med. 2021;384(5):428–39.
Takahashi M, Tonoki H, Tada M, Kashiwazaki H, Furuuchi K, Hamada J, et al. Distinct prognostic values of p53 mutations and loss of estrogen receptor and their cumulative effect in primary breast cancers. Int J Cancer. 2000;89(1):92–9.
Purshouse K, Schuh A, Fairfax BP, Knight S, Antoniou P, Dreau H, et al. Whole-genome sequencing identifies homozygous BRCA2 deletion guiding treatment in dedifferentiated prostate cancer. Mol Case Stud. 2017;3(3): a001362.
Acknowledgements
The authors acknowledge Cancer Genetics Unit at the Clinical Pathology Department, Faculty of Medicine, Alexandria University, Egypt, established by Science Technology and Innovation Funding Authority (STDF) (Grant No. 22832) for instruments facilities and providing some reagents. The authors also acknowledge associated professor Rania Gaber for her role in the pathological assessment of FFPE samples. The authors would like to thank all participants in this study.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
NHZ, DH, MHS, NH, AE, and ET participated in the study design. AE and NH were responsible for the recruitment of the study subjects, and the collection of clinical information. NHZ, DH, MHS, ET, and AE were responsible for the genetic and data analysis using Ion S5™ next-generation sequencing system. AE drafted the manuscript. NHZ, DH, MHS, NH, AE, and ET reviewed and edited the manuscript. All the authors read and approved the final form of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Alexandria University, Egypt. Informed consent was obtained from all individual participants included in the study. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest that are directly relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zakaria, N.H., Hashad, D., Saied, M.H. et al. Genetic mutations in HER2-positive breast cancer: possible association with response to trastuzumab therapy. Hum Genomics 17, 43 (2023). https://doi.org/10.1186/s40246-023-00493-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40246-023-00493-5