Abstract
Objectives
The objective of this systematic review and meta-analysis was to evaluate the effect of chewing gum on orthodontic pain and to determine the rate of bracket breakage associated with fixed orthodontic appliances.
Methods
This review and its reporting were performed according to the Cochrane Handbook for Systematic Reviews of Interventions and the PRISMA guidelines. Six electronic databases were searched up to March 16, 2023, to identify relevant studies that met the inclusion and exclusion criteria. Furthermore, grey literature resources were searched. The Cochrane Collaboration Risk of Bias tool 2 was used to assess the quality of the included studies. Meta-analysis was conducted using RevMan, and sensitivity analysis and publication bias analysis were performed using STATA software. GRADE tool was used to evaluate the certainty of evidence.
Results
Fifteen studies with 2116 participants were ultimately included in this review, and 14 studies were included in the meta-analysis. Compared with the blank group, chewing gum had a significant pain relieving effect at all times after fixation of the initial archwire (P ≤ 0.05). No significant difference was found between the chewing gum group and the analgesics group at any timepoints (P > 0.05). Only four studies evaluated the rate of bracket breakage and revealed that chewing gum did not increase the rate of bracket breakage. The sensitivity analysis showed that there was no significant difference in the pooled outcomes after the included studies were removed one at times, and Egger analysis revealed no significant publication bias in included studies (P > 0.05).
Conclusions
Chewing gum is a non-invasive, low-cost and convenient method that has a significant effect on relieving orthodontic pain and has no effect on the rate of bracket breakage. Therefore, chewing gum can be recommended as a suitable substitute for analgesics to reduce orthodontic pain.
Similar content being viewed by others
Introduction
Orthodontic treatment guides tooth movement and bone remodeling to align dentition, coordinate jawbone, improve occlusal function, and enhance facial beauty by applying force through orthodontic devices. In recent years, the demand for orthodontic treatment has increased dramatically. However, orthodontic appliances and their generated orthodontic force often cause pain, anxiety and irritability, thereby having a negative impact on oral hygiene and patients’ daily lives [1]. Pain has become the main negative complication during orthodontic treatment, especially fixed orthodontic treatment [2]. Approximately 90–95% of patients report some level of discomfort or pain after applying fixed appliances, and they also feel pain after monthly return visits during long-term treatment [3]. Pain not only leads to low patient satisfaction and low compliance with orthodontic treatment, but also causes a large proportion of patients to discontinue or resist orthodontic treatment. Therefore, alleviating orthodontic pain is an urgent problem for orthodontists and patients.
Many pharmacological and nonpharmacological methods have been proposed to relieve orthodontic pain. Analgesics, mainly nonsteroidal anti-inflammatory drugs (NSAIDs), have obvious effects on reducing orthodontic pain [4]. However, analgesics have some side effects, such as gastric ulcers, gastric bleeding, thrombocytopenia, renal insufficiency, hepatotoxicity, atherosclerosis and hypertension [5, 6]. Moreover, some NSAIDs may hinder orthodontic tooth movement, which is detrimental to orthodontic treatment [7]. Therefore, most orthodontists do not prescribe analgesics to relieve orthodontic pain in clinical practice.
Nonpharmacological methods, such as low-level laser therapy (LLLT) [8,9,10], transcutaneous electrical nerve stimulation (TENS) [11, 12], low-intensity pulsed ultrasound (LIPUS) [13] and vibrating stimulation [14], plastic wafers [15, 16] and chewing gum [17], have emerged as approaches for relieving pain among patients treated with orthodontic appliances [18]. Among these nonpharmacological methods, chewing gum is a non-invasive, effective, convenient and inexpensive way to relieve orthodontic pain [19,20,21,22]. Many studies have confirmed that chewing gum has the same effect as analgesics for pain relief after fixing the initial arch wire [23,24,25,26,27]. In addition, M. Waheed-Ul-Hamid et al. found that chewing gum has a better pain relief effect than analgesics [28]. However, many reports have suggested that chewing gum has no clinically significant effect on orthodontic pain [29,30,31]. In addition, many orthodontists believe that chewing gum does not relieve orthodontic pain and does increase the rate of bracket breakages [32]. Therefore, it is still unclear whether chewing gum can relieve orthodontic pain and increase the rate of bracket loss; this lack of clarity is not conducive to the widespread use and promotion of chewing gum for orthodontic pain relief.
Former systematic reviews and meta-analyses have been conducted on the same topic with a very low quality of evidence: Jabr et al.'s study only included limited early phase studies and only evaluated pain value between chewing gum and conventional analgesic drugs [33]; Mando et al.'s study only evaluated pain score at its peak intensity [34]; these two studies assessed the risk of bias of these included studies according to the Cochrane Collaboration Risk of Bias tool 1 (RoB 1), and both studies included the experiments, where patients were treated with separators only, which may cause clinical heterogeneity, because various orthodontic appliances may lead to different force magnitudes and tissue response, thereby causing varying degrees of self-reported orthodontic pain. In addition, the previous studies did not include all relevant studies. Therefore, it is necessary to conduct a more scientific and accurate systematic review and meta-analysis.
Therefore, this review aimed to evaluate the effect of chewing gum on orthodontic pain and the rate of bracket breakage in patients who are planning to be treated with fixed orthodontic appliances. The finding can provide evidence-based recommendations for the clinical application and promotion of chewing gum to relieve orthodontic pain.
Methods
This review was conducted in accordance with the Cochrane Handbook for Systematic Reviews of Interventions [35] and reported in line with the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) [36]. In addition, the protocol of the present systematic review was registered in PROSPERO (#CRD42022360679).
Search strategy
The Medline (via PubMed), Science Direct, Cochrane Library, Web of Science, WangFang and ZhiWang databases were searched until March 16th, 2023, to identify relevant articles. There were no publication language restrictions. In addition, the reference lists of relevant studies, including previously published reviews, were screened for additional studies. Unpublished articles were found by searching ClinicalTrials.gov and National Research Register. Grey literature resources were also searched using Open Grey, Google Scholar, and PROQUEST Thesis and Dissertations. The main search terms include “chewing gum”, “orthodontic” and “pain”. Two authors (Mingli Xiang and Qiushuang Guo), respectively, searched and selected the included studies according to the PRISMA method. We first excluded the studies by reviewing the titles and abstracts, and then, we selected the included studies by evaluating the full texts according to the eligibility criteria. Any differences between the authors were resolved through discussion with the third author (Xiaoyan Guan). Final decisions were taken after consensus had been reached.
Eligibility criteria
The eligibility criteria were defined according to PICOS criteria (patient; intervention; comparison; outcome; study design).
Patient: participants were treated with fixed orthodontic appliances.
Intervention: chewing gum after fixation of the initial archwire.
Comparison: blank group: no intervention or taking placebo after initial archwire fixation; Analgesics group: taking analgesics after fixation of the initial archwire.
Outcome: primary outcome, pain score assessed by visual–analogue scale (VAS) or numeric rating scale (NRS); Secondary outcome: rate of bracket breakage.
Study design: randomized controlled trials (RCTs).
Data collection
Study characteristics data were extracted: (1) author's name and publication year, (2) setting, (3) participants' characteristics, (4) bracket and archwire, (5) groups, (6) outcomes and (7) conclusion. orthodontic pain usually begins at 2 h after initial archwire placement, peaks at 24 h, and lasts for 7 days [37]. Therefore, this study evaluated patients' pain scores (mean and standard deviation) at 2 h, 6 h, 12 h, 24 h, 2 d, 3 d and 7 d after initial archwire fixation. Pain scores can be quantified using the VAS scale (10 cm or 100 mm) and the Numeric Rating Scale (10 cm). To standardize the pain scales to a single scale, we assumed that 10 cm VAS and 10 cm NRS were equivalent, and these scales were converted to 100 mm VAS by multiplying the pain scores by 10 [38]. If orthodontic pain was recorded in different occlusal states (e.g., resting, biting, etc.) in one study, we combined these pain values to obtain a single estimate according to previous studies [39, 40]. The rate of bracket breakage can also be evaluated and synthetized if there is sufficient data in these included studies. When these data were reported only graphically, it could also be extracted using the Windows-based digitizing computer program UnGraph (version 5.0; Biosoft, Cambridge, United Kingdom) [41]. If these data are not available directly from the articles, they can be calculated [42, 43] and obtained by contacting the corresponding author for the numerical data.
Quality assessment
Two authors (Mingli Xiang and Qiushuang Guo) independently assessed the Risk of Bias of these included studies according to the Cochrane risk-of-bias tool for randomized trials (RoB 2) [44]. This includes the following domains: (D1) randomization process, (D2) deviations from intended interventions, (D3) missing outcome data, (D4) measurement of the outcome, and (D5) selection of the reported result. The studies were rated as having a low risk of bias, some concerns of bias, or high risk of bias for each. When a single study reported multiple outcomes of interest, the overall risk of bias was assessed rather than the risk of bias for each outcome.
The strength of the body of evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool [45]. This tool evaluates the quality of evidence in the following domains: study design, risk of bias, inconsistency, indirectness and imprecision.
Statistical analysis
The primary outcome was patient-reported pain scores at 2 h, 6 h, 12 h, 24 h, 2 d, 3 d or 7 d after initial archwire fixation. The mean differences and standard error were combined using RevMan 5.1 (Cochrane Collaboration, Copenhagen, Denmark) [46]. Data were considered suitable for pooling if the retrieved studies met to the selected criteria. The statistical significance of the hypothesis test was set at P < 0.05 (two-tailed z tests). We chose a random effects model to estimate all pooled data considering the inherent differences in these studies. Heterogeneity was assessed using the I2 index. I2 index ≥ 50% indicates moderate heterogeneity and I2 index ≥ 75% indicates high heterogeneity. If high heterogeneity existed, sensitivity analyses were performed using the ‘metaninf’ command in Stata 17.0 (StataCorp, College Station, TX) [47] to evaluate the effect of individual studies on the overall mean difference. The Egger’s rank correlation test was conducted to detect publication bias if the number of included studies exceeded 8.
Results
Searching and selection results
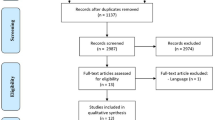
A total of 640 studies were identified from the search strategy, 3 of which were derived from the reference lists of relevant studies and 1 from ClinicalTrials.gov. After removing duplicates, 464 remained; after screening the title and abstract, 377 were excluded; and 87 were excluded after evaluating the full text according to the eligibility criteria. Finally, 15 studies [19,20,21,22,23,24,25,26,27,28,29,30,31, 48, 49] were included in qualitative synthesis, and 14 studies [19,20,21,22,23,24,25,26,27,28,29,30,31, 49] were included in meta-analysis. The PRISMA flow diagram is shown in Fig. 1.
Characteristics of the included studies
The characteristics of the included studies are summarized in Table 1. All included studies were RCTs, and 2116 patients were included. Patients received fixed orthodontic appliances with the initial aligning archwire only and without other auxiliary orthodontic devices, such as transpalatal arch, headgear, mini-screw, etc. These patients were excluded when they had some conditions affecting their pain scores, such as oral ulcers, oral diseases, taking analgesics recently, etc. In addition, tooth extraction for orthodontic treatment was conducted at least 2 weeks before the experiment [22, 24, 26, 28]. Six studies [19, 21, 29,30,31, 49] evaluated the effect of chewing gum on pain control compared to the blank group, five studies [23, 26,27,28, 48] analysed pain scores comparing the chewing gum group with analgesics, and four studies [20, 22, 24, 25] assessed the pain value in the chewing gum group, analgesics group, and blank group. Patients in eight studies [19, 21,22,23,24, 26, 31, 48] received fixed orthodontic treatment on bimaxillary arch, patients in five studies [20, 27,28,29,30] received only one arch, and two studies [25, 49] did not specify two or one arch. The aligning archwire included 0.012" NT [19, 21], 0.014" NT [20, 22, 29,30,31, 49] and 0.016" NT [23, 24, 26, 28], and the archwire size was unclear in 3 studies [25, 27, 48]. Fourteen studies quantified pain values using the VAS scale, and one study applied the NRS scale [22]. Two studies [20, 27] recorded pain scores when resting and biting, one study [48] recorded pain scores when biting and chewing, one study [26] recorded pain scores when fitting posterior teeth, biting and chewing, two studies [22, 24] recorded pain scores when chewing, biting, fitting anterior teeth and fitting posterior teeth, and other studies did not specify the occlusal state when pain was recorded. Only four studies evaluated the rate of appliance breakage [23, 27, 48, 49] and found that chewing gum did not increase the rate of bracket breakage when compared to the control group or analgesics group.
Risk of bias assessment
Figure 2 illustrate the results of the risk of bias. According to the quality of the evidence, nine RCTs were low risk, three RCTs were high risk, and other RCTs was unclear risk. The higher risk was caused by the higher dropout due to some patients do not feel pain or taken analgesics.
Data synthesis
Ten studies evaluated pain scores after initial archwire placement in the chewing gum group and blank group [19,20,21,22, 24, 25, 29,30,31, 49]. As shown in Fig. 3, chewing gum showed a significant effect on pain relief for orthodontic patients compared to blank group at 2 h (MD = − 6.24, 95% CI − 8.88 to − 3.59, P < 0.00001, I2 = 0%), 6 h (MD = − 13.97, 95% CI − 18.39 to − 9.56, P < 0.00001, I2 = 0%), 12 h (MD = − 16.53, 95% CI − 22.61 to − 10.46, P < 0.00001, I2 = 38%), 24 h (MD = − 13.99, 95% CI − 19.20 to − 8.79, P < 0.00001, I2 = 53%), 2 days (MD = − 10.98, 95% CI − 15.81 to − 6.16, P < 0.00001, I2 = 51%), 3 days (MD = − 7.97, 95% CI − 12.49 to − 3.46, P = 0.0005, I2 = 50%) and 7 days (MD = − 3.97, 95% CI − 7.99 – 0.06, P = 0.05, I2 = 73%). Eight studies analysed orthodontic pain between the chewing gum group and the analgesics group [20, 22,23,24,25,26,27,28]. As shown in Fig. 4, no significant difference was found between the chewing gum group and the analgesics group at 2 h (MD = 1.66, 95% CI − 2.61–5.93, P = 0.45, I2 = 25%), 6 h (MD = 1.62, 95% CI − 3.20 – 6.44, P = 0.51, I2 = 0%),12 h (MD = 1.26, 95% CI − 6.82 – 9.35, P = 0.76, I2 = 79%), 24 h (MD = − 2.95, 95% CI − 8.73 − 2.82, P = 0.32, I2 = 80%), 2 days (MD = 0.33, 95% CI − 8.01–8.67, P = 0.94, I2 = 88%), 3 days (MD = − 1.04, 95% CI − 5.86–3.77, P = 0.67, I2 = 74%) and 7 days (MD = − 1.99, 95% CI − 8.21– 4.22, P = 0.53, I2 = 97%).
Risk of bias across studies and additional analyses
Pain is a subjective value, and clinical and demographic diversity existed across studies regarding participants' characteristics. Therefore, we chose the random effects model to estimate all pooled data. However, low heterogeneity was found at 2, 6, and 12 h, and moderate or severe heterogeneity at 24 h, 2 d, 3 d, and 7 d according to the I2 index when comparing the chewing gum group with the blank group (Fig. 3). The pooled results were not significantly different after excluding the included studies one by one (Fig. 5a). The Egger analysis showed no significant publication bias in included studies (P = 0.592 > 0.05). There was low heterogeneity at 2 h and 6 h, moderate heterogeneity at 3 d, and severe heterogeneity at 12 h, 24 h, 2 d, and 7 d when comparing chewing gum with analgesics (Fig. 4). The pooled results were not significant difference after removing the included studies one by one (Fig. 5b). The Egger analysis showed no significant publication bias in included studies (P = 0.489 > 0.05). The quality of the evidence across studies was evaluated according to the GRADE tool, and it was found that there was a very low quality of evidence (Table 2).
Discussion
Pain is considered the main negative aspect of orthodontic treatment, a deterrent to patient compliance, and the principal reason for discontinuation of treatment. Emerging studies have found that chewing gum, as a nonpharmacological method, has obvious effects on orthodontic pain relief [27, 28]. However, many orthodontists disagree with these views and believe that chewing gum will increase the rate of bracket loss, which is not conducive to the clinical application and promotion of chewing gum to relieve orthodontic pain. Therefore, this review is conducted to analyse the effect of chewing gum on relieving orthodontic pain compared to the blank group and analgesic group. In accordance with Mando et al.'s study [34], we found that chewing gum significantly reduced pain intensity when compared to the blank group. However, Mando and colleagues showed that chewing gum significantly reduced pain intensity compared to analgesics, which is inconsistent with our results. We found that the chewing gum had the same pain relief effect as analgesics, which was similar to Jabr et al.'s study [33]. This possibly because Mando et al.'s study included Ireland et al.'s multicenter RCTs in meta-analysis, although this study showed the differences between chewing gum and analgesic had no clinical importance in relieving orthodontic pain. In summary, we found that chewing gum significantly reduced orthodontic pain when compared to the blank group and had the equal pain relief effect when compared to analgesics. Nevertheless, chewing gum can be recommended as a suitable substitute for analgesics to reduce orthodontic pain.
Orthodontic pain is produced by metabolic activity in periodontal tissue caused by orthodontic force, including ischemia, inflammation, or edema in periodontal ligaments [50]. The mediators, such as prostaglandins, leukotrienes, histamine, substance P, bradykinin, dopamine, serotonin, glycine, glutamate gamma-aminobutyric acid, etc., released in periodontal tissue, initiate the inflammatory reaction, create the hyperalgesic response, and ultimately cause pain when orthodontic force is applied [3, 51, 52]. In addition, the pulp irritation caused by orthodontic tooth movement also induces orthodontal pain [53]. Therefore, it is believed that any factor that can temporarily displace the teeth under orthodontic force can resolve the pressure and prevent the formation of ischemic areas, thereby reducing pain.
Chewing gum has both local and central effects on pain relief [17]. Chewing gum increases blood flow into and around the periodontal membrane, loosens tightly grouped fibers around nerves and blood vessels, restores normal vascular and lymphatic circulation, and prevents or relieves inflammation in the periodontal tissue, thereby reducing pain [50]. Meanwhile, chewing gum for 20 min activated the ventral part of the prefrontal cortex and evoked augmented activity of 5-HT neurons in the dorsal raphe nucleus and, therefore, suppressed nociceptive responses [54]. Chewing gum also has pharmacological pain-relieving effects for orthodontic pain [55]. Distraction is an effective way to reduce pain, because the brain can only focus on one thing at a time. Chewing gum can transfer patients' attention to mastication, reduce the neuronal response to the harmful stimulus, and make them feel happy. Sometimes, patients can even release pain or irritability by chewing gum.
Chewing gum has great benefits in relieving pain compared to analgesics. It has the advantages of noninvasive, inexpensive and convenient, and avoids the side effects caused by analgesics. Simultaneously, chewing gum has other benefits. Chewing gum can be a simple and effective way to reduce stress and tension, and it can enhance α brain wave, which is a sign that the spirit is in a calm state. Chewing gum is beneficial to improve digestive function by stimulating saliva secretion to promote swallowing and digestive activity. Chewing gum is also beneficial for oral cleaning and reduces the occurrence of demineralization and caries by increasing the saliva flow rate and PH value [56,57,58]. In addition, gum can be used as a carrier for drugs or active molecules to improve its function. For example, chewing gum containing sodium metaphosphate can effectively remove coffee stains [59], chewing gum containing potassium chloride can reduce dental hypersensitivity for a long time [60], and chewing gum containing analgesics can enhance its pain relief effect [61].
In addition, bracket breakage is one of the factors affecting patient satisfaction, and many doctors believe that chewing gum will cause bracket breakage, which will not only increase the time of operation beside the chair but also prolong the treatment cycle. Four studies evaluated the effect of chewing gum on the rate of appliance breakage and found that chewing gum did not increase the rate of bracket breakage when compared to the blank group or analgesics group [23, 27, 48, 49]. Moreover, chewing gum will not increase the rate of bracket breakages but will be beneficial to oral health and dental caries [56].
There was moderate or severe heterogeneity in some pooled results according to the I2, which were caused by clinical heterogeneity, methodological heterogeneity and statistical heterogeneity in this meta-analysis. Although all studies are well-designed RCTs, it is inevitable that there are some differences in participants characteristics, malocclusion, types of fixed appliances, treatment plan, clinical operation, etc. In addition, pain is a subjective feeling that is affected by many factors, such as age, gender, pain threshold, cultural differences, etc. Therefore, we applied the random effect model and performed sensitivity analysis. The sensitivity analysis showed no significant difference for the pooled results after excluding the included studies one by one.
Although this meta-analysis was conducted carefully, there were still some limitations. Orthodontic pain is a subjective feeling that is influenced by psychological, physiological, social and other factors, such as the patient's age [62], gender [63], type of orthodontic appliances [64, 65], magnitude of orthodontic force [66], treatment motivation [66], expectations of orthodontic treatment outcomes [67], emotional state [68] and personality traits [69]. Similarly, patient characteristics, including the crowding degree of dentition, whether tooth extraction or not, single or two dental arches, and the size of the initial arch wire, will affect the patient's pain intensity. Although each study noted that they included similar participants, the baseline characteristics of participants in each study were not always the same. In addition, the level of certainty of the meta-analysis results was assessed as very low level of certainty according GRADE tool. Therefore, more well-designed RCT studies with large samples are needed to obtain more reliable conclusions in the future.
Conclusions
This review has demonstrated that chewing gum has a significant effect on relieving orthodontic pain and can be recommended as a safe, low-cost and convenient alternative to analgesics with no side effects to reduce orthodontic pain during fixed orthodontic appliances in daily orthodontic practice.
Availability of data and materials
The data sets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis
- RCT:
-
Randomized clinical trial
- VAS:
-
Visual–analog scale
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- LLLT:
-
Low-level laser therapy
- TENS:
-
Transcutaneous electrical nerve stimulation
- LIPUS:
-
Low-intensity pulsed ultrasound
- NRS:
-
Numeric Rating Scale
References
Banerjee S, Banerjee R, Shenoy U, Agarkar S, Bhattacharya S. Effect of orthodontic pain on quality of life of patients undergoing orthodontic treatment. Indian J Dent Res. 2018;29(1):4–9.
Simmons KE, Brandt M. Control of orthodontic pain. J Indiana Dent Assoc. 1992;71(4):8–10.
Scheurer PA, Firestone AR, Bürgin WB. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1996;18(4):349–57.
Monk AB, Harrison JE, Worthington HV, Teague A. Pharmacological interventions for pain relief during orthodontic treatment. Cochrane Database Syst Rev. 2017;11(11):Cd003976.
Miettinen OS. Side effects of non-narcotic analgesics as a determinant of prescribing. Drugs. 1986;32(Suppl 4):206–8.
Del Vecchio G, Spahn V, Stein C. Novel opioid analgesics and side effects. ACS Chem Neurosci. 2017;8(8):1638–40.
Bartzela T, Türp JC, Motschall E, Maltha JC. Medication effects on the rate of orthodontic tooth movement: a systematic literature review. Am J Orthod Dentofacial Orthop. 2009;135(1):16–26.
Farzan A, Khaleghi K, Pirayesh Z. Effect of low-level laser therapy on bone formation in rapid palatal expansion: a systematic review. J Lasers Med Sci. 2022;13: e13.
Brito MH, Nogueira CQ, Cotrin P, Fialho T, Oliveira RC, Oliveira RG, et al. Efficacy of low-level laser therapy in reducing pain in the initial stages of orthodontic treatment. Int J Dent. 2022;2022:3934900.
Al-Jewair T, Farsaii A. Low-level laser therapy may reduce pain associated with orthodontic separator placement. J Evid Based Dent Pract. 2022;22(3): 101752.
Zhang Y, Zhang J, Wang L, Wang K, Svensson P. Effect of transcutaneous electrical nerve stimulation on jaw movement-evoked pain in patients with TMJ disc displacement without reduction and healthy controls. Acta Odontol Scand. 2020;78(4):309–20.
Cacho A, Tordera C, Colmenero C. Use of transcutaneous electrical nerve stimulation (TENS) for the recovery of oral function after orthognathic surgery. J Clin Med. 2022;11(12):3268.
Badiee M, Tehranchi A, Behnia P, Khatibzadeh K. Efficacy of low-intensity pulsed ultrasound for orthodontic pain control: a randomized clinical trial. Front Dent. 2021;18:38.
Lobre WD, Callegari BJ, Gardner G, Marsh CM, Bush AC, Dunn WJ. Pain control in orthodontics using a micropulse vibration device: a randomized clinical trial. Angle Orthod. 2016;86(4):625–30.
Murdock S, Phillips C, Khondker Z, Hershey HG. Treatment of pain after initial archwire placement: a noninferiority randomized clinical trial comparing over-the-counter analgesics and bite-wafer use. Am J Orthod Dentofacial Orthop. 2010;137(3):316–23.
Bayani S, Rostami S, Ahrari F, Saeedipouya I. A randomized clinical trial comparing the efficacy of bite wafer and low level laser therapy in reducing pain following initial arch wire placement. Laser Ther. 2016;25(2):121–9.
Proffit WRFH, Sarver DM. Contemporary orthodontics. St Louis: Mosby Elsevier; 2007.
Fleming PS, Strydom H, Katsaros C, Curatolo MDLCI, Fudalej MP, et al. Non-pharmacological interventions for alleviating pain during orthodontic treatment. Cochrane Database Syst Rev. 2016;12(12):010263.
Yang ZJY, Huang L, Xiao Y, Yuan X, Xu X. Preliminary study of chewing gum on relieving the initial orthodontic pain. J Luzhou Med College. 2013;36(3):248–50.
Santos D Jr. Chewing gum as a non-pharmacological alternative for orthodontic pain relief: a randomized clinical trial using an intention-to-treat analysis. Korean J Orthod. 2021;51(5):346–54.
Liu YFQ-XJI, Zhao Z. Fixed appliance influencing factors in patients with periodontal pain and psychological intervention effect on periodontal pain. Gen J Stomatol. 2015;2(10):66–7.
Delavarian M, Imani MM, Delavarian F, Bayani S. Comparison of chewing gum and ibuprofen in alleviating orthodontic pain: a single centre, randomised clinical trial. Australas Orthod J. 2020;36(1):38–44.
Shayea EA. Comparative assessment between Ibuprofen, chewing gum, and bite wafers in pain control following first archwire placement in orthodontic patients. J Contemp Dent Pract. 2020;21(4):416–20.
Farzanegan F, Zebarjad SM, Alizadeh S, Ahrari F. Pain reduction after initial archwire placement in orthodontic patients: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2012;141(2):169–73.
Elvina Elvina JK, Halim H, Roeslan BO. Chewing gum, acetaminophen, and green tea effect in reducing pain after orthodontic appliance placement. Sci Dental J. 2018;2(2):51–7.
Basam LC, Singaraju GS, Obili S, Keerthipati T, Basam RC, Prasad M. Orthodontic pain control following arch wire placement; a comparison between pre-emptive tenoxicam and chewing gum: a randomized clinical trial. J Dent Anesth Pain Med. 2022;22(2):107–16.
Alshammari AK, Huggare J. Pain relief after orthodontic archwire installation-a comparison between intervention with paracetamol and chewing gum: a randomized controlled trial. Eur J Orthod. 2019;41(5):478–85.
Waheed-Ul-Hamid MAH, Mahmood HS, Azeem M, Irfan S. Comparison between Ibuprofen and chewing gum for orthodontic pain control. Pakistan Oral Dental J. 2016;36(1):9–83.
Celebi F, Bicakci AA, Kelesoglu U. Effectiveness of low-level laser therapy and chewing gum in reducing orthodontic pain: a randomized controlled trial. Korean J Orthod. 2021;51(5):313–20.
Çelebi F. Mechanical vibration and chewing gum methods in orthodontic pain relief. Turk J Orthod. 2022;35(2):133–8.
Alqareer A, Alyahya A, Al-Anezi SA, AlAwadhi A, Al Qabandi S, Alyaseen M. Efficacy of chewing gum to reduce orthodontic pain compared to Placebo: a blinded, parallel-group, preliminary clinical trial. J Oral Facial Pain Headache. 2019;33(3):301–7.
Ferney P, Clauss F, Offner D, Wagner D. Preventive and therapeutic advantages of sugar-free chewing gums in orthodontics. A study conducted on practitioners and patients. Orthod Fr. 2017;88(3):275–81.
Jabr L, Altuhafy M, Barmak AB, Rossouw PE, Michelogiannakis D. Sugar-free chewing gum versus conventional analgesic drugs for pain relief with fixed orthodontic appliances. A systematic review and meta-analysis. J Orthod. 2023;50(2):215–28.
Mando M, Talaat S, Bourauel C. The efficacy of chewing gum in the reduction of orthodontic pain at its peak intensity: a systematic review and meta-analysis. Angle Orthod. 2023;93(5):580–90.
Higgins JPT SJ, Page MJ, Elbers RG, Sterne JAC. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane. 2023.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
Krishnan V. Orthodontic pain: from causes to management–a review. Eur J Orthod. 2007;29(2):170–9.
Mbizvo GK, Nolan SJ, Nurmikko TJ, Goebel A. Placebo responses in long-standing complex regional pain syndrome: a systematic review and meta-analysis. J Pain. 2015;16(2):99–115.
Sandhu SS, Piepho HP, Khehra HS. Comparing the effectiveness profile of pharmacological interventions used for orthodontic pain relief: an arm-based multilevel network meta-analysis of longitudinal data. Eur J Orthod. 2017;39(6):601–14.
Sandhu SS, Cheema MS, Khehra HS. Comparative effectiveness of pharmacologic and nonpharmacologic interventions for orthodontic pain relief at peak pain intensity: a Bayesian network meta-analysis. Am J Orthod Dentofacial Orthop. 2016;150(1):13–32.
Shadish WR, Brasil ICC, Illingworth DA, White KD, Galindo R, Nagler ED, et al. Using UnGraph to extract data from image files: verification of reliability and validity. Behav Res Methods. 2009;41(1):177–83.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
McGrath S, Zhao X, Steele R, Thombs BD, Benedetti A. Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis. Stat Methods Med Res. 2020;29(9):2520–37.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Zhou L, Chen Y, Yuan X, Zeng L, Zhu J, Zheng J. Preoperative pelvic floor muscle exercise for continence after radical prostatectomy: a systematic review and meta-analysis. Front Public Health. 2023;11:1186067.
Zhang C, Guo J, Yin H, Yin C, Peng Y. Traditional Chinese medicine for neonatal hypoxic-ischemic encephalopathy: a Bayesian network meta-analysis. J Ethnopharmacol. 2023;11:117317.
Ireland AJ, Ellis P, Jordan A, Bradley R, Ewings P, Atack NE, et al. Comparative assessment of chewing gum and ibuprofen in the management of orthodontic pain with fixed appliances: a pragmatic multicenter randomized controlled trial. Am J Orthod Dentofacial Orthop. 2016;150(2):220–7.
Benson PE, Razi RM, Al-Bloushi RJ. The effect of chewing gum on the impact, pain and breakages associated with fixed orthodontic appliances: a randomized clinical trial. Orthod Craniofac Res. 2012;15(3):178–87.
Long H, Wang Y, Jian F, Liao LN, Yang X, Lai WL. Current advances in orthodontic pain. Int J Oral Sci. 2016;8(2):67–75.
Tang Z, Zhou J, Long H, Gao Y, Wang Q, Li X, et al. Molecular mechanism in trigeminal nerve and treatment methods related to orthodontic pain. J Oral Rehabil. 2022;49(2):125–37.
Sergl HG, Klages U, Zentner A. Pain and discomfort during orthodontic treatment: causative factors and effects on compliance. Am J Orthod Dentofacial Orthop. 1998;114(6):684–91.
Cave SG, Freer TJ, Podlich HM. Pulp-test responses in orthodontic patients. Aust Orthod J. 2002;18(1):27–34.
Kamiya K, Fumoto M, Kikuchi H, Sekiyama T, Mohri-Lkuzawa Y, Umino M, et al. Prolonged gum chewing evokes activation of the ventral part of prefrontal cortex and suppression of nociceptive responses: involvement of the serotonergic system. J Med Dent Sci. 2010;57(1):35–43.
Sekine N, Okada-Ogawa A, Asano S, Takanezawa D, Nishihara C, Tanabe N, et al. Analgesic effect of gum chewing in patients with burning mouth syndrome. J Oral Sci. 2020;62(4):387–92.
Newton JT, Awojobi O, Nasseripour M, Warburton F, Di Giorgio S, Gallagher JE, et al. A systematic review and meta-analysis of the role of sugar-free chewing gum in dental caries. JDR Clin Trans Res. 2020;5(3):214–23.
Nasseripour M, Newton JT, Warburton F, Awojobi O, Di Giorgio S, Gallagher JE, et al. A systematic review and meta-analysis of the role of sugar-free chewing gum on plaque quantity in the oral cavity. Front Oral Health. 2022;3: 845921.
Miller CS, Danaher RJ, Kirakodu S, Carlson CR, Mumper RJ. Effect of chewing gum containing Xylitol and blackberry powder on oral bacteria: a randomized controlled crossover trial. Arch Oral Biol. 2022;143: 105523.
Makino S, Kawamoto C, Ikeda T, Doi T, Narise A, Tanaka T, et al. Whitening efficacy of chewing gum containing sodium metaphosphate on coffee stain: Placebo-controlled, double-blind In Situ examination. Oper Dent. 2019;44(5):469–75.
Krahwinkel T, Theiss P, Willershausen B. Clinical effectiveness of a potassium chloride containing chewing gum in the treatment of hypersensitive teeth. Eur J Med Res. 2001;6(11):483–7.
Al-Melh MA, Nada A, Badr H, Andersson L. Effect of an anesthetic chewing gum on the initial pain or discomfort from orthodontic elastomeric separator placement. J Contemp Dent Pract. 2019;20(11):1286–92.
Campos MJ, Fraga MR, Raposo NR, Ferreira AP, Vitral RW. Assessment of pain experience in adults and children after bracket bonding and initial archwire insertion. Dental Press J Orthod. 2013;18(5):32–7.
Bergius M, Berggren U, Kiliaridis S. Experience of pain during an orthodontic procedure. Eur J Oral Sci. 2002;110(2):92–8.
Čelar A, Schedlberger M, Dörfler P, Bertl M. Systematic review on self-ligating vs. conventional brackets: initial pain, number of visits, treatment time. J Orofac Orthop. 2013;74(1):40–51.
Cardoso PC, Espinosa DG, Mecenas P, Flores-Mir C, Normando D. Pain level between clear aligners and fixed appliances: a systematic review. Prog Orthod. 2020;21(1):3.
Campos MJ, Vitral RW. The influence of patient’s motivation on reported pain during orthodontic treatment. Dental Press J Orthod. 2013;18(3):80–5.
Supakomonnun S, Mitrirattanakul S, Chintavalakorn R, Saengfai NN. Influence of functional and esthetic expectations on orthodontic pain. J Orofac Orthop. 2023;84(3):141–6.
Firestone AR, Scheurer PA, Bürgin WB. Patients’ anticipation of pain and pain-related side effects, and their perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1999;21(4):387–96.
Abu Alhaija ES, Abu Nabaa MA, Al Maaitah EF, Al-Omairi MK. Comparison of personality traits, attitude toward orthodontic treatment, and pain perception and experience before and after orthodontic treatment. Angle Orthod. 2015;85(3):474–9.
Funding
This study was supported by the National Natural Science Foundation of China (82060205); and The Project to Cultivate Young Scientific and Technological Talents in Colleges and Universities of Guizhou Province (Qian Jiao He KY [2021] 215); Zunyi Science and technology plan project (Zun Shi Ke He HZ Zi (2022)423).
Author information
Authors and Affiliations
Contributions
Mingli Xiang and Qiushuang Guo realized the research and were the major contributor in writing the manuscript. Chengcheng Liao also realized the research and helped with the writing. Xiaoyan Guan and Linlin Xiao helped with the research and corrected the writing. Meiling Xiang and Sicen Long corrected the writing and contributed with the correct structure of this article. Jianguo Liu corrected all the steps of this systematic review and corrected the writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guo, Q., Liao, C., Guan, X. et al. Effect of chewing gum on orthodontic pain in patients receiving fixed orthodontic treatment: a systematic review and meta-analysis. Eur J Med Res 28, 491 (2023). https://doi.org/10.1186/s40001-023-01467-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01467-y