Abstract
Background
Patients who had gone through orthodontic treatment experienced pain and discomfort which could be the highest-ranking reason for treatment disturbance or early termination. Thus, this review aimed to assess the efficacy of analgesics on the relief of pain in orthodontic treatment.
Methods
A computerized literature search was conducted in the databases of EMBASE (via OVID, 1974 to 2019 Week 50), MEDLINE (via OVID, 1946 to Dec 2019), the Cochrane Central Register of Controlled Trials (CENTRAL) (December 2019). The Cochrane Collaboration’s Review Manager 5.3 software was applied in the present study. And methodological quality was evaluated by the Cochrane Risk of Bias Tool.
Results
We identified twelve publications including 587 patients in 19 randomized controlled trials. The results showed that the mean difference of naproxen in visual analogue scale (VAS) were − 1.45 (95% CI -2.72, − 0.19; P = .02), − 2.11 (95% CI -3.96, − 0.26; P = .03) and − 1.90 (95% CI -3.33, − 0.47; P = .009) in 2 h, 6 h and 24 h respectively. As for ibuprofen, the standard mean differences were − 1.10 (95% CI -1.49, − 0.71), − 1.63(95% CI -2.32, − 0.95) and − 1.34 (95% CI -2.12, − 0.55) at 2 h, 6 h, and 24 h, with the overall P values all < 0.001. The mean difference of acetaminophen is − 0.68, − 1.34, − 1.91 at three time points and the overall P values all < 0.01.
Conclusions
This meta-analysis suggests that the use of analgesics is effective for patients in controlling orthodontic pain. Ibuprofen and naproxen are both of stable analgesic effects which could peak at 6 h, while the analgesic effect of acetaminophen increases steadily from 2 h through 24 h. Compared with ibuprofen and acetaminophen, naproxen shows a stronger analgesic effect either at 2 h or 6 h, and its effect lasts to 24 h.
Similar content being viewed by others
Background
Despite all the technological advances in orthodontics, pain is inevitable and hard to bear in the process of orthodontic treatment. The existing literature suggests that all the clinical operation (initial archwire placement, separator placement and activations) can be the root cause of orthodontic pain. There is no denying the fact that fixed appliances could produce more pain compared with functional or removable appliances. A survey of patients who had ever gone through orthodontic treatment found that 91% experienced pain during treatment and 50% had difficulty in eating and were limited even in their daily life [1, 2]. Similarly, pain has been reported to be the highest-ranking reason for treatment disturbance or early termination [3, 4]. However, not enough attentions have been paid to the orthodontic pain neither in clinic or research, and there is no universal recommendation on the interventions for pain relief as well. Ways to relieve orthodontic pain have differed greatly among which nonsteroidal anti-inflammatory drugs (NSAIDs) are the most popular drugs for pain controlling. In specific, ibuprofen and paracetamol/acetaminophen are drugs commonly recommended for this purpose, whereas other methods such as low-level laser therapy, anesthetic gel, transcutaneous electrical nerve stimulation and even bite wafers, have also been mentioned in some trials. Orthodontic tooth movement leads to inflammation of the periodontal membrane and the dental pulp response, which stimulates the release of a variety of biochemical mediators bringing about pain sensation [5, 6]. NSAIDs function by blocking the synthesis of arachidonic acid in the prostaglandin production cycle reducing the formation of prostaglandins. As we all know that prostaglandin is the main mediators in the process of inflammatory reaction after the orthodontic force [7, 8]. Nevertheless, there is lack of adequate clinical evidence to assess the validity of various analgesics, let alone a standard medication protocols up to date.
The purpose of this systematic review and meta-analysis is to compare the efficacy of commonly used analgesics in orthodontic pain management and develop a recommendation on the medication for pain management.
Materials and methods
Search strategy
We searched online databases, including EMBASE (via OVID, 1974 to 2019 Week 50), MEDLINE (via OVID, 1946 to Dec 2019) and the Cochrane Central Register of Controlled Trials (CENTRAL) (December 2019). World Health Organization International Clinical Trials Registry Platform was searched for clinical trials in progress. No restrictions about language, country or date of publication. MeSH terms and free text words used for orthodontic pain were combined as follows: “orthodontics” or “orthodontic treatment” or “tooth movement”, “pain” or “discomfort”, “analgesia” or “NSAIDS” or “ibuprofen” or “acetaminophen” with every possible combination considered. Reference lists of all the studies included were checked. Efforts were made to contact all corresponding authors for more information when data were missing.
Data extractions
No restrictions were imposed to maintain more specific methodological characteristics on the search. The inclusion and exclusion criteria are listed in Table 1. Two independent investigators (C.-Q. C. and T.X.) selected studies based on titles and abstracts. The names of the journals or authors were hidden in the filter and articles accord with the criteria above were included. Disagreements regarding the inclusion were resolved by discussion to reach consensus in this review. Then full texts were evaluated in the same way by the reviewers independently. The data were collected by two authors (C.-Q. C. and T.X) through consultation on the items including first author, publication year, original country, case number, type of design, medication dose and outcomes. Attempts had been made to contact the authors of the selected trials by e-mail for relevant data that were not specified in the articles.
Risk of bias assessment
The methodological quality of studies was assessed using the Cochrane Risk of Bias 2 (RoB-2) [9]. The tool assesses five areas of potential bias including: (1) randomization process, (2) deviations from the intended interventions, (3) missing outcome data, (4) measurement of the outcome, and (5) selection of the reported result. Each domain assessed and each study overall is shown to have either a low risk of bias, some concerns relating to the risk of bias, or a high risk of bias, as determined by a validated a priori algorithm. Two reviewers independently read the articles to assess the trials more accurately.
Data synthesis and analysis
Review Manager 5.3 from The Cochrane Collaboration was implemented in this review. The DerSimonian and Laird random effects model was used to identify the VAS outcome of orthodontic pain. The estimates were represented as mean difference (MD) as well as 95% confidence interval (CI). Heterogeneity was identified using Cochran’s Q test and quantified by the I2statistic and Tau2 as measurements of inconsistent level and between-study variance [10]. Sensitivity analysis integrating RoB-2 assessment was conducted to test the stability of the results. We also conducted subgroup analysis according to orthodontic treatment pattern (separator placement or archwire placement). To explore possible publication bias, a funnel plot would be performed when the number of studies pooled was over 10.
Results
Search results
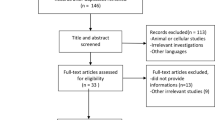
194 publications were collected after the first screening (last updated on Dec. 2019). Twenty-one studies remained for full-text screen and 12 studies were finally identified in the present review as shown in the flow chart (Fig. 1). In total, 12 eligible trials which were all randomized placebo-controlled trials comprising 587 subjects which met the inclusion criteria. The characteristics and data summary of these studies are displayed in Table 2 [11,12,13,14,15,16,17,18,19,20,21,22].
Study quality
As evaluated by the RoB-2, 5 of 12 studies showed some concerns across all domains and three studies exhibited high risks of potential bias. In specific, the randomization process domain demonstrated several high risks of bias and the measurement of the outcome were all low risks of bias. Two studies suggested high risk of bias as a result of missing outcome data, while one study showed some concerns. These issues related to studies where more than 5% of participants were lost to follow-up or had missing data, yet analyses to assess those lost to follow-up were not conducted. Deviations from the intended intervention also suggested a need for caution, with one study showing high risk and two some concerns. Risk of bias due to selection of the reported result revealed two studies as some concerns (Fig. 2).
Sensitivity analysis was performed and the results were consistent after removing trials with high risks of bias as shown in Fig. S1, S2 and S3. Additionally, the subgroup analysis of separator placement did not reduce the heterogeneity significantly but demonstrated the consistent results with the total analysis (Fig. S4, S5 and S6).
Ibuprofen vs placebo group
Nine of the twelve included studies measured the same outcome (ibuprofen vs placebo). The meta-analysis of nine studies involving 393 patients showed that ibuprofen was more effective in controlling orthodontic pain compared with placebo at different time points. The standard mean differences were − 1.10 (95% CI -1.49, − 0.71), − 1.63 (95% CI -2.32, − 0.95) and − 1.34 (95% CI -2.12, − 0.55) at 2 h, 6 h and 24 h respectively, with the overall P values all < 0.001, indicating that the results favored the ibuprofen group more than the placebo group (Fig. 3).
Acetaminophen vs placebo group
Six investigators reported the efficacy between acetaminophen and placebo including 316 patients at different time points. The standard mean differences of 2 h were − 0.68 (95% CI -1.14, − 0.22; P = .004) and the heterogeneity was acceptable (χ2 = 6.20, P = 0.18, I2 = 35%). At 6 h and 24 h, the mean differences were − 1.34 (95% CI -1.93, − 0.74; P < .0001) and − 1.91 (95% CI -2.87, − 0.95; P < .0001). The results of Patel et al. and Salmassian et al. indicated no statistical difference for pain relief at the all three time points (Fig. 4).
Naproxen vs placebo group
Four studies totally 170 patients compared naproxen with placebo, in which two studies (Kohli et al. and Polat et al.) suggested significant pain relief in naproxen group. While Patel et al. and Eslamian et al. showed no statistical difference between the naproxen and the placebo. The mean differences of three time points (2 h, 6 h, 24 h) were − 1.45 (95% CI -2.72, − 0.19; P = .02), − 2.11 (95% CI -3.96, − 0.26; P = .03) and − 1.90 (95% CI -3.33, − 0.47; P = .009) respectively (Fig. 5).
Discussion
Orthodontic treatment has widely been accepted by the public, but it is still associated with pain regardless of the technique advance in orthodontics. Moderate statistical evidence has been shown for efficacy of analgesics managing orthodontic pain in the short term. An average decrease in VAS of 15 mm was recorded, which could be significant in clinic [23, 24]. From our analysis, the use of NSAIDs had statistically significant analgesic effects for patients in controlling orthodontic pain among which naproxen shows a stronger analgesic effect either at 2 h or 6 h, and its effect lasts to 24 h compared with ibuprofen and acetaminophen. Ibuprofen and naproxen are both of stable analgesic effect which could peak at 6 h, while the analgesic effect of acetaminophen increases steadily from 2 h through 24 h. The trials of Negan et al. revealed that patients may feel painful within 4 h after the first archwire placement or separator placement. And pain peaked at 24 h and gradually disappeared in a week [25]. The use of analgesics may help patients get through the hard times after orthodontic appointments.
The present study has included larger quantities of articles than previous reviews, also the meta-analysis were more comprehensive and convictive. Of twelve included trials, nine reported using separator placement and three archwire placement. It is believed that these appliances resulted in similar pain experience, and therefore their data were synthesized in this meta-analysis. Dose assessment was important for the analysis of analgesics research, which could recommend an applicable dose and avoid unnecessary effects. Our findings showed that the mean dosage of ibuprofen (400 mg) and acetaminophen (600 mg) one hour before the treatment and six hours after the treatment are optimum. As for naproxen, it exhibits a long half-life of 50–60 h, which permits once daily dosing. The recommended dosage of naproxen is 20–30 mg once daily. We recommend a multi-center, pragmatic trial in an appropriately powered study to test the effectiveness of parameters of this order.
The concern about NSAIDs is that they may delay the rate of tooth movement [26,27,28]. Walker et al. reported that NSAIDs inhibit the cyclooxygenase pathway and therefore the production of PGE, and it was thought that NSAIDs may inhibit the osteoclastic activity necessary for tooth movement and slow the speed of tooth movement [29]. Acetaminophen is preferred on grounds that it is inactive as an anti-inflammatory agent in peripheral tissues and does not prevent prostaglandin synthesis, which means that it has no influence on the speed of tooth movement [6, 30]. In fact, the dosage applied in clinic is relatively low and the time is short. In a healthy patient, the dosage of these analgesics would be eliminated from the body before the tooth movement starts [31]. Therefore, administrations of low doses analgesics for a short period will not prevent the potential of slowing tooth movement process. Researchers also pay attention to some long-acting NSAIDs (piroxicam and tenoxicam) and cyclooxygenase-2 (COX-2) inhibitors (valdecoxib) these days. Unfortunately, we could not make meta-analysis because of the limited amount of relevant evidence. It is expected for more well work-out studies to address the efficacy of these analgesics.
Several limitations in the present study should be acknowledged. Firstly, the gender distributions between subgroups were not evenly distributed in two of twelve included studies [11, 17]. Although large numbers of studies have found no difference between the genders after orthodontic treatment [32, 33], two studies found that girls reported more pain and ulcerations than boys [2, 34]. Secondly, some studies showed a relative high heterogeneity but we did not find key covariates that was responsible for heterogeneity. We carried out sensitive analysis restricting to same orthodontic intervention in order to determine whether different orthodontic treatment was the cause. The results showed that the heterogeneity still remained although it did account for some heterogeneity, indicating that other unreported confounding factors might affect the heterogeneity. Additionally, it was reported that peak pain intensity may vary between the archwire placement and separator placement [35], the results of sensitive analysis were comparable before and after excluding 3 studies using archwire placement in the present study. Also, we have to admit that we did not pre-register this study, but our analysis was conducted in strict accordance with the systematic review process. Furthermore, a clinical medication should take all factors which affect perception of pain into consideration including the age, the level of anxiety and self-medication history so as to decrease potential risks that can lead to severe complications.
Conclusions
Based on the data available, the use of analgesics is effective for patients in controlling orthodontic pain. Ibuprofen and naproxen are both of stable analgesic effect which could peak at 6 h, while the analgesic effect of acetaminophen increases steadily from 2 h through 24 h. And naproxen shows a stronger analgesic effect either at 2 h or 6 h, and its effect lasts to 24 h compared with ibuprofen and acetaminophen. More well-designed RCTs about long-acting NSAIDs and COX-2 inhibitors will be needed to draw a comprehensive conclusion.
Availability of data and materials
The summary of data extraction in this study is available upon request to the corresponding author.
Abbreviations
- VAS:
-
visual analogue scale
- NSAIDs:
-
nonsteroidal anti-inflammatory drugs
- RoB-2:
-
the Cochrane Risk of Bias 2
- MD:
-
mean difference
- CI:
-
confidence interval
- COX-2:
-
cyclooxygenase-2
- RCT:
-
randomized controlled trial
References
Lew KK. Attitudes and perceptions of adults towards orthodontic treatment in an Asian community. Community Dent Oral Epidemiol. 1993;21(1):31–5.
Ngan P, Kess B, Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofac Orthop. 1989;96(1):47–53.
Oliver RG, Knapman YM. Attitudes to orthodontic treatment. Br J Orthod. 1985;12(4):179–88.
Xiaoting L, Yin T, Yangxi C. Interventions for pain during fixed orthodontic appliance therapy. A systematic review. Angle Orthod. 2010;80(5):925–32.
Kyrkanides S, O'Banion MK, Subtelny JD. Nonsteroidal anti-inflammatory drugs in orthodontic tooth movement: metalloproteinase activity and collagen synthesis by endothelial cells. Am J Orthod Dentofac Orthop. 2000;118(2):203–9.
Roche JJ, Cisneros GJ, Acs G. The effect of acetaminophen on tooth movement in rabbits. Angle Orthod. 1997;67(3):231–6.
Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol. 1971;231(25):232–5.
Shibazaki T, Yozgatian JH, Zeredo JL, Gonzales C, Hotokezaka H, Koga Y, Yoshida N. Effect of celecoxib on emotional stress and pain-related behaviors evoked by experimental tooth movement in the rat. Angle Orthod. 2009;79(6):1169–74.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:Ed000142.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Bernhardt MK, Southard KA, Batterson KD, Logan HL, Baker KA, Jakobsen JR. The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. Am J Orthod Dentofac Orthop. 2001;120(1):20–7.
Farzanegan F, Zebarjad SM, Alizadeh S, Ahrari F. Pain reduction after initial archwire placement in orthodontic patients: a randomized clinical trial. Am J Orthod Dentofac Orthop. 2012;141(2):169–73.
Kohli SS, Kohli VS. Effectiveness of piroxicam and ibuprofen premedication on orthodontic patients' pain experiences. Angle Orthod. 2011;81(6):1097–102.
Minor V, Marris CK, McGorray SP, Yezierski R, Fillingim R, Logan H, Wheeler TT. Effects of preoperative ibuprofen on pain after separator placement. Am J Orthod Dentofac Orthop. 2009;136(4):510–7.
Patel S, McGorray SP, Yezierski R, Fillingim R, Logan H, Wheeler TT. Effects of analgesics on orthodontic pain. Am J Orthod Dentofac Orthop. 2011;139(1):e53–8.
Polat O, Karaman AI, Durmus E. Effects of preoperative ibuprofen and naproxen sodium on orthodontic pain. Angle Orthod. 2005;75(5):791–6.
Salmassian R, Oesterle LJ, Shellhart WC, Newman SM. Comparison of the efficacy of ibuprofen and acetaminophen in controlling pain after orthodontic tooth movement. Am J Orthod Dentofac Orthop. 2009;135(4):516–21.
Sudhakar V, Vinodhini TS, Mohan AM, Srinivasan B, Rajkumar BK. The efficacy of different pre- and post-operative analgesics in the management of pain after orthodontic separator placement: a randomized clinical trial. J Pharm Bioallied Sci. 2014;6(Suppl 1):S80–4.
Gupta M, Kandula S, Laxmikanth SM, Vyavahare SS, Reddy SB, Ramachandra CS. Controlling pain during orthodontic fixed appliance therapy with non-steroidal anti-inflammatory drugs (NSAID): a randomized, double-blinded, placebo-controlled study. J Orofac Orthop. 2014;75(6):471–6.
Eslamian L, Kianipour A, Mortazavi SAR. The analgesic efficacy of 5% naproxen gel for pain associated with orthodontic separator placement: a randomized double-blind controlled trial. Anesth Pain Med. 2017;7(2):e42708.
Hosseinzadeh Nik T, Shahsavari N, Ghadirian H, Ostad SN. Acetaminophen versus liquefied ibuprofen for control of pain during separation in orthodontic patients: a randomized triple blinded clinical trial. Acta Med Iran. 2016;54(7):418–21.
Kaur H, Bansal N, Abraham R. A randomized, single-blind, placebo-controlled trial to evaluate the effectiveness of verbal behavior modification and acetaminophen on orthodontic pain. Angle Orthod. 2019;89(4):617–23.
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–58.
Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, Bellamy N, Bombardier C, Felson D, Hochberg M, van der Heijde D, et al. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis. 2005;64(1):29–33.
Ngan P, Wilson S, Shanfeld J, Amini H. The effect of ibuprofen on the level of discomfort in patients undergoing orthodontic treatment. Am J Orthod Dentofac Orthop. 1994;106(1):88–95.
White DW, Julien KC, Jacob H, Campbell PM, Buschang PH. Discomfort associated with Invisalign and traditional brackets: a randomized, prospective trial. Angle Orthod. 2017;87(6):801–8.
Sandy JR, Harris M. Prostaglandins and tooth movement. Eur J Orthod. 1984;6(3):175–82.
Mehlisch DR, Sollecito WA, Helfrick JF, Leibold DG, Markowitz R, Schow CE Jr, Shultz R, Waite DE. Multicenter clinical trial of ibuprofen and acetaminophen in the treatment of postoperative dental pain. J Am Dent Assoc. 1990;121(2):257–63.
Walker JB, Buring SM. NSAID impairment of orthodontic tooth movement. Ann Pharmacother. 2001;35(1):113–5.
Arias OR, Marquez-Orozco MC. Aspirin, acetaminophen, and ibuprofen: their effects on orthodontic tooth movement. Am J Orthod Dentofac Orthop. 2006;130(3):364–70.
Krishnan V. Orthodontic pain: from causes to management--a review. Eur J Orthod. 2007;29(2):170–9.
Jones M, Chan C. The pain and discomfort experienced during orthodontic treatment: a randomized controlled clinical trial of two initial aligning arch wires. Am J Orthod Dentofac Orthop. 1992;102(4):373–81.
Jones ML, Chan C. Pain in the early stages of orthodontic treatment. J Clin Orthod. 1992;26(5):311–3.
Erdinc AM, Dincer B. Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod. 2004;26(1):79–85.
Panda S, Verma V, Sachan A, Singh K. Perception of pain due to various orthodontic procedures. Quintessence Int. 2015;46(7):603–9.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 81771114 and No.81970967).
Author information
Authors and Affiliations
Contributions
CC and TX conducted the literature search and data extractions, CC performed the statistical analysis and draft the manuscript. JW and CC designed the study and revised the manuscript. All authors read and approved the final version of submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Figure S1.
Sensitivity analysis excluding trials at high risk of bias. Pooled estimate of VAS scores of ibuprofen vs. placebo at 2 h(A), 6 h(B) and at 24 h(C) respectively after removing studies with high risk of bias. The effect of pain relief is depicted as MD and its 95% CI. I 2 represents the amount of heterogeneity.
Additional file 2: Figure S2.
Sensitivity analysis excluding trials at high risk of bias. Pooled estimate of VAS scores of acetaminophen vs. placebo at 2 h(A), 6 h(B) and at 24 h(C) respectively after removing studies with high risk of bias. The effect of pain relief is depicted as MD and its 95% CI. I 2 represents the amount of heterogeneity.
Additional file 3: Figure S3.
Sensitivity analysis excluding trials at high risk of bias. Pooled estimate of VAS scores of naproxen vs. placebo at 2 h(A), 6 h(B) and at 24 h(C) respectively after removing studies with high risk of bias. The effect of pain relief is depicted as MD and its 95% CI. I 2 represents the amount of heterogeneity.
Additional file 4: Figure S4.
Subgroup analysis of separator placement. Pooled estimate of VAS scores of ibuprofen vs. placebo at 2 h(A), 6 h(B) and at 24 h(C) respectively in the group of separator placement. The effect of pain relief is depicted as MD and its 95% CI. I 2 represents the amount of heterogeneity.
Additional file 5: Figure S5.
Subgroup analysis of separator placement. Pooled estimate of VAS scores of acetaminophen vs. placebo at 2 h(A), 6 h(B) and at 24 h(C) respectively in the group of separator placement. The effect of pain relief is depicted as MD and its 95% CI. I 2 represents the amount of heterogeneity.
Additional file 6: Figure S6.
Subgroup analysis of separator placement. Pooled estimate of VAS scores of naproxen vs. placebo at 2 h(A), 6 h(B) and at 24 h(C) respectively in the group of separator placement. The effect of pain relief is depicted as MD and its 95% CI. I 2 represents the amount of heterogeneity.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, C., Xie, T. & Wang, J. The efficacy of analgesics in controlling orthodontic pain: a systematic review and meta-analysis. BMC Oral Health 20, 259 (2020). https://doi.org/10.1186/s12903-020-01245-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-020-01245-w