Abstract
Background
Perioperative neuro-endocrine stress response may contribute to acquired muscle weakness. Regional anaesthesia has been reported to improve the outcome of patients having total hip arthroplasty. In this study, it was hypothesized that spinal anaesthesia (SA) decreases the perioperative neuro-endocrine stress response and perioperatively acquired muscle weakness (PAMW), as compared to general anaesthesia (GA).
Methods
Fifty subjects undergoing bilateral total hip arthroplasty (THA) were randomly allocated to receive a standardized SA (n = 25) or GA (n = 25). Handgrip strength was assessed preoperatively, on the first postoperative day (primary endpoint) and on day 7 and 28. Respiratory muscle strength was measured by maximal inspiratory pressure (MIP). Stress response was assessed by measuring levels of Adrenocorticotropic hormone (ACTH), cortisol and interleukin-6 (IL-6).
Results
Handgrip strength postoperatively (day 1) decreased by 5.4 ± 15.9% in the SA group, versus 15.2 ± 11.7% in the GA group (p = 0.02). The handgrip strength returned to baseline at day 7 and did not differ between groups at day 28. MIP increased postoperatively in patients randomized to SA by 11.7 ± 48.3%, whereas it decreased in GA by 12.2 ± 19.9% (p = 0.04). On day 7, MIP increased in both groups, but more in the SA (49.0 ± 47.8%) than in the GA group (14.2 ± 32.1%) (p = 0.006). Postoperatively, the levels of ACTH, cortisol and IL-6 increased in the GA, but not in the SA group (p < 0.004).
Conclusion
In patients having bilateral THA, SA preserved the postoperative respiratory and peripheral muscle strength and attenuated the neuro-endocrine and inflammatory responses.
Trial registration: clinicaltrials.gov NCT03600454.
Similar content being viewed by others
Background
PAMW may cause short-term functional impairment [1]. Pathophysiological mechanisms and preventive strategies are not known, although PAMW has some similarities with intensive care unit acquired weakness (ICUAW). Increased release of catabolic hormones and cytokines (neuro-endocrine stress response) are among the proposed mediators in the complex pathophysiological process of ICUAW and could be responsible also for PAMW [2, 3]. THA elicits the greatest stress response next to cardiac surgery and major abdominal and vascular surgery [4]. The surgically induced neuro-endocrine stress response can be detrimental and leads to systemic inflammatory response syndrome (SIRS), hyper-metabolism, and hyper-catabolism associated with postoperative complications such as muscle wasting, impaired immune function and wound healing, organ failure and even death [5, 6]. Previous studies have documented that neuraxial anaesthesia attenuates the neuro-endocrine stress response after surgery [7,8,9,10]. The clinical relevance of this attenuation and any effects on PAMW after major surgery are not known. Hypothetically, attenuation of the neuro-endocrine stress response may affect PAMW and early mobilization postoperatively [11,12,13].
In a recent propensity matched analysis comparing SA to GA in more than 70,000 patients undergoing THA, Ferreira et al. found a significant reduced operative time in the SA group, as well as also found significantly less 30-day complications, readmissions, and reoperations. [14] Another recent propensity-matched cohort analyses demonstrated a small but significant increase in incidence of major complications, pneumonia and mortality with GA as opposed to SA [15]. SA was also associated with a significant decrease in postoperative surgical site infections after THA in a recent meta-analysis [16]. It is clear that further investigations are necessary to determine the role of SA in the perioperative management and outcomes of patients undergoing THA.
In this study, it was hypothesized that SA attenuates the neuro-endocrine stress response and the magnitude of PAMW to a greater extent than GA. This exploratory prospective randomized controlled trial was performed in a well-defined cohort of patients undergoing bilateral THA under either SA or GA.
Methods
Study population
This randomized controlled trial was approved by the Ethical Committee of Ziekenhuis Oost-Limburg, Genk (March 22, 2018-18/0010U-B371201835378) and was registered at clinicaltrials.gov (NCT03600454- July 26, 2018). Initially the hypothesis was planned to be tested in two independent, but complementary, studies in patients having bilateral THA (Arm 1;SA), and in patients having major abdominal surgery (Arm 2; epidural anaesthesia).
Due to implementation of Enhanced Recovery After Surgery (ERAS) protocols in major abdominal surgery patients in our hospital after approval of this study epidural anaesthesia was abandoned, preventing recruitment of subjects in Arm 2. Consequently, the protocol was amended to eliminate Arm 2. All surgical procedures were performed by one surgeon using the anterior approach. Inclusion criteria were: (1) patients aged 18 years or older (2) bilateral THA. Exclusion criteria were: (1) inability to understand or give an informed consent; (2) urgent surgery; (3) contra-indications for SA; (4) allergy or contraindications to any products used in the protocol; (5) history of chronic opioid use; (6) preoperative use of corticosteroids [less than 3 months before surgery]; (7) history of muscle wasting disease [e.g., Steinert disease, amyotrophic lateral sclerosis; Duchenne dystrophy].
Patient characteristics, American Society of Anesthesiologists (ASA) classification, comorbidities (diabetes mellitus, hypertension, coronary heart disease, renal insufficiency, liver cirrhosis, cancer), duration of surgery, total amount of anaesthetics administered, postoperative Numeric Rating Scale (NRS) pain scores, and total hospital length of stay were recorded. Written informed consent was obtained from each patient before inclusion in the study.
Primary and secondary outcomes
The primary outcome variable was the change in peripheral limb muscle strength at postoperative day 1, 7 and 28, relative to baseline preoperative muscle strength. The baseline preoperative muscle strength is the muscle strength measured before surgery. The secondary outcomes were: (1) change in MIPat postoperative day 1, 7 and 28, (2) general health status as assessed by EQ-5D-5L questionnaires at postoperative day 1, 7 and 28 and (3) levels of markers of the neuro-endocrine stress and inflammatory response.
To reach sufficient statistical power (1-beta 0.80, based on a two-sided t-test with alpha 0.05) 22 subjects per group should be included. This power calculation was based on the assumption that a 10% decrease in muscle strength is clinically relevant in patients undergoing GA and that this could be reduced to a 7% drop in muscle strength when using SA with a SD of 3.5% [1]. A relative reduction of muscle weakness of 30% or more was considered as clinically relevant.
Study design
Patients were enrolled between September 2018 and November 2019. Randomization was performed using a computer-generated permuted block randomization sequence (variable block-size, 1:1 allocation) and occurred during the preoperative anaesthesia assessment. Patients were randomized in two groups: (1) SA combined with monitored anaesthesia care (MAC); and (2) GA.
Anaesthetic protocol
SA was performed thirty minutes before the onset of surgery using a standardized technique, consisting of 10 mg of intrathecal isobaric bupivacaine 0.5% administered at level L4–L5. During spinal anaesthesia, MAC was established with the administration of intravenous (IV) midazolam 1–2 mg and S-ketamine 5 mg. MAC was defined as the administration of anesthetics with the goal of patient comfort, while preserving meaningful patient contact. During surgery, MAC was administered to patients with IV propofol through target-controlled infusion (TCI); a target effect site concentration (EC) was maintained at 1.0 µg/ml (Marsh model).
During the induction of GA, patients received IV fentanyl 2 µg/kg and IV propofol through TCI; a target EC was maintained at 3.0 µg/ml (Marsh model) as maintenance of anaesthesia. Neuromuscular blockade was obtained with IV rocuronium 0.6 mg/kg. At the end of surgery, the neuromuscular blockade was reversed with the administration of IV sugammadex 4 mg/kg.
Intraoperatively, all patients received IV paracetamol 15 mg/kg (with a maximum dose of 1000 mg) and IV ketorolac 0.5 mg/kg (with a maximum dose of 30 mg). In the PACU, pain was treated by titrating IV piritramide 0.02 mg/kg, until the patient reported a NRS of 4 or less as per institutional protocol. On the ward, patients received IV paracetamol 15 mg/kg (with a maximum dose of 1000 mg) every 6 h and IV ketorolac 0.5 mg/kg (with a maximum dose of 30 mg) every 8 h. Intramuscular (IM) piritramide 0.2 mg/kg (maximum dose of 15 mg) up to four times a day was administered parenterally for NRS scores higher than 4. After oral intake was resumed, the oral analgesia protocol consisted of paracetamol 1000 mg each 6 h; diclofenac 75 mg each 12 h; tramadol slow-release 100 mg each 12 h; and tramadol fast-release 50 mg up to 4 times a day, when NRS were higher than 4.
Postoperative protocol
All subjects followed the institutional protocol for patients undergoing bilateral THA. They were all admitted to the ICU overnight for continuous haemodynamic observation. On postoperative day one they were allowed to walk under supervision of the physiotherapist. They were allowed to leave the hospital on postoperative day 2. An outpatient follow-up visit was planned 6 weeks after the surgery.
Peripheral limb muscle strength
Limb muscle strength was defined as the handgrip strength in the dominant hand and was measured using a handgrip dynamometer (Jamar® Plus Digital;Cognatus Innovations,LLC) with the patient in a sitting position and the elbow of the dominant arm in 90 degrees flexion. For each assessment, the average of three measurements was calculated and used in the analyses. Preoperatively, these values were normalized for age, gender and height using validated reference values (normalized strength = measured mean strength/reference value), which are shown in Table 1 for both groups [17]. For the rest of the analyses, relative changes compared to these baseline values are used or shown in figures.
Respiratory muscle strength
Respiratory muscle strength testing was performed using spirometry (Powerbreathe K3; POWERbreathe International Ltd.; UK). The MIP is a frequently used measure of the strength of inspiratory muscles, primarily the diaphragm, and allows for the assessment of ventilatory failure, restrictive lung disease and respiratory muscle strength and has been validated as a marker of ICUAW [18,19,20]. MIP was measured with the patient in sitting position. For each assessment, the average of three measurements was calculated and used in the analyses. Preoperatively, these values were normalized for age, gender and height using validated reference values (normalized MIP = measured mean MIP/reference value), which are shown in Table 1 for both groups [21]. For the rest of the analyses, relative changes compared to these baseline values are used or shown in figures.
General health status
General health status was assessed using the EuroQol EQ-5D-5L questionnaire (Additional file 1). The descriptive system comprises five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension has 5 levels: no problems, slight problems, moderate problems, severe problems and extreme problems. Handgrip strength, MIP and general health status were measured at four time points: (1) during the preoperative anaesthesia assessment, which served as a baseline measurement; (2) on postoperative day one; (3) and during a home visit on postoperative day 7 and (4) on postoperative day 28.
Biochemical data
Since the neuro-endocrine and inflammatory stress response is known to play an important role in the development of ICUAW, the levels of the markers of these pathways, including the documented mediators concerning muscle function, HPA-axis and IL-6 were evaluated as these are validated markers of the surgically induced neuro-endocrine stress response and inflammatory response [5].
Blood was collected right before and at the end of surgery and 24 h after surgery in K2-EDTA tubes (BD Vacutainer, Ref 367864; BD, UK). Samples were centrifuged for 10 min at 1500 RCF and plasma was frozen at − 80 °C within 1 h after collection and kept frozen until analyzed. Analyses for ACTH, cortisol and IL-6 were performed on cobas e801. Quality controls were performed according to the ISO 15189 procedures of the central laboratory.
Statistical analyses
Data are presented as means and standard deviations. Statistical analyses were performed with JMP version 15.0 (SAS Institute Inc., Cary, NC). Parametric comparisons between groups were made with the student t-test for normally distributed data. Normality of the data was evaluated using the Anderson–Darling test. Two-sided p-values of 0.05 or lower were considered statistically significant.
Results
Study population and patient characteristics
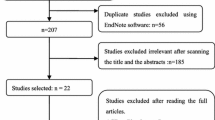
A total of 50 patients were included and randomized. In the GA group, 1 patient withdrew consent and 1 patient received corticosteroids during surgery and was excluded due to protocol violation. In the SA group, 1 patient was converted to GA and 1 patient received peripheral blocks to SA, which was a protocol violation (Fig. 1). Therefore, the final analysis included a total of 46 patients, or 23 in each group. Patient demographics are shown in Table 1. No patients were lost to follow-up at day 7; 2 patients were lost to follow-up at day 28.
Peripheral muscle function
Preoperative handgrip strength was comparable among both groups and was reduced to 82.72% (SD 20.78%) in the GA group and 76.63% (SD 18.79%) in the SA group (p = 0.28) as compared to their preoperatively baseline values (Table 1) [17].
Patients who received GA had a decrease in handgrip strength, as compared to their preoperative baseline values, by a mean 15.25% (SD 11.77%) on postoperative day 1, as opposed to a decrease of 5.49% (SD 15.96%) in the SA group (p = 0.02). Handgrip strength was restored to preoperative values by day 7 in both groups [+ 1.92% from baseline (SD 10.26%) in the GA group; + 2.98% from baseline (SD 14.40%) in the SA group (p = 0.78)]. At the 28-day follow-up, handgrip strength was comparable to preoperative values in both groups (0.25% (SD 10.22%) decrease in the GA group and a + 7.5% (SD 22.84%) from baseline in the SA group (p = 0.15). The changes of handgrip strength over time for each type of anaesthesia are shown in Fig. 2 and Table 2.
The evolution over time of changes in handgrip strength and the effect of type of anaesthesia. Mean and standard deviation of handgrip strength are shown on different time points as a percentage relative to baseline being the preoperative values and this for the different types of anaesthesia. P-values indicate the relative difference between the two types of anaesthesia on the different time points. GA general anaesthesia, SA spinal anesthesia, MIP maximum inspiratory pressure
Respiratory muscle function
The baseline MIP, adjusted for age and gender, was comparable between the two groups and was reduced as compared to their expected baseline values (Table 1) [21].
Hip replacement surgery under GA was associated with a decrease in MIP, as compared to their baseline value, by a mean 12.24%, (SD 19.95%) on postoperative day 1, whereas MIP increased in the SA group by 11.72% (SD 48.30%) (p = 0.04). On day 7 MIP increased in both groups, as compared to the preoperative values. The increase in MIP was larger in patients receiving SA [mean increase 49.06% (SD 47.88%) in the SA group and 14.28% (SD 32.18%) in the GA group (p = 0.006)]. At the 28-day follow-up, MIP was increased in both groups as compared to preoperative values, however, without a statistically significant difference between groups, respectively, a 51.10% (SD 60.05%) increase in the SA group and a (27.77% (SD 43.39%) increase in the GA group (p = 0.16). The evolution over time of postoperative MIP and the effect of anaesthesia are shown in Table 2 and Fig. 3. No correlation between the duration of surgery and MIP on postoperative day 1 was found.
The evolution over time of changes in MIP and the effect of type of anaesthesia. Mean and standard deviation of MIP are shown on different time points as a percentage relative to baseline being the preoperative values and this for the different types of anaesthesia. P-values indicate the relative difference between the two types of anaesthesia on the different time points. GA general anaesthesia, SA spinal anesthesia, MIP maximum inspiratory pressure
Health status
Median length of hospital stay was 3.5 days (IQR 3–6) in the GA group versus 3 days (IQR 3–5) in the SA group (p = 0.41).
The EQ5D-5L index was similar among both groups at baseline, with the mean EQ5D-5L index 0.81 (SD 0.09) in the GA group and 0.78 (SD 0.08) in the SA group (p = 0.30) (Table 1). On postoperative day 1, the EQ5D-5L index decreased by a mean 50.74% decrease in the GA group (SD 22.37%) and a mean 52.21% decrease in the SA group (SD 22.97%). This decrease was not associated with the type of anaesthesia (p = 0.82). Over the postoperative period, the EQ5D-5L index recovered, reaching similar preoperative values at follow-up day 28. Pain scores on postoperative day 1, during evaluation of the peripheral and lung muscle function, were comparable between the two groups (p = 0.61) (Fig. 4).
Markers of neuro-endocrine stress response and inflammatory response (Table 3)
ACTH levels were elevated at the end of surgery in the GA group, but not in the SA group (p = 0.003) (Fig. 5). This elevated ACTH level was accompanied by elevation in cortisol level. The levels of ACTH and cortisol were not elevated in the SA group (p < 0.0001) (Fig. 5). Interestingly, on postoperative day 1, cortisol was similarly elevated in both groups (p = 0.54) with low ACTH levels.
The evolution over time of changes of markers of the neuro-endocrine and inflammatory stress response and the effect of type of anesthesia. Mean values and standard deviations of ACTH, Cortisol and IL-6 are shown on different time points for the different types of anaesthesia. P-values indicate the relative difference between the two types of anaesthesia on the different time points. ACTH adrenocorticotropic hormone, IL-6 interleukin-6
IL-6 levels increased at the end of surgery twice as much in the GA group as compared to the SA group (p = 0.0029). The highest increase in IL-6 was seen on postoperative day 1, with no difference between both groups (p = 0.40) (Fig. 5).
Discussion
This exploratory prospective randomized controlled trial demonstrated that patients who underwent bilateral hip replacement developed generalized muscle weakness postoperatively. Thereby note that a bilateral hip replacement is more invasive than a unilateral replacement. The degree of muscle weakness was greater in patients who received GA compared to patients who received SA. The SA patients also had a higher postoperative handgrip strength, MIP and lower levels of ACTH, cortisol, and IL-6 in the immediate postoperative period. The modulating effect on the neuro-endocrine pathway of neuraxial anaesthesia has been reported previously [22, 23]. Since it is known that several components of the neuro-endocrine stress response, such as cortisol, and the inflammatory response, for example IL-6, may induce muscle catabolism, the effect of the intervention on markers of these pathways was evaluated. SA yielded lower levels of ACTH, cortisol, and IL-6, but only in the immediate postoperative period on day 1. These data suggest that SA may modulate the immediate neuro-endocrine and inflammatory responses in patients having lower limb orthopaedic surgery. A recent systematic review, however, suggests that neuraxial anaesthesia does not influence IL-6 as compared to GA, but the interpretation of that review is limited by high heterogeneity [24]. In contrast, the current study has high internal validity (single center, only patients undergoing bilateral THA and one surgeon). Furthermore, measuring the levels of cytokines at only one time point might be insufficient to detect an effect. Therefore, further studies are needed to elucidate the effects of neuraxial anaesthesia on inflammatory pathways.
Handgrip dynamometry is an effective screening tool for global muscle weakness as a surrogate for the Medical Research Council (MRC) score and, it is associated with hospital mortality [25, 26]. In the current study, elective bilateral hip replacement under GA resulted in a 15% decrease in peripheral handgrip strength of the dominant arm. In the study by Lachmann et al., however, the PAMW persisted for more than one month, whereas in the current study the muscle strength was already restored to preoperative values after 7 days and this regardless of the type of anaesthesia [1]. However, the patients in the study of Lachmann et al. were generally older and underwent more invasive surgery [1]. In contrast, Petersson et al. did not find a decrease in peripheral muscle strength after elective cholecystectomy [27]. The discrepancy in these reports suggests that perioperative weakness may be lesser in young patients having less invasive surgery, but more severe and/or longer lasting in older patients having major surgery. This hypothesis, however, needs to be further substantiated. Nevertheless, patients who received SA in the current study had only a minor reduction in the muscle weakness (5% decrease in handgrip strength), or just a third of the reduction observed in the GA group (15% reduction). It is important to realize that the perioperative peripheral muscle weakness was only a transient effect, possibly influencing the postoperative period, but wasn’t sustained until one month after surgery. Therefore, the choice of anesthesia might influence the direct postoperative period, which is important in early recovery after surgery, but not in the long term.
Postoperative respiratory muscle function also appeared to recover faster in patients who had SA, as opposed to patients who received GA. In the GA group, there was a decrease in respiratory muscle strength on postoperative day 1, followed by a gradual recovery in MIP in the postoperative period. SA resulted in a better respiratory muscle strength in the direct postoperative period and this effect lasted during the following assessments on postoperative day 7 and day 28. It is well established that even a limited duration of mechanical ventilation may induce atrophy of the diaphragm, and that anaesthetics negatively affect the postoperative pulmonary function [28]. Regardless, the prolonged decrease in MIP that was documented on day 7 and day 28, could not cogently be explained. The reduced MIP at baseline in patients receiving bilateral hip replacement could be due to deconditioning.
The decrease in global health status in the immediate postoperative period, and its return to the pre-operative level after one month, was unaffected by the type of anaesthesia. The use of more sensitive questionnaires investigating fatigue and early recovery after surgery, such as QOR-15, in future larger studies could potentially clarify if this muscle strength preserving effect of SA translates in a better recovery after surgery.
Our study findings are in agreement with Lattermann et al. who reported that neuraxial anaesthesia decreases the catabolic stress response after surgery, and protein catabolism [7]. The reduction in muscle catabolism by modulating the stress response could be one of the factors that may be responsible for the lower effect seen on muscle strength in patients who received SA for bilateral THA. However, anaesthesia technique-related neuromuscular coupling/uncoupling and the central effects of anaesthesia on volitional testing cannot be excluded. Our data also confirm the findings of Lachmann et al. that surgery does indeed induce substantial muscle weakness [1]. To our knowledge, this study is the first to report a modulating effect of the type of anaesthesia on this PAMW. This may be of clinical importance, since reduction of PAMW may negatively affect early mobilization, rehabilitation, and ERAS protocols, therefore favoring SA in patients having bilateralTHA.
Limitations
The effect of anaesthesia in bilateral total hip replacement surgery through the anterior approach was investigated in the current study. Therefore, these results should not be extrapolated to other surgical procedures. In addition, anterior approach to total hip arthroplasty is considered as “minimally invasive” and associated with a lower inflammatory response in comparison to traditional approaches [29]. Therefore, the difference between the GA and SA group could be different with traditional techniques for hip replacement. Moreover, dexamethasone or similar steroids were not administered in the perioperative phase although these medications reduce the surgical stress response and, therefore, could have an added value in the recovery of THA patients. Future studies need to evaluate the effect of glucocorticoids on postoperative muscle weakness and their impact on early recovery. Although the current study was adequately powered, a type 1 error is possible in smaller studies. Furthermore, since we investigated the change in muscle strength and not the muscle strength per se, we haven’t stratified for sex, BMI, or age since one wouldn’t expect a modulatory effect on muscle strength of these factors, however, one can’t exclude this possibility. Hence, larger confirmatory studies are needed to increase the external validity of the findings. Thirdly, while MIP and handgrip strength are commonly used as validated and objective measurements of muscle weakness, the effect of the intervention on other muscle related outcomes, such as a 6 min walking test, was not investigated. Moreover, the central effects of GA on the volitional nature of the MIP and PAMW measurements may have disfavored the GA group. Fourthly, our exploratory study was designed and powered to detect a difference in peripheral muscle weakness, a recently identified perioperative complication. However, larger, subsequent studies are necessary to study whether the observed effect on muscle weakness is associated with improved clinical outcomes, such as fatigue and fast tracking after surgery.
Conclusion
In our study, in patients having bilateral THA, SA attenuated neuro-endocrine and inflammatory responses, and preserved the postoperative respiratory and peripheral muscle strength, compared to GA.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACTH:
-
Adrenocorticotropic hormone
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- EC:
-
Effect site concentration
- ERAS:
-
Enhanced recovery after surgery
- GA:
-
General anaesthesia
- ICUAW:
-
Intensive care unit acquired muscle weakness
- IL-6:
-
Interleukin 6
- IM:
-
Intramuscular
- IQR:
-
Interquartile range
- IV:
-
Intravenous
- MAC:
-
Monitored anaesthesia care
- MIP:
-
Maximal inspiratory pressure
- MRC:
-
Medical Research Council
- NRS:
-
Numeric rating scale
- PACU:
-
Post anaesthesia care unit
- PAMW:
-
Perioperatively acquired muscle weakness
- SA:
-
Spinal anaesthesia
- SD:
-
Standard deviation
- TCI:
-
Target-controlled infusion
- THA:
-
Total hip arthroplasty
References
Lachmann G, Mörgeli R, Kuenz S, BIOCOG Consortium, et al. Perioperatively acquired weakness. Anesth Analg. 2020;130(2):341–51.
Friedrich O, Reid MB, Van den Berghe G, et al. The sick and the weak: neuropathies/myopathies in the critically ill. Physiol Rev. 2015;95(3):1025–109.
Hermans G, Van den Berghe G. Clinical review: intensive care unit acquired weakness. Crit Care. 2015;19(1):274.
Watt DG, Horgan PG, McMillan DC. Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery. 2015;157(2):362–80.
Cusack B, Buggy DJ. Anaesthesia, analgesia, and the surgical stress response. BJA Educ. 2020;20(9):321–8.
Park JT, Kim JY, Kim YW, Choi KH, et al. Stress-induced cardiomyopathy after general anesthesia for total gastrectomy—a case report. Korean J Anesthesiol. 2010;58(3):299–303.
Lattermann R, Belohlavek G, Wittmann S, et al. The anticatabolic effect of neuraxial blockade after hip surgery. Anesth Analg. 2005;101(4):1202–8.
Kouraklis G, Glinavou A, Raftopoulos L, et al. Epidural analgesia attenuates the systemic stress response to upper abdominal surgery: a randomized trial. Int Surg. 2000;85:353–7.
Lattermann R, Carli F, Schricker T. Epidural blockade suppresses lipolysis during major abdominal surgery. Reg Anesth Pain Med. 2002;27(5):469–75.
Holte K, Kehlet H. Epidural anaesthesia and analgesia-effects on surgical stress responses and implications for postoperative nutrition. Clin Nutr. 2002;21:199–206.
Shyam Kumar AJ, Beresford-Cleary N, Kumar P, et al. Preoperative grip strength measurement and duration of hospital stay in patients undergoing total hip and knee arthroplasty. Eur J Orthop Surg Traumatol. 2013;23(5):553–6.
Oosting E, Hoogeboom TJ, Dronkers JJ, et al. The influence of muscle weakness on the association between obesity and inpatient recovery from total hip arthroplasty. J Arthroplasty. 2017;32(6):1918–22.
Mitrovic D, Davidovic M, Erceg P, et al. The effectiveness of supplementary arm and upper body exercises following total hip arthroplasty for osteoarthritis in the elderly: a randomized controlled trial. Clin Rehabil. 2017;31(7):881–90.
Ferreira AC, Hung CW, Ghanta RB, et al. Spinal anesthesia is a grossly underutilized gold standard in primary total joint arthroplasty: propensity-matched analysis of a national surgical quality database. Arthroplasty. 2023;5(1):7.
Harris AB, Valenzuela J, Andrade N, et al. Comparison of pneumonia and major complications after total joint arthroplasty with spinal versus general anesthesia: a propensity-matched cohort analysis. J Am Acad Orthop Surg. 2023. https://doi.org/10.5435/JAAOS-D-23-00192.
Li Z, Xu X, Zhuang Z, et al. Impact of spinal Anaesthesia versus general Anaesthesia on the incidence of surgical site infections after knee or hip arthroplasty: a meta-analysis. Int Wound J. 2023. https://doi.org/10.1111/iwj.14369.
Steiber N. Strong or weak hand grip? Normative reference values for the german population across the life course stratified by sex, age, and body height. PLoS ONE. 2016;11(10):e0163917.
Sachs MC, Enright PL, Hinckley Stukovsky KD, Multi-Ethnic Study of Atherosclerosis Lung Study, et al. Performance of maximum inspiratory pressure tests and maximum inspiratory pressure reference equations for 4 race/ethnic groups. Respir Care. 2009;54(10):1321–8.
American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518–624.
Tzanis G, Vasileiadis I, Zervakis D, et al. Maximum inspiratory pressure, a surrogate parameter for the assessment of ICU-acquired weakness. BMC Anesthesiol. 2011;11:14.
Sclauser Pessoa IM, Franco Parreira V, Fregonezi GA, et al. Reference values for maximal inspiratory pressure: a systematic review. Can Respir J. 2014;21(1):43–50.
Møller IW, Hjortsø E, Krantz T, et al. The modifying effect of spinal anaesthesia on intra- and postoperative adrenocortical and hyperglycaemic response to surgery. Acta Anaesthesiol Scand. 1984;28(3):266–9.
Lee TW, Grocott HP, Schwinn D, Winnipeg High-Spinal Anesthesia Group, et al. High spinal anesthesia for cardiac surgery: effects on beta-adrenergic receptor function, stress response, and hemodynamics. Anesthesiology. 2003;98(2):499–510.
Alhayyan A, McSorley S, Roxburgh C, et al. The effect of anesthesia on the postoperative systemic inflammatory response in patients undergoing surgery: a systematic review and meta-analysis. Surg Open Sci. 2019;2(1):1–21.
Ali NA, O’Brien JM Jr, Hoffmann SP, Midwest Critical Care Consortium, et al. Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med. 2008;178(3):261–8.
Leong DP, Teo KK, Rangarajan S, Prospective Urban Rural Epidemiology (PURE) Study investigators, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015;386(9990):266–73.
Petersson B, Wernerman J, Waller SO, et al. Elective abdominal surgery depresses muscle protein synthesis and increases subjective fatigue: effects lasting more than 30 days. Br J Surg. 1990;77:796–800.
Warner DO. Preventing postoperative pulmonary complications: the role of the anesthesiologist. Anesthesiology. 2000;92(5):1467–72.
Bergin PF, Doppelt JD, Kephart CJ, et al. Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J Bone Joint Surg Am. 2011;93(15):1392–8.
Acknowledgements
The authors would like to acknowledge the instrumental help of the nurses of the regional anaesthesia team and Jirka Cops researcher at the New York School of Regional Anesthesia.
Funding
Support was provided solely from institutional and/or departmental sources.
Author information
Authors and Affiliations
Contributions
SVB: this author helped with concept and design of the study, acquisition of data, analysis and interpretation of data, drafting and revising article, final approval of the version to be submitted. LP: this author helped with concept and design of the study, acquisition of data, analysis and interpretation of data, drafting and revising article, final approval of the version to be submitted. DD: this author helped with concept and design of the study, acquisition of data, analysis and interpretation of data, drafting and revising article, final approval of the version to be submitted. JP: this author helped with acquisition of data, analysis and interpretation of data, drafting article, final approval of the version to be submitted. AH: this author helped with acquisition of data, analysis and interpretation of data, drafting article, final approval of the version to be submitted. IM: this author helped with acquisition of data, analysis and interpretation of data, drafting article, final approval of the version to be submitted. KC: this author helped with concept and design of the study, analysis and interpretation of data, drafting and revising article, final approval of the version to be submitted. DM: this author helped with concept and design of the study, acquisition of data, analysis and interpretation of data, drafting and revising article, final approval of the version to be submitted. ST: this author helped with concept and design of the study, acquisition of data, analysis and interpretation of data, drafting and revising article, final approval of the version to be submitted. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval by Ethisch comité, Ziekenhuis Oost-Limburg Genk, Belgium, Chair Dr. P Noyens 18/0010U-B371201835378. All subjects gave written consent to participate in this trial.
Consent for publication
All subjects gave a written consent to accept publication of the data of the study.
Competing interests
AH has consulted, advised and/or performed industry-sponsored research for Philipps, GE, Sonosite, Konica Minolta, Codman & Shurtleff, Inc (Johnson and Johnson), Cadence, Insitu Biologics, Heron Therapeutics, Pacira, Baxter and BBraun Medical. Dr. Hadzic receives royalty income from BBraun Medical. He owns and directs NYSORA, the New York School of Regional Anesthesia. The other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: General health status was assessed using the EuroQol EQ-5D-5L questionnaire
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Van Boxstael, S., Peene, L., Dylst, D. et al. The effect of spinal versus general anaesthesia on perioperative muscle weakness in patients having bilateral total hip arthroplasty: a single center randomized clinical trial. Eur J Med Res 28, 450 (2023). https://doi.org/10.1186/s40001-023-01435-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-023-01435-6