Abstract
Background
Antimicrobial resistance (AMR) is a growing global health threat that contributes to substantial neonatal mortality. Bangladesh has reported some of the highest rates of AMR among bacteria causing neonatal sepsis. As AMR colonization among newborns can predispose to infection with these bacteria, we aimed to characterize the frequency of and risk factors for colonization of mothers and newborns during hospitalization for delivery.
Methods
We enrolled pregnant women presenting for delivery to a tertiary care hospital in Faridpur, Bangladesh. We collected vaginal and rectal swabs from mothers pre- and post-delivery, rectal swabs from newborns, and swabs from the hospital environment. Swabs were plated on agars selective for extended-spectrum-beta-lactamase producing bacteria (ESBL-PB) and carbapenem-resistant bacteria (CRB). We performed logistic regression to determine factors associated with ESBL-PB/CRB colonization.
Results
We enrolled 177 women and their newborns during February-October 2020. Prior to delivery, 77% of mothers were colonized with ESBL-PB and 15% with CRB. 79% of women underwent cesarean deliveries (C-section). 98% of women received antibiotics. Following delivery, 98% of mothers and 89% of newborns were colonized with ESBL-PB and 89% of mothers and 72% of newborns with CRB. Of 290 environmental samples, 77% were positive for ESBL-PB and 69% for CRB. Maternal pre-delivery colonization was associated with hospitalization during pregnancy (RR for ESBL-PB 1.24, 95% CI 1.10–1.40; CRB 2.46, 95% CI 1.39–4.37). Maternal post-delivery and newborn colonization were associated with C-section (RR for maternal CRB 1.31, 95% CI 1.08–1.59; newborn ESBL-PB 1.34, 95% CI 1.09–1.64; newborn CRB 1.73, 95% CI 1.20–2.47).
Conclusions
In this study, we observed high rates of colonization with ESBL-PB/CRB among mothers and newborns, with pre-delivery colonization linked to prior healthcare exposure. Our results demonstrate this trend may be driven by intense use of antibiotics, frequent C-sections, and a contaminated hospital environment. These findings highlight that greater attention should be given to the use of perinatal antibiotics, improved surgical stewardship for C-sections, and infection prevention practices in healthcare settings to reduce the high prevalence of colonization with AMR organisms.
Similar content being viewed by others
Introduction
Antimicrobial resistance (AMR) is a growing global health threat that disproportionately affects low- and middle-income countries (LMIC) and represents one of the leading causes of mortality worldwide [1, 2]. Neonates are a key risk group for infections with AMR organisms given their immature microbiome and underdeveloped host defenses [3, 4]. Neonates are often exposed to a wide range of bacteria at the time of birth, which can result in colonization. Colonization occurs when bacteria persist in or on body surfaces without causing illness. Although colonization does not directly cause disease, colonization with resistant bacteria can predispose individuals to developing drug-resistant infections, particularly among newborns with prematurity and low birthweight [5,6,7]. Neonatal sepsis caused by AMR organisms results in higher rates of mortality compared with non-AMR infections [8]. An estimated 200,000 neonatal deaths annually have been attributed to infections with AMR organisms [1, 9].
In many LMICs, the majority of cases of neonatal sepsis are caused by Gram-negative bacteria, many of which are multidrug resistant [8, 10,11,12,13]. A report from 2020 demonstrated that 81% of Gram-negative bacteria causing sepsis in newborns across three neonatal care units in Bangladesh were resistant to carbapenems, one of the last line antibiotic options [12]. Similar concerning trends of increasing AMR in neonatal infections have been observed elsewhere in South and Southeast Asia, including among homebirths, demonstrating an increasing community reservoir for AMR [14,15,16].
Healthcare facilities, in particular, have been implicated as an important source of AMR amplification because of the associated intense antibiotic use and admixing of ill and susceptible patients [17, 18]. This is further exacerbated in low-resource hospitals because of overcrowding, understaffing, inadequate hygiene and sanitation, and a lack of access to diagnostics. In these settings, antibiotics are often used liberally in healthcare facilities as a substitute for improved hygiene and sanitation, and the lack of diagnostics precludes antibiotic stewardship practices [19, 20]. Understanding the environments that are promoting evolution and transmission of such organisms to newborns is an essential step towards preventing exposure, thereby avoiding downstream consequences such as resistant infections that may be difficult or impossible to treat.
The objective of this study was to estimate the burden of and risk factors for colonization with extended-spectrum beta-lactamase producing bacteria (ESBL-PB) and carbapenem-resistant bacteria (CRB) among mothers and newborns in the context of facility-based deliveries. As one step in the infection pathway, colonization provides a useful parameter for monitoring transmission patterns that could predispose to infection [21,22,23].
Methods
Participant enrollment
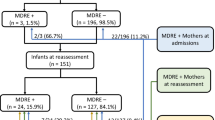
We enrolled pregnant women presenting for delivery at a tertiary care public medical college hospital in Faridpur, Bangladesh, during February – March and August – October, 2020. A four-month interruption in enrollment (April-July) occurred as a result of data collection restrictions during the COVID-19 pandemic. A trained member of the nursing staff collected a set of vaginal and rectal swabs. The project research physician conducted interviews with the participants to obtain demographic and community exposure information about exposures that were hypothesized could be related to AMR colonization, including socioeconomic status, sanitation, animal contact, antibiotic use, and healthcare contact (S1 Fig). Over the course of the hospitalization, the research physician gathered information from the medical charts and care providers regarding treatments and interventions. Prior to hospital discharge, and at least 24 h after delivery, the nursing staff collected a second set of vaginal and rectal swabs from the mothers and a rectal swab from their newborns. A total of 177 mother/baby pairs completed data collection (Fig. 1).
Environmental sampling
During the same time interval as participant enrollment, the study team collected samples of the hospital environment from the perinatal ward, labor room, and the operating room in which cesarean deliveries (C-sections) were performed. The selection of sampled items was determined following a three-day observation period during which frequently touched surfaces and shared equipment were identified and counts of hand contacts were noted for each type of surface or equipment. We purposefully sampled these sites throughout the study period. The sampling sites included hands of healthcare workers and patient attendants, shared medical equipment, beds, faucets, doors, toilet facilities, oxygen delivery devices, floors, and other surfaces. For each day of participant enrollment, we obtained three environmental swabs. Swabs were first moistened with sterile water before sampling surfaces.
Bacterial culturing of swab samples
Participant (rectal and vaginal) and environmental swabs were placed in Amies media and stored at 2–8 °C until they could be transported to the lab. All swabs were processed within 24 h of collection. Participant swabs were directly inoculated onto CHROMagar ESBL and CHROMagar mSuperCARBA (CHROMagar, Paris, France). Environmental swab samples were enriched with trypticase soy broth (TSB) with overnight incubation at 37 °C before the samples were inoculated onto the same media as the participant swabs. From the chromogenic agars, bacterial colony growth color and characteristics were recorded after overnight incubation at 37 °C.
Statistical analysis
We performed descriptive statistics to summarize epidemiologic characteristics of participants. We compared the proportion of colonized individuals and environmental samples before the start of the COVID-19 pandemic (Feb-Mar) and during the pandemic (Aug-Oct). To examine the relationship between community-based exposures on pre-delivery AMR colonization patterns and hospital-based exposures on post-delivery AMR colonization patterns, we performed logistic regression. We calculated unadjusted risk ratios for all community- and hospital-based exposures. The sample size for the risk factor analysis was determined using an estimated 80% colonization with at least one AMR organism and a 20% expected difference in outcomes between exposed and unexposed individuals, considering a design effect of 1.2. We used McNemar’s test to determine differences in colonization prevalence across various time points for paired samples and a test of proportions to determine differences in colonization for unpaired samples.
Community or hospital exposures with p-values < 0.2 that had at least 10% prevalence and were not collinear were included in multivariable analysis. In the newborn analyses, we did not control for maternal post-delivery colonization to avoid masking potentially significant newborn exposures. No additional model refining was performed as the objective of the analysis was not to optimize a final predictive model, which would likely not be robust given the limited dataset, but to generate hypotheses regarding factors most likely to drive AMR colonization. Participants with missing data were excluded from the respective analyses, which only included age (eight participants) and income (one participant). All analyses were conducted using the statistical program Stata (Version 17.0, StataCorp, College Station, TX).
Results
Demographics of pregnant women enrolled in the study
Of the 177 women enrolled in the study, the median age was 25 years (range 17–40) (Table 1). The majority of participants (73%) had at least a secondary school education. The median monthly household income was 201 USD (amounting to $1.34/person/day). Almost all households had improved drinking water sources, with 98% of households reporting tube wells as the main water source. Pit latrines were the most common toilet type (79%). Approximately one-third (33%) of the women had no prior pregnancies. While most women had received some prenatal care, only 14% reported four or more visits. Anemia was the most frequent pregnancy complication, reported by nearly half of participants. Two-thirds of deliveries occurred at or post-term.
The majority of women (79%) delivered via C-section (Table 2). Duration of hospitalization was longer for women undergoing C-section compared with vaginal delivery (4.0 versus 1.6 days, p < 0.001). Nearly all women received perinatal prophylactic antibiotics (98%), of whom, 91% received them before or during delivery. The prescribed duration of antibiotics was longer for women who underwent C-section compared with vaginal delivery (10 versus 7.6 days, p < 0.001). The most common antibiotics administered were metronidazole (89%), flucloxacillin (69%), and third-generation cephalosporins (ceftriaxone or cefixime) (67%) (S1 Table). The most frequent antibiotic regimen was a combination of a third-generation cephalosporin, metronidazole, and flucloxacillin (48%). No carbapenem use was reported. More than half of the participants experienced a pregnancy complication, including fetal distress/cord prolapse (40%), obstructed/prolonged labor (27%), or prolonged rupture of membranes (> 24 h) (23%).
Among the newborns, nearly all received airway clearing, wiping and wrapping, temperature and weight measuring, and feeding initiation within the first hour of birth (Table 3). Approximately one-quarter underwent resuscitation with two newborns requiring artificial ventilation. 5% of newborns received antibiotics, including three (2%) newborns with clinically-diagnosed neonatal sepsis. No blood cultures were collected at the time of diagnosis or during the course of treatment. No neonatal deaths occurred among enrolled newborns during the course of the study.
Colonization patterns of mothers and newborns with ESBL-PB and CRB
On admission, 17% of women (n = 30) had vaginal colonization and 71% (n = 125) had rectal colonization with organisms recovered from CHROMagar ESBL plates (hereafter referred to as ESBL-PB), but only 15% (n = 27) had rectal or vaginal colonization with organisms recovered from CHROMagar mSuperCARBA plates (hereafter referred to as CRB) (Fig. 2). At the time of discharge following delivery, nearly all women had either rectal or vaginal colonization with ESBL-PB (98%, n = 174), 86% (n = 153) had rectal CRB colonization, and 74% (n = 130) had vaginal CRB colonization. Newborns demonstrated rectal colonization patterns similar to maternal colonization patterns on discharge: 89% (n = 157) were colonized with ESBL-PB, and 72% (n = 128) were colonized with CRB.
Vaginal and rectal colonization of mothers and rectal colonization of newborns with ESBL-producing and carbapenem resistant bacteria at a tertiary care facility, Faridpur, Bangladesh, 2020 (N = 177). Prevalence of colonization patterns among mothers and newborns. Colonization was compared pre- and post-delivery to determine differences between community-based colonization and colonization following healthcare exposure. ESBL-PB = organisms recovered from agar selective for extended-spectrum beta-lactamase-producing bacteria; CRB = organisms recovered from agar selective for carbapenem resistant bacteria. ***McNemar’s test p < 0.001
Prevalence of ESBL-PB and CRB in environmental samples
A total of 290 environmental swab samples were collected from the perinatal ward, labor room, and operating room (S2 Table). Overall, 77% (n = 222) of samples were positive for ESBL-PB and 69% (n = 201) were positive for CRB; patterns were similar across types of samples analyzed (Fig. 3). However, many surfaces had multiple colony morphologies on the selective plates, demonstrating broad organism diversity (S2 Fig).
Environmental detection of ESBL-producing and carbapenem resistant bacteria in the obstetric facilities of a tertiary care hospital, Faridpur, Bangladesh, 2020 (N = 290). Frequency of contamination of various hospital environmental surfaces during the study period. Hand samples were taken from healthcare workers as well as patient attendants. A full list of sampled surfaces is in S3 Table. ESBL-PB = organisms recovered from agar selective for extended-spectrum beta-lactamase-producing bacteria; CRB = organisms recovered from agar selective for carbapenem resistant bacteria
Prevalence of ESBL-PB/CRB colonization in relation to COVID-19
Pre-delivery rectal ESBL-PB colonization was significantly higher after the start of the COVID-19 pandemic (81%) compared with before COVID (63%, p = 0.01) (S3 Table). Similarly, pre-delivery rectal CRB colonization increased during COVID (8% vs. 20%, p = 0.02). Pre-delivery vaginal ESBL-PB and CRB colonization also increased, but the differences were not significant (ESBL-PB: 15% vs. 20%, p = 0.43; CRB: 2% vs. 6%, p = 0.13).
In contrast, post-delivery rectal colonization was similar before and after the start of COVID (ESBL-PB: 96% vs. 99%, p = 0.28; CRB 83% vs. 91%, p = 0.13). Post-delivery vaginal colonization was also stable (ESBL-PB: 92% vs. 86%, p = 0.18; CRB: 72% vs. 75%, p = 0.62). Newborn colonization increased, but the differences were only marginally significant (ESBL-PB: 85% vs. 94%, p = 0.08; CRB: 67% vs. 79%, p = 0.07).
Overall environmental contamination with ESBL-PB and CRB was markedly higher during COVID compared with before the pandemic (ESBL-PB: 54% vs. 94%, p < 0.001; CRB: 45% vs. 89%, p < 0.001) (S3 Figure).
Community and hospital exposures associated with ESBL-PB/CRB colonization in mothers and newborns
Colonization outcome variables were grouped by resistance phenotype as the selective pressures contributing to colonization with a given phenotype are likely to be similar regardless of body site. Although vaginal colonization with AMR organisms was generally lower than rectal colonization, this is likely a result of different microbiome constitutions, with a predominance of Gram-negative organisms colonizing the rectum compared with the vaginal canal.
In the multivariate analysis of community-based exposures, variables associated with an increased risk for pre-delivery ESBL-PB colonization included prior hospitalization during pregnancy (RR 1.24, 95% CI 1.10–1.40) and preterm delivery (1.18, 95% CI 1.02–1.37) (Table 4). Variables associated with pre-delivery CRB colonization were seven or more people living in the household (RR 2.39, 95% CI 1.11–5.11), goats outside the home (RR 0.44, 95% CI 0.24–0.80), prior hospitalization during pregnancy (RR 2.46, 95% CI 1.39–4.37), and antibiotic use within the prior 30 days (RR 2.51, 95% CI 1.45–4.35). While it did not reach statistical significance at a p < 0.05 cutoff, raising ducks outside the home had the highest measures of association with pre-delivery CRB colonization (RR 6.36, 95% CI 0.91–44.3).
Although the prevalence was too low to allow inclusion in the multivariate analysis, other significant variables associated with ESBL-PB colonization in the bivariate analysis included tending livestock or poultry (RR 1.23, 95% CI 1.04–1.46), having a private pit latrine compared with a shared pit latrine (RR 0.79, 95% CI 0.64–0.97), and straining drinking water through cloth (RR 1.23, 95% CI 1.04–1.46) (S5 Table). Factors associated with CRB colonization were tending livestock or poultry (RR 4.08, 95% CI 2.09–7.94), storing water in a container with a wide opening compared with a narrow opening (RR 0.33, 95% CI 0.12–0.95), and being underweight (RR 4.64, 95% CI 1.92–11.2).
Among hospital exposures, no variables were associated with post-delivery maternal ESBL-PB colonization at a p < 0.2 cutoff, so no multivariable model was created. Factors associated with post-delivery maternal CRB colonization included undergoing C-section (RR 1.31, 95% CI 1.08–1.59) and experiencing complications at the time of delivery (RR 1.13, 95% CI 1.03–1.24) (Table 5). Because duration of hospitalization was collinear with type of delivery, it was not included in the multivariable analysis. Similarly, antibiotics administered to mothers before delivery was also collinear with type of delivery and was thus excluded from multivariable analysis. We did not control for colonization pre-delivery as most mothers with CRB colonization post-delivery did not have colonization pre-delivery.
Newborn ESBL-PB colonization was also associated with C-section (RR 1.34, 95% CI 1.09–1.64) and maternal pre-delivery CRB colonization (RR 1.15, 95% CI 1.09–1.21). The only factor associated with newborn CRB colonization at a p < 0.2 cutoff was delivery by C-section (RR 1.73, 95% CI 1.20–2.47) (S7 Table). Although not included in the multivariate analysis, newborn CRB colonization was significantly associated with maternal post-delivery CRB colonization (RR 2.45, 95% CI 1.25–4.77). No association was found with maternal post-delivery ESBL-PB colonization.
Discussion
This study revealed a high prevalence of perinatal colonization with ESBL-PB and CRB among mothers and newborns undergoing facility-based deliveries at a tertiary care hospital in Bangladesh. Colonization prevalence was substantially higher in mothers at the time of discharge compared with admission, particularly for CRB. The less notable changes in ESBL-PB colonization may be attributable to the frequent ESBL-PB colonization on admission. Additionally, there were concurrently high rates of C-sections and frequent prescribing of prolonged courses of prophylactic antibiotics.
Newborn colonization prevalence more closely resembled maternal colonization at discharge compared with admission and occurred within the context of widespread environmental contamination. A similarly high prevalence of ESBL-PB colonization in newborns has been reported from studies in India, Cambodia, Madagascar, and Tanzania, though CRB colonization was infrequent [24,25,26,27]. Another study from Bangladesh revealed that 82% of healthy infants were colonized with Escherichia coli resistant to third-generation cephalosporins [28]. Much lower neonatal AMR colonization rates have been reported in high-income countries such as Israel and Sweden where ESBL-PB colonization ranged from 5 to 14% [29, 30]. This may reflect differences in local epidemiology as well as facility-based practices. This study has revealed one of the highest reported prevalences of CRB colonization among newborns, which is particularly concerning given the lack of effective treatment options for infections with these organisms. It is likely these organisms are leading to infections given studies showing high levels of CRBs causing neonatal sepsis in Bangladesh [12]. Furthermore, the remarkably high prevalence of CRB colonization occurred despite no reported use of carbapenem antibiotics, demonstrating that other beta-lactam antibiotics may be promoting CRB colonization [31, 32].
This particular hospital is a tertiary care facility where many high-risk pregnancies are referred, which may partially explain the high rates of C-sections. However, this also reflects national trends in Bangladesh. In 2018, one-third of deliveries occurred by C-section, including 67% of facility-based deliveries [33]. This is well above the 10–15% recommendation by WHO for rates of C-section [34]. The WHO threshold is based on a review of data demonstrating no improvement in perinatal mortality for higher rates of C-section [35]. This trend of increasing C-sections is growing fastest in LMICs [36]. Rather than reflecting improved global access to a life-saving procedure, the disparities in rates of C-sections – from 5% in sub-Saharan Africa to 43% in Latin America and the Caribbean – reveal ongoing incongruencies and inappropriate surgical stewardship. By 2030, nearly a third of all deliveries globally are expected to occur by C-section, with the vast majority (nearly 90%) occurring in LMICs [36].
Along with frequent C-sections, perinatal antibiotic use was high among participants. Despite WHO guidance recommending only a single dose of pre-operative prophylactic antibiotics for C-sections, most participants who underwent C-section were advised to complete prolonged courses of antibiotics [37]. Moreover, the WHO guidance emphasizes the use of narrow-spectrum antibiotics for prophylaxis. Reports from India demonstrate prolonged courses of prophylactic antibiotics being given to 80% of women undergoing C-sections, including frequent use of three-drug regimens [38]. A study from China revealed that 100% of women who underwent C-sections received a standard seven-day antibiotic regimen [39]. Similar practices have been reported from other LMICs, indicating the use of prolonged prophylactic antibiotics for C-sections may be widespread, despite evidence showing no benefit from multiple doses of antibiotics [40,41,42,43]. This contrasts with practices in high-resource contexts, such as the U.S., where multiple doses of antibiotics are rare [44, 45].
Although the analysis conducted here was exploratory, prior hospitalization was consistently associated with increased risk for maternal ESBL-PB/CRB colonization, implicating the role of healthcare settings in the propagation of AMR. Additionally, there was an association between preterm delivery and maternal vaginal ESBL-PB colonization. This suggests that the vaginal microbiome may be having an effect on preterm delivery, which has been previously demonstrated [46, 47]. It remains unclear what the mechanism is for how colonization with resistant organisms modulates preterm delivery. However, it has been proposed that antibiotic resistant bacteria may be associated with more inflammation and perhaps reflective of dysbiosis [48, 49]. Further studies are needed to characterize this potential dynamic.
Animal contact appears to be connected with colonization. Duck rearing was associated with increased pre-delivery maternal CRB colonization risk, though the relatively low number of participants with this exposure likely resulted in it not being statistically significant. Similarly, tending livestock or poultry was associated with pre-delivery ESBL-PB and CRB colonization in bivariate analysis but was not included in the multivariate analysis because so few participants had this exposure. The only other significant association with animals was an apparent protective effect of goats outside the house. These findings may warrant further investigation into the One Health processes that could be contributing to AMR propagation and dissemination.
C-section was associated with post-delivery maternal CRB colonization as well as newborn ESBL-PB/CRB colonization. Other factors commonly associated with AMR such as length of hospital stay and antibiotic administration could not be included in the multivariate analyses because these were collinear with mode of delivery. This is consistent with another study in a low-resource context examining associations with neonatal AMR colonization that found aspects of the healthcare setting to be the most highly associated factors, including antibiotic use, longer hospital stays, prematurity, and lower staffing ratios [50]. Additionally, C-sections have been shown to lead to a disrupted colonizing microbiota among neonates [51,52,53], which may be exacerbated by antibiotic use [54]. Even when the antibiotics are only administered to the mother, studies have demonstrated negative health outcomes in the newborn, including necrotizing enterocolitis [55], neonatal sepsis [56], and growth stunting [54]. Further, the magnitude of disruption on the neonatal microbiome attributable to intrapartum antibiotics administered to mothers has been found to be similar to postnatal antibiotics administered to newborns directly [57]. Thus, ESBL-PB and/or CRB colonization may be a marker of dysbiosis, induced by upstream factors such as antibiotic exposure that provide an opportunity for colonization with resistant bacteria [49, 58]. Accordingly, fecal microbiota transplantation has been tried as a successful strategy for restoring the microbiota in neonates born by C-section [59]. In this study, the impact of maternal antibiotic use on newborn colonization could not be assessed since nearly all women received perinatal antibiotics, with the majority of antibiotic courses started prior to delivery.
While there are likely many aspects of the healthcare setting contributing to ESBL-PB/CRB colonization, both antibiotic use and C-section rates are potentially modifiable. Apart from contributing to AMR, unnecessary C-sections may have additional negative health ramifications, such as surgical site infections, blood clots, or injury to other organs. A review of indications for C-sections in Bangladesh found that the majority were not performed out of medical necessity [60]. This is a clear area for ongoing surveillance and changes to current practices.
Overuse of antibiotics is a known driver of AMR. The prolonged antibiotic courses received by the majority of mothers for the purposes of prophylaxis pose a threat to community rates of AMR through direct and indirect effects on resistance [61]. The situation in the delivery ward is unlikely to be unique in Bangladesh given high levels of antibiotic resistance reported across a variety of settings [62, 63]. Reasons for liberal antibiotic use in Bangladesh include lack of understanding of antibiotic function, low awareness of antibiotic resistance, overemphasis on use of antibiotics for prevention, and a perception of antibiotics as a symbol of power [64]. Additionally, this tertiary care facility does not have a functioning microbiology laboratory or infectious disease consultant, limiting the ability to select appropriate antibiotics based on antibiograms or culture results or seek expert consultation.
The high level of antibiotic use for prophylaxis also points to a heightened concern for healthcare-associated infections (HAI) [65]. Hospital-acquired neonatal infections are up to 20 times more common in LMICs compared with high-income contexts [66]. Accordingly, Zaidi, et al. note in the context of LMICs, any newborn infection in a hospital-born baby should be considered a HAI, regardless of the timing of onset [66]. In LMICs such as Bangladesh, antibiotics are a readily-available tool to mitigate HAIs, certainly more accessible than infrastructure changes to improve hygiene and sanitation or even incentives for hospital workers to prioritize cleanliness. In this scenario, antibiotics are likely acting both as a substitute for and an extension of infection prevention and control efforts [20]. In fact, a prior study from Bangladesh demonstrated that antibiotics given to patients on admission resulted in less hospital-onset diarrhea resulting from contaminated food [67].
Simultaneous recovery of abundant ESBL-PB/CRB from the hospital environment further suggests that the environment is likely contributing to AMR transmission. This has been corroborated by other studies in similar contexts that have shown that surface colonization predicts infecting organisms in neonates [68, 69]. Antibiotic-resistant Klebsiella pneumoniae strains isolated from newborns hospitalized in a neonatal intensive care unit were found to be genetically closely related to strains isolated from other infants on the ward, supporting the notion of transmission being driven by healthcare workers and/or shared equipment [50]. Another study found that while K. pneumoniae transmission to newborns appears to be driven by direct contact with colonized healthcare workers, spread of E. coli and Enterobacter cloacae are mediated through indirect contamination [25]. Further supporting the linkage between exposure to the healthcare environment and ESBL-PB/CRB colonization is the increased environmental contamination during COVID-19 and concomitant increase in neonatal AMR colonization. Increased environmental contamination during COVID-19 may have resulted from decreased routine cleaning by staff who were concerned about heightened exposure to SARS-CoV-2 in the hospital setting. This supports the need for enhanced environmental cleaning and infection prevention efforts to reduce HAIs and AMR.
Some of the strengths of this study are that it employs a relatively low-cost method of AMR surveillance that could be replicated in other low-resource contexts [70]. It also uses colonization to detect AMR burden and transmission, allowing for the implementation of directed preventive measures in advance of infectious outcomes [70]. Further, the examination of both community and hospital-related factors and the measurement of colonization at two time points allows for better triangulation of the most important risk factors for AMR colonization in the same population across both settings.
This study has several limitations. The homogeneity of participants’ community and hospital exposures that we hypothesized to have strong associations with AMR colonization meant that the associations between some factors and ESBL-PB/CRB colonization could not be evaluated. However, the descriptive characteristics provide insight on common practices that may be implicated in AMR transmission, such as abundant antibiotic use. Additionally, we relied on the results of chromogenic agars for classifying ESBL-PB/CRB colonization. Prior studies using similar specimen types have reported 98–100% sensitivity for the ESBL agar and 93–100% for the mSuperCARBA agar but with lower specificities (72–100%) [71,72,73,74]. However, these studies were specifically assessing the performance of the agars for identifying ESBL-producing or carbapenemase-producing Enterobacterales. This contrasts with the objectives of this study, which were not limited only to Enterobacterales or to production of specific resistance determinants but to all Gram-negative isolates with the resistant phenotypes of interest. Moreover, we did not use the chromogenic findings as a means of definitive identification, and instead highlighted the relative changes between pre- and post-delivery as comparable and informative indicators of underlying trends.
Furthermore, we only measured colonization status, which does not in itself carry negative health consequences and may rapidly change after returning to the home environment. Yet, other studies have shown that neonatal colonization patterns can persist for up to five years, with greater persistence of more virulent bacterial strains [29, 75]. A meta-analysis examining the relationship between Gram-negative bacterial colonization and bloodstream infections in neonates did not find a statistically significant correlation, though the analysis was limited by a small number of studies to draw from and high heterogeneity between studies [6]. However, subsequent studies and other studies not included in the meta-analysis have supported the role of intestinal colonization as a predisposing factor to infection [24, 27, 68, 76].
Our findings do not prove that the environment was the source of ESBL-PB/CRB colonization among mothers and neonates as we lack bacterial characterization data. Regardless, the remarkable abundance of ESBL-PB/CRB throughout the hospital environment suggests this is likely to be a factor in at least some of the transmission pathways. Future studies including whole genome sequencing-based characterization of isolates would add further clarity to transmission dynamics and AMR diversity in this setting.
Conclusion
The scenario of rising AMR among newborns is becoming increasingly common across LMICs and demands a close examination of the factors surrounding hospital-based deliveries, including indications for C-sections and antibiotic administration. The findings of this study highlight the need to avoid overmedicalization of deliveries. Pregnant women presenting to a hospital for delivery may be more likely to be construed as “patients in need of treatment”. Separating routine perinatal care from a healthcare facility to an adjacent birthing center may help decrease the treatment imperative. Conducting randomized controlled trials demonstrating the non-inferiority of reduced antibiotic use could further support changes in antibiotic prescribing. However, this may not be supported without concomitant improvements in infection prevention and control – with an emphasis on environmental cleaning – coupled with enhanced access to diagnostics and microbiologic laboratory capacity. Unnecessary C-sections must also be curtailed to reduce the disruption of the newborn microflora and associated morbidity. Interventions to reduce C-sections could focus on understanding and dismantling the incentives driving increasing rates of C-sections. Overall, these findings demonstrate the urgent and pressing need for better AMR surveillance and associated interventions to ensure safer birthing environments.
Data availability
All data generated or analyzed during this study are included within the article and its supplementary information files.
Abbreviations
- AMR:
-
Antimicrobial resistance
- COVID-19 (COVID):
-
Coronavirus infectious disease 2019
- CRB:
-
Carbapenem resistant bacteria
- C-section:
-
Cesarean delivery
- ESBL-PB:
-
Extended-spectrum beta-lactamase producing bacteria
- HAI:
-
Healthcare-associated infection
- ICU:
-
Intensive care unit
- LMIC:
-
Low- and middle-income countries
References
Review on Antimicrobial Resistance. Tackling drug-resistant infections globally: Final report and recommendations. 2016.
Murray CJL, Ikuta KS, Sharara F, Swetschinski L, Robles Aguilar G, Gray A, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022. https://doi.org/10.1016/S0140-6736(21)02724-0.
Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A. 2010;107:11971–5.
Chu DM, Ma J, Prince AL, Antony KM, Seferovic MD, Aagaard KM. Maturation of the infant microbiome community structure and function across multiple body sites and in relation to mode of delivery. Nat Med. 2017;23:314–26.
Chan GJ, Lee ACC, Baqui AH, Tan J, Black RE. Risk of early-onset neonatal infection with maternal infection or colonization: a global systematic review and meta-analysis. PLoS Med. 2013;10:e1001502.
Folgori L, Tersigni C, Hsia Y, Kortsalioudaki C, Heath P, Sharland M, et al. The relationship between Gram-negative colonization and bloodstream infections in neonates: a systematic review and meta-analysis. Clin Microbiol Infect. 2018;24:251–7.
Nurjadi D, Eichel VM, Tabatabai P, Klein S, Last K, Mutters NT, et al. Surveillance for colonization, transmission, and infection with Methicillin-Susceptible Staphylococcus aureus in a neonatal Intensive Care Unit. JAMA Netw Open. 2021;4:e2124938.
Investigators of the Delhi Neonatal Infection Study (DeNIS) collaboration. Characterisation and antimicrobial resistance of sepsis pathogens in neonates born in tertiary care centres in Delhi, India: a cohort study. Lancet Glob Health. 2016;4:e752–60.
Laxminarayan R, Matsoso P, Pant S, Brower C, Røttingen JA, Klugman K, et al. Access to effective antimicrobials: a worldwide challenge. Lancet. 2016;387:168–75.
Chaurasia S, Sivanandan S, Agarwal R, Ellis S, Sharland M, Sankar MJ. Neonatal sepsis in South Asia: huge burden and spiralling antimicrobial resistance. BMJ. 2019;364:k5314.
Okomo U, Akpalu ENK, Le Doare K, Roca A, Cousens S, Jarde A, et al. Aetiology of invasive bacterial infection and antimicrobial resistance in neonates in sub-saharan Africa: a systematic review and meta-analysis in line with the STROBE-NI reporting guidelines. Lancet Infect Dis. 2019. https://doi.org/10.1016/S1473-3099(19)30414-1.
Li G, Bielicki JA, Ahmed ASMNU, Islam MS, Berezin EN, Gallacci CB, et al. Towards understanding global patterns of antimicrobial use and resistance in neonatal sepsis: insights from the NeoAMR network. Arch Dis Child. 2020;105:26–31.
Zaidi AK, Thaver D, Ali SA, Khan TA. Pathogens associated with sepsis in newborns and young infants in developing countries. Pediatr Infect Dis J. 2009;28:10–8.
Jajoo M, Manchanda V, Chaurasia S, Sankar MJ, Gautam H, Agarwal R, et al. Alarming rates of antimicrobial resistance and fungal sepsis in outborn neonates in North India. PLoS ONE. 2018;13:e0180705.
Ghafoor T, Hussanain A, Qureshi MM, Mehmood T, Ali L. Antimicrobial susceptibility pattern of blood culture isolates from patients with suspected neonatal sepsis in a tertiary care hospital in Pakistan. Sri Lankan J Infect Dis. 2020;10:30.
Le NK, Hf W, Vu PD, Khu DTK, Le HT, Hoang BTN, et al. High prevalence of hospital-acquired infections caused by gram-negative carbapenem resistant strains in Vietnamese pediatric ICUs: a multi-centre point prevalence survey. Medicine. 2016;95:e4099.
Struelens MJ. The epidemiology of antimicrobial resistance in hospital acquired infections: problems and possible solutions. BMJ. 1998;317:652–4.
Fischer MM, Bild M. Hospital use of antibiotics as the main driver of infections with antibiotic-resistant bacteria– a reanalysis of recent data from the European Union. bioRxiv. 2019:553537. https://doi.org/10.1101/553537.
Pearson M, Doble A, Glogowski R, Ibezim S, Lazenby T, Haile-Redai A et al. Antibiotic prescribing and resistance: Views from low- and middle-income prescribing and dispensing professionals. World Health Organization; 2018. Available: https://www.who.int/antimicrobial-resistance/LSHTM-Antibiotic-Prescribing-LMIC-Prescribing-and-Dispensing-2017.pdf.
Willis LD, Chandler C. Quick fix for care, productivity, hygiene and inequality: reframing the entrenched problem of antibiotic overuse. BMJ Global Health. 2019;e001590. https://doi.org/10.1136/bmjgh-2019-001590.
Baier C, Pirr S, Ziesing S, Ebadi E, Hansen G, Bohnhorst B, et al. Prospective surveillance of bacterial colonization and primary sepsis: findings of a tertiary neonatal intensive and intermediate care unit. J Hosp Infect. 2019;102:325–31.
Graham PL, Della-Latta P, Wu F, Zhou J, Saiman L. The gastrointestinal tract serves as the reservoir for Gram-negative pathogens in very low birth weight infants. Pediatr Infect Dis J. 2007;26:1153–6.
Goldmanln DA. Bacterial colonization and infection in the neonate. Am J Med. 1981;70:417–22.
Smith A, Anandan S, Veeraraghavan B, Thomas N. Colonization of the Preterm neonatal gut with Carbapenem-resistant Enterobacteriaceae and its Association with neonatal Sepsis and Maternal Gut Flora. J Glob Infect Dis. 2020;12:101–4.
Bonneault M, Andrianoelina VH, Herindrainy P, Rabenandrasana MAN, Garin B, Breurec S, et al. Transmission routes of extended-spectrum beta-lactamase-producing Enterobacteriaceae in a Neonatology Ward in Madagascar. Am J Trop Med Hyg. 2019;100:1355–62.
Silago V, Kovacs D, Msanga DR, Seni J, Matthews L, Oravcová K, et al. Bacteremia in critical care units at Bugando Medical Centre, Mwanza, Tanzania: the role of colonization and contaminated cots and mothers’ hands in cross-transmission of multidrug resistant gram-negative bacteria. Antimicrob Resist Infect Control. 2020;9:58.
Turner P, Pol S, Soeng S, Sar P, Neou L, Chea P, et al. High prevalence of antimicrobial-resistant Gram-negative colonization in hospitalized Cambodian infants. Pediatr Infect Dis J. 2016;35:856–61.
Islam MA, Amin MB, Roy S, Asaduzzaman M, Islam MR, Navab-Daneshmand T, et al. Fecal colonization with Multidrug-Resistant E. Coli among healthy infants in Rural Bangladesh. Front Microbiol. 2019;10:640.
Nordberg V, Jonsson K, Giske CG, Iversen A, Aspevall O, Jonsson B, et al. Neonatal intestinal colonization with extended-spectrum β-lactamase-producing Enterobacteriaceae-a 5-year follow-up study. Clin Microbiol Infect. 2018;24:1004–9.
Leikin-Zach V, Shany E, Yitshak-Sade M, Eshel R, Shafat T, Borer A, et al. Neonatal risk factors for colonization with extended-spectrum beta-lactamase-producing Bacteria in the neonatal Intensive Care Unit. Isr Med Assoc J. 2018;20:286–90.
Kritsotakis EI, Tsioutis C, Roumbelaki M, Christidou A, Gikas A. Antibiotic use and the risk of carbapenem-resistant extended-spectrum-{beta}-lactamase-producing Klebsiella pneumoniae infection in hospitalized patients: results of a double case-control study. J Antimicrob Chemother. 2011;66:1383–91.
Wang Q, Zhang Y, Yao X, Xian H, Liu Y, Li H, et al. Risk factors and clinical outcomes for carbapenem-resistant Enterobacteriaceae nosocomial infections. Eur J Clin Microbiol Infect Dis. 2016;35:1679–89.
Bangladesh Demographic and Health Survey 2017-18: Key Indicators. National Institute of Population Research and Training; 2019 Nov. Available: https://dhsprogram.com/pubs/pdf/PR104/PR104.pdf.
WHO statement on caesarean section rates. World Health Organization; 2015 Apr. Available: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/cs-statement/en/.
Betran AP, Torloni MR, Zhang J, Ye J, Mikolajczyk R, Deneux-Tharaux C, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 2015;12:57.
Betran AP, Ye J, Moller A-B, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health. 2021;6. https://doi.org/10.1136/bmjgh-2021-005671.
WHO recommendation on prophylactic antibiotics for women undergoing caesarean section. Geneva: WHO; 2021 Jun. Available: https://apps.who.int/iris/bitstream/handle/10665/341865/9789240028012-eng.pdf.
Mishra S, Raheja A, Agarwal K, Gandhi G. Antibiotic prophylaxis in cesarean sections: a tertiary care hospital based survey. Int J Reprod Contracept Obstet Gynecol. 2021;10:2221–4.
Liu R, Lin L, Wang D. Antimicrobial prophylaxis in caesarean section delivery. Exp Ther Med. 2016;12:961–4.
Dohou AM, Buda VO, Yemoa LA, Anagonou S, Van Bambeke F, Van Hees T, et al. Antibiotic usage in patients having undergone caesarean section: a three-level study in Benin. Antibiot (Basel). 2022;11. https://doi.org/10.3390/antibiotics11050617.
Carshon-Marsh R, Squire JS, Kamara KN, Sargsyan A, Delamou A, Camara BS, et al. Incidence of Surgical Site infection and use of antibiotics among patients who underwent caesarean section and herniorrhaphy at a Regional Referral Hospital, Sierra Leone. Int J Environ Res Public Health. 2022;19. https://doi.org/10.3390/ijerph19074048.
Pobee F. Single versus multiple doses antibiotic prophylaxis for elective caesarean section at the Korle Bu Teaching Hospital. 2022. https://doi.org/10.21203/rs.3.rs-1396754/v1.
Huang Y, Yin X, Wang X, Zhou F, Cao X, Han Y, et al. Is a single dose of commonly used antibiotics effective in preventing maternal infection after cesarean section? A network meta-analysis. PLoS ONE. 2022;17:e0264438.
Argani C, Notis E, Moseley R, Huber K, Lifchez S, Price LA, et al. Survey of cesarean delivery infection prevention practices across US academic centers. Infect Control Hosp Epidemiol. 2015;36:1245–7.
Reiff ES, Habib AS, Carvalho B, Raghunathan K. Antibiotic Prophylaxis for Cesarean Delivery: a Survey of anesthesiologists. Anesthesiol Res Pract. 2020;2020:3741608.
DiGiulio DB, Callahan BJ, McMurdie PJ, Costello EK, Lyell DJ, Robaczewska A, et al. Temporal and spatial variation of the human microbiota during pregnancy. Proc Natl Acad Sci U S A. 2015;112:11060–5.
Callahan BJ, DiGiulio DB, Goltsman DSA, Sun CL, Costello EK, Jeganathan P, et al. Replication and refinement of a vaginal microbial signature of preterm birth in two racially distinct cohorts of US women. Proc Natl Acad Sci U S A. 2017;114:9966–71.
Wolf AJ, Liu GY, Underhill DM. Inflammatory properties of antibiotic-treated bacteria. J Leukoc Biol. 2017;101:127–34.
Korach-Rechtman H, Hreish M, Fried C, Gerassy-Vainberg S, Azzam ZS, Kashi Y, et al. Intestinal dysbiosis in carriers of Carbapenem-Resistant Enterobacteriaceae. mSphere. 2020;5. https://doi.org/10.1128/mSphere.00173-20.
Crellen T, Turner P, Pol S, Baker S, Nguyen Thi Nguyen T, Stoesser N, et al. Transmission dynamics and control of multidrug-resistant Klebsiella pneumoniae in neonates in a developing country. Elife. 2019;8. https://doi.org/10.7554/eLife.50468.
Bäckhed F, Roswall J, Peng Y, Feng Q, Jia H, Kovatcheva-Datchary P, et al. Dynamics and stabilization of the human gut microbiome during the First Year of Life. Cell Host Microbe. 2015;17:690–703.
Korpela K, Costea P, Coelho LP, Kandels-Lewis S, Willemsen G, Boomsma DI, et al. Selective maternal seeding and environment shape the human gut microbiome. Genome Res. 2018;28:561–8.
Korpela K. Impact of Delivery Mode on Infant Gut Microbiota. Ann Nutr Metab. 2021:1–9.
Uzan-Yulzari A, Turta O, Belogolovski A, Ziv O, Kunz C, Perschbacher S, et al. Neonatal antibiotic exposure impairs child growth during the first six years of life by perturbing intestinal microbial colonization. Nat Commun. 2021;12:443.
Silverman MA, Konnikova L, Gerber JS. Impact of antibiotics on necrotizing enterocolitis and Antibiotic-Associated Diarrhea. Gastroenterol Clin North Am. 2017;46:61–76.
Zhou P, Zhou Y, Liu B, Jin Z, Zhuang X, Dai W, et al. Perinatal antibiotic exposure affects the transmission between maternal and neonatal microbiota and is Associated with Early-Onset Sepsis. mSphere. 2020;5. https://doi.org/10.1128/mSphere.00984-19.
Tapiainen T, Koivusaari P, Brinkac L, Lorenzi HA, Salo J, Renko M, et al. Impact of intrapartum and postnatal antibiotics on the gut microbiome and emergence of antimicrobial resistance in infants. Sci Rep. 2019;9:10635.
Goldmann DA, Leclair J, Macone A. Bacterial colonization of neonates admitted to an intensive care environment. J Pediatr. 1978;93:288–93.
Korpela K, Helve O, Kolho K-L, Saisto T, Skogberg K, Dikareva E, et al. Maternal fecal microbiota transplantation in Cesarean-Born infants rapidly restores normal gut Microbial Development: a proof-of-Concept Study. Cell. 2020;183:324–334e5.
Begum T, Rahman A, Nababan H, Hoque DME, Khan AF, Ali T, et al. Indications and determinants of caesarean section delivery: evidence from a population-based study in Matlab, Bangladesh. PLoS ONE. 2017;12:e0188074.
Lipsitch M, Samore MH. Antimicrobial use and antimicrobial resistance: a population perspective. Emerg Infect Dis. 2002;8:347–54.
Ahmed I, Rabbi MB, Sultana S. Antibiotic resistance in Bangladesh: a systematic review. Int J Infect Dis. 2019;80:54–61.
Safain KS, Bhuyan GS, Tasnim S, Hasib SH, Sultana R, Islam MS et al. Situation of antibiotic resistance in Bangladesh and its association with resistance genes for horizontal transfer. bioRxiv. 2020. pp. 2020.04.06.027391. doi:10.1101/2020.04.06.027391.
Nahar P, Unicomb L, Lucas PJ, Uddin MR, Islam MA, Nizame FA, et al. What contributes to inappropriate antibiotic dispensing among qualified and unqualified healthcare providers in Bangladesh? A qualitative study. BMC Health Serv Res. 2020;20:656.
Kumar S, Shankar B, Arya S, Deb M, Chellani H. Healthcare associated infections in neonatal intensive care unit and its correlation with environmental surveillance. J Infect Public Health. 2018;11:275–9.
Zaidi AK, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, Goldmann DA. Hospital-acquired neonatal infections in developing countries. Lancet. 2005;365:1175–88.
Bhuiyan MU, Luby SP, Zaman RU, Rahman MW, Sharker MAY, Hossain MJ, et al. Incidence of and risk factors for hospital-acquired diarrhea in three tertiary care public hospitals in Bangladesh. Am J Trop Med Hyg. 2014;91:165–72.
Dias M, Saleem J. Surface colonization and subsequent development of infections with multi drug resistant organisms in a neonatal intensive care unit. Ann Clin Microbiol Antimicrob. 2019;18:12.
Reich P, Boyle M, Sullivan M, Hogan PG, Thompson R, Muenks C, et al. Familial and environmental impact on colonization with antibiotic-resistant organisms in the neonatal Intensive Care Unit. Open Forum Infect Dis. 2017;4:685–S685.
Vurayai M, Strysko J, Kgomanyane K, Bayani O, Mokomane M, Machiya T, et al. Characterizing the bioburden of ESBL-producing organisms in a neonatal unit using chromogenic culture media: a feasible and efficient environmental sampling method. Antimicrob Resist Infect Control. 2022;11:14.
Grohs P, Tillecovidin B, Caumont-Prim A, Carbonnelle E, Day N, Podglajen I, et al. Comparison of five media for detection of extended-spectrum beta-lactamase by use of the wasp instrument for automated specimen processing. J Clin Microbiol. 2013;51:2713–6.
Saito R, Koyano S, Nagai R, Okamura N, Moriya K, Koike K. Evaluation of a chromogenic agar medium for the detection of extended-spectrum ß-lactamase-producing Enterobacteriaceae. Lett Appl Microbiol. 2010;51:704–6.
García-Fernández S, Hernández-García M, Valverde A, Ruiz-Garbajosa P, Morosini MI, Cantón R. CHROMagar mSuperCARBA performance in carbapenem-resistant Enterobacteriaceae isolates characterized at molecular level and routine surveillance rectal swab specimens. Diagn Microbiol Infect Dis. 2017;87:207–9.
Soria Segarra C, Larrea Vera G, Berrezueta Jara M, Arévalo Mendez M, Cujilema P, Serrano Lino M, et al. Utility of CHROMagar mSuperCARBA for surveillance cultures of carbapenemase-producing Enterobacteriaceae. New Microbes New Infect. 2018;26:42–8.
Nowrouzian FL, Oswald E. Escherichia coli strains with the capacity for long-term persistence in the bowel microbiota carry the potentially genotoxic pks island. Microb Pathog. 2012;53:180–2.
Basu S. Neonatal sepsis: the gut connection. Eur J Clin Microbiol Infect Dis. 2015;34:215–22.
Acknowledgements
We are grateful to all the participants of this study for providing consent to collect samples and invaluable information in a crucial time during their labor as well as post-natal period. We extend our gratitude to the colleagues at the Department of Pediatrics and Department of Obstetrics and Gynaecology at Bangabandhu Sheikh Mujib Medical College Hospital (BSMMCH), Faridpur, Bangladesh, for their extensive support in data collection and sample processing efforts. icddr,b acknowledges with gratitude the Governments of Bangladesh, Canada, Sweden, and the UK for providing core/unrestricted support.
Funding
Funding was provided by NIH FIC Global Health Equity Scholars D43 TW010540 as well as the Thrasher Research Fund (award #15188). The funders had no role in the study design, interpretation of results, or decision to publish.
Author information
Authors and Affiliations
Contributions
AS designed the study protocol, conducted data analyses, and drafted the manuscript. AP, DZ, MBA, MAI, ESG, and SL contributed to the conceptual design of the study and interpretation of results and provided substantial edits to the manuscript. MBA, KIH, MIH, SRS conducted the microbiology methods. AA carried out participant enrollment and data collection. HP contributed substantially to the statistical analyses. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We obtained written informed consent from all adult study participants. Consent for newborn enrollment was provided by the parents and/or legal guardians. The study protocol was reviewed and approved by the IRB at Stanford University (protocol #53442) and the Research and Ethics Review Committees at icddr,b (protocol #PR-19119).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Styczynski, A., Amin, M.B., Hoque, K.I. et al. Perinatal colonization with extended-spectrum beta-lactamase-producing and carbapenem-resistant Gram-negative bacteria: a hospital-based cohort study. Antimicrob Resist Infect Control 13, 13 (2024). https://doi.org/10.1186/s13756-024-01366-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-024-01366-9