Abstract
Background
Elizabethkingia anophelis is a multi-drug resistant emerging opportunistic pathogen with a high mortality rate, causing healthcare-associated outbreaks worldwide.
Methods
We report a case of E. anophelis pleuritis, resulting from transmission through lung transplantation, followed by a literature review of outbreak reports and strategies to minimize E. anophelis transmission in healthcare settings.
Results
From 1990 to August 2022, 14 confirmed E. anophelis outbreak cohorts and 21 cohorts with suspected E. anophelis outbreaks were reported in literature. A total of 80 scientific reports with recommendations on diagnostics and infection control measures were included and summarized in our study.
Conclusion
Strategies to prevent and reduce spread of E. anophelis include water-free patient rooms, adequate hygiene and disinfection practices, and optimized diagnostic techniques for screening, identification and molecular typing.
Similar content being viewed by others
Background
Elizabethkingia anophelis is an emerging opportunistic pathogen that has caused several outbreaks in hospitals and health-care facilities around the world in recent years [1,2,3,4,5,6]. As of today, the largest outbreak has been reported in the Midwestern United States, with a confirmed number of 65 infected patients, of which 20 people deceased. After this outbreak the CDC issued a nationwide alert, followed by a temporary nationwide obligation to report any Elizabethkingia species isolate to the CDC [7, 8].
The genus Elizabethkingia has first been described in 2005. Two former members of the Chryseobacterium genus, namely C. meningosepticum and C. miricola, were shown through 16 S rRNA gene sequencing to represent a separate lineage within the family Flavobacteriaceae and consequently renamed Elizabethkingia. [9] E. anophelis was first isolated from the midgut of the Anopheles gambiae mosquito in 2011 [10]. The new species E. endophytica was introduced in 2015, but soon after recognized as E. anophelis through whole genome sequencing (WGS) [11]. As of today there are six recognized species in the genus Elizabethkingia: E. meningoseptica, E. miricola, E. anophelis, E. bruuniana, E. ursingii and E. occulta [12, 13].
Members of the Elizabethkingia genus are aerobic gram-negative, non-motile rods. E. anophelis colonies are smooth, yellowish, translucent, and shiny. They are catalase- and oxidase positive. Unlike other Elizabethkingia species, E. anophelis does not grow on MacConkey agar [10]. As a result of inconsistent phenotypic characteristics between different species and misidentification using API/ID32 phenotyping, Phoenix 100 ID/AST, VITEK-2, and matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) systems, E. anophelis isolates have often been mistaken for E. meningoseptica. [14,15,16,17,18,19] Since 2017, MALDI-TOF MS systems are able to correctly identify E. anophelis isolates [20, 21].
Elizabethkingia anophelis has been implied as the causative pathogen in neonatal meningitis, (catheter-related) bacteremia and pneumonia, and are associated with high mortality rates ranging from 18% up to 70% [4, 5, 14, 22]. Treatment of infections with antimicrobial therapy is challenging: E. anophelis is a multidrug-resistant bacterium that harbors resistance genes against multiple antibiotic drug classes, such as beta-lactams including carbapenems, aminoglycosides, tetracyclines, fluoroquinolones, macrolide/lincosamide/streptogramins, glycopeptides, folate pathway inhibitors, rifampicin and chloramphenicol [2, 23,24,25]. Susceptibility rates are highest for minocycline (> 98%), followed by doxycycline (83–92%), piperacillin/tazobactam (27–92%), levofloxacin (16–79%) and trimethoprim-sulfamethoxazole (4–92%) [15, 20, 26]. Furthermore, this micro-organism is difficult to eradicate in the environment, as it can survive in chlorinated water [27]. The possibility of forming a strong biofilm contribute to the pathogenesis and resilience of this micro-organism [28].
Given the high mortality rates of infected patients, the limited therapeutic options and the probability of nosocomial outbreaks, E. anophelis is a bacterium of great concern. Optimization of detection methods and infection control measures are necessary to minimize future nosocomial outbreaks by E. anophelis. In this article we describe a case of E. anophelis pleuritis transmitted through bilateral lung transplantation, followed by a review of the literature on healthcare-associated E. anophelis outbreaks, and provide recommendations on infection prevention strategies and control measures based on the published scientific evidence and our own experience.
Case presentation
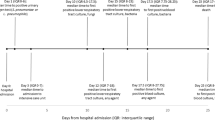
A 61-year-old man with severe pulmonary emphysema received a bilateral lung transplant from a non-heart-beating donor in July 2021. Inspection of the lungs including bronchoscopy during the procurement procedure did not show any irregularities. The lungs were transplanted to the patient without the need of extracorporeal circulation. The patient was extubated according to protocol after inspection by bronchoscopy on the first day after surgery.
Respiratory secretions obtained from the donor lung prior to transplantation and by bronchoscopy on the first day after transplantation initially only grew Haemophilus influenzae and methicillin-susceptible Staphylococcus aureus. On the fifth day after transplantation the right thoracic drain was removed and cultured on 5% sheep blood agar (BA) plates at 35˚C O2 for 48 h and on and MacConkey agar (MAC) plates at 35˚C CO2 for 48 h. Grey colonies were visible on BA, which were identified as E. anophelis by MALDI-TOF MS (MALDI Biotyper v9.0, Brucker Daltonics, Bremen, Germany). No growth was seen on MAC. The cultures were found to be positive for E. anophelis. 16 S- and SNP-based molecular analysis of the whole genome sequence of this isolate was performed as described previously, confirming the species determination of E. anophelis (Fig. 1) [29].
Antibiotic susceptibility was tested by gradient strips (Etest®; bioMérieux S.A., Marcy l’Etoile, France) on Mueller Hinton Agar, by broth microdilution test (Sensititer, Thermo Fisher Scientific, Waltham, MA,) and by automated susceptibility testing (BD Phoenix, Sparks, MD). The isolate was susceptible only to trimethoprim/sulfamethoxazole (1 mg/L), minocycline (0.25 mg/L) and doxycycline (1 mg/L) but resistant to all other drugs tested including ampicillin, amoxicillin/clavulanic acid, ceftriaxone, ceftazidime, cefepime, aztreonam, imipenem, amikacin, tobramycin, and colistin. Very major discrepancies were observed for ciprofloxacin and moxifloxacin between susceptibility methods. In such cases the result of broth microdilution was leading. The susceptibility pattern was consistent with existing literature [15, 16, 20]. Further information regarding susceptibility results can be found in Supplementary Table 1.
Because of the multidrug resistant nature of E. anophelis and its propensity for nosocomial spread, the patient was placed in contact isolation measures immediately after identifying the isolate. As part of source detection, frozen respiratory samples from the donor lung were thawed and cultured again, this time on Burkholderia cepacia selective agar (BCSA) containing gentamicin, vancomycin, and polymyxin B sulphate (Mediaproducts BV, Groningen, The Netherlands), revealing the presence of E. anophelis in two samples. These findings suggest that E. anophelis had been introduced via the donor lung, and most probably spread to the pleural cavity as a result of leakage or spill during surgery. Screening cultures of rectal swabs and throat swabs of three close contact patients using BCSA were negative. The hospital where the donor lungs were harvested was notified of our finding. Contact isolation precautions were maintained until three consecutive sputum samples were negative. These samples were collected during a second period of hospitalization two months after the last positive cultures, on three separate days with one day in between each day. The patient did not receive any antibiotic therapy when the follow-up samples were collected.
The patient was treated with a combination of trimethoprim/sulfamethoxazole 960 mg twice daily and minocycline 100 mg twice daily. Despite prompt treatment, there was an increase in CRP levels (up to 100 mg/L), leukocyte count (20.6*10^9/L) and pleural effusion in the second week after surgery. There was no fever. The inflammatory parameters slowly decreased after five days of antibiotic therapy. Nevertheless, cultures of the fluid from the second right thoracic drain remained positive until removal of the drain on day 16 post-transplantation. Culture of this drain tip also revealed E. anophelis. Antibiotic treatment with trimethoprim/sulfamethoxazole and minocycline was discontinued two weeks after all drains were removed. The patient was discharged in good condition on day 33 after surgery. Cultures were negative during two months follow up after transplantation.
Literature review
Search strategy and selection criteria
A literature search was performed on March 18, 2022 with the following search terms in Pubmed “(Elizabethkingia[title/abstract] OR Chryseobacterium[title/abstract])” (filters applied: English language, human studies), in Scopus “TITLE-ABS-KEY (elizabethkingia OR chryseobacterium) AND (LIMIT-TO (SUBJAREA, “MEDI”)) AND (LIMIT-TO (LANGUAGE, “English”) AND (LIMIT-TO (EXACTKEYWORD, “Human”))”, and in Embase “(((elizabethkingia:ab,ti OR chryseobacterium:ab,ti) AND english:la) AND ‘human’/de)”. On August 12, 2022 an additional search was performed to include studies that were missed in the first search. The following search terms were used: “(elizabethkingia[title/abstract] OR “chryseobacterium meningosepticum“[title/abstract])” in Pubmed, “TITLE-ABS-KEY (elizabethkingia OR “chryseobacterium meningosepticum”) AND (LIMIT-TO (SUBJAREA, “MEDI”)) AND (LIMIT-TO (LANGUAGE, “English”))” in Scopus, and “Elizabethkingia:ab,ti OR ‘Chryseobacterium meningosepticum’:ab,ti” in Embase. Only full text articles describing outbreaks or recommendations for diagnostics or infection control were included in the final selection. Studies on E. anophelis identified by molecular methods or by MALDI-TOF MS after 2017 were included as confirmed outbreak cases. Molecular identification before 2017 is less reliable, since the 16 S rRNA of E. anophelis and E. meningoseptica are 99% similar, which have caused misidentified species in reference databases [30]. Elisabethkingia/Chryseobacterium species with no growth on MAC before 2017 were included as possible E. anophelis outbreak cases. Studies published prior to 1990 were excluded (Fig. 2).
Results
Up to March 2022, 20 studies with results from environmental culturing and/or genotyping (outbreak reports) were published related to 14 cohorts with confirmed E. anophelis cases (Table 1).
Additionally, there were 22 outbreak reports related to 21 patient cohorts in which the causative pathogen was probably E. anophelis. (Supplementary Table 2). Taken together, 35 outbreaks with E. anophelis have been reported from hospitals on all continents, and the majority of outbreaks were reported from Taiwan (n = 11), India (n = 5), and the United States (n = 5). The outbreaks by E. anophelis have taken place in both adult and pediatric wards or ICUs. Environmental surveillance was performed in 8 of 13 confirmed E. anophelis outbreaks (Table 2). In cohorts with positive environmental cultures, water points were most commonly identified as the source of the outbreak. Genotyping was performed in 13 of the 14 confirmed E. anophelis outbreak cohorts included in our review. All these studies reported clusters of isolates identified by molecular typing methods such as RAPD, rep-PCR, PFGE, and WGS (Table 3). The outbreak numbers in Tables 2 and 3 correspond with the outbreak numbers in Table 1.
Genetically related isolates were not always geographically related, and some completely identical isolates were found in different countries which implies a different route of transmission. For example, in one incident the international export of medical equipment contributed to the worldwide spread of E. anophelis through contaminated commercial SARS-CoV-2 swab kits [41].
Recommendations for infection prevention and outbreak control
In Table 4, we present a summary of recommendations for infection control and diagnostics to prevent and control E. anophelis outbreak along with the references that support the recommendations.
Prevention of outbreaks
The first set of recommendations focuses on the prevention of outbreaks. Water taps in patient rooms in general, and those with aerators in particular, have most commonly been identified as source of outbreaks. Infection control specialists should be counciled in the design of patient rooms. In high risk units like intensive cares, the use of wet points should be avoided as much as possible. If the use of water can not be avoided, the design should be in such a way that the risks of splashing and contaminating patients, bedding and towels, and medical equipment are minimized. The use of aerators should be avoided. In addition, taps should be flushed daily to avoid colonization of taps in biofilms. The periodical surveillance of watertaps for contamination is important to identify risks in an early stage. Tap water system contamination with gram-negative bacilli (GNB) is associated with patient colonization, and removal of sinks on ICU wards has been proven to reduce the colonization rate of patients with GNB [42, 43]. In a small experiment performed by Yung et al., acquisition of E. anophelis through hand washing with chlorhexidine soap and water from a contaminated water source has been proven [34]. It is therefore recommended to aim for water-free patient care, especially in vulnerable populations, and to focus on alcohol rub instead of hand washing with water and soap during hand hygiene procedures. In general, the colonization and infection of patients could be prevented by lowering antibiotic selective pressure through antibiotic stewardship. In populations with high risk of acquisition of highly resistant microorganisms due to increased antibiotic use such as in the ICU, it is recommended to screen patients for colonization with GNB in sputum, throat swabs and rectal swabs. It is recommended to collect antimicrobial resistance data including the E. anophelis prevalence in a national surveillance program. Such a database could be consulted when confronted with an unexpected finding. Since E. anophelis has scarcely been detected in other Dutch hospitals, there was no indication of an inter-hospital outbreak.
Outbreak control
In the second set of recommendations in Table 4, we focus on outbreak control. In outbreak management, it is important to conduct source investigation and contact tracing, including environmental cultures, water samples and testing of close contacts. Changes of care providers should be restricted until the source of the outbreak is found. In most of the clusters described in the literature, contaminated water points have been identified as the source of the outbreak. Such sources should be eliminated as soon as possible to control the outbreak. The contaminated water source can also be outside of the hospital: several outbreaks have been reported in Taiwan, possibly introduced into healthcare settings after the Formosa Fun Coast dust explosion where burn victims were cooled with pool water [44].
In addition to waterpoints, transmission through ERCP and mother-to-infant transmission have been described [45, 46]. Infections derived from donors have been identified in two patients who underwent transplantation of tendon-bone and ligament allografts. The likely cause of contamination was during the processing stage as the organism was found in the sink drains and traps in the clean processing rooms [47]. Unlike in our case, in other reported cases of Elizabethkingia spp. infections after solid organ transplantation the source or transmission route have never been identified [48].
In order to prevent donor-transmitted bacterial pneumonia, lung transplant recipients are treated with a broad-spectrum antibiotic, which is modified on the basis of cultures obtained from the donor lungs [49]. In our medical center we culture sputum from donor lungs on BA (ambient air, 35 °C, 48 h), CHOC and MAC (both 5% CO2, 35 °C, 48 h), and on Sabouraud agar with aztreonam and vancomycin (ambient air, 35 °C, 5 days and 28 °C, 4 weeks). With this screening protocol E. anophelis can easily be missed in the cultured flora on non-selective BA and CHOC. In order to be able to selectively detect E. anophelis, BCSA was shown useful.
Patients that are positive for E. anophelis should be placed within barrier precautions to prevent patient-to-patient transmission. In addition, the disinfection of the patient environment should be enhanced. Chlorine-disinfectants are reported to be insufficient against E. anophelis. [27, 39, 50] Disinfection with hydrogen peroxide-based agents has been recommended as an adjunctive measure [51]. In our hospital, we use hydrogen-peroxide based wipes (Incidin™ OxyWipe, Ecolab, The Netherlands) to disinfect small surfaces and equipment, and a hydrogen-peroxide based solution (Terralin© PAA, Schülke & Mayr, Germany) to disinfect larger contaminated patient areas.
Typing methods
To detect and characterize an outbreak, molecular typing should be performed. The typing results provide information if there is clonal transmission of a strain, or if multiple clones from potentially different sources are involved. For instance, the typing results of the largest described outbreak in an ICU in a hospital in South Korea which inclused 79 confirmed cases showed that there had been transmission of multiple different clones [35].
Typing results can be challenging to interpret. Cut-off values for typing are not well-established and range from 80 to 93% in PFGE in our literature search. For WGS there are no standardized cut-off points to identify clusters: in the study by Navon et al., < 60 SNPs was chosen as the cut-off value to discriminate isolates from each other [5]. Genetic distance is impacted by pre-existing diversity in the source host, plus the amount of SNPs that accumulates in the source and recipient hosts over time [52]. Since genomic instability is species-specific cutoff values cannot be extrapolated by default. To determine a cut-off value it is therefore essential to sequence a large collection of isolates, which is a challenge with infrequently cultured micro-organisms. Compared to PCR-based typing methods, genome sequencing has a greater discriminatory power and provides more information regarding the phylogeny [53]. Isolates belonging to the same PFGE patterns can have variable resistance profiles [54]. This could be either attributed to unreliable resistance profiling, or to insufficient discriminatory value of PFGE typing. The higher discriminatory power and transferability of data makes WGS the typing method of choice whenever possible.
Concluding remarks
The transmission described in this study did not lead to further transmission to contacts of the lung transplant recipient. We have notified the transplant coordinator on the positive E. anophelis cultures after the lung transplant, since other donated organs may also be contaminated. Because the privacy of donors is strictly protected, we have not been informed on positive cultures in other donated organs, or transmission in the institution of the donor. Unfortunately, the isolate obtained from the donor was no longer available for sequencing to confirm their clonality. Prior to this case E. anophelis was cultured only once in our medical center from a deep wound infection in April 2021. This isolate was still available and found not to be related using WGS analysis (42.067 single nucleotide difference, marked as UMCG 8831 in Fig. 1). Direct transmission from the organ donor to the recipient in our case is therefore the most likely transmission route. Several recommendations were already implemented in our medical center, reducing the likelihood of spread. For instance, our intensive care units are designed without water taps in patient areas. Extensive environmental screening was not performed because it was assumed that the E. anophelis was either community acquired or acquired in the donor hospital.
Conclusion
In conclusion, E. anophelis is a multi-drug resistant nosocomial pathogen, as demonstrated by the plentitude of healthcare-related outbreak reports. Surveillance and water management are important measures to prevent large outbreaks. Outbreak investigation should include contact investigations and environmental sampling using selective culturing agars, to find and eradicate a source. The most commonly detected sources of outbreaks were water taps with aerators, however, transmission from patient-to-patient, through contaminated medical equipment or donor tissue as in the presented case are also established routes. Isolates should be typed preferably by WGS to characterize outbreaks, identify clonal transmission and facilitate exchange of genetic data.
Data Availability
Sequencing data is available from the European Nucleotide Archive, Bioproject PRJEB61750.
Abbreviations
- BA:
-
Blood agar
- BCSA:
-
Burkholderia cepacia selective agar
- CHOC:
-
Chocolate agar
- GNB:
-
Gram negative bacilli
- ICU:
-
Intensive care unit
- MAC:
-
MacConkey agar
- MALDI-TOF:
-
MS Matrix-assisted laser desorption ionization time-of-flight mass spectrometry
- SNP:
-
Single nucleotide polymorphism
- SNV:
-
Single nucleotide variants
- WGS:
-
Whole genome sequencing
References
Janda JM, Lopez DL. Mini review: new pathogen profiles: Elizabethkingia anophelis. Diagn Microbiol Infect Dis. 2017;88:201–5.
Teo J, Tan SY-Y, Liu Y, Tay M, Ding Y, Li Y, et al. Comparative genomic analysis of Malaria Mosquito Vector-Associated Novel Pathogen Elizabethkingia anophelis. Genome Biol Evol. 2014;6:1158–65.
Perrin A, Larsonneur E, Nicholson AC, Edwards DJ, Gundlach KM, Whitney AM, et al. Evolutionary dynamics and genomic features of the Elizabethkingia anophelis 2015 to 2016 Wisconsin outbreak strain. Nat Commun. 2017;8:15483.
Figueroa Castro CE, Johnson C, Williams M, VanDerSlik A, Graham MB, Letzer D, et al. Elizabethkingia anophelis: clinical experience of an Academic Health System in Southeastern Wisconsin. Open Forum Infect Dis. 2017;4:ofx251.
Navon L, Clegg WJ, Morgan J, Austin C, McQuiston JR, Blaney DD, et al. Notes from the field: investigation of Elizabethkingia anophelis Cluster - Illinois, 2014–2016. MMWR Morb Mortal Wkly Rep. 2016;65:1380–1.
Lee Y-L, Liu K-M, Chang H-L, Lin J-S, Kung F-Y, Ho C-M, et al. A dominant strain of Elizabethkingia anophelis emerged from a hospital water system to cause a three-year outbreak in a respiratory care center. J Hosp Infect. 2021;108:43–51.
Recent Outbreaks | Elizabethkingia | CDC [Internet]. 2018 [cited 2021 Oct 26]. Available from: https://www.cdc.gov/elizabethkingia/outbreaks/index.html
Coyle AL. Elizabethkingia anophelis: exploring the outbreak of disease in the Midwest. Nurs (Lond). 2017;47:61–3.
Kim KK, Kim MK, Lim JH, Park HY, Lee S-T. 2005. Transfer of Chryseobacterium meningosepticum and Chryseobacterium miricola to Elizabethkingia gen. nov. as Elizabethkingia meningoseptica comb. nov. and Elizabethkingia miricola comb. nov. Int J Syst Evol Microbiol. 2005;55:1287–93.
Kämpfer P, Matthews H, Glaeser SP, Martin K, Lodders N, Faye I. Elizabethkingia anophelis sp. nov., isolated from the midgut of the mosquito Anopheles gambiae. Int J Syst Evol Microbiol. 2011;61:2670–5.
Doijad S, Ghosh H, Glaeser S, Kämpfer P, Chakraborty T. Taxonomic reassessment of the genus Elizabethkingia using whole-genome sequencing: Elizabethkingia endophytica Kämpfer 2015 is a later subjective synonym of Elizabethkingia anophelis Kämpfer 2011. Int J Syst Evol Microbiol. 2016;66:4555–9.
Lin J-N, Lai C-H, Yang C-H, Huang Y-H. Elizabethkingia Infections in humans: from Genomics to Clinics. Microorganisms. 2019;7:295.
Nicholson AC, Gulvik CA, Whitney AM, Humrighouse BW, Graziano J, Emery B, et al. Revisiting the taxonomy of the genus Elizabethkingia using whole-genome sequencing, optical mapping, and MALDI-TOF, along with proposal of three novel Elizabethkingia species: Elizabethkingia bruuniana sp. nov., Elizabethkingia ursingii sp. nov., and Elizabethkingia occulta sp. nov. Antonie Van Leeuwenhoek. 2018;111:55–72.
Lau SKP, Chow W-N, Foo C-H, Curreem SOT, Lo GC-S, Teng JLL, et al. Elizabethkingia anophelis bacteremia is associated with clinically significant infections and high mortality. Sci Rep. 2016;6:26045.
Chew KL, Cheng B, Lin RTP, Teo JWP. Elizabethkingia anophelis is the Dominant Elizabethkingia Species found in blood cultures in Singapore. J Clin Microbiol. 2018;56.
Han M-S, Kim H, Lee Y, Kim M, Ku NS, Choi JY, et al. Relative prevalence and Antimicrobial susceptibility of clinical Isolates of Elizabethkingia Species based on 16S rRNA gene sequencing. J Clin Microbiol. 2017;55:274–80.
McTaggart LR, Stapleton PJ, Eshaghi A, Soares D, Brisse S, Patel SN, et al. Application of whole genome sequencing to query a potential outbreak of Elizabethkingia anophelis in Ontario, Canada. Access Microbiol. 2019;1:e000017.
Sahoo RK, Sahoo S, Das A, Gaur M, Bhanjadeo D, Panda P, et al. A phylogenetic study of Elizabethkingia anophelis bloodstream isolates obtained from inpatients at a single medical center. Infect Control Hosp Epidemiol. 2019;40:1202–4.
Lin J-N, Lai C-H, Yang C-H, Huang Y-H, Lin H-F, Lin H-H. Comparison of four automated microbiology systems with 16S rRNA gene sequencing for identification of Chryseobacterium and Elizabethkingia species. Sci Rep. 2017;7:13824.
Cheng Y-H, Perng C-L, Jian M-J, Cheng Y-H, Lee S-Y, Sun J-R, et al. Multicentre study evaluating matrix-assisted laser desorption ionization-time of flight mass spectrometry for identification of clinically isolated Elizabethkingia species and analysis of antimicrobial susceptibility. Clin Microbiol Infect off Publ Eur Soc Clin Microbiol Infect Dis. 2019;25:340–5.
Burnard D, Gore L, Henderson A, Ranasinghe A, Bergh H, Cottrell K, et al. Comparative Genomics and Antimicrobial Resistance profiling of Elizabethkingia isolates reveal nosocomial transmission and in Vitro susceptibility to Fluoroquinolones, Tetracyclines, and Trimethoprim-Sulfamethoxazole. J Clin Microbiol. 2020;58:e00730–20.
Pereira GH, Garcia D, de O, Abboud, Barbosa CS, de B VL, da Silva PSL. Nosocomial infections caused by Elizabethkingia meningoseptica: an emergent pathogen. Braz J Infect Dis off Publ Braz Soc Infect Dis. 2013;17:606–9.
Kukutla P, Lindberg BG, Pei D, Rayl M, Yu W, Steritz M et al. Insights from the Genome Annotation of Elizabethkingia anophelis from the Malaria Vector Anopheles gambiae. Tu Z, editor. PLoS ONE. 2014;9:e97715.
Breurec S, Criscuolo A, Diancourt L, Rendueles O, Vandenbogaert M, Passet V, et al. Genomic epidemiology and global diversity of the emerging bacterial pathogen Elizabethkingia anophelis. Sci Rep. 2016;6:30379.
Lin J-N, Lai C-H, Yang C-H, Huang Y-H, Lin H-H. Genomic features, phylogenetic relationships, and comparative genomics of Elizabethkingia anophelis strain EM361-97 isolated in Taiwan. Sci Rep. 2017;7:14317.
Lin J-N, Lai C-H, Yang C-H, Huang Y-H, Lin H-H. Clinical manifestations, molecular characteristics, antimicrobial susceptibility patterns and contributions of target gene mutation to fluoroquinolone resistance in Elizabethkingia anophelis. J Antimicrob Chemother. 2018;73:2497–502.
Ratnamani M, Rao R. Elizabethkingia meningoseptica: emerging nosocomial pathogen in bedside hemodialysis patients. Indian J Crit Care Med. 2013;17:304–7.
Puah SM, Fong SP, Kee BP, Puthucheary SD, Chua KH. Molecular identification and biofilm-forming ability of Elizabethkingia species. Microb Pathog. 2022;162:105345.
Lisotto P, Couto N, Rosema S, Lokate M, Zhou X, Bathoorn E, et al. Molecular Characterisation of Vancomycin-Resistant Enterococcus faecium isolates belonging to the lineage ST117/CT24 Causing Hospital Outbreaks. Front Microbiol. 2021;12:728356.
Chen S, Soehnlen M, Walker ED. Genome sequence of Elizabethkingia meningoseptica EM1, isolated from a patient with a bloodstream infection. Genome Announc. 2016;4.
Guerpillon B, Fangous MS, Le Breton E, Artus M, le Gall F, Khatchatourian I, et al. Elizabethkingia anophelis outbreak in France. Infect Dis Now. 2022;52:299–303.
Nievas J, Luz Ibañez M, Allende L, Altclas J, Antezana G, Campos J, et al. Emergence of Elizabethkingia anophelis. First case of E. anophelis outbreak in a neonatal unit of a hospital in Argentina. Clin Infect Pract. 2022;13:100122.
Jian M-J, Cheng Y-H, Chung H-Y, Cheng Y-H, Yang H-Y, Hsu C-S, et al. Fluoroquinolone resistance in carbapenem-resistant Elizabethkingia anophelis: phenotypic and genotypic characteristics of clinical isolates with topoisomerase mutations and comparative genomic analysis. J Antimicrob Chemother. 2019;74:1503–10.
Yung C-F, Maiwald M, Loo LH, Soong HY, Tan CB, Lim PK, et al. Elizabethkingia anophelis and association with tap Water and Handwashing, Singapore. Emerg Infect Dis. 2018;24:1730–3.
Choi MH, Kim M, Jeong SJ, Choi JY, Lee I-Y, Yong T-S, et al. Risk factors for Elizabethkingia Acquisition and clinical characteristics of patients, South Korea. Emerg Infect Dis. 2019;25:42–51.
Elbadawi LI, Borlaug G, Gundlach K, Monson T, Noble-Wang J, Moulton-Meissner H, et al. A large and primarily Community Associated Outbreak of Elizabethkingia anophelis Infections, Wisconsin, 2015–2016. Open Forum Infect Dis. 2016;3:LB–9.
Lee Y-L, Liu K-M, Chang H-L, Liao Y-C, Lin J-S, Kung F-Y, et al. The Evolutionary Trend and genomic features of an emerging lineage of Elizabethkingia anophelis strains in Taiwan. Microbiol Spectr. 2022;10:e0168221.
Teo J, Tan SY-Y, Tay M, Ding Y, Kjelleberg S, Givskov M, et al. First case of E anophelis outbreak in an intensive-care unit. Lancet Lond Engl. 2013;382:855–6.
Balm MND, Salmon S, Jureen R, Teo C, Mahdi R, Seetoh T, et al. Bad design, bad practices, bad bugs: frustrations in controlling an outbreak of Elizabethkingia meningoseptica in intensive care units. J Hosp Infect. 2013;85:134–40.
Wang L, Zhang X, Li D, Hu F, Wang M, Guo Q, et al. Molecular characteristics and antimicrobial susceptibility profiles of Elizabethkingia clinical isolates in Shanghai, China. Infect Drug Resist. 2020;13:247–56.
Xu L, Peng B, He Y, Cui Y, Hu Q, Wu Y, et al. Isolation of Elizabethkingia anophelis from COVID-19 Swab kits. Front Microbiol. 2021;12:799150.
Wang J-L, Chen M-L, Lin YE, Chang S-C, Chen Y-C. Association between contaminated faucets and colonization or infection by nonfermenting gram-negative bacteria in intensive care units in Taiwan. J Clin Microbiol. 2009;47:3226–30.
Hopman J, Tostmann A, Wertheim H, Bos M, Kolwijck E, Akkermans R, et al. Reduced rate of intensive care unit acquired gram-negative bacilli after removal of sinks and introduction of water-free patient care. Antimicrob Resist Infect Control. 2017;6:59.
Lin T-C, Wu R-X, Chiu C-C, Yang Y-S, Lee Y, Lin J-C, et al. The clinical and microbiological characteristics of infections in burn patients from the Formosa Fun Coast Dust Explosion. J Microbiol Immunol Infect Wei Mian Yu Gan Ran Za Zhi. 2018;51:267–77.
Zong Z. Biliary tract infection or colonization with Elizabethkingia meningoseptica after endoscopic procedures involving the biliary tract. Intern Med Tokyo Jpn. 2015;54:11–5.
Lau SKP, Wu AKL, Teng JLL, Tse H, Curreem SOT, Tsui SKW, et al. Evidence for Elizabethkingia anophelis transmission from mother to infant, Hong Kong. Emerg Infect Dis. 2015;21:232–41.
Cartwright EJ, Prabhu RM, Zinderman CE, Schobert WE, Jensen B, Noble-Wang J, et al. Transmission of Elizabethkingia meningoseptica (formerly Chryseobacterium meningosepticum) to tissue-allograft recipients: a report of two cases. J Bone Joint Surg Am. 2010;92:1501–6.
Ramanan P, Razonable RR. Elizabethkingia species sepsis after lung transplantation: case report and literature review. Transpl Infect Dis off J Transplant Soc. 2013;15:E229–234.
Speich R, van der Bij W. Epidemiology and management of infections after lung transplantation. Clin Infect Dis off Publ Infect Dis Soc Am. 2001;33(Suppl 1):58–65.
Moore LSP, Owens DS, Jepson A, Turton JF, Ashworth S, Donaldson H, et al. Waterborne Elizabethkingia meningoseptica in adult critical care. Emerg Infect Dis. 2016;22:9–17.
Maynard E. Prevention and control of multidrug-resistant organisms within the healthcare water supply. Perspect Public Health. 2016;136:330–2.
Coll F, Raven KE, Knight GM, Blane B, Harrison EM, Leek D, et al. Definition of a genetic relatedness cutoff to exclude recent transmission of meticillin-resistant Staphylococcus aureus: a genomic epidemiology analysis. Lancet Microbe. 2020;1:e328–35.
Deurenberg RH, Bathoorn E, Chlebowicz MA, Couto N, Ferdous M, García-Cobos S, et al. Application of next generation sequencing in clinical microbiology and infection prevention. J Biotechnol. 2017;243:16–24.
Jiang X, Wang D, Wang Y, Yan H, Shi L, Zhou L. Occurrence of antimicrobial resistance genes sul and dfrA12 in hospital environmental isolates of Elizabethkingia meningoseptica. World J Microbiol Biotechnol. 2012;28:3097–102.
Crist MB, McQuiston JR, Spalding Walters M, Soda E, Moulton-Meissner H, Nicholson A, et al. Investigations of Healthcare-Associated Elizabethkingia Infections - United States, 2013–2019. Open Forum Infect Dis. 2020;7:472.
Decker BK, Palmore TN. The role of water in healthcare-associated infections. Curr Opin Infect Dis. 2013;26:345–51.
Perkins KM, Reddy SC, Fagan R, Arduino MJ, Perz JF. Investigation of healthcare infection risks from water-related organisms: Summary of CDC consultations, 2014–2017. Infect Control Hosp Epidemiol. 2019;40:621–6.
Kottapalli P, Deepika C, Jyothi S, Mol R, Sadhana Y, Chander Reddy PN. Outbreak investigation of Elizabethkingia meningoseptica at a tertiary care hospital. J Patient Saf Infect Control. 2021;9:77–82.
Ceyhan M, Celik M. Elizabethkingia meningosepticum (Chryseobacterium meningosepticum) infections in children. Int J Pediatr. 2011;2011:215237.
Shaik Ismail B, Ling ML, Seah JH, Toh HX. Still think that hand washing is best - think again? Antimicrob Resist Infect Control. 2019;8:148.
Ceyhan M, Yildirim I, Tekeli A, Yurdakok M, Us E, Altun B, et al. A Chryseobacterium meningosepticum outbreak observed in 3 clusters involving both neonatal and non-neonatal pediatric patients. Am J Infect Control. 2008;36:453–7.
Tai P-W, Tsai C-Y, Tsui K-C, Huang C-H. Elizabethkingia meningosepticum outbreak among patients using mechanical ventilator in a medical intensive care unit of a hospital in Northern Taiwan. J Microbiol Immunol Infect. 2015;48:88.
Arvanitidou M, Vayona A, Spanakis N, Tsakris A. Occurrence and antimicrobial resistance of Gram-negative bacteria isolated in haemodialysis water and dialysate of renal units: results of a greek multicentre study. J Appl Microbiol. 2003;95:180–5.
Chan JC, Chong CY, Thoon KC, Tee NWS, Maiwald M, Lam JCM, et al. Invasive paediatric Elizabethkingia meningoseptica infections are best treated with a combination of piperacillin/tazobactam and trimethoprim/sulfamethoxazole or fluoroquinolone. J Med Microbiol. 2019;68:1167–72.
Huang Y-C, Wu P-F, Lin Y-T, Wang F-D. Comparison of clinical characteristics of bacteremia from Elizabethkingia meningoseptica and other carbapenem-resistant, non-fermenting gram-negative bacilli at a tertiary medical center. J Microbiol Immunol Infect Wei Mian Yu Gan Ran Za Zhi. 2019;52:304–11.
Jean SS, Lee WS, Chen FL, Ou TY, Hsueh PR. Elizabethkingia meningoseptica: an important emerging pathogen causing healthcare-associated infections. J Hosp Infect. 2014;86:244–9.
Rastogi N, Mathur P, Bindra A, Goyal K, Sokhal N, Kumar S, et al. Infections due to Elizabethkingia meningoseptica in critically injured trauma patients: a seven-year study. J Hosp Infect. 2016;92:30–2.
Sedigh Ebrahim-Saraie H, Heidari H, Khashei R, Nabavizadeh SH. A rare case of complicated pericardial effusion with Elizabethkingia meningoseptica from Iran. Cell Mol Biol (Noisy-le-grand). 2018;64:53–5.
Ganesan V, Rajendran T, Charles J. PBI-006 - invasive Elizabethkingia meningoseptica infections – a descriptive study from South India. Abstr 13th Int Symp Antimicrob Agents Resist ISAAR 2021. 2021;58:21003009.
O’Brien TF, Clark A, Peters R, Stelling J. Why surveillance of antimicrobial resistance needs to be automated and comprehensive. J Glob Antimicrob Resist. 2019;17:8–15.
Tseng W-P, Chen Y-C, Yang B-J, Chen S-Y, Lin J-J, Huang Y-H, et al. Predicting multidrug-resistant gram-negative bacterial colonization and associated infection on hospital admission. Infect Control Hosp Epidemiol. 2017;38:1216–25.
Tekerekoglu MS, Durmaz R, Ayan M, Cizmeci Z, Akinci A. Analysis of an outbreak due to Chryseobacterium meningosepticum in a neonatal intensive care unit. New Microbiol. 2003;26:57–63.
Maraki S, Scoulica E, Manoura A, Papageorgiou N, Giannakopoulou C, Galanakis E. A Chryseobacterium meningosepticum colonization outbreak in a neonatal intensive care unit. Eur J Clin Microbiol Infect Dis off Publ Eur Soc Clin Microbiol. 2009;28:1415–9.
Issack MI, Neetoo Y. An outbreak of Elizabethkingia meningoseptica neonatal meningitis in Mauritius. J Infect Dev Ctries. 2011;5:834–9.
Weaver KN, Jones RC, Albright R, Thomas Y, Zambrano CH, Costello M, et al. Acute emergence of Elizabethkingia meningoseptica infection among mechanically ventilated patients in a long-term acute care facility. Infect Control Hosp Epidemiol. 2010;31:54–8.
Pokrywka M, Viazanko K, Medvick J, Knabe S, McCool S, William Pasculle A, et al. A Flavobacterium meningosepticum outbreak among intensive care patients. AJIC Am J Infect Control. 1993;21:139–45.
Yannelli B, Koj IG, Cunha BA. Chryseobacterium meningosepticum bacteremia secondary to central intravenous line-related infection. Am J Infect Control. 1999;27:533–5.
Sahu MK, Balasubramaniam U, Singh CB, Talwar SP. Elizabethkingia Meningoseptica: an Emerging Nosocomial Pathogen causing septicemia in critically ill patients. Indian J Crit Care Med Peer-Rev off Publ Indian Soc Crit Care Med. 2019;23:104–5.
Jassat R, Jeena PM. The emergence of Elizabethkingia meningoseptica infections in a quaternary-level paediatric intensive care unit in Durban, South Africa. South Afr J Child Health. 2022;16:39–44.
Price E, Weaver G, Hoffman P, Jones M, Gilks J, O’Brien V, et al. Decontamination of breast pump milk collection kits and related items at home and in hospital: guidance from a joint Working Group of the Healthcare infection society and infection Prevention Society. J Hosp Infect. 2016;92:213–21.
Price E, Hoffman P, Weaver G, Gilks J, Jones M, O’Brien V, et al. Difficulty with decontaminating dummies (pacifiers, soothers or comforters) for infants in hospital. J Hosp Infect. 2017;97:316.
Checklin D, Gray J. Microbiological risks of reusing dummies for infants in hospital. J Hosp Infect. 2018;99:365–6.
Kanamori H, Weber DJ, Rutala WA. Healthcare Outbreaks Associated with a Water Reservoir and infection Prevention Strategies. Clin Infect Dis. 2016;62:1423–35.
Flaherty KA, Brennan-Krohn T, Kinlay J, Scanlon P, Potter-Bynoe G, Sandora T. Improving use of sterile water for oral care and tube flushes in pediatric intensive care units. Am J Infect Control. 2015;43:66.
McArthur DB. Emerging Infectious Diseases. Nurs Clin North Am. 2019;54:297–311.
Govindaswamy A, Bajpai V, Trikha V, Mittal S, Malhotra R, Mathur P. Multidrug resistant Elizabethkingia meningoseptica bacteremia-experience from a level 1 trauma centre in India. Intractable Rare Dis Res. 2018;7:172–6.
Jung SH, Lee B, Mirrakhimov AE, Hussain N. Septic shock caused by Elizabethkingia meningoseptica: a case report and review of literature. BMJ Case Rep. 2013;2013.
Tai I-C, Liu T-P, Chen Y-J, Lien R-I, Lee C-Y, Huang Y-C. Outbreak of Elizabethkingia meningoseptica sepsis with meningitis in a well-baby nursery. J Hosp Infect. 2017;96:168–71.
Lin Y-T, Chiu C-H, Chan Y-J, Lin M-L, Yu K-W, Wang F-D, et al. Clinical and microbiological analysis of Elizabethkingia meningoseptica bacteremia in adult patients in Taiwan. Scand J Infect Dis. 2009;41:628–34.
Dias M, Fernandes A, Furtado Z. Case series: Elizabethkingia meningosepticum. J Clin Diagn Res. 2012;6:1550–1.
Dias M, Prashant K, Pai R, Scaria B. Chryseobacterium meningosepticum bacteremia in diabetic nephropathy patient on hemodialysis. Indian J Nephrol. 2010;20:203–4.
Güngör S, Ozen M, Akinci A, Durmaz R. A Chryseobacterium meningosepticum outbreak in a neonatal ward. Infect Control Hosp Epidemiol. 2003;24:613–7.
Khan ID, Lall M, Sen S, Ninawe SM, Chandola P. Multiresistant elizabethkingia meningoseptica infections in tertiary care. Med J Armed Forces India. 2015;71:282–6.
Snesrud E, McGann P, Walsh E, Ong A, Maybank R, Kwak Y, et al. Clinical and genomic features of the first cases of Elizabethkingia anophelis infection in New York, including the First Case in a healthy infant without previous nosocomial exposure. J Pediatr Infect Dis Soc. 2019;8:269–71.
Larkin PMK, Mortimer L, Malenfant JH, Gaynor P, Contreras DA, Garner OB, et al. Investigation of phylogeny and Drug Resistance Mechanisms of Elizabethkingia anophelis isolated from blood and lower respiratory tract. Microb Drug Resist Larchmt N. 2021;27:1259–64.
Acknowledgements
We thank Jochem Buil of the Radboud University Medical Center Nijmegen for performing additional susceptibility tests on the clinical isolate.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
LM conceptualized the study, searched the literature, selected studies, and composed and edited the report. SR analyzed the WGS results, composed the SNP tree and reviewed and edited the report. EB conceptualized the study, and composed and edited the report. RHV and AV reviewed, edited and supervised the report. All authors critically reviewed the extracted data, contributed to writing and review of the manuscript, and approved the final version.
Corresponding author
Ethics declarations
Ethical approval
Preparation of a case report for publication does not require review by the ethics board in the Netherlands.
Informed consent
A written informed consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mallinckrodt, L., Huis in ’t Veld, R., Rosema, S. et al. Review on infection control strategies to minimize outbreaks of the emerging pathogen Elizabethkingia anophelis. Antimicrob Resist Infect Control 12, 97 (2023). https://doi.org/10.1186/s13756-023-01304-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-023-01304-1