Abstract
Background
Multi-drug resistance (MDR) in Gram-negative organisms is an alarming problem in the world. MDR and extensively-drug resistance (XDR) is in increasing trend due to the production of different types of beta (β)-lactamases. Thus the aim of this study was to document the incidence of MDR and XDR in clinical isolates of Escherichia coli and also to find out the enzymatic mechanisms of β-lactam antibiotics resistance.
Methods
Two hundred clinical isolates of Escherichia coli (E. coli) identified by standard laboratory methods were studied. Antibiotic susceptibility profile was performed for all the isolates and the suspected isolates were phenotypically tested for the production of extended spectrum β-lactamase (ESBL), metallo β-lactamase (MBL) and AmpC β-lactamase (AmpC) by recommended methods.
Results
Around three-fourth (78%) of the total isolates were multi-drug resistant. ESBL, MBL and AmpC production was found in 24%, 15% and 9% of isolates respectively. Amikacin, chloramphenicol and colistin were found to be the most effective antibiotics.
Conclusions
High percentage of MDR was observed. β-lactamase mediated resistance was also high. Thus, regular surveillance of drug resistance due to β-lactamases production and infection control policy are of utmost importance to minimize the spread of resistant strains.
Similar content being viewed by others
Background
Resistance to broad spectrum β-lactams, mediated by extended spectrum β-lactamases (ESBL), metallo β-lactamases (MBL) and AmpC β-lactamases (AmpC) enzymes is an increasing problem worldwide [1]. Presence of the latter two enzymes in clinical infections can result in treatment failure if one of the second- or third-generation cephalosporin is used. The scenario worsens in cases of MBL production where the drugs of last resort the carbapenems are rendered inactive [2]. Due to extensive use of β-lactam antibiotics over the last several decades in the clinical practice, various β-lactamases have emerged. ESBLs are the enzymes produced by Gram-negative bacilli that have the ability to hydrolyze β-lactam antibiotics containing an oxyimino group (third generation cephalosporins and aztreonam) and are inhibited by β-lactamase inhibitors such as clavulanic acid, sulbactam and tazobactam [3].
ESBLs were first identified in 1983. Since the time, they have been found worldwide in a number of organisms, including Klebsiella pneumoniae (K. pneumoniae), Klebsiella oxytoca, Escherichia coli (E. coli), Proteus mirabilis, Enterobacter cloacae, Morganella morganii, Serratia marcescens, Shigella dysenteriae, Pseudomonas aeruginosa, Burkholderia cepacia, Capnocytophaga ochracea, Citrobacter species, and Salmonella species [4-10].
The emergence of ESBL producing bacteria, particularly E. coli and K. pneumoniae, is now a critical concern for the development of therapies against bacterial infection. The major ESBL producer was K. pneumoniae before 2000, but now E. coli has become an important ESBL carrier in Western countries [11-13]. Since the ESBL genes are usually found in large plasmids, they also contain other antimicrobial resistant genes. Therefore, most ESBL producing organisms are also resistant to aminogylcosides, fluororquinolones, tetracyclines, chloramphenicol, sulfonamides. Carbapenems are the mainstay of therapy for infections caused by ESBL producing organisms [14]. Therefore, resistance against these agents poses therapeutic challenge. Based on molecular studies, carbapenem hydrolyzing enzymes are classified into four groups A, B, C and D. The MBLs belong to group B and are enzymes requiring divalent cations as cofactors for enzyme activity, being inhibited by the action of a metal ion chelator [15]. The MBLs efficiently hydrolyze all β-lactams, except aztreonam in vitro [16].
AmpC-mediated β-lactam resistance in E. coli and Klebsiella spp. is an emerging problem [17]. High level AmpC production is typically associated with in vitro resistance to all β-lactam antibiotics except for carbapenems and cefepime. In addition, treatment failures with broad-spectrum cephalosporins have been documented [18,19].
The production of β-lactamases is the single most prevalent mechanism responsible for resistance to β-lactams among clinical isolates belonging to the family of Entrobacteriaceae [20]. Over the years, many new β-lactam antibiotics have been developed. However, with each new class of antibiotics, a new β-lactamase has emerged and caused resistance to it. Presumably, the selective pressure imposed by the use and overuse of new antibiotics in the treatment of patients has resulted in the emergence of new variants of β-lactamases [21]. In this perspective, the present study was designed to document the existence of ESBL, MBL and AmpC-production in clinical isolates of multi-drug and extensively-drug resistant E. coli and to determine whether any alternative regimens are available to treat them.
Methods
A total of 200 random, non-redundant and non-repetitive community acquired clinical isolates of E. coli (urine 90, sputum 50, pus 40, blood 20), identified by standard microbiological technique [22] in the bacteriological laboratory of Chitwan Medical College Teaching Hospital (CMCTH), a 600 bed tertiary care center of central Nepal in 2013, were subjected to phenotypic determination of the antimicrobial susceptibility, identification of MDR, XDR and pan drug resistant (PDR); and detection of ESBL, MBL and AmpC β-lactamase production.
Antimicrobial susceptibility testing
Antibiograms of the isolates were determined by modified Kirby-Bauer disk diffusion method on Mueller-Hinton agar standard media using commercially prepared disks (HiMedia Laboratories Pvt. Limited, India) in compliance with Clinical and Laboratory Standards Institute (CLSI) guidelines [23]. Antimicrobials used were: penicillin [ampicillin (10 μg)], penicillins with β-lactamase inhibitors [ampicillin-sulbactam (10/10 μg), amoxicillin-clavulanic acid (10 μg)], narrow spectrum cephalosporin [cefazolin (30 μg)], extended spectrum cephalosporins [ceftazidime (30 μg), ceftriaxone (30 μg), cefepime (30 μg)], cephamycin [cefoxitin (30 μg)], antipseudomonal penicillins with β-lactamase inhibitors [piperacillin-tazobactam (100/10 μg), ticarcillin-clavulanic acid (75/10 μg)], monobactam [aztreonam (30 μg)], carbapenems [imipenem (10 μg), meropenem (10 μg)], aminoglycosides [gentamicin (10 μg), amikacin (30 μg), tobramycin (10 μg)], fluoroquinolones [ciprofloxacin (5 μg), ofloxacin (5 μg)], folate pathway inhibitor [co-trimoxazole (25 μg)], phenicol [chloramphenicol (30 μg)] and polymyxin [colistin (10 μg)]. Interpretation of susceptibility was made according to the tables for interpretative zone diameters of CLSI [23]. E. coli 25922 was used as a control organism for antibiotic sensitivity testing.
Identification of MDR, XDR and PDR isolates
MDR, XDR and PDR isolates were identified according to the guidelines recommended by joint initiative of the European Centre for Disease Prevention and Control (ECDC) and the Centers for Disease Control and Prevention (CDC) [24]. According to the guidelines, the isolates showing non-susceptibility to at least one agent in three or more antimicrobial categories were identified as MDR, non-susceptibility to at least one agent in all but two or fewer antimicrobial categories (i.e. bacterial isolates remained susceptible to only one or two categories) were identified as XDR and non-susceptibility to all agents in all antimicrobial categories were identified as PDR. To ensure correct application of these definitions, bacterial isolates were tested against all or nearly all of the commercially available antimicrobial agents within the antimicrobial categories (recommended by ECDC and CDC) and selective reporting and suppression of results were avoided [24].
Phenotypic detection of ESBL
Isolates of E. coli were examined for their susceptibility to 3rd generation cephalosporins by using ceftazidime (30 μg) and cefotaxime (30 μg) disks. The isolates showing diameter of ≤ 22 mm zone of inhibition for ceftazidime and/or ≤ 27 mm for cefotaxime were considered as ESBLs suspects as per National Committee for Clinical Laboratory Standards (NCCLS) guidelines [25]. All suspected isolates for ESBLs production were confirmed by the combination disk method on Mueller Hinton agar plates that were inoculated with standardized inoculums (comparable to 0.5 McFarland standards) of the isolates to form a lawn culture. Separate commercial disks containing cefotaxime (30 μg) and ceftazidime (30 μg) with and without clavulanic acid (10 μg) were placed over the lawn culture. An increase in zone size of more than or equal to 5 mm for cefotaxime and ceftazidime with and without clavulanic acid indicated ESBL production as described by Carter et al. [26].
Phenotypic detection of MBL
Isolates that were found resistant to imipenem, meropenem or third generation cephalosporins (ceftazidime) in Kirby Bauer disk diffusion method were presumptively considered MBL producers and were confirmed by the imipenem disk with EDTA methods. Briefly, the test inoculums (comparable to 0.5 McFarland standards) were prepared and transferred on to Mueller Hinton agar plates. Two imipenem (10ug) disks were placed on the surface of agar plate and 10 μl EDTA solutions was added to one of them to obtain a desired concentration of 750 μg. Plates were incubated for 16 to 18 hours at 35°C. An increase in zone size of more than or equal to 7 mm for imipenem-EDTA disk compared to imipenem disk alone indicated MBL producer strain as described by Yong et al. [27].
Phenotypic detection of AmpC
All E. coli isolates resistant to cefoxitin in Kirby-Bauer disk diffusion method were confirmed for AmpC β-lactamase production by modified Hodge test. In the test, a cefoxitin susceptible E. coli indicator strain (ATCC 25922) was plated on Muller Hinton agar medium and the cefoxitin disk was placed. Test organism was streaked toward the cefoxitin disk. If the test organism expressed AmpC, it hydrolyzed the cefoxitin and showed growth along the intersection of the streak and the zone of inhibition from the cefoxitin disk [28].
Ethical consideration
The samples used in this study were from routine clinical specimens; however, verbal consent was taken from the patients. The ethical approval was obtained from Institutional Review Committee of Chitwan Medical College Teaching Hospital (CMCTH), Bharatpur, Nepal to conduct the study.
Results
Resistance pattern of E. coli
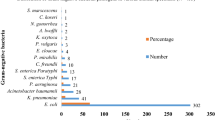
All of the E. coli isolates tested exhibited resistance to amoxicillin-clavulanic acid and 77 % of them remained resistant to ciprofloxacin whereas all the isolates were susceptible to colistin and few isolates (7%) were resistant to imipenem (Table 1).
MDR and XDR isolate
Of total 200 E. coli isolates tested, 156 (78%) isolates were MDR and 14 (7%) isolates were XDR whereas no PDR isolate was identified (Table 1).
All MDR isolates were resistant to amoxicillin-clavulanic acid and 91% isolates were resistant to ciprofloxacin whereas amikacin, imipenem and colistin were found as the most effective antibiotics for the MDR isolates. All XDR isolates were resistant to most of the antibiotics tested whereas colistin was found as the effective regimen against all XDR isolates (Table 1).
ESBL, MBL and AmpC producing isolates and their resistance profile
Among total tested isolates, the synthesis of ESBL, MBL and AmpC was detected in 48 (24%), 30 (15%) and 18 (9%) isolates respectively (Tables 2 and 3). Most of the antibiotics tested were non-effective against ESBL, MBL and AmpC producers whereas imipenem, amikacin, chloramphenicol and colistin were found effective regimens against ESBL producers and only colistin was effective against MBL and Amp C producing isolates (Table 2).
Multi-type β-lactamase production
Of the tested isolates, 10 (5%) were producers of both ESBL and MBL, 8 (4%) isolates synthesized both ESBL and AmpC whereas 6 (3%) isolates produced both MBL and Amp C. All the three types of β-lactamases (i.e. ESBL, MBL and AmpC) were detected in 4 (2%) isolates (Table 3).
Resistance rates of antibiotics with different mode of action
All of the tested isolates were resistant to at least one cell wall inhibiting agents followed by folic acid metabolism inhibiting agent (59%) whereas no isolates were resistant to cytoplasmic membrane damaging agent (Table 4).
Incidence of resistant isolates
Very minor numbers of isolates (4%) were resistant to only one antibiotic whereas majorities (85%) of isolates were resistant to at least three antibiotics (Table 5).
Discussions
The production of \( \beta \)-lactamases as a major problem have drawn attention to a need for better diagnostic techniques and newer drugs to allow more specific therapy because of the emergence and spread of antimicrobial resistance. Therefore, the detection, characterization and antibiotic susceptibility pattern of \( \beta \)-lactamase producing organisms can lead to successful infection control, involving antimicrobial stewardship and public health interventions aimed at controlling the emergence of such life-threatening MDR bacteria. The global rise of MDR organisms and their production of resistant enzymes is a serious public health threat now a day.
There are various documented literatures on investigation of ESBL, MBL and AmpC producing isolates from Nepal. To the best of our knowledge, this is the first report from Nepal with an exclusive focus on investigating the current incidence and antimicrobial susceptibility patterns to a large number of antibiotics tested among ESBL, MBL and AmpC producing MDR and XDR E. coli isolates.
In current study we investigated 200 clinical isolates of E. coli, all of which were resistant to amoxicillin-clavulanic acid and 77 % of the isolates were found resistant to ciprofloxacin. Our finding is similar to the observation of Khanal et al. who reported that 66.7% of isolates were resistant to ciprofloxacin [29]. However, Khadgi et al. reported 100% resistance to ciprofloxacin [30]. Among the antimicrobials tested, colistin (100%), imipenem (93%) and amikacin (90%) were found as the most effective agents against E. coli in our study. Polymyxin (colistin) and amikacin as the most effective antibiotics has also been defined by other authors and it can be concluded that amikacin is a promising regimen for the empirical therapy [29-31]. Chloramphenicol is still an effective drug after so many years in use as only small percentage of isolates (17%) were resistant to it, a drug approved in 1947 for human clinical use.
In present study, of total isolates tested, 156 (78%) isolates were MDR. Similarly, higher rate of MDR was also reported by Sharma et al. (90.8%) [32] whereas Khanal et al. (50%) [29] and Baral et al. (38.2%) [31] reported its lower rate from Nepal. A high incidence of MDR E. coli was also observed by Ibrahim et al. (92.2%) from Sudan [33]. As it was a big concern for us, 7% of isolates exhibited XDR in the present study. However, we did not find any previous literature reporting XDR E. coli in Nepal.
All MDR isolates in this study were resistant to amoxicillin-clavulanic acid. Resistance to fluoroquinolones varies geographically and is an emerging problem in both developed and developing countries [34,35]. In the present study, MDR E. coli isolates showed relatively high resistance rates to ciprofloxacin (91%). This has been hypothesized to be related to the inappropriate use (over-use and miss-use) of fluoroquinolones for humans [36]. Also, prolonged use of low dose of the more potent fluoroquinolones such as ciprofloxacin has been shown to be the most significant risk factor for acquisition of resistance [37]. Majority of the MDR isolates were resistant to ampicillin (78%) and cotrimoxazole (65.4%). A few isolates also showed resistance to other antibiotics such as amikacin (3.8) and chloramphenicol (12.8) and no isolates were found to be resistant to imipenem and colistin. Likewise, Baral et al. from Nepal also reported similar resistance rates of ciprofloxacin (92.6%), ampicillin (94.1%), cotrimoxazole (86.8%), amikacin (6.2%) and chloramphenicol (27.1%) [31]. All XDR isolates were resistant to most of the antimicrobials tested whereas colistin was found as the most effective agent against all the XDR isolates.
ESBL-producing E. coli have been described in hospitals to cause various outbreaks, but their presence in community has also been documented [38-40]. The reduced susceptibility of Gram-negative isolates to the later generation cephalosporins could be attributable to ESBL or AmpC β-lactamase production or some other relevant underlying mechanisms. In this study, 48 (24%) ESBL and 18 (9%) AmpC β-lactamase producing E. coli strains were detected. Higher prevalence of ESBL producing E. coli has also been reported by other authors [31,41,42] but a lower prevalence of ESBL (8.6%) and similar prevalence of AmpC (7.8%) has been reported by Khanal et al. in Nepal [29]. This lower prevalence of ESBL by Khanal et al. may be due to the selection of only tracheal isolates from ICU. A higher prevalence of ESBL (67%) and AmpC (33%) has been reported by Altun et al. from Turkey [43]. This higher prevalence of ESBL and AmpC by Altun et al. may be because of the selection of various types of clinical samples from the ICU patients. MBL production is also in increasing trend causing the carbapenems to be the ineffective regimens. In our study we found, 30 (15%) MBL producers among tested isolates. Our finding is similar to 13.4% documented by Wadekar et al. from India [42].
Susceptibility pattern of ESBL-producing isolates showed that these strains are not only resistant to β-lactams but also to other classes of antibacterials including gentamicin, cotrimoxazole and fluoroquinolones. In this study, we found that the β-lactamases producing isolates were resistant to most of the antibiotics tested but amikacin, imipenem, chloramphenicol and colistin showed promising efficacy against ESBL and AmpC producing isolates, which is in accordance with the other report from Nepal [41]. The carbapenem group of antibiotics is the most effective regimen for ESBL and AmpC producers but the increasing rate of MBL production makes the serious problem in infection treatment. We observed that more than half of the MBL producers were resistant to nearly all the antibiotics tested while colistin was found effective against all the MBL producing isolates.
Multi type β-lactamases producing isolates were also reported in our study. Among total tested isolates, 10 (5%) isolates were producers of both ESBL and MBL. ESBL together with AmpC production was seen in 8 (4%) isolates, whereas, 6 (3%) isolates produced both MBL and AmpC and 4 (2%) isolates did all, ESBL, MBL and AmpC. Similar result of ESBL with AmpC production (5.4%) was also documented by Kaur et al. from India [44].
Over the past 20 years there has been increased resistance to β-lactam antibiotics due to production of ESBL mediated by plasmids. This type of resistance is now observed in all species of Enterobacteriaceae and currently disseminated worldwide [45]. In this study, no isolates were documented resistant to cytoplasmic membrane damaging agents (colistin) whereas all isolates were found resistant to at least one cell wall inhibiting agents (β-lactams) and provided a significant contribution for MDR. In addition, isolates resistant to protein synthesis inhibiting agents and DNA replication inhibiting agents seem to have contributed considerably in the production of MDR. Similar contribution of different antimicrobial agents was also noticed by Aly et al. in Egypt [46].
In the present study, we found that all the isolates were resistant to at least one agent and 170 (85%) isolates were resistant to at least 3 agents while 22 (11%) isolates were resistant to two agents and 8 (4%) isolates were resistant to only one antimicrobial agent.
Conclusions
This study concluded that, there is high prevalence of community acquired MDR E. coli and high rate of ESBL, MBL and AmpC β-lactamase production in our set up. A strict hospital infection control policies and a prudent use of antimicrobial regimens are to be adopted by the concerned people to minimize the development of resistant strains. It is also essential to have a regular and routine monitoring of ESBL, MBL and AmpC β-lactamase producing clinical isolates in clinical laboratories. Regular nation wise surveillance of multidrug resistance seems necessary step to combat the severity of infections caused by MDR pathogens. Further studies at molecular level may be beneficial to rule out the cause of MDR pattern.
References
Singhal S, Mathur T, Khan S, Upadhyay DJ, Chugh S, Gaind R, et al. Evaluation of methods for AmpC beta-lactamase in gram negative clinical isolates from tertiary care hospitals. Indian J Med Microbiol. 2005;23:120–4.
Thomson KS. Controversies about Extended-Spectrum and AmpC Beta-Lactamases. Emerg Infect Dis. 2001;7:333–6.
Bradford PA. Extended-spectrum β-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev. 2001;14:933–51.
Goussard S, Courvalin P. Updated sequence information for TEM beta-lactamase genes. Antimicrob Agents Chemother. 1999;43:367–70.
Heritage J, M'Zali FH, Gascoyne-Binzi D, Hawkey PM. Evolution and spread of SHV extended-spectrum betalactamases in gram-negative bacteria. J Antimicrob Chemother. 1999;44:309–18.
Jacoby GA, Medeiros AA. More extended-spectrum beta-lactamases. Antimicrob Agents Chemother. 1991;35:1697–04.
Marchandin H, Carriere C, Sirot D, Pierre HJ, Darbas H. TEM-24 produced by four different species of Enterobacteriaceae, including Providencia rettgeri, in a single patient. Antimicrob Agents Chemother. 1999;43:2069–73.
Mugnier P, Dubrous P, Casin I, Arlet G, Collatz EA. TEM derived extended-spectrum beta-lactamase in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1996;40:2488–93.
Palzkill T, Thomson KS, Sanders CC, Moland ES, Huang W, Milligan TW. New variant of TEM-10 beta-lactamase gene produced by a clinical isolate of Proteus mirabilis. Antimicrob Agents Chemother. 1995;39:1199–200.
Philippon A, Labia R, Jacoby GA. Extended-spectrum beta- lactamases. Antimicrob Agents Chemother. 1989;33:1131–6.
Cantón R, Coque TM. The CTX-M beta-lactamase pandemic. Curr Opin Microbiol. 2006;9:466–75.
Pitout JD, Laupland KB. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis. 2008;8:159–66.
Ramphal R, Ambrose PG. Extended-spectrum beta-lactamases and clinical outcomes: current data. Clin Infect Dis. 2006;42:164–72.
Tumbarello M, Spanu T, Sanguinetti M, Citton R, Montuori E, Leone F, et al. Bloodstream infections caused by Extended-spectrum β-lactamase producing Klebsiella pneumoniae: Risk factors, molecular epidemiology, and clinical outcome. Antimicrob Agents Chemother. 2006;50:498–04.
Ambler RP. The structure of beta-lactamases. Philos Trans R Soc London Bio Sci. 1980;289:321–31.
Bush K, Jacoby GA, Medeiros AA. A functional classification scheme for b-lactamases and its correlation with molecular structure. Antimicrob Agents Chemother. 1995;39:1211–33.
Philippon A, Arlet G, Jacoby GA. Plasmid-determined AmpC type-lactamases. Antimicrob Agents Chemother. 2002;46:1–11.
Odeh R, Kelkar S, Hujer AM, Bonomo RA, Schreckenberger PC, Quinn JP. Broad resistance due to plasmid-mediated AmpC betalactamases in clinical isolates of Escherichia coli. Clin Infect Dis. 2002;35:140–5.
Wong-Beringer A, Hindler J, Loeloff M, Queenan AM, Lee N, Pegues DA, et al. Molecular correlation for the treatment outcomes in bloodstream infections caused by Escherichia coli and Klebsiella pneumoniae with reduced susceptibility to ceftazidime. Clin Infect Dis. 2002;34:135–46.
Conceição T, Brízio A, Duarte A, Barros R. First isolation of bla (VIM-2) in Klebsiella oxytoca clinical isolates from Portugal. Antimicrob Agents Chemother. 2005;49(1):476.
Narayanaswamy A, Mallika M. Prevalence and Susceptibility of extended spectrum beta-lactamases in urinary isolates of Escherichia coli in a Tertiary Care Hospital, Chennai-South India. Int J Med Update. 2011;6(1):39–3.
Isenberg HD. Clinical Microbiology Procedures Handbook. 2nd ed. Washington DC: ASM press; 2004.
Clinical and Laboratory Standard Institute (CLSI). Performance standards for antimicrobial susceptibility testing. USA: CLSI: M100-S16. Wayne, PA; 2006.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81.
National Committee for Clinical Laboratory Standards (NCCLS). Performance Standards for Antimicrobial Susceptibility Testing; Eighth Informational Supplement. NCCLS document M100-S8. NCCLS, Wayne, PA; 1998.
Carter MW, Oakton KJ, Warner M, Livermore DM. Detection of extended spectrum betalactamases in Klebsiella with the Oxoid combination disk method. J Clin Microbiol. 2000;38:4228–32.
Yong D, Lee K, Yum JH, Shin HB, Rossolini GM, Chong Y. Imipenem-EDTA disc method for differentiation of metallo-ß-lactamase-producing clinical isolates of Pseudomonas spp. and Acinetobacter spp. J Clin Microbiol. 2002;40(10):3798–01.
Rand KH, Turner B, Seifert H, Hansen C, Johnson JA, Zimmer A. Clinical laboratory detection of AmpC bet-lactamase. Does it affect patient outcome? Am J Clin Pathol. 2011;135:572–6.
Khanal S, Joshi DR, Bhatta DR, Devkota U, Pokhrel BM. Production of multidrug resistant bacterial pathogens from tracheal aspirates of intensive care unit patients at National Institute of Neurological and Allied Sciences, Nepal. ISRN Microbiol. 2013;2:847569. doi:10.1155/2013/847569.
Khadgi S, Timilsina U, Shrestha B. Plasmid profiling of multidrug resistant Escherichia coli strains isolated from urinary tract infection patients. Int J Appl Sci Biotechnol. 2013;1(1):1–4.
Baral P, Neupane S, Marasini BP, Ghimire KR, Lekhak B, Shrestha B. High prevalence of multidrug resistance in bacterial uropathogens from Kathmandu, Nepal. BMC Res Notes. 2012;5:38.
Sharma AR, Bhatta DR, Shrestha J, Banjara MR. Antimicrobial susceptibility pattern of Escherichia coli isolated from uninary tract infected patients attending Bir hospital, Nepal. J Sci Technol. 2013;14(1):177–84.
Ibrahim ME, Bilal NE, Hamid ME. Increased multi-drug resistant Escherichia coli from hospitals in Khartoum state, Sudan. Afr Health Sci. 2012;12(3):368–75.
Boyd LB, Atmar R, Randall GL, Hamill RJ, Steffen D, Zechiedrich L. Increased fluoroquinolone resistance with time in Escherichia coli from >17,000 patients at a large county hospital as function of culture site, age, sex, and location. BMC Infect Dis. 2008;8:4.
Namboodiri SS, Opintan JA, Lijek RS, Newman MJ, Okeke IN. Quinolone resistance in Escherichia coli from Accra, Ghana. BMC Microbiol. 2011;11:44.
Drago L, Nicola L, Mattina R, Vecchi ED. In vitro lselection of resistance in Escherichia coli and Klebsiella spp. at in vivo fluoroquinolone concentrations. BMC Microbiol. 2010;10:119.
Chenia HY, Pillay B, Pillay D. Analysis of the mechanisms of fluoroquinolone resistance in urinary tract pathogens. J Antimicrob Chemother. 2006;58:1274–8.
Arpin C, Dubois V, Coulange L, André C, Fischer I, Noury P, et al. Extended spectrum bata-lactamase producing Enterobacteriaceae in community and private health care centers. Antimicrob Agents Chemother. 2003;47:3506–14.
Rodríguez-Baño J, Navarro MD, Romero L, Martínez-Martínez L, Muniain MA, Perea EJ, et al. Epidemiology and clinical of infectious caused by extended-spectrum bata-lactamase producing Escherichia coli in nonhospitalized patients. J Clin Microbiol. 2004;42:1089–94.
Brigante G, Luzzaro F, Perilli M, Lombardi G, Colì A, Rossolini GM, et al. Evolution of CTX-M-type beta-lactamases in isolates of Escherichia coli infecting hospital and community patients. Int J Antimicrob Agents. 2005;25:157–62.
Chander A, Shrestha CD. Prevalence of extended spectrum beta lactamase producing Escherichia coli and Klebsiella pneumoniae urinary isolates in a tertiary care hospital in Kathmandu, Nepal. BMC Res Notes. 2013;6:487.
Wadekar MD, Anuradha K, Venkatesha D. Phenotypic detection of ESBL and MBL in clinical isolates of Enterobacteriaceae. Int J Current Res Acad Rev. 2013;1(3):89–5.
Altun S, Tufan ZK, Yağcı S, Önde U, Bulut C, Kiniki S, et al. Extended spectrum beta-lactamases, AmpC and metallo beta-lactamases in emerging multi-drug resistant Gram-negative bacteria in intensive care unit. Sci Rep. 2013;2(4):707.
Kaur J, Chopra S, Sheevani Mahajan G. Modified double disc synergy test to detect ESBL production in urinary isolates of Escherichia coli and Klebsiella pneumonia. J Cli Diag Res. 2013;7(2):229–33.
Bourjilat F, Bouchrif B, Dersi N, Claude JD, Amarouch H, Timinouni M. Emergence of extended-spectrum beta-lactamase-producing Escherichia coli in community-acquired urinary infections in Casablanca, Morocco. J Infect Dev Ctries. 2011;5(12):850–5.
Aly MEA, Essam TM, Amin MA. Antibiotic resistance profile of Escherichiaa coli strains isolated from clinical specimens and food samples in Egypt. Int J Microbiol Res. 2012;3(3):176–82.
Acknowledgement
We, the author and co-authors are very grateful to all the patients from whom the clinical isolates were obtained. We also thank all the staffs of Microbiology Department of Chitwan Medical College Teaching Hospital (CMCTH) for their support to conduct the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SA conceived the design of the study and performed the experiments with help from SS and PN. HPN, RG and MLC guided the necessary laboratory tests. SA and GG reviewed the published literatures. SA wrote the manuscript and MLC and HPN guided the manuscript preparation. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ansari, S., Nepal, H.P., Gautam, R. et al. Community acquired multi-drug resistant clinical isolates of Escherichia coli in a tertiary care center of Nepal. Antimicrob Resist Infect Control 4, 15 (2015). https://doi.org/10.1186/s13756-015-0059-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-015-0059-2