Abstract
Background
This study aimed to synthetize the evidence on the effectiveness of harm minimization interventions on reducing blood-borne infection transmission and injecting behaviors among people who inject drugs (PWID) through a comprehensive overview of systematic reviews and evidence gap mapping.
Methods
A systematic review was conducted with searches in PubMed and Scopus to identify systematic reviews assessing the impact of interventions aimed at reducing the harms associated with injectable drug use. The overall characteristics of the studies were extracted and their methodological quality was assessed using AMSTAR-2. An evidence gap map was constructed, highlighting the most frequently reported outcomes by intervention (CRD42023387713).
Results
Thirty-three systematic reviews were included. Of these, 14 (42.2%) assessed the impact of needle/syringe exchange programs (NSEP) and 11 (33.3%) examined opioid agonist therapy (OAT). These interventions are likely to be associated with reductions of HIV/HCV incidence (10–40% risk reduction for NSEP; 50–60% for OAT) and sharing injecting paraphernalia (50% for NSEP, 25–85% for OAT), particularly when combined (moderate evidence). Behavioral/educational interventions were assessed in 12 reviews (36.4%) with most authors in favor/partially in favor of the use of these approaches (moderate evidence). Take-home naloxone programs and supervised-injection facilities were each assessed in two studies (6.1%), which reported inconclusive results (limited/inconsistent evidence). Most authors reported high levels of heterogeneity and risk of bias. Other interventions and outcomes were inadequately reported. Most systematic reviews presented low or critically low quality.
Conclusion
The evidence is sufficient to support the effectiveness of OAT, NSEP and their combination in reducing blood-borne infection transmission and certain injecting behaviors among PWID. However, evidence of other harm minimizations interventions in different settings and for some outcomes remain insufficient.
Similar content being viewed by others
Introduction
Injecting drugs remains a substantial contributor to global morbidity and mortality. While the patterns of drugs injected have changed, injecting behaviors have, in general, been on the decline in several regions for the past decade. Globally, out of the more than 12 million people who inject drugs (PWID), approximately 6 million are living with acquired blood-borne infectious diseases, particularly caused by the human immunodeficiency virus—HIV (accounting for 12.5% of new infections) and hepatitis B and C virus (HBV, HCV) (20–40% of cases) [1,2,3]. Unsafe drug practices among PWID are also associated with higher risk of overdose and drug-related fatalities [1, 2]. It is estimated that 20.5% (95% CI, 15.0–26.1%) and 41.5% (95% CI, 34.6–48.4%) of PWID have experienced at least one non-fatal overdose in the previous 12 months and in their lifetime, respectively [4]. Pooled crude mortality rates among PWID are 2.35 deaths per 100 person-years (95% CI 2.12–2.58) [5]. Furthermore, drug use places additional burdens on PWID and the society at large, including healthcare costs, efforts to combat crime, and lost productivity, [6].
Over the past 35 years, many countries have developed policy and public health initiatives aimed at addressing the health, societal, and economic adverse consequences of drug use [7, 8]. In addition to outreach programs and rehabilitation clinics, strategies involving a range of providers have been implemented globally to reduce or minimize the harms associated with drug use for individuals who are not prepared to quit. [7, 9]. Some of the most common harm minimization interventions include: (i) providing naloxone (i.e., naloxone dispensing without an external prescription through take-home naloxone programs – THN); (ii) opioid agonist or substitution therapies – OAT/OST, including medications for opioid use disorders (MOUD) such as methadone; (iii) supply-reduction interventions for opioids (e.g., prescription monitoring programs, tamper-resistant formulations, and prescribing limits); (iv) non-prescription sales or provision of sterile syringes through needle and syringe exchange programs (NSEP), including within supervised drug consumption facilities or supervised injection facilities (SCF or SIF); and (v) integration of testing and treatment for blood-borne diseases through screening and point-of-care testing (i.e., diagnostic testing conducted outside a laboratory environment, generally at or near to the patient’s location) [10].
The literature is abundant with studies, including a dozen systematic reviews and meta-analyses that have assessed the impact of these interventions in improving drug-related harms. However, substantial variations in methods, outcome measures, and transparency of their reporting exist, which can lead to results suggesting interventions that may not be effective. Moreover, when interventions are implemented, they may not be adequately translated into practice or tailored to suit the relevant populations. While there are a limited number of literature overviews (i.e., systematic reviews of systematic reviews) available, they tend to focus on specific interventions (e.g., NSEP) and outcomes (e.g., HIV-related harms). These overviews are often outdated (last publications from 2022 including primary studies published until 2019–2020) and tend to concentrate on the broader category of people who use drugs. Furthermore, they may not thoroughly evaluate the roles of PWID and stakeholders on harm minimization initiatives (e.g., barriers to implementation and upscale) [11,12,13,14,15,16].
Considering the persistent global drug use crisis, coupled with strained healthcare resources and growing associated burdens, a pressing need for the implementation of higher-quality, scaled up evidence-based approaches in this field exists. These approaches are essential to facilitate informed decision-making and the development of strategies for future policy planning. This study aimed to answer the question ‘What is the extent and current state of evidence regarding the effectiveness of harm minimization interventions in reducing blood-borne infection transmission and injecting behaviors among PWID?’ This was accomplished through a comprehensive and up-to-date overview of systematic reviews and evidence gap mapping.
Methods
A systematic review of systematic reviews (overview or umbrella review) was conducted following the Joanna Briggs Institute and the Cochrane recommendations and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [17,18,19]. (Protocol PROSPERO—CRD42023387713).
Search and eligibility criteria
A systematic search was conducted in PubMed and Scopus without timeframe or language limits (updated December 2022). In addition, a manual search was performed in the reference lists of included studies, and conventional search engines (i.e., Google and Google Scholar). Search strategies are available in the Supplementary Material.
Studies retrieved were organized into Endnote X7 and duplicate records removed. Two reviewers conducted independent screening (title/abstract reading) and full-text evaluation using Microsoft Excel 2013. Data extraction and methodological quality assessment for the included studies were performed by a single reviewer and verified by another. Discrepancies were addressed through discussion involving a third reviewer.
This review included articles: (i) published peer-reviewed systematic reviews (with or without meta-analysis) that included primary studies of any design (interventional, observational); (ii) aimed at assessing the effects of any intervention, method, or approach (i.e., program, service, or study) provided by any professional with the aim of reducing or minimizing harm associated with injectable drug use in any setting; and (iii) provided results related to the reduction or alterations of risk behaviors’ outcomes, such as illicit opioid use, overdose, drug-related fatalities, injecting behavior, sharing of needle/syringe or equipment, as well as HIV and HCV incidence or prevalence rates. Study protocols, overviews, articles that were restricted to people who use drugs without differentiation of results for PWID, and studies written in non-Roman characters were excluded.
Data extraction and quality assessment
To collect data, we used a standardized data collection form. This form was used to extract: general characteristics of the reviews (authors, publication year, sample size [number and design of included studies]); type of intervention and comparator (when available); setting; main reported outcomes and results.
The methodological quality of the studies was evaluated using the A MeaSurement Tool to Assess systematic Reviews (AMSTAR-2), designated to assess the quality of the systematic reviews of both randomized and non-randomized studies of health interventions [20]. AMSTAR-2 comprises 16 domains, and for each domain reviewers provide answers among ‘yes’, ‘partial yes’, ‘no’, ‘not applicable’. The quality rating is determined by identifying the weaknesses in the critical domains, and the final score enables grading and ranking methodological quality, ranging from ‘critically low’ to ‘high’.
Data synthesis and evidence gap mapping
The individual results of the studies and effect-size measures were summarized considering the information provided by the authors. The outcomes were measured using different effect size metrics, including: odds ratio (OR), adjusted odds ratio (aOR), standardized mean difference (SMD), risk ratio (RR), weighted mean (WM). Confidence interval (CI) of effect size measures was collected, along with the information about the level of statistical significance and heterogeneity between studies (I2 index) when reported.
The findings were ultimately synthesized into an evidence gap map, considering the most frequently reported outcomes and the methodological quality of the systematic reviews for each intervention. This approach provides a visual summary of the breadth and availability of information within a specific area and the gaps in the current evidence, which may ground further research, and policy development [21].
Results
Studies’ overall characteristics and methodological quality
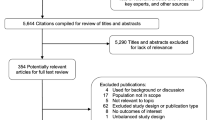
A total of 275 records were retrieved from the databases after duplicates removal. Following screening, 61 articles were considered for full-text analysis, and 31 studies met the eligibility criteria for data extraction. Four studies were added through manual searches, totaling 35 included studies (see Fig. 1) [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56]. Excluded studies are available in the Supplementary Material.
The 35 articles report 33 systematic reviews published between 1998 and 2021, of which16 (48.5%) are qualitative systematic reviews, and 17 (51.5%) include statistical analyses (i.e., meta-analysis or meta-synthesis). These systematic reviews encompassed various primary study designs, most of which assessed as having low-moderate methodological quality (i.e., moderate or high risk of bias). The most frequently evaluated outcomes were the incidence and prevalence of HIV and HCV, overall risk behavior (including sexual risk behavior, injecting behavior or drug use), injecting behavior (including reusing of syringes, injecting outdoors, and rushing injections), injection drug use, sharing of needles/syringes, and illicit opioid use. Conversely, assessments of drug treatment entry, overdose rates, and drug-related fatalities were limited (Table 1).
The methodological quality assessment of the included systematic reviews using AMSTAR 2 is summarized in Table 2. Most studies (n = 17; 51.5%) presented low quality. Shortcomings included instances where authors did not: provide the list of excluded studies and justified these exclusions (item 7); employ a technique for assessing the risk of bias in primary studies (item 9); report the sources of funding (item 10); account for risk of bias in individual studies when interpreting or discussing the results (item 13); offer explanation for, or discussion of, observed heterogeneity in the results (item 14). In contrast, 6 studies (18.2%) were rated as having high methodological quality. These studies reported various interventions, including behavioral or psychosocial interventions [39, 42], NSEP [23, 24], OAT [35], and both NSEP and OAT [53, 54]).
NSEP and OAT
Approximately one-third of studies (n = 9; 27.3%) exclusively evaluated the impact of NSEP on PWID. Five of these had moderate or high methodological quality, while four had critically low or low methodological quality. OAT on its own was assessed in six reviews (18.2%), two with moderate or high methodological quality and four with critically low or low quality. Five studies (12.1%) compared the effects of NSEP, OAT, and their combination in reducing drug-injecting related harms. Among these, three had moderate or high methodological quality, and two had critically low quality. The most frequently reported outcomes were related to the transmission of HIV/HCV.
Considering authors’ conclusions, most studies were in favor or partially in favor of these interventions (i.e., benefits for some outcomes) in various settings. Specifically, 71.4% of the studies on NSEP and 100% on OAT indicated positive results, including benefits in reducing HIV transmission and prevalence, HCV prevalence, and risk behaviors such as sharing needles/syringes (Table 1). Only one review (Jones et al. 2010) [28] (low methodological quality) concluded that there were no significant benefits from NSEP (outcomes of injecting behavior, incidence of blood borne viral infections and drug treatment entry). Three other studies (21.4%), two with high or moderate methodological quality, and one with critically low quality, were inconclusive. In these reviews, there was no consistent association between NSEP and its impact, primarily due to high between-studies heterogeneity, low methodological quality, and inconsistent data (e.g., non-standardized outcomes to enable comparisons)[24, 26, 27].
According to the meta-analyses performed by Hagan et al. [50], Platt et al. [52,53,54], and Turner et al. [55] (respectively moderate, high and moderate methodological quality), the use of OAT was associated with significant reductions in HCV incidence. RR ranged from 0.60 [95% CI 0.35–1.03] (I2 = 45%) to RR 0.50 [95% CI 0.40–0.63] (I2 = 0%). Additionally, an aOR of 0.41 [0.21–0.82], was reported. In contrast, NSEP yielded less significant and yet more heterogeneous results for this outcome (results ranged from RR 1.62 [95% CI, 1.04–2.52] (I2 = 81%) to RR 0.79 [95% CI 0.39–1.61] (I2 = 77%) and an aOR 0.48 [95% CI 0.25–0.93]). These meta-analyses indicated that multi-component interventions (e.g., NSEP and OAT) can contribute to a substantial reduction in the risk of acquiring HCV (around 75–80%). The authors suggested that this reduction is likely attributable to the OAT component.
Aspinall et al. [23] and MacArthur et al. [35] (both high methodological quality) reported significant reductions of HIV transmission with NSEP and OAT in health settings (RR 0.42 [95% 0.22–0.81] (I2 = 79%), and RR 0.60 [95% 0.42–0.85] (I2 = 23%), respectively). However, Hedrich et al. [32] (low methodological quality) found no significant effects of OAT on HCV/HIV incidence in prison settings.
Sawangjit et al. [30] and Cross et al. [49] (respectively moderate and low methodological quality) reported favorable results of NSEP on reducing sharing needles/syringes (OR 0.50 [95% CI 0.34–0.73]; I2 = 60%) and overall risk behaviors (weighted mean 0.279 [95% CI 0.207–0.352]). Reductions in sharing paraphernalia, ranging from 25 to 86%, were observed by Gowing et al. [31] and Larney et al. [34] (respectively moderate and low methodological quality) following the implementation of OAT. According to the meta-analysis by Moore et al. 2019 (low methodological quality), OAT was also significantly associated with a reduction in illicit opioid use (including in prisons) [36] (OR 0.22 [95% CI 0.15–0.32], I2 = 0%). These findings were consistent with Gowing et al. [31] and Larney et al. [34] with reduction rates ranging from 32 to 91%.
Behavioral and psychosocial interventions
Behavioral, psychological, or educational/engagement interventions were focused in seven studies (21.2%) (four with moderate or high and three with critically low methodological quality). Five additional studies compared the effectiveness of these interventions with other approaches (e.g., OAT) (one with moderate and four with critically low or low methodological quality). Most authors (75.0%) were in favor of the use of behavioral interventions for reducing at least one injecting behavior in PWID.
Deuba et al. [38] (moderate methodological quality) concluded that behavioral, psychological, and educational/engagement strategies were not effective for reducing unsafe injection practices and HIV prevalence among PWID, especially in low-income settings. In contrast, a systematic review by Sacks-Davis et al. 2012 (high methodological quality) [42] suggested that behavioral approaches may have some effects on reducing HCV transmission. However, the review noted significant variations among observational studies in terms of design, outcomes, magnitude/direction, and statistical significance, which resulted in inconclusive data. Gilchrist et al. [39] and Semaan et al. [43] (respectively high and critically low methodological quality) found evidence that psychological and behavioral strategies were associated with reductions in sexual risk behaviors (SMD − 0.19 [95% CI − 0.30, 0.01], I2 = 58%, and OR 0.86 [95% CI 0.76–0.98]; I2 = 47%, respectively), and sharing paraphernalia (SMD − 0.43 [95% CI, − 0.69 to − 0.18], I2 = 68%). However, a high level of between-studies heterogeneity was reported. Other authors did not find significant results favoring these interventions.
SCF/SIF
Naloxone access programs (i.e., THN) and supervised facilities (SCF or SIF) were evaluated in only two studies (6.1%) each, all of which reported inconclusive results on the benefits for PWID. This inconclusiveness is caused by limited data, such as the availability of few observational studies [ranging from five to nine] for each outcome of interest, inconsistent comparisons (THN or SIF vs. various controls), and variations in outcomes across primary studies. Kennedy et al. 2017 and Levengood et al. 2021 (respectively critically low and moderate methodological quality) [44, 45] suggested that supervised facilities might mitigate some overdose-related harms, with around 75–80% of studies reporting a reduction in related morbidity and mortality rates, and a reduction in unsafe drug use (approximately 85% reported a reduction of injecting behaviors). However, other outcomes including sexual risk behaviors and crime or public nuisance in the surrounding community require further medium and long-term studies. Similarly, evidence by McAuley et al. [46] and McDonald et al. [47] (respectively critically low and moderate methodological quality) from observational studies demonstrated that THN programs may reduce overdose mortality with a low rate of adverse events, but other outcomes in this setting are poorly reported. This evidence is further limited by the evaluation design and number of successful reversals. Only one systematic review without meta-analysis by Bouzanis et al. [48] (critically low methodological quality) mentioned the use of point-of-care HIV/HCV testing and treatment interventions, such as integrated multidisciplinary HIV and HCV care, supportive housing models, and addiction treatments for this population. Results should be carefully approached given the limitations in primary studies, including lack of randomization, self-reported measurements, and challenges in data generalizability (i.e., experiences often specific to PWID).
Table 3 summarizes the findings of this overview by means of an evidence gap map. The most reported outcomes were categorized as: HIV incidence/transmission, HIV prevalence, HCV incidence/transmission, HCV prevalence, overall risk behavior, illicit opioid use, injecting behavior, injection drug use, sharing needles/syringes, drug treatment entry, overdose, and deaths.
Discussion
This overview synthetized and critically appraised the methodological quality of 33 systematic reviews and meta-analyses published between 1998 and 2021 that assessed the effectiveness of harm minimization interventions (categorized into NSEP, OAT, behavioral/educational interventions, SCF or SIF, THN and combined approaches) in reducing risk behaviors associated with injecting drug use. These findings update and expand existing knowledge derived from previous overviews and may inform policy makers, practitioners and other stakeholders about the risk–benefit- ratio of these interventions for PWID, and underpin the development or improvement of guidance for implementation and upscale [57].
The inception of harm reduction policy emerged primarily as a response to the HIV/AIDS outbreak, shifting from an approach focusing on changing addictive behaviors to encompass broader public safety measures (e.g., reforming criminal policies) and harm reduction strategies to reduce the likelihood of individuals acquiring blood borne diseases, drug-related morbidity and fatality [58, 59]. These strategies should be implemented within a comprehensive public health framework, characterized by a pragmatic and humanistic approach and grounded on evidence-based evaluations [59, 60].
While over 90 countries had at least one harm reduction program implemented by [61], current debates revolve around the long-term cost-effectiveness of these interventions (or their combination) tailored to individual scenarios [59, 60]. As highlighted in our overview, despite numerous publications, the evidence seems primarily derived from low to moderate quality studies, with significant heterogeneity, inconsistent data (e.g., lack of standardized interventions, unclear adjustments for confounders) and relatively short follow-up periods. These factors hampered statistical evaluations in over 45% of the systematic reviews. Among the systematic reviews including statistical synthesis, the evidence was inconclusive in approximately 12% and partially in favor of the intervention (i.e., benefits found only for some outcomes) in around 40%.More than half of the systematic reviews presented low methodological quality, marked by differences in methods, outcomes, and transparency of report. Among the six high-quality systematic reviews, five reported at least one benefit in favor of the interventions, either NSEP [23], OAT [35, 52,53,54] or behavioral and psychosocial interventions [39]. The remaining two high-quality studies reported conflicting evidence [24, 42]. Previous studies have suggested that weak evidence, including studies with methodological flaws and high risk of bias, along with misleading and conflicting reports, can lead to biased recommendations and potentially distort decision-making. [62,63,64]. We advocate for the development of a core outcome set (COS), which entails a consensus-derived collection of outcomes and instruments to enable consistent measurement and reporting of harm minimization interventions [65, 66].
The World Health Organization (WHO) recommends targets for harm minimization interventions, including the distribution of 300 needles per PWID per year, the provision of OAT to more than 40 people per 100 PWID and viral hepatitis vaccination. However, these targets may fall short for meeting the needs of PWID daily or more frequently, estimated to correspond to 68.1% (95% CI 64.5–71.6%) on a global scale [67]. Moreover, 18% of PWID engage in receptive needle/syringe sharing at their last injection [68, 69]. A multinational study pointed to 33 (uncertainty interval [UI], 21–50) needle-syringes distributed via NSEP per PWID annually and 16 (UI, 10–24) OAT recipients per 100 PWID, significantly below recommendations [15, 68].
NSEP aims to advise PWID on safe injection practices, overdose prevention, and to facilitate referrals to treatment of drug use disorders. While evidence of NSEP on reducing HIV transmission and sharing needles/syringes can be graded as ‘sufficient’, it is often ‘inconsistent’ for HCV infection, other overall risk behaviors, and mortality [70,71,72]. This variability in findings may result from the intricacies of NSEP interventions, varied implementation and performance, differences across settings and geographical regions, all of which can lead to an over- or underestimation of the true effect of these programs in real-world [73,74,75]. These conclusions align with previous overviews by Fernandes et al. [11] (n = 13 systematic reviews) and Palmateer et al. [12] (n = 27 reviews), both reporting mixed results for NSEP. These authors highlighted that comprehensive harm reduction interventions at structural level and within multi-component programs may be associated with further significant benefits, likely due to the OAT component. In fact, according to the United Nations Office on Drugs and Crime and the WHO, interventions for reducing or eliminating HCV should be integrated, designed for simplified service delivery with a public health approach, and should include target HCV testing, care and treatments with direct-acting antivirals [76, 77]. The meta-analysis by Platt et al. 2017/2018 (high methodological quality) found a 74% reduction in the risk of HCV associated with the uptake of combined OAT with high coverage NSEP when compared to no OAT and low coverage or no NSEP (RR 0.26 [95% CI 0.07–0.89], based on studies presenting adjusted effect sizes). This effect size is larger than the one observed for OAT or NSEP alone (RR 0.50 [95% CI 0.40–0.63] and RR 0.79 [95% CI 0.39–1.61], respectively) [52,53,54]. OAT services aim to replace illicit drug use with medically prescribed, orally administered opiates such as buprenorphine or methadone. Their availability is increasing in prisons, as noted in our overview [78]. Nevertheless, additional research is needed to gain a better understanding of the impact of OAT in humanistic, social and economic outcomes.
Behavioral and psychosocial interventions are designed to address the psychological and social aspects of drug use. and are often delivered together with OAT by public institutions or non-governmental organizations, typically in outpatient settings [79]. Although with critically low or low methodological quality, the systematic reviews by Semaan et al., Copenhaver et al. and Meader et al. [37, 40, 43] concurred in suggesting that these interventions are effective in reducing risk behaviors. This effect was notable when associated with sexual exposure, suggesting that brief standard education can be a treatment option alongside other elective interventions in community outreach programs [22]. Our evidence gap map highlights the need for further evaluation of the impact of these interventions on more objective outcomes such as the transmission of blood-borne diseases, overdose rates, and drug-related fatalities. This is critical because behavioral outcomes are often self-reported, which may introduce reporting bias [12, 80].
In recent years, SCF or SIF have increasingly been implemented, particularly in areas characterized by frequent injecting in public places. They are designed to provide PWID with sterile injecting equipment, offer counselling services (before, during and after consumption), emergency care in the event of overdose, and facilitate referral to various forms of care [44, 45]. However, the evidence on SCF/SIF effectiveness is insufficient, primarily due to the lack of standardized outcomes and comparators. It may be necessary to consider intermediate outcomes (e.g., changes in practices) jointly with epidemiological data when evaluating interventions without a comparator. Other benefits such as number of diagnostics and immunization, referrals to detoxification, and decreased use of medical services, should be explored [48].
Our overview reveals a similar pattern of inconclusive findings from systematic reviews of low to moderate methodological quality on the impact of THN programs on PWID. THN programs’ primary aim is to reduce or prevent overdoses by providing users with training and naloxone kits. While previous studies demonstrated THN programs’ potential association with increased rates of overdose survival and successful overdose reversals [47, 81, 82], the review by Ansari et al. 2020 found mixed evidence [83].
Despite recent recommendations from WHO advocating decentralized, integrated and task-sharing services employing point-of-care viral load assays and reflex viral load testing to reduce HCV/HIV related harms in key populations, the evidence-base found in our study for point-of-care testing is inconclusive [77, 84].
Research should prioritize further methodologically robust primary studies on the impact of harm reduction interventions on HCV and specific subpopulations (e.g., prison). Studies focusing on standardization of outcomes related to drug overdose, mortality and injecting behaviors are essential to improve the evidence-base. Interrupted time series analyses have proven to be suitable to evaluate the effects of policy initiatives and could be used to assess the impact of harm minimization [85]. The literature on the long-term cost-effectiveness of these programs, particularly in community-based settings, remains heterogenous and somewhat inconclusive, which may be a barrier to program implementation and participant enrollment [83, 86]. Implementation of harm minimization may face external barriers (e.g., low political prioritization, inadequate coordination and integration, limited advocacy, and conflicting intersectoral policies). Additionally, stigma, ethical issues, and changes in drug consumption patterns pose challenges in participant engagement/acceptance, and program evaluation in real-world settings [87, 88]. This means that strategies and policies should be constantly adapted and innovated to address these evolving patterns and align with the culture and population characteristics [78, 89].
Our study has limitations. We did not assess the overlap of systematic reviews as it was not our primary objective. We used the AMSTAR-2, as it is a valid and reliable tool [20]. However, other approaches as the Risk Of Bias In Systematic Reviews (ROBIS) could yield similar results. The conclusions of the systematic reviews were considered as presented by authors, meaning that evidence may not be immediately transposed to different scenarios/settings and geographical regions. The critical appraisal of this overview may contain elements of subjectivity, which we tried to minimize by conducting a comprehensive systematic review (with no limitations on outcomes) according to international guidelines of conduct and report.
Conclusions
The body of empirical findings synthetized in this overview, along with the evidence gap map, provides sufficient evidence to primarily support the role of OAT, NSEP, and especially their combination in reducing HIV/HCV transmission and some injecting risk behaviors among PWID. Further evaluations of objective outcomes, such as overdoses and drug-related fatality, should be explored in both short and long-term studies. Behavioral or psychological interventions were associated with reductions in sexual risk behaviors and, thus, should be considered as part of a structural-level approach. This approach focusses on strategies that aim to modify social conditions and arrangements by addressing the key drivers of HIV/HCV vulnerability through policy, legal, and environmental changes, as well as the empowerment of communities and groups for this population. Evidence on the effect of other harm minimization interventions, namely SCF or SIF and THN, as well as evidence in other settings or contexts remain insufficient. The impact of combined strategies is challenging to assess, since one or more components of interventions may contribute to the reduction of harmful outcomes. Therefore, further well-designed observational studies with standardized COS and consistent measurement of exposure to single interventions or the intensity of harm minimization interventions are needed to strengthen these findings.
Disclosures
FAC works as a consultant for the World Health Organization, Regional Office for Europe. The author alone is responsible for the views expressed in this publication and these do not necessarily represent the decisions or the stated policy of the World Health Organization.
Availability of data and materials
All data is available upon reasonable request to the authors.
References
Elflein J. Global drug use—statistics & facts. 2021. https://www.statistacom/topics/7786/global-drug-use/#dossierKeyfigures.
European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2021: trends and developments. Publications Office of the European Union – Luxembourg. 2021. https://www.emcdda.europa.eu/publications/edr/trends-developments/2021_en.
Grebely J, Larney S, Peacock A, Colledge S, Leung J, Hickman M, et al. Global, regional, and country-level estimates of hepatitis C infection among people who have recently injected drugs. Addiction. 2019;114(1):150–66.
Colledge S, Peacock A, Leung J, Larney S, Grebely J, Hickman M, et al. The prevalence of non-fatal overdose among people who inject drugs: a multi-stage systematic review and meta-analysis. Int J Drug Policy. 2019;73:172–84.
Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91(2):102–23.
Marshall Z, Dechman MK, Minichiello A, Alcock L, Harris GE. Peering into the literature: a systematic review of the roles of people who inject drugs in harm reduction initiatives. Drug Alcohol Depend. 2015;151:1–14.
Department of Health - Australian Government. Topic 6: Harm minimisation in AOD work. Module 5: young people, society and AOD: learner's workbook. 2004. www.health.gov.au.
Lennings CJ. Harm minimization or abstinence: an evaluation of current policies and practices in the treatment and control of intravenous drug using groups in Australia. Disabil Rehabil. 2000;22(1–2):57–64.
Zinberg N. Drug, set and setting: the basis for controlled intoxicant use. Boston: Yale University Press; 1984.
Batra S, Connealy M, Xavier J. Chapter 7—point-of-care testing. In: Shesser R, Pourmand A, Keim A, editors. The emergency department technician handbook. New Delhi: Elsevier; 2024. p. 43–51.
Fernandes RM, Cary M, Duarte G, Jesus G, Alarcao J, Torre C, et al. Effectiveness of needle and syringe Programmes in people who inject drugs—an overview of systematic reviews. BMC Public Health. 2017;17(1):309.
Palmateer N, Hamill V, Bergenstrom A, Bloomfield H, Gordon L, Stone J, et al. Interventions to prevent HIV and Hepatitis C among people who inject drugs: latest evidence of effectiveness from a systematic review (2011 to 2020). Int J Drug Policy. 2022;109:103872.
MacArthur GJ, van Velzen E, Palmateer N, Kimber J, Pharris A, Hope V, et al. Interventions to prevent HIV and Hepatitis C in people who inject drugs: a review of reviews to assess evidence of effectiveness. Int J Drug Policy. 2014;25(1):34–52.
Puzhko S, Eisenberg MJ, Filion KB, Windle SB, Hebert-Losier A, Gore G, et al. Effectiveness of interventions for prevention of common infections among opioid users: a systematic review of systematic reviews. Front Public Health. 2022;10:749033.
Larney S, Peacock A, Leung J, Colledge S, Hickman M, Vickerman P, et al. Global, regional, and country-level coverage of interventions to prevent and manage HIV and hepatitis C among people who inject drugs: a systematic review. Lancet Glob Health. 2017;5(12):e1208–20.
Mbuagbaw L, Hajizadeh A, Wang A, Mertz D, Lawson DO, Smieja M, et al. Overview of systematic reviews on strategies to improve treatment initiation, adherence to antiretroviral therapy and retention in care for people living with HIV: part 1. BMJ Open. 2020;10(9):e034793.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons, 2019.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Aromataris E, Munn Z. JBI manual for evidence synthesis. 2020.. https://synthesismanual.jbi.global.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Snilstveit B, Vojtkova M, Bhavsar A, Stevenson J, Gaarder M. Evidence & Gap Maps: a tool for promoting evidence informed policy and strategic research agendas. J Clin Epidemiol. 2016;79:120–9.
Abdul-Quader AS, Feelemyer J, Modi S, Stein ES, Briceno A, Semaan S, et al. Effectiveness of structural-level needle/syringe programs to reduce HCV and HIV infection among people who inject drugs: a systematic review. AIDS Behav. 2013;17(9):2878–92.
Aspinall EJ, Nambiar D, Goldberg DJ, Hickman M, Weir A, Van Velzen E, et al. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis. Int J Epidemiol. 2014;43(1):235–48.
Davis SM, Daily S, Kristjansson AL, Kelley GA, Zullig K, Baus A, et al. Needle exchange programs for the prevention of hepatitis C virus infection in people who inject drugs: a systematic review with meta-analysis. Harm Reduct J. 2017;14(1):25.
Des Jarlais DC, Feelemyer JP, Modi SN, Abdul-Quader A, Hagan H. High coverage needle/syringe programs for people who inject drugs in low and middle income countries: a systematic review. BMC Public Health. 2013;13:53.
Gibson DR, Flynn NM, Perales D. Effectiveness of syringe exchange programs in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS. 2001;15(11):1329–41.
Gillies M, Palmateer N, Hutchinson S, Ahmed S, Taylor A, Goldberg D. The provision of non-needle/syringe drug injecting paraphernalia in the primary prevention of HCV among IDU: a systematic review. BMC Public Health. 2010;10:721.
Jones L, Pickering L, Sumnall H, McVeigh J, Bellis MA. Optimal provision of needle and syringe programmes for injecting drug users: A systematic review. Int J Drug Policy. 2010;21(5):335–42.
Ksobiech K. Beyond needle sharing: meta-analyses of social context risk behaviors of injection drug users attending needle exchange programs. Subst Use Misuse. 2006;41(10–12):1379–94.
Sawangjit R, Khan TM, Chaiyakunapruk N. Effectiveness of pharmacy-based needle/syringe exchange programme for people who inject drugs: a systematic review and meta-analysis. Addiction. 2017;112(2):236–47.
Gowing L, Farrell MF, Bornemann R, Sullivan LE, Ali R. Oral substitution treatment of injecting opioid users for prevention of HIV infection. Cochrane Database Syst Rev. 2011;8:CD004145.
Hedrich D, Alves P, Farrell M, Stover H, Moller L, Mayet S. The effectiveness of opioid maintenance treatment in prison settings: a systematic review. Addiction. 2012;107(3):501–17.
Karki P, Shrestha R, Huedo-Medina TB, Copenhaver M. The impact of methadone maintenance treatment on HIV risk behaviors among high-risk injection drug users: a systematic review. Evid Based Med Public Health. 2016;2:e1229.
Larney S. Does opioid substitution treatment in prisons reduce injecting-related HIV risk behaviours? A systematic review. Addiction. 2010;105(2):216–23.
MacArthur GJ, Minozzi S, Martin N, Vickerman P, Deren S, Bruneau J, et al. Opiate substitution treatment and HIV transmission in people who inject drugs: systematic review and meta-analysis. BMJ. 2012;345:e5945.
Moore KE, Roberts W, Reid HH, Smith KMZ, Oberleitner LMS, McKee SA. Effectiveness of medication assisted treatment for opioid use in prison and jail settings: a meta-analysis and systematic review. J Subst Abuse Treat. 2019;99:32–43.
Copenhaver MM, Johnson BT, Lee IC, Harman JJ, Carey MP, Team SR. Behavioral HIV risk reduction among people who inject drugs: meta-analytic evidence of efficacy. J Subst Abuse Treat. 2006;31(2):163–71.
Deuba K, Sapkota D, Shrestha U, Shrestha R, Rawal BB, Badal K, et al. Effectiveness of interventions for changing HIV related risk behaviours among key populations in low-income setting: a meta-analysis, 2001–2016. Sci Rep. 2020;10(1):2197.
Gilchrist G, Swan D, Widyaratna K, Marquez-Arrico JE, Hughes E, Mdege ND, et al. A systematic review and meta-analysis of psychosocial interventions to reduce drug and sexual blood borne virus risk behaviours among people who inject drugs. AIDS Behav. 2017;21(7):1791–811.
Meader N, Li R, Des Jarlais DC, Pilling S. Psychosocial interventions for reducing injection and sexual risk behaviour for preventing HIV in drug users. Cochrane Database Syst Rev. 2010;2010(1):CD007192.
Prendergast ML, Urada D, Podus D. Meta-analysis of HIV risk-reduction interventions within drug abuse treatment programs. J Consult Clin Psychol. 2001;69(3):389–405.
Sacks-Davis R, Horyniak D, Grebely J, Hellard M. Behavioural interventions for preventing hepatitis C infection in people who inject drugs: a global systematic review. Int J Drug Policy. 2012;23(3):176–84.
Semaan S, Des Jarlais DC, Sogolow E, Johnson WD, Hedges LV, Ramirez G, et al. A meta-analysis of the effect of HIV prevention interventions on the sex behaviors of drug users in the United States. J Acquir Immune Defic Syndr. 2002;30(Suppl 1):S73-93.
Kennedy MC, Karamouzian M, Kerr T. Public health and public order outcomes associated with supervised drug consumption facilities: a systematic review. Curr HIV/AIDS Rep. 2017;14(5):161–83.
Levengood TW, Yoon GH, Davoust MJ, Ogden SN, Marshall BDL, Cahill SR, et al. Supervised injection facilities as harm reduction: a systematic review. Am J Prev Med. 2021;61(5):738–49.
McAuley A, Aucott L, Matheson C. Exploring the life-saving potential of naloxone: a systematic review and descriptive meta-analysis of take home naloxone (THN) programmes for opioid users. Int J Drug Policy. 2015;26(12):1183–8.
McDonald R, Strang J. Are take-home naloxone programmes effective? Systematic review utilizing application of the Bradford Hill criteria. Addiction. 2016;111(7):1177–87.
Bouzanis K, Joshi S, Lokker C, Pavalagantharajah S, Qiu Y, Sidhu H, et al. Health programmes and services addressing the prevention and management of infectious diseases in people who inject drugs in Canada: a systematic integrative review. BMJ Open. 2021;11(9):e047511.
Cross J, Saunder C, Bartelli D. The effectiveness of educational and needle exchange programs: a meta-analysis of HIV prevention strategies for injecting drug users. Qual Quant. 1998;32:165–80.
Hagan H, Pouget ER, Des Jarlais DC. A systematic review and meta-analysis of interventions to prevent hepatitis C virus infection in people who inject drugs. J Infect Dis. 2011;204(1):74–83.
McNeil R, Small W. “Safer environment interventions”: a qualitative synthesis of the experiences and perceptions of people who inject drugs. Soc Sci Med. 2014;106:151–8.
Platt L, Sweeney S, Ward Z, Guinness L, Hickman M, Hope V, et al. Assessing the impact and cost-effectiveness of needle and syringe provision and opioid substitution therapy on hepatitis C transmission among people who inject drugs in the UK: an analysis of pooled data sets and economic modelling. Southampton: Public Health Research; 2017.
Platt L, Minozzi S, Reed J, Vickerman P, Hagan H, French C, et al. Needle and syringe programmes and opioid substitution therapy for preventing HCV transmission among people who inject drugs: findings from a Cochrane Review and meta-analysis. Addiction. 2018;113(3):545–63.
Platt L, Minozzi S, Reed J, Vickerman P, Hagan H, French C, et al. Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database Syst Rev. 2017;9:CD012021.
Turner KM, Hutchinson S, Vickerman P, Hope V, Craine N, Palmateer N, et al. The impact of needle and syringe provision and opiate substitution therapy on the incidence of hepatitis C virus in injecting drug users: pooling of UK evidence. Addiction. 2011;106(11):1978–88.
Wright NM, Tompkins CN. A review of the evidence for the effectiveness of primary prevention interventions for hepatitis C among injecting drug users. Harm Reduct J. 2006;3:27.
EMCDDA. ECDC and EMCDDA guidance. Prevention and control of infectious diseases among people who inject drugs. 2022. https://www.emcddaeuropaeu/publications/ecdc-emcdda-guidance_en.
McKeganey N. The lure and the loss of harm reduction in UK drug policy and practice. Addict Res Theory. 2006;14(6):557–88.
Steenholdt D, Colquhoun R, Varcoe S. 30 Years of harm minimization—how far have we come? Evidence based review of the influence and impact on drug use in Australia under the ‘Harm Minimisation Strategy. Dalgarno Institute. 2015. https://www.unodc.org/documents/ungass2016/Contributions/Civil/Dalgarno/30Years_of_HarmMinimisation_FinalUNGASS.pdf.
Davoli M, Simon R, Griffiths P. European Monitoring Centre for Drugs and Drug Addiction—EMCDDA. Harm reduction: evidence, impacts and challenges. Current and future perspectives on harm reduction in the European Union. 2010. https://www.emcddaeuropaeu/publications/monographs/harm-reduction_en.
Harm Reduction International—HRI. The global state of harm reduction. 2020. https://www.hriglobal/files/2021/03/04/Global_State_HRI_2020_BOOK_FA_Webpdf.
Ioannidis JP. The mass production of redundant, misleading, and conflicted systematic reviews and meta-analyses. Milbank Q. 2016;94(3):485–514.
Page MJ, Altman DG, Shamseer L, McKenzie JE, Ahmadzai N, Wolfe D, et al. Reproducible research practices are underused in systematic reviews of biomedical interventions. J Clin Epidemiol. 2018;94:8–18.
Bonetti AF, Tonin FS, Lucchetta RC, Pontarolo R, Fernandez-Llimos F. Methodological standards for conducting and reporting meta-analyses: Ensuring the replicability of meta-analyses of pharmacist-led medication review. Res Soc Adm Pharm. 2022;18(2):2259–68.
Kirkham JJ, Williamson P. Core outcome sets in medical research. BMJ Med. 2022;1(1):e000284.
Webbe J, Sinha I, Gale C. Core outcome sets. Arch Dis Child Educ Pract Ed. 2018;103(3):163–6.
World Health Organization (WHO). 2017. Action plan for the health sector response to viral hepatitis in the WHO European Region—World Health Organization. Regional Office for Europe. https://apps.whoint/iris/handle/10665/344154.
Colledge S, Leung J, Larney S, Peacock A, Grebely J, Hickman M, et al. Frequency of injecting among people who inject drugs: a systematic review and meta-analysis. Int J Drug Policy. 2020;76: 102619.
Tran LT, Peacock A, Colledge S, Memedovic S, Grebely J, Leung J, et al. Injecting risk behaviours amongst people who inject drugs: a global multi-stage systematic review and meta-analysis. Int J Drug Policy. 2020;84:102866.
van Ameijden EJ, Coutinho RA. Maximum impact of HIV prevention measures targeted at injecting drug users. AIDS. 1998;12(6):625–33.
Thakarar K, Sankar N, Murray K, Lucas FL, Burris D, Smith RP. Injections and infections: understanding syringe service program utilization in a rural state. Harm Reduct J. 2021;18(1):74.
U.S. Agency for International Development—USAID. Needle and syringe programs rigorous evidence—usable results USAID. 2010. https://www.jhsphedu/research/centers-and-institutes/research-to-prevention/publications/needleandsyringepdf.
Logez S, Hutin Y, Somda P, Thuault J, Holloway K. Safer injections following a new national medicine policy in the public sector, Burkina Faso 1995–2000. BMC Public Health. 2005;5:136.
Heinzerling KG, Kral AH, Flynn NM, Anderson RL, Scott A, Gilbert ML, et al. Unmet need for recommended preventive health services among clients of California syringe exchange programs: implications for quality improvement. Drug Alcohol Depend. 2006;81(2):167–78.
Kwon JA, Iversen J, Law M, Dolan K, Wand H, Maher L. Estimating the number of people who inject drugs and syringe coverage in Australia, 2005–2016. Drug Alcohol Depend. 2019;197:108–14.
World Health Organization (WHO), United Nations Office on Drugs and Crime (UNODC). Implementing comprehensive HIV and HCV programmes with People Who Inject Drugs—Practical Guidance for Collaborative Interventions. 2017. https://www.unodcorg/documents/hiv-aids/publications/Implementing_Comprehensive_HIV_and_HCV_Programmes_with_People_Who_Inject_Drugs_PRACTICAL_GUIDANCE_FOR_COLLABORATIVE_INTERVENTIONSpdf.
World Health Organization (WHO). Updated recommendations on simplified service delivery and diagnostics for hepatitis C infection. 2022. https://www.whoint/publications/i/item/9789240052697.
Roy E, Arruda N, Leclerc P, Morissette C, Blanchette C, Blouin K, et al. Drug use practices among people who inject drugs in a context of drug market changes: challenges for optimal coverage of harm reduction programs. Int J Drug Policy. 2017;45:18–24.
Merson MH, Dayton JM, O’Reilly K. Effectiveness of HIV prevention interventions in developing countries. AIDS. 2000;14(Suppl 2):S68-84.
Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51(3):253–63 (discussion 67-8).
Bird SM, McAuley A, Perry S, Hunter C. Effectiveness of Scotland’s National Naloxone Programme for reducing opioid-related deaths: a before (2006–10) versus after (2011–13) comparison. Addiction. 2016;111(5):883–91.
Chronister KJ, Lintzeris N, Jackson A, Ivan M, Dietze PM, Lenton S, et al. Findings and lessons learnt from implementing Australia’s first health service based take-home naloxone program. Drug Alcohol Rev. 2018;37(4):464–71.
Ansari B, Tote KM, Rosenberg ES, Martin EG. A rapid review of the impact of systems-level policies and interventions on population-level outcomes related to the opioid epidemic, United States and Canada, 2014–2018. Public Health Rep. 2020;135(1_suppl):100S-S127.
World Health Organization (WHO). Consolidated guidelines on HIV, viral hepatitis and STI prevention, diagnosis, treatment and care for key populations. 2022. https://www.whoint/publications/i/item/9789240052390.
Lopez Bernal J, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol. 2018;47(6):2082–93.
Mueller SR, Walley AY, Calcaterra SL, Glanz JM, Binswanger IA. A review of opioid overdose prevention and naloxone prescribing: implications for translating community programming into clinical practice. Subst Abus. 2015;36(2):240–53.
Irwin KS, Fry CL. Strengthening drug policy and practice through ethics engagement: an old challenge for a new harm reduction. Int J Drug Policy. 2007;18(2):75–83.
Stockings E, Hall WD, Lynskey M, Morley KI, Reavley N, Strang J, et al. Prevention, early intervention, harm reduction, and treatment of substance use in young people. Lancet Psychiatry. 2016;3(3):280–96.
Greene MC, Kane JC, Khoshnood K, Ventevogel P, Tol WA. Challenges and opportunities for implementation of substance misuse interventions in conflict-affected populations. Harm Reduct J. 2018;15(1):58.
Acknowledgements
This study was supported in part by UIDB/04138/2020 and UIDP/04138/2020—from FCT to iMed.ULisboa.
Funding
No funding has been obtained for this study.
Author information
Authors and Affiliations
Contributions
FST: Data curation, Formal analysis, Investigation, Visualization, Writing- Original draft preparation. FF-L: Methodology, Software, Validation, Visualization, Reviewing and Editing. FAC: Conceptualization, Investigation, Reviewing and Editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have contributed to this manuscript, have read and approved its final version and agreed to its submission and publication.
Competing interests
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tonin, F.S., Alves da Costa, F. & Fernandez-Llimos, F. Impact of harm minimization interventions on reducing blood-borne infection transmission and some injecting behaviors among people who inject drugs: an overview and evidence gap mapping. Addict Sci Clin Pract 19, 9 (2024). https://doi.org/10.1186/s13722-024-00439-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13722-024-00439-9