Abstract
Background
Long-term care insurance (LTCI) was implemented in China to solve the elderly care problems caused by the aging population. It is crucial to evaluate the effectiveness of LTCI implementation from the perspective of value-based healthcare.
Objective
This study aimed to investigate the impact of LTCI on medical care expenditure and health status in China.
Methods
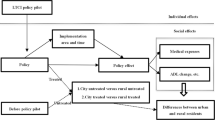
We used staggered difference-in-differences (DID) analysis to analyze the effect of LTCI policy on medical expenditure and health status based on China Health and Retirement Longitudinal Study data from 2011 to 2018.
Results
Our findings confirmed the positive contribution of LTCI policies to medical expenditures and health status. We found that the implementation of LTCI significantly reduced inpatient and outpatient expenditure, scores of self-report of health, and CESD scores by 26.3%, 12.3%, 0.103, and 0.538, respectively. It also decreased ADL scores, but the decrease was not significant. The impact of LTCI on reducing inpatient expenditure was greater for individuals aged between 65 and 80 and those residing in urban areas and eastern cities. In terms of outpatient costs, the effect of LTCI was more pronounced among median and high-income people and people living in central and eastern cities. The impact of LTCI on self-report of health is stronger for rural populations, individuals under 80, and those in central and eastern cities. For ADL scores, LTCI affected those aged 65–80 the most. About the CESD scores, LTCI had a greater impact on rural populations, people aged 45–65, median income groups, and those in eastern cities.
Conclusions
Our study underscored LTCI’s effectiveness in curbing medical expenditures and enhancing health status, offering valuable insights for future LTCI development in China and beyond. Accelerating the development of LTCI is conducive to improving the quality of life of the disabled elderly, enhancing the well-being of people’s livelihoods, and realizing the goal of value-based healthcare.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Text box 1. Contributions to the literature |
|---|
• There is limited evidence on the contribution of long-term care insurance to the medical expenditure and health status of middle-aged and elderly people from the perspective of value-based care. |
• There is limited evidence on how the effects of long-term care insurance policies differ among middle-aged and elderly people of different ages, urban and rural areas, regions, and household incomes. |
• There is an urgent need for health policies to improve the long-term care insurance policy system in order to further enhance the value of health care services for middle-aged and elderly people, especially in developing countries. |
Introduction
The global shift towards an aging population poses unprecedented challenges, with over 1 billion individuals expected to be aged 65 and above by 2030 [1]. China, home to the largest population over 65, faces a mounting crisis in its healthcare system due to accelerated aging [2]. One of the notable impacts of an aging population is the increase in the number of disabled and demented elderly, with projections foreseeing over 57% of the total disabled population and a staggering 77.65 million individuals by 2030 [3]. However, many families lack sufficient time and expertise to care for their family members [4]. The reliance on expensive tertiary hospitals for unmet long-term care needs exacerbates medical expenditures and hospital congestion [5, 6]. The elderly with unmet long-term care needs face lower quality of life, increased psychological distress, and higher mortality rates [7,8,9,10].
Long-term care insurance (LTCI) has emerged as a pivotal financial instrument amid the backdrop of an aging populace, where the welfare and prosperity of the middle-aged and elderly constituents have assumed paramount importance [11]. To solve the problems of the aging population, such as aging at home, medical care instead of nursing care, and unmet health needs, the LTCI policies were implemented in many cities in China [12]. In July 2012, Qingdao was the first city to start piloting LTCI within the urban area. Subsequently, in 2015, this bold attempt was extended outward to rural areas [13]. On June 27, 2016, the Ministry of Human Resources and Social Security (MOHRSS) announced that it was launching a pilot program for LTCI in 15 districts, an important initiative that was fully rolled out in 2017 [14]. The LTCI system is waiting for the full maturity of various favorable conditions and will be fully rolled out nationwide.
LTCI in China is a social insurance program initiated and implemented by the Chinese government. It is an important part of China’s social security system and is characterized as a welfare-oriented, mutual-aid, and mandatory social insurance. LTCI aims to meet the care needs of individuals who required long-term care services due to disability or old age, to mitigate the economic risks associated with receiving long-term healthcare services, and to improve their health status. LTCI targets individuals enrolled in Urban Employee Basic Medical Insurance (UEBMI) and/or Urban-Rural Resident Basic Medical Insurance (URRBMI). It provides basic living care and reimburses medical services for severely disabled persons bedridden for six months or more. Service modes include hospital care, institutional care, and home care. Most pilot cities use a “service payment” approach, reimbursing eligible nursing care expenses either at a fixed amount or proportionally, based on incapacity level and service type. By 2021, the number of pilot cities for LTCI had increased to 49, with over 140 million insured and more than 1 million receiving treatment.
Navigating towards “value-based healthcare” becomes imperative for sustainable development. The purpose of LTCI is to reduce the medical expenditure of insured individuals while also improving their health status, which aligns with the concept of “value-based healthcare.” In the realm of health services, value is redefined as the monetary investment in achieving health outcomes [15]. For individuals, the value of healthcare services lies in obtaining medical services at a lower cost while significantly improving their health status. Therefore, to better evaluate the policy effects of LTCI based on value-based healthcare, this study assessed the policy effects of LTCI from the perspective of both medical expenditure and health status of insured individuals. In terms of measuring the medical expenditure of insured individuals, this study selected two indicators: inpatient expenditure and outpatient expenditure. For assessing the health status of insured individuals, the study selected three indicators: self-report of health, ADL (Activities of Daily Living) scores, and CESD (Center for Epidemiological Studies Depression Scale) scores. Self-report of health reflects subjective health status, while ADL scores and CESD scores objectively reflect physical and mental health status, respectively. This comprehensive approach allows for a thorough assessment of the health status of insured individuals from both subjective and objective, as well as physical and mental perspectives. These indicators for measuring medical expenditure and health status were also commonly used by previous researchers to study the policy effects of LTCI [4, 12, 16,17,18], representing a comprehensive and representative system of indicators.
With the acceleration of the aging process, the physical and mental health of middle-aged and elderly people has attracted much attention. A large number of studies have shown that the provision of tailored LTC services to meet the needs of older adults in activities of daily living can effectively enhance health [19,20,21]. At the same time, encouraging the utilization of LTC services, will not only reduce the elderly’s reliance on hospital care services and improve their health but also serve to control medical expenditures. Amid accelerating promotion and deepening policy design, studying the impact of LTCI on medical expenditures and health holds theoretical and practical significance.
The impact of LTCI on medical expenditures and health status is still uncertain, and academics have yet to reach a unified conclusion. There are two main arguments against the impact of LTCI on medical expenditures: On the one hand, there is a substitution relationship between LTCI and medical expenditures. Gade et al. [22] found that LTCI provides medical care to critically ill patients, reducing ICU use and hospital stays, and achieving expenditures reduction. Studies found that LTCI in the U.S. reduces care costs, relieves elderly patients’ financial burden, and saves outpatient expenditure [23, 24]. Feng et al. [12] conducted an empirical study using Shanghai data to examine the impact of LTCI on medical utilization and expenditures, showing that additional spending on LTCI reduces health insurance expenditures by RMB 8.6. On the other hand, it is argued that LTCI has no impact on health care services and expenditures or has the effect of freeing up medical expenditures. Wooldridge and Schore [25] analyzed the use of hospitals and nursing homes in the U.S. and found that the decline or lack of decline in the number of nursing home residents did not affect the hospital’s operating figures. Mcknight [26] found that home care expenditures offset a portion of out-of-pocket medical expenditures, and therefore did not achieve the goal of medical expenditures containment.
The ultimate goal of LTCI must be to improve the health of the population. Na and Streim [27] suggested that older adults with higher levels of ADL Disability Index limitations are more socially isolated and have poorer mental health. Therefore, helping to improve the level of disablement and increase social support through LTC can help to reduce the likelihood of isolation and depression. Tang et al. [28] have found through research that self-report health, activities of daily living (ADLs), and mental health improved after the implementation of LTCI. Cao et al. [29] utilized the CHARLS database from 2011 to 2018 thus finding that the implementation of LTCI policies has a positive impact on reducing the incidence of disability in people over 45 years of age.
In summary, due to differences in research perspectives, research methods, and other factors, existing research conclusions on the impact of LTCI policies on medical expenditure and physical and mental health are often inconsistent. Additionally, there is a lack of research on the effectiveness of LTCI policies in developing countries among scholars. This study extended the survey to provincial pilot cities beyond the traditional 15 national LTCI pilots. The study addressed a gap in empirical scholarship by thoroughly exploring how LTCI relates to both physical and mental health. The paper skillfully integrated a value-based perspective on healthcare while incorporating self-report of health, ADL scores, and CESD scores as key variables that intertwine medical expenditures with impacts on physical and mental health. The heterogeneity analysis explored the impact of LTCI on different populations from different perspectives. The findings offer valuable guidance for policymakers, healthcare practitioners, and researchers to improve policies and meet the needs of the global aging population.
Methods
Data source and samples
We draw our data from the China Health and Retirement Longitudinal Study (CHARLS). CHARLS is a large nationwide survey project led by the National School of Development at Peking University and executed by the China Center for Economic Research. It aims to study various aspects of China’s elderly population aged 45 and over, including their social, health, and economic circumstances [30]. The project employed a multistage sampling approach, utilizing the probability proportional to size (PPS) sampling method at the county/district and village/community stages [31]. The nationwide baseline survey was conducted in 2011, followed by subsequent tracking surveys every two years. CHARLS has collected cross-sectional data for five waves so far (In 2011, 2013, 2015, 2018, and 2020, respectively).
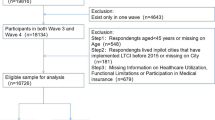
First, we merged the first four-wave cross-sectional data of CHARLS into panel data, resulting in a sample size of 77,233 (The 2020 wave data was excluded because it lacked the key medical expenditure variables required for this study due to the COVID-19 epidemic). Since our study focused on middle-aged and elderly individuals, we excluded samples with ages less than 45. In order to ensure that the treatment cities were indeed affected by the LTCI policy, this study selected samples from cities that had implemented LTCI for at least 6 months before August, 2018 (CHARLS wave4), as the treatment group. Figure 1 shows the treatment cities in this study. The control group was composed of samples from cities that had not implemented LTCI before August, 2018. Samples from the city of Weihai, which implemented LTCI between February 1, 2018, and August 1, 2018, were excluded. Furthermore, we eliminated samples with missing values in age and dependent variables, as well as samples with only one follow-up, resulting in a final sample size of 37,771. For covariates with missing values, we employed the random forest imputation method to impute these missing values. Figure 2 illustrates the sample processing procedure in our study.
Outcome variable
To evaluate the effects of LTCI from the perspective of value-based healthcare, this study selected outcome variables from the CHARLS dataset based on the two most critical aspects of value-based healthcare: medical expenditure and health outcomes. The selected variables included inpatient expenditure, outpatient expenditure, self-report of health, ADL scores, and CESD scores. Inpatient expenditure and outpatient expenditure respectively reflect the total inpatient medical expenditure incurred over the past year and the total outpatient medical expenditure incurred over the past month, including the portion paid by insurance.Inpatient expenditure and outpatient expenditure were subjected to a natural log transformation to normalize their distribution. Self-report of health reflects the respondents’ evaluation of their health status. In CHARLS, respondents are asked, “How do you rate your current health status?” There are five options: 1 represents very good, 2 represents good, 3 represents fair, 4 represents poor, and 5 represents very poor. ADL scores reflect the respondents’ ability to perform daily activities. In CHARLS, respondents are asked about any difficulties they encounter in performing 11 daily activities, such as bathing, dressing, cooking, etc. There are four answer options for each question: 1 indicates no difficulty, 2 indicates difficulty but still able to complete independently, 3 indicates difficulty and requiring assistance, and 4 indicates inability to complete. By summing up the answers to these 11 questions, ADL scores of the respondents are obtained. CESD scores reflect the respondents’ level of depression. CHARLS adopts the Center for Epidemiologic Studies Depression Scale to measure the degree of depression in respondents. This scale consists of 10 questions regarding depressive symptoms, with four answers for each question: 0 for “almost none”, 1 for “sometimes”, 2 for “often”, and 3 for “most of the time”. By summing up the answers to these 10 questions, CESD scores of the respondents are obtained. Lower values in the three variables, self-report of health, ADL scores, and CESD scores, all indicate better health status of the respondent.
Independent variable
The main dependent variable in this study is the coverage of LTCI (DID), which represents whether the samples are from cities where LTCI has been implemented for at least 6 months. DID is an interaction term between “treat” and “post”. “treat” is a binary variable used to distinguish the treatment group. In this study, for samples from treatment cities (Qingdao, Weifang, Liaocheng, Anqing, etc.), “treat” is assigned a value of 1. “post” is a binary variable used to differentiate between the periods before and after policy implementation. In this study, since Qingdao implemented LTCI in 2012, and Weifang and Liaocheng implemented LTCI in January 2015, the “post” variable is assigned a value of 1 for the samples from Qingdao in 2013, 2015, and 2018, and the samples from Weifang and Liaocheng in 2015 and 2018. For the samples from other cities in 2018, the “post” variable is assigned a value of 1.
Covariates
According to the Andersen model of healthcare service utilization, healthcare utilization behavior is influenced by factors such as demographic characteristics and socioeconomic status [32]. Therefore, this study includes individual demographic variables, socioeconomic status variables, and health level variables as covariates. Individual demographic covariates include age, gender, residence, marital status, type of BMI, region, and number of children alive. Socioeconomic status covariates include education and income. Health level covariates include drink, smoke, and chronic disease. Appendix 1 presents the outcome variables and covariates used in this study along with their definitions.
Statistical analysis
To assess the impact of the implementation of LTCI on the healthcare burden and health status of the objects, due to the LTCI being implemented at different times in the treatment cities, following previous research [17, 33], this study employed a staggered difference-in-differences model that incorporates individual fixed effects and time fixed effect:
Yijt represents the outcome variables in this study, including Ln (Inpatient expenditure + 1), Ln (Outpatient expenditure + 1), Self-report of health, ADL scores, and CESD scores. i represents an individual. j represents the city where the individual resides, and t represents time or the year. DIDijt (an interaction term between the dummy variables “treat” and “post”) represents the coverage of LTCI. Xijt represents covariates. λt represents individual fixed effects. ϖt represents the random error term. The coefficient β is the focus of this study, reflecting the magnitude of the LTCI policy effect.
One important prerequisite for a staggered difference-in-differences analysis is that the trend in the outcome variables between the treatment and control groups remains the same before the policy implementation. Following the research methodology proposed by previous study [34], this study employed the Event Study Analysis (ESA) to conduct a common trends test, using the − 1 period (baseline) as the benchmark group, to examine the policy effects of LTCI.
In the case of a large sample, there is a potential endogeneity issue in the staggered difference-in-differences analysis due to selection bias. To mitigate the endogeneity arising from the implementation of LTCI, following a previous study [35], this study employed the Propensity Score Matching (PSM) method in conjunction with staggered difference-in-differences model to further examine the policy effects. We used covariates from the staggered difference-in-differences model as matching variables in PSM, employing logistic regression and nearest-neighbor matching to match two control group samples for each treatment group sample. We assessed the matching effectiveness by comparing the kernel density curves before and after matching. Subsequently, we conducted the staggered difference-in-differences analysis using the matched samples (samples with common trends) and compared the results with the previous findings to test the robustness of the earlier results.
To assess the robustness of the staggered difference-in-differences results, this study further employed staggered difference-in-differences analysis with out-of-pocket inpatient expenditure (log-transformed), out-of-pocket outpatient expenditure (log-transformed), inpatient frequency, and outpatient frequency as outcome variables.
To assess the policy effects of LTCI in different populations, this study conducted a heterogeneity analysis of the policy effects of LTCI from the perspective of individual characteristics within the sample. This study categorized the samples into different subgroups based on urban/rural residence, age, income, and region to examine the policy effects of LTCI across these subgroups.
Results
Descriptive statistics
Table 1 displays the descriptive statistics of the treatment group before and after the implementation of the LTCI policy. In the main outcome variables, the mean values of Ln (outpatient expenditure + 1), the score of self-report of health, and CESD scores decreased after the implementation of LTCI. On the other hand, the mean values of Ln (inpatient expenditure + 1) and ADL scores increased after the implementation of LTCI. However, a simple comparison of the mean values of outcome variables before and after policy implementation did not necessarily indicate the policy effect of LTCI. In the following section, a staggered difference-in-differences model would be used to further validate the findings.
Table 2 displays the descriptive statistics of the control group in each wave of CHARLS data. The control group in the study showed a rising trend in Ln (outpatient expenditure + 1) and ADL scores, indicating an overall increase in outpatient expenditure and a decrease in the overall level of disability. No significant changes were observed in other outcome variables.
Main effect of LTCI
Table 3 displays the effect of LTCI on medical expenditure and health status of the objects, with the coefficients of the DID representing the magnitude of the effects. From the table, we can observe that, compared to cities without LTCI implementation, cities with LTCI significantly reduced the medical expenditure of the objects. Inpatient expenditure decreased by 26.3% at the 1% significance level, and outpatient expenditure decreased by 12.3% at the 10% significance level. Furthermore, the health status of the objects in LTCI-implemented cities showed significant improvement compared to those without LTCI. Lower values in the variables reflecting health status indicate better health status. Scores of self-report of health significantly decreased by 0.103 at the 1% significance level. CESD scores significantly decreased by 0.538 at the 1% significance level, indicating a significant improvement in mental health. ADL scores also decreased by 0.028, indicating some improvement in physical health, although not statistically significant.
According to the research findings, LTCI indeed significantly reduced medical expenditure for middle-aged and elderly individuals in implementing cities while improving their health status.
Common trend test
Figure 3 displays the results of the common trends test. To avoid collinearity, the − 1 group was removed as the benchmark group. From the figure, it can be observed that before the implementation of LTCI, the point estimates of policy effects for various outcome variables fluctuated around 0, and the 95% confidence intervals all included 0. This indicated that before the implementation of LTCI, there were no significant differences in the changing trends of outcome variables between the treatment group and the control group, satisfying the common trends assumption.
Common trend test. The horizontal axis represents a particular year relative to the year of policy implementation, with 0 indicating the year of policy implementation. The vertical axis represents the magnitude of the coefficient, and the dashed line range represents the 95% confidence interval of the coefficient
PSM-DID
Figure 4 presents the results of Propensity Score Matching (PSM). Before matching, there was a substantial difference in the kernel density distribution of propensity scores between the treatment group and the control group. After matching, the kernel density curves of propensity scores for the treatment and control groups became much closer, and their means were more similar, indicating a successful matching process.
Table 4 displays the results of PSM-DID. After matching, the effect of LTCI on medical expenditure and the health status of the objects remained similar to the previous results. Compared to the control group, the treatment group exhibits a significant 27.3% reduction in inpatient expenditure at the 1% significance level, a significant 0.106 decrease in scores of self-report of health at the 1% significance level, and a significant 0.548 decrease in CESD score at the 1% significance level. Additionally, outpatient expenditure decreased by 12% and ADL scores decreased by 0.018, but these results were not statistically significant. The results of the PSM-DID analysis are consistent with the main effect results of LTCI, demonstrating the robustness of the earlier findings on the main effect of LTCI.
Effect of LTCI on out-of-pocket medical expenditure and medical services utilization frequency
Table 5 presents the effect of LTCI on out-of-pocket medical expenditure and medical services utilization frequency of the objects. Compared to the control group, the objects in the treatment group experienced a significant 21.8% reduction in out-of-pocket inpatient expenditure at the 5% significance level, a significant 0.062 reduction in inpatient frequency at the 1% significance level, and a significant 0.146 reduction in outpatient visit frequency at the 1% significance level. Additionally, outpatient out-of-pocket expenditure decreased by 10.6%, although not statistically significant. These results indicated that the implementation of LTCI did indeed lead to a reduction in out-of-pocket medical expenditure and inpatient and outpatient visit frequency of the objects, thus confirming the robustness of the main effect of LTCI.
Heterogeneity
Figure 5 and Appendix 2 show the results of heterogeneity analysis. From the perspective of urban/rural residence, the effect of LTCI on reducing medical expenditure was more significant in urban areas compared to rural areas. In urban areas, the inpatient expenditure significantly decreased by 33.4%. In contrast, the effect of LTCI on improving health status was more significant in rural areas compared to urban areas. In rural areas, Scores of self-report of health significantly decreased by 0.152, and CESD scores significantly decreased by 0.789.
Regarding age, the effects of LTCI on reducing medical expenditure and improving health status were more significant among objects aged 65–80. For the elderly aged 65–80, inpatient expenditure significantly decreased by 58.7%. Scores of self-report of health significantly decreased by 0.119. ADL scores significantly decreased by 0.36, and CESD scores significantly decreased by 0.61.
In terms of income, the effect of LTCI on reducing medical expenditure was more significant among low-income and high-income objects compared to median-income objects. For low-income objects, inpatient expenditure significantly decreased by 74.2%. For high-income objects, inpatient expenditure and outpatient expenditure significantly decreased by 62% and 33.4%, respectively. In addition, the effect of LTCI on improving health status showed no significant difference among objects in three different income groups.
In terms of region, the effects of LTCI on reducing medical expenditure and improving health status were more significant in eastern cities. As for objects lived in eastern cities, inpatient expenditure and outpatient expenditure significantly decreased by 30.8% and 26.5%, respectively. Scores of self-report of health significantly decrease by 0.101, and CESD scores significantly decrease by 0.463. However, for objects living in western cities, the implementation of LTCI increased the inpatient expenditure significantly.
Heterogeneous effects of LTCI. The four graphs above indicate the heterogeneous effects of LTCI from the perspective of individual factors: urban/rural residence, age, income, and region. Each pair is based on a separate regression with interaction terms between LTCI and indicators for each subgroup. The regression model controls for fixed effects of time and individual. The dots mark the point estimates, and the lines indicate 95% confidence intervals
Discussion
This study analyzed the impact of LTCI on medical expenditures and physical and mental health using CHARLS follow-up data from 2011 to 2018. The results showed that the implementation of LTCI can effectively reduce medical expenditures without compromising individual health, which is in line with the spirit of “value-based healthcare”.
The decline in medical expenditures reflected the substitution effect of nursing services in LTCI replacing nursing services in health care facilities. The substitution effect refers to the fact that LTCI reduces the incidence of “social hospitalization” through the provision of in-home or institutional care, thereby reducing the cost of medical services by shifting patients who would otherwise receive care in hospitals to in-home or institutional care. Much of the literature before this concluded that such an alternative relationship existed. Two Korean studies found that LTCI policies significantly reduced personal healthcare expenditures for the elderly [36, 37]. Forder used UK data to estimate that among 75-year-olds, for every extra 1 pound spent in a nursing home, spending in a hospital is reduced by 0.35 pounds [38]. Choi conducted an in-depth study of healthcare costs and the use of healthcare resources among the elderly in Japan and found that LTCI holders had significantly fewer hospitalizations, shorter hospital stays, and significantly lower healthcare cost burdens [39]. Matsuda and Mejhert found that lower quality of life is the most important factor affecting medical expenditures for the elderly and that LTCI improves the quality of life of the elderly, thereby reducing healthcare costs [40, 41].
The empirical results showed that the implementation of LTCI had significantly reduced the hospital medical expenses of middle-aged and elderly people, which suggested that LTCI has indeed effectively promoted the substitution of home care and institutional care for hospital care services, and has effectively alleviated the burden of care costs on the elderly with disabilities. Viewing the objective of the pilot LTCI policy from the perspective of value-based healthcare, it is to reduce the rising trend of public medical expenditure on the one hand and to maintain and enhance the health status of the elderly or disabled on the other hand, that is to say, its health effect. The health effect refers to the fact that LTCI improves the health of beneficiaries, including both physical and mental health. Studies have been conducted to provide empirical evidence of the health effects of LTCI. Na and Streim’s study showed that high-quality LTCI interventions not only improve the health status and activities of daily living of older adults but also reduce mortality [27]. By analyzing longitudinal panel data on elderly people in Korea, Sohn.M et al. concluded that LTCI is effective in reducing mortality among the elderly [42]. Our study showed a 2.8% decrease in ADL scores, a statistically insignificant result that still provided some indication that LTC policies can be effective in improving activities of daily living.
The heterogeneity results showed that the reduction in inpatient expenditure for the objects in urban areas was higher than in rural areas during the implementation of the LTCI policy. This may be because the LTCI policy had not been able to achieve full and effective coverage in rural areas, resulting in a much lower degree of responsiveness to the policy in rural areas. In addition, urban areas were more directly affected by the policy, received greater financial support from the policy, were more likely to receive financial compensation, and the substitution effect of LTCI care services was more significant. A point of interest was that the health effects of the LTCI policy were more pronounced for the rural objects, with significant improvements in their self-report of health and CESD scores. This may be attributed to the increased susceptibility of rural populations to the psychological support and caring effects provided by LTCI policies. This psychological factor is likely to amplify the impact of LTCI on improving their health status. Therefore, the coverage of LTCI should be expanded as much as possible, and the successful experience of pilot cities should be extended to the whole country as soon as possible, to make full use of the function of LTCI in dispersing the pressure of caring for the target groups and improving their health.
In terms of age, the older the individual was, the greater the reduction in medical expenditure, especially for those aged 65–80 years, who had relatively high improvements in health status. It may be because such people usually pay more attention to health and take more health management measures. At the same time, due to differences in LTCI policies, some regions may give higher compensation to those who are older, thus reducing the medical expenditure borne by individual elderly people. Therefore, the LTCI policy should raise the level of compensation for the beneficiaries, so that the middle-aged and the elderly can improve their health through care services, reduce their use and consumption of medical services, give full play to the health and economic effects of LTCI, and realize “value-based healthcare”, and in the long run reduce the pressure on the operation of basic medical insurance.
On the income side, inpatient expenditure for middle-aged and elderly individuals from low-income and high-income families was significantly reduced, but the impact on middle-income families was not significant. Regarding system design, a bottom-up support mechanism has been adopted to a certain extent for objects from low-income families, taking into account the issue of equity. For objects from high-income families, the impact on medical expenditure was greater because of their relative financial well-being and relatively rational lifestyles (regular medical check-ups, self-medication, etc.). There was no significant difference in the impact of LTCI on the health of objects from different income families. The establishment of tiered levels of subsidy for different income groups will allow for more effective and rational risk control and improve the operational efficiency of the fund.
On the regional side, in the eastern cities, medical expenditures for the middle-aged and the elderly had dropped considerably and their health status had improved significantly. In western cities, the cost of hospitalization for objects had even increased significantly. This may be due to the different levels of economic development in the regions and the different levels of policy support for LTCI, which is similar to the differences in sensitivity between urban and rural areas to LTCI policies mentioned above. Therefore, it is possible to explore the establishment of a multi-level LTC protection system. For economically developed eastern regions, the development of commercial care insurance linked to LTCI can be encouraged to meet the diversified needs for long-term care protection; for central and western regions, at the initial stage of implementation, social forces can be leveraged to create a multi-level financing system through tax incentives and other policies.
This study used the first four-wave cross-sectional data of CHARLS to examine the impact of LTCI on the medical expenditure and health status of middle-aged and elderly people, bridging a gap in the research on the effects of LTCI in China in terms of a national study based on real-world evidence. Based on the value-based healthcare perspective, the study examined the impact of LTCI policies on the medical expenditure of middle-aged and elderly people, while at the same time examining the impact of LTCI on health status. However, our study also had some limitations: first, this study analyzed the pilot status of LTCI in the pilot cities only through policy information and lacked analysis of the specific implementation situation in the pilot cities. Second, the current study faced limitations stemming from the restricted scope of information within the CHARLS database, resulting in a relatively small sample size. It’s worth mentioning that the CHARLS database does not specifically focus on long-term care insurance policies. While this study narrowed down the data collection scope based on service recipients in each pilot city, there remains a potential for sample gaps and biases. Third, since this study was based on value-based healthcare and focused on the value of healthcare services received by individuals, the heterogeneity tests were centered on analyzing the differences in policy effects among different population groups based on individual characteristics. The differences in policy effects under different policy implementation models were not analyzed, indicating that there was potential for further expansion of the research content.
Conclusion
In summary, this study found that the implementation of LTCI had a positive and significant effect on inpatient expenditure, outpatient expenditure, self-report of health, and CESD for the middle-aged and elderly population in the pilot areas across the country. The results of this study further complement the existing empirical evidence on the effects of LTCI, supporting that LTCI has a positive overall effect on the health of middle-aged and elderly people while reducing medical expenditures. Therefore, LTCI is an initiative in line with “value-based healthcare”. This study provided important policy implications for the future development of LTCI policies.
Data availability
The original data is publicly available on the CHARLS website. The data analyzed in this study can be obtained by contacting the corresponding author for access.
Abbreviations
- ADL:
-
Activities of Daily Living
- BMI:
-
Basic Medical Insurance
- CESD:
-
Center for Epidemiological Studies Depression Scale
- CHARLS:
-
China Health and Retirement Longitudinal Study
- LTCI:
-
Long-term care insurance
- NRCMS:
-
New Rural Cooperative Medical Scheme
- UEBMI:
-
Urban Employee Basic Medical Insurance
- URMBI:
-
Urban Resident Basic Medical Insurance
- URRBMI:
-
Urban and Rural Resident Basic Medical Insurance
References
Chen L-K. Urbanization and population aging: converging trends of demographic transitions in modern world. Arch Gerontol Geriatr. 2022;101:104709.
Lu J, Liu Q. Four decades of studies on population aging in China. China Popul Dev Stud. 2019;3(1):24–36.
Luo Y, Su B, Zheng X. Trends and challenges for Population and Health during Population Aging - China, 2015–2050. China CDC Wkly. 2021;3(28):593–8.
Deng X, Liao J, Peng R, Chen J. The impact of long-term Care Insurance on Medical utilization and expenditures: evidence from Jingmen, China. Int J Environ Res Public Health. 2022;19(19).
Gaughan J, Gravelle H, Siciliani L. Testing the Bed-blocking hypothesis: does nursing and Care Home Supply reduce delayed Hospital discharges? Health Econ. 2015;24:32–44.
Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. 2019;394(10204):1192–204.
Gibson MJ, Satyendra KV. Just getting by: Unmet Needs for Personal Assistance Services among Persons 50 or older with disabilities. AARP, Public Policy Institute; 2006.
Komisar HL, Feder J, Kasper JD. Unmet long-term care needs: an analysis of Medicare-Medicaid dual eligibles. Inquiry: J Med care Organ Provis Financing. 2005;42(2):171–82.
Quail JM, Wolfson C, Lippman A. Unmet need for assistance to perform activities of daily living and psychological distress in community-dwelling elderly women. Can J Aging = La Revue Canadienne Du Vieillissement. 2011;30(4):591–602.
Zhen Z, Feng Q, Gu D. The impacts of Unmet needs for long-term care on Mortality among older adults in China. J Disabil Policy Stud. 2013;25(4):243–51.
Chen L, Zhang L, Xu X. Review of evolution of the public long-term care insurance (LTCI) system in different countries: influence and challenge. BMC Health Serv Res. 2020;20(1):1057.
Feng J, Wang Z, Yu Y. Does long-term care insurance reduce hospital utilization and medical expenditures? Evidence from China. Soc Sci Med. 2020;258:113081.
Yang W, Chang S, Zhang W, Wang R, Mossialos E, Wu X, et al. An initial analysis of the effects of a long-term Care Insurance on Equity and Efficiency: a case study of Qingdao City in China. Res Aging. 2021;43(3–4):156–65.
Zhou W, Dai W. Shifting from Fragmentation to Integration: a systematic analysis of long-term Care Insurance policies in China. Int J Integr Care. 2021.
Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–81.
Wang JY, Guan J, Wang GJ. Impact of long-term care insurance on the health status of middle-aged and older adults. Health Econ. 2023;32(3):558–73.
Lei XY, Bai C, Hong JP, Liu H. Long-term care insurance and the well-being of older adults and their families: evidence from China. Volume 296. Social Science & Medicine; 2022.
Luo YN, Yuan KX, Li YX, Liu YT, Pan Y. The spillover effect of long-term care insurance in China on spouses’ health and well-being. Volume 340. SOCIAL SCIENCE & MEDICINE; 2024.
Andrew N, Meeks S. Fulfilled preferences, perceived control, life satisfaction, and loneliness in elderly long-term care residents. Aging Ment Health. 2018;22(2):183–9.
Choi NG, McDougall G. Unmet needs and depressive symptoms among low-income older adults. J Gerontol Soc Work. 2009;52(6):567–83.
Ji L, Qiao X, Jin Y, Si H, Liu X, Wang C. Functional disability mediates the relationship between pain and depression among community-dwelling older adults: age and sex as moderators. Geriatr Nurs. 2021;42(1):137–44.
Glenn Gade IV, Douglas Conner K, McGrady J, Beane RH, Richardson MP, Williams. Marcia Liberson, Mark Blum, and Richard Della Penna. Impact Inpatient Palliat Care Team: Randomized Controlled Trial. 2008;11(2):180–90.
McCarthy IM, Robinson C, Huq S, Philastre M, Fine RL. Cost savings from palliative care teams and guidance for a financially viable palliative care program. Health Serv Res. 2015;50(1):217–36.
Penrod JD, Deb P, Dellenbaugh C, Burgess JF Jr., Zhu CW, Christiansen CL, et al. Hospital-based palliative care consultation: effects on hospital cost. J Palliat Med. 2010;13(8):973–9.
Wooldridge J, Schore J, The evaluation of the National Long Term Care Demonstration. 7. The effect of channeling on the use of nursing homes, hospitals, and other medical services. Health services research. 1988;23(1):119 – 27.
McKnight R. Home care reimbursement, long-term care utilization, and health outcomes. J Public Econ. 2006;90(1–2):293–323.
Na L, Streim JE. Psychosocial Well-Being Associated with activity of Daily Living stages among Community-Dwelling older adults. Gerontol Geriatric Med. 2017;3:2333721417700011.
Tang Y, Chen T, Zhao Y, Taghizadeh-Hesary F. The impact of the long-term Care Insurance on the medical expenses and Health Status in China. Front Public Health. 2022;10:847822.
Cao N, Shi T, Pan C. Does long-term care insurance reduce the disability among middle-aged and older adults? Evidence from China. BMC Public Health. 2023;23(1):1138.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
Chen X, Smith J, Strauss J, Wang Y, Zhao Y. China Health and Retirement Longitudinal Study (CHARLS). In: Pachana NA, editor. Encyclopedia of Geropsychology. Singapore: Springer Singapore; 2015. pp. 1–8.
Andersen RM. National health surveys and the behavioral model of health services use. Med Care. 2008;46(7):647–53.
Liu PC, Yang YL, Yang YX, Cheng JX. Different impact on health outcomes of long-term care insurance between urban and rural older residents in China. Sci Rep-Uk. 2023;13(1).
Nunn N, Qian N. The Potato’s contribution to Population and Urbanization: evidence from a historical experiment. Q J Econ. 2011;126(2):593–650.
Ma GB, Xu K. Value-Based Health Care: long-term Care Insurance for Out-of-Pocket Medical expenses and self-rated health. Int J Env Res Pub He. 2023;20(1).
Kim HB, Lim W. Long-term care insurance, informal care, and medical expenditures. J Public Econ. 2015;125:128–42.
Han NK, Chung W, Kim R, Lim S, Park C-Y, editors. Effect of the long-term care. Insurance Policy on Medical Expenditures for the Elderly; 2013.
Forder J. Long-term care and hospital utilisation by older people: an analysis of substitution rates. Health Econ. 2009;18(11):1322–38.
Choi JW, Park EC, Lee SG, Park S, Ryu HG, Kim TH. Does long-term care insurance reduce the burden of medical costs? A retrospective elderly cohort study. Geriatr Gerontol Int. 2018;18(12):1641–6.
Mejhert M, Lindgren P, Schill O, Edner M, Persson H, Kahan T. Long term health care consumption and cost expenditure in systolic heart failure. Eur J Intern Med. 2013;24(3):260–5.
Morrison RS, Dietrich J, Ladwig S, Quill T, Sacco J, Tangeman J, et al. Palliative care consultation teams cut hospital costs for Medicaid beneficiaries. Health Aff. 2011;30(3):454–63.
Moon S, Park HJ, Sohn M. The impact of long-term care service on total lifetime medical expenditure among older adults with dementia. Soc Sci Med. 2021;280:114072.
Acknowledgements
We would like to thank National School of Development at Peking University, the responsible unit of CHARLS, as well as all the interviewees who participated in the CHARLS survey.
Funding
This study is supported by the National Natural Science Foundation of China for the General Program “Research on the collaborative mechanism of medical insurance payment and compensation from the perspective of economic toxicity of cancer patients” (Approval number:72074090).
Author information
Authors and Affiliations
Contributions
Lan Yao and Yifan Yao conceived and designed this study. Yifan Yao, Shanshan Yin, and Wen Chen collated data. Yifan Yao, Shanshan Yin, Wen Chen, and Changli jia conducted the statistical analysis. Wen Chen and Shanshan Yin drafted the manuscript. Yifan Yao, Shanshan Yin, Wen Chen, and Lan Yao revised the manuscript critically. All authors contributed to this manuscript and approved the final version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The CHARLS is organized and implemented by the National School of Development at Peking University. It has obtained approval from the Biomedical Ethics Review Committee of Peking University (IRB00001052-11015). All respondents anonymously filled out questionnaires and provided written informed consent before the survey.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yin, S., Chen, W., Jia, C. et al. Effect of long-term care insurance on medical expenditure and health status: National cohort study. Arch Public Health 82, 152 (2024). https://doi.org/10.1186/s13690-024-01388-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-024-01388-0