Abstract
Background
The growing demand for LTC (Long-term care) services for disabled elderly has become a daunting task for countries worldwide, especially China, where population aging is particularly severe. According to CSY (China Statistical Yearbook,2019), the elderly aged 65 or above has reached 167 million in 2018, and the number of disabled elderly is as high as 54%. Germany and other countries have alleviated the crisis by promoting the public LTCI (Long-Term Care Insurance) system since the 1990s, while China’s public LTCI system formal pilot only started in 2016. Therefore, the development of the public LTCI system has gradually become a hot topic for scholars in various countries, including China.
Methods
This review has been systematically sorted the existing related literature to discuss the development of public LTCI (Long-Term Care Insurance)system form four aspects, namely, the comparison of public LTCI systems in different countries, the influence of public LTCI, challenge of public LTCI, and the relationship between public LTCI and private LTCI. We searched some databases including Web of Science Core Collection, Medline, SCOPUS, EBSCO, EMBASE, ProQuest and PubMed from January 2008 to September 2020. The quality of 38 quantitative and 21 qualitative articles was evaluated using the CASP(Critical Appraisal Skills Programme) critical evaluation checklist.
Results
The review systematically examines the development of public LTCI system from four aspects, namely, the comparison of public LTCI systems in different countries, the influence of public LTCI, the challenge of public LTCI, and the relationship between public LTCI and private LTCI. For example, LTCI has a positive effect on the health and life quality of the disabled elderly. However, the role of LTCI in alleviating the financial burden on families with the disabled elderly may be limited.
Conclusion
Some policy implications on the future development of China’s LTCI system can be obtained. For example, the government should fully consider the constraints such as price rise, the elderly disability rate, and the substantial economic burden. It also can strengthen the effective combination of public LTCI and private LTCI. It does not only help to expand the space for its theoretical research but also to learn the experiences in the practice of the LTCI system in various countries around the world. It will significantly help the smooth development and further promote the in-depth reform of the LTCI system in China.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The aging of the population has become a global problem. According to the World Population Outlook (2019) (WPP2019, United Nations Population Division), the Aging degree (proportion of the population aged 65 and above) of Japan, Italy, South Korea, and China will reach 28.4, 23.3, 15.8, and 12.0% respectively in 2020, while by 2050, the Aging degree of South Korea, Japan, Italy, and Germany will reach 38.1, 37.7, 36.0, and 30.0% respectively, and China will surge to 26.1%, which is equivalent to the average level of developed countries (26.9%). Subsequently, the cost of long-term care for the elderly who have lost their Activities of Daily Living (ADL) will bring a heavy economic burden to their families [1]. Therefore, the Long-term care insurance (LTCI) system came into being [2].
Long term care insurance (LTCI) system refers to an institutional arrangement to share the nursing expenses incurred by people who cannot take care of themselves due to chronic diseases or physical and psychological disability (WHO) [3]. From the perspective of whether it is compulsory or not, Long term care insurance (LTCI) system includes public-LTCI and private-LTCI. Private-LTCI exists as a supplement to public-LTCI, and its development is seriously insufficient. Therefore, at present, the focus of government and academic discussion is in the field of public-LTCI, which is also the main research object of this paper.
Practice of long-term care insurance (LTCI) system in different countries
Long-term care insurance (LTCI) system originated in European countries. The Netherlands was the first country that introduced a universal mandatory social health insurance scheme for covering a broad range of long-term care (LTC) services provided in a variety of care settings in the 1960s. Germany is the first country to implement public LTCI(Long-term care insurance) in the form of social legislation. In 1995, LTCI law came into effect and became the fifth pillar insurance after endowment insurance, medical insurance, accidental injury insurance, and unemployment insurance. Since then, the United States and other countries have also formally enacted public LTCI.
Japan and South Korea are the first countries to implement public LTCI in Asia. After the implementation of public LTCI system in Japan since 2000, it has gone through five major changes (2000, 2004, 2006, 2009, 2014), and has a careful design in the funding sources, identification procedures, and service content. According to the Japanese “ LTCI law”, the insured only pays 10% of the total nursing expenses when receiving long-term care services, and the remaining expenses are borne by 50% of the premium paid by the insured and 50% of the government’s public expenses. This way of financing can ensure that the family’s economic burden is not too heavy and not cause too much financial pressure, and ensure that the public LTCI system can be carried out persistently and stably. Korea has also implemented public LTCI to maintain and improve the health and well-being of the elderly since 2008.
The increasingly aging population has highlighted the urgency of the crisis in health care services for the elderly in China in recent years. According to CSY (China Statistical Yearbook,2019), the elderly aged 65 or above has reached 167 million in 2018, accounting for 11.9% of the total population. The ODR (Old-age dependency ratio) has climbed from 9.9% in 2000 to 16.8% in 2018. Among them, the number of disabled elderly due to chronic diseases, environmental pollution, accidental injuries, and natural aging is increasing, and the prevalence rate of chronic diseases in the elderly is as high as 54% [4,5,6,7,8]. Although the LTC (Long-Term Care) services demand for the elderly was snowballing, the provision of LTC (Long-Term Care) services such as policy formulation, operational models, and especially fundraising lag far behind. As a result, the “healthy China strategy” has been proposed in the Report of the 19th National Congress of China. At the same time, Government-mandated public LTCI (Long-Term Care Insurance) was piloted in 15 cities since 2016, including Qingdao of Shandong province, Chengdu of Sichuan province, and Chongqing, which had a profound impact on the people and economies of the pilot areas(as shown in Table 1).
Academic study of long-term care insurance (LTCI) system in different countries
Academic research on Long-term care insurance is carried out from two main lines: public LTCI and private LTCI. The research on private LTCI mainly focuses on the design of different types of LTCI insurance and people’s willingness to purchase private LTCI [9]. The research on public LTCI mainly focuses on two aspects. One is how to optimize the financing method to ensure the public LTCI can be carried out continuously and stably. The second is to discuss the effect of LTCI implementation on the health or financial burden of people who benefit from LTCI. For example, Choi & Joung used Cox proportional risk regression model to prove that LTCI (Long-Term Care Insurance) services can help reduce health expenditure and protect the health of the elderly aged 65 and above [10]. All the studies show that LTCI has a positive impact on the health of the disabled elderly, and the theoretical research is becoming more and more in-depth, which were conducted from the perspectives of different age groups, nursing time, and health recovery degrees. Etc.
Looking at the historical evolution of the Long-term care insurance system, we can find that although private LTCI is an important aspect of LTCI system, it is essentially only a supplement to public LTCI. Therefore, this paper only takes public LTCI as the research object to discuss the development of public LTCI system form four aspects, namely, the comparison of public LTCI systems in different countries, the influence of public LTCI, challenge of public LTCI, and the relationship between public LTCI and private LTCI.
Methods
The review aimed to show the influence and challenge of the public Long-Term Care Insurance (LTCI) System in Different Countries. By the way, we also discussed the development process of public LTCI in major countries (such as Germany, Japan, South Korea, and China) and its relationship with private LTCI.
Search process
The following main databases were taken into account: Web of Science Core Collection, Medline, SCOPUS, EBSCO, EMBASE, ProQuest and PubMed. Considering the regional limitations and the disorder of Chinese literature, CNKI(China) was not included in this literature search. The following combinations of terms were practiced with the Boolean phrase “and/or” to maximize the scope and type of material achieved in the search: ‘LTCI’ OR “Long Term Care Insurance”.
Inclusion and exclusion criteria
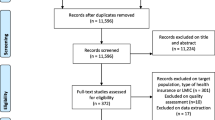
By September 30, 2020, we have searched for a total of 445 papers. The selection criteria for publications were as follows: (1) In terms of publication time, we limit it from 2008 to September 30, 2020 (the time of revision of this paper). Although the ‘Long Term Care Insurance’ article first appeared back in 1984 (Meiners&Tave.1984 [11]; Schechter,1984 [12]; Meiners&Trapnell,1984 [13]), but they simply put forward the concept of ‘Long Term Care Insurance’, and there were few studies on the subject over the next 25 years. It was not until 2008 that Brown & Finkelstein (2008) [14] first discussed the relationship between American public LTCI and private LTCI, and Ariizumi(2008) [15] first discussed the effect of public long-term care insurance on consumption and welfare, that the topic of long term care insurance began to attract the attention of a large number of scholars. Therefore, this paper takes 2008 as the starting point of research time. (2) The following types of documents are not included: Meeting abstract, Editorial Material, Letter, Proceedings paper, and other types such as Opinions or Comments (194 articles in total). In the end, we determined a total of 59 articles, including 38 quantitative research and 21 qualitative research.
Data extraction process
All publication information was exported to the Excel database via Endnote, and duplicate sections were removed. The results were initially extracted by one researcher and then cross-checked by another to ensure that all data had been screened and reviewed. If there is a difference of opinion between the two researchers, the third researcher will be invited to express his opinion and finally reach an agreement.
The information extracted from all the included publication was as follows: Author, Publication date, Sample country, Research method, Research objective, and Key findings. All the analysis results are analyzed in the following process (as shown in Fig. 1).
Quality appraisal
We used the Critical Appraisal Skills Programme (CASP) to evaluate all 59 papers that were selected and selected 4 of the original 10 questions within the CASP Checklist that was suitable for our paper to evaluate the quality of the paper (shown in Table 2). The five questions are: (1)Did the paper address a clearly focused question? (2)Do you think all the important, relevant studies were included? (3) Can the results be applied to the local population? (4) Were all important outcomes considered? All the questions were asked to answer one of the following answers: Yes; No; Can’t Tell. The evaluation results of all literatures are shown in Table 2.
Results
Preliminary review of relevant literature
Of the 59 papers selected, 38 were quantitative and 21 were qualitative. Among them, quantitative research is mainly carried out from two perspectives. One is empirical research through microscopic investigation data, such as logistic regression analysis. The second is to discuss the long-term sustainable development of public LTCI caused by financing problems by comparing the financing of public LTCI with the macro data of cost demand.
The publication time and sample countries of public LTCI thematic research are closely related to the development experience of public LTCI in each country. Figure 2 shows some information.
As shown in Fig. 2(a), the research on public LTCI is mainly concentrated in Korea(16), Japan (14), and Germany(8). Germany is the first country in the world to formally legislate public LTCI (1995), while Japan (2000) and South Korea (2008) are the first countries in Asia to formally legislate public LTCI. In recent years, these three countries have been carrying out many reforms to different degrees for public LTCI according to their national conditions. It is worth noting that since China began to pilot public LTCI in 15 cities in 2016, relevant research has begun to emerge. In addition, the research on Thailand’s public LTCI began to appear. Although Thailand’s public LTCI system has not been formally implemented, it at least shows that Thailand is trying to make relevant efforts. The information is given in Fig. 2(b) is also very interesting. It shows that the research on public LTCI can be divided into three climaxes in terms of time, namely, 2009–2010, 2014–2015, and 2017–2019.
Comparison of public LTCI systems in different countries
As early as 10 years ago, Campbell et al. (2010) [2] compared the differences between Germany and Japan in the objectives, qualification procedures, scale, and sustainability of the public LTCI system, hoping to learn from the experience and find a suitable LTCI system for the American situation. Bakx et al. (2015) [2] used data from the Netherlands and Germany, two countries with general public LTCI, and found that although the overall use rate of LTC was similar in the two countries, the use of formal care was more common in the Netherlands and the use of informal care was more common in Germany. Courbage et al. (2020) [2] also performed similar comparative studies on Italy and Spain through cross-sectional data from the European Health, Ageing, and Retirement Survey (SHARE) database. Rhee et al. (2015) [2] compared the public LTCI systems of Korea, Japan, and Germany from the perspective of financing, and believed that in order to achieve the sustainable development of LTCI, the financing of LTCI should be planned in advance in terms of income generation, welfare design, and qualification. A more meaningful study was conducted by Chandoevwit&Wasi (2020) [2], who discussed the feasibility and benefits of introducing public LTCI to middle-income countries such as Thailand through discrete Choice experiment (DCEs). To sum up, the comparison of public LTCI system in different countries is mainly carried out from the three aspects of structure design, fund raising and policy effect of public LTCI system (as shown in Table 3).
Influence of public LTCI
The social and economic impact of public LTCI on population aging is enormous, and many scholars have analyzed its influence from different angles (as shown in Table 4).
Firstly, the impact of public LTCI on the health of beneficiaries. As the first country with formal legislation and public LTCI, Germany has made remarkable achievements in LTCI reform. The physical health of the beneficiaries of the public LTCI has improved significantly for the most part, especially those receiving good home care (Buscher, et al. 2010). The changes in Japan (Olivares-Tirado et al. 2012; Ohwaki, et al. 2009; Chen et al. 2013) and South Korea (Lee et al. 2014 ; Sohn et al. 2020), the two Asian countries that decided on public LTCI in 2000 and 2008 respectively, have also been remarkable.
Secondly, the impact of LTCI on the economic burden of beneficiary families, which is an inevitable problem that must be solved in the process of sustainable development of public LTCI. For instance, after the implementation of public LTCI, German people’s perception of financial security also increases with the increase of income (Zuchandke et al. 2010), but there is a gender and age difference. When the age is older, women spend more than men of the same age (Schwarzkopf, et al. 2012). The introduction of the public LTCI in 2000 helped Japanese families reduce welfare losses associated with members of families with disabilities (Yamada et al. 2009; Iwamoto et al. 2010; Washio et al. 2012). In Korea, the burden of medical costs for LTCI beneficiaries was significantly reduced compared to non-beneficiaries, although medical costs for the elderly increased (Kim& Lim, 2015; Choi et al. 2018). In China, the introduction of public LTCI has greatly reduced the length of stay, hospitalization costs and medical insurance costs in tertiary hospitals by 41.0, 17.7 and 11.4%, respectively. The cost-benefit analysis shows that each additional dollar spent at LTCI reduces health insurance spending by $8.6(Feng et al. 2020).
Thirdly, the impact of public LTCI on long-term care providers, i.e., the labor market. German scholars Geyer designed a structural model of labor supply and family caregiver welfare choices and found that benefits in kind had a small positive effect on labor supply (Geyer&Korfhage, 2015; Geyer, et al. 2017). Japanese researchers found that the introduction of public LTCI had a significant positive spillover effect on the labor force participation of family caregivers, and the effects varied by gender and age (Umegaki et al. 2014; Fu et al. 2017; Kondo, 2019).
Finally, the influence of LTC system design, including nursing style, is discussed. The influence of public LTCI on the choice of long-term care methods in various countries, such as home care, community care, and institutional care, is restricted by income level, family environment, and other factors (Strier,& Werner , 2016; Bascans et al. 2017; Tomita et al. 2010; Seok, 2010; Kim et al. 2013; Hyun et al. 2014; Kim et al. 2019; Zhang&Yu,2019).
Challenge of public LTCI
As a new type of insurance coexisting with endowment insurance and medical insurance, LTCI system has experienced different degrees of difficulties and challenges in the development process of different countries, which will affect the long-term sustainability and stability of LTCI system development (as shown in Table 5).
Firstly, the challenges from the sustainability of LTCI financing, which is a core issue for LTCI’s long-term development. For instance, the success of the Netherlands LTCI reform depends to a large extent on the accuracy of the LTCI needs assessment and the proper budgeting of LTC costs (Schut& van den Berg,2010). Germany’s public LTCI has undergone several reforms, as has Japan (Tamiya et al. 2011; Kato,2018), focusing on solving the financing problem through higher contribution rates and the creation of a “population reserve Fund” since 1995(Rothgang,2010; Nadash et al. 2018). Financing is one of the greatest challenges in the development of China’s LTCI system and most pilot cities mainly rely on Urban Employees Basic Medical Insurance funds as the financing source for LTCI (Wang et al.2018; Zhang et al.2020).
Secondly, the challenges from design flaw of LTCI system, including certification. For instance, publicly provided health-based LTC crowds out the medical spending among low health individuals in USA (Ariizumi, 2008),while future policy experimentation on LTCI reform in China needs to address the some policy issues such as expanding the coverage of LTCI and narrowing rural-urban disparities in access (Zhu& Osterle,2019). The lack of coordination between the health sector and the long-term care sector is a weak point in the development of Korea’s public LTCI (Kang et al.2012; Chon, 2013,2014).
Thirdly, challenges from traditional social concepts or family relationships. For example, Whether in Europe (Costa-Font, 2010) or Israel (Ayalon, 2018), family relationships or family culture are correlated with the benefit coverage of LTCI. This is especially true in South Korea, which is heavily influenced by traditional East Asian culture. Many Korean studies found that the state has difficulty in regulating the market and costs, and deeply embedded familialism seems difficult to overcome (Chon, 2012; Kim& Choi2013; Ha et al.2017).
Finally, how to balance fairness and efficiency is also a big challenge for the future development of public LTCI. For example, Dutch using prior utilization and expenditure as risk adjusters reduces incentives for efficiency, creating a trade-off between equity and efficiency (Bakx et al.2015).Long-term care reforms in Korea should continue to concentrate on expanding insurance coverage and reducing the inequities reflected in disparities in consumer cost sharing and associated patterns of utilization across plans (Park, 2015). There remain sizable disparities in financial burden among insurance participants, despite an emphasis on ensuring equitable access to care in China (Yang et al.2020) and Japan (Saito et al.2018).
Relationship between public LTCI and private LTCI
As shown in Table 6, Brown&Finkelstein (2008) ‘s study published in AMERICAN ECONOMIC REVIEW in 2008 was the first classic paper in the world to discuss the relationship between PUBLIC LTCI and private LTCI. Two years later, the difference between public nursing institutions and private nursing institutions in the Long term care effect of disabled elderly after the formal launch of public LTCI system in Japan since 2000 was compared (Yoshioka et al.,2010). Their study found that private LTCI plays an important role in promoting the use of care services, but the quality of care may be problematic. In the following years, some scholars conducted in-depth discussions on the crowding out effect of public LTCI and private LTCI (Cremer&Pestieau,2014; Costa-Font&Courbage,2015), cooperation mode (Schmitz& Giese,2019) and other aspects.
In addition, Before China officially launched the pilot system of public LTCI in 2016, some Chinese scholars discussed what roles public LTCI and private LTCI should play in response to China’s huge long-term care needs. For instance, Shen& Li (2014) conducted a cross-sectional survey of 814 residents (ages 18–59) and found that public LTCI was likely to be more popular in terms of participation and contribution. Factors associated with public LTCI demand are medical costs, household income, and for private LTCI, these factors include the proportion of living expenses, concerns about future care, and medical costs. Therefore, policy makers should develop public LTCI as a solid foundation and perfect private LTCI as an alternative.
Discussion
In order to deal with the aging population and its long-term nursing costs, the research on LTCI has become the international academic frontier and hot topic. Judging from the current development of global LTCI system, the development of private LTCI is still in its infancy. Countries including Germany, the United States, Japan, South Korea and China all focus on the construction and sustainable development of public LTCI system. In practice, although the LTCI system originated in the Netherlands, Germany (1995) and Japan (2000) are the first countries in the world and Asia to legislate public LTCI, and have been carrying out many reforms and improvements for more than 20 years. Since 2016, China, as the country with the largest aging population in the world, began to pilot public LTCI, which has a great impact on people’s daily life and academic circles. This paper attempts to systematically sort out the relevant research literature on public LTCI, and to explore the continuous reform and improvement of LTCI system in Germany, Japan and South Korea, so as to seek experience and promote the further sustainable development of China’s public LTCI. This is also a further thinking to cope with the impact of covid-19 and other similar public health events on subsequent LTC services.
Firstly, a preliminary review of relevant literature was done. Of the 59 papers selected, 38 were quantitative and 21 were qualitative. Among them, quantitative research is mainly carried out from two perspectives. One is empirical research through microscopic investigation data, such as logistic regression analysis. The second is to discuss the long-term sustainable development of public LTCI caused by financing problems by comparing the financing of public LTCI with the macro data of cost demand. With the passage of time, there are more and more researches on public LTCI, which shows that the development of public LTCI is paid more and more attention by governments and academic circles. The research on public LTCI is mainly concentrated in Korea, Japan and Germany. Relevant research has begun to emerge in China since 2016. It also shows that the research on public LTCI can be divided into three climaxes in terms of time, namely, 2009–2010, 2014–2015 and 2017–2019. The first climax period (2009–2010) is the next 2 years after the official implementation of public LTCI (2008) in South Korea, so there are a lot of studies on Korean public LTCI during this period. The second climax period (2014–2015) is the second 2 years of the fifth reform of public LTCI in Japan, during which there are many relevant studies in Japan. The third climax period (2017–2019) is driven by China’s public LTCI pilot project in 15 cities in 2016.
Secondly, from the comparison of public LTCI systems in different countries, By comparing the development of public LTCI in the Netherlands, Germany, South Korea and Japan, we find that the structural design of public LTCI, including fund-raising and qualification procedures, has different characteristics in different countries (Campbell et al. 2010; Bakx et al. 2015;Courbage et al. 2020;Rhee et al. 2015;Chandoevwit&Wasi,2020). In order to operate stably and sustainably, public LTCI must adapt to local conditions and reform continuously.
Thirdly, the social and economic impact of public LTCI on population aging is enormous. Firstly, The physical health of the beneficiaries of the public LTCI has improved significantly, especially those receiving good home care in Germany,Japan,and Korea (Buscher, et al. 2010; Olivares-Tirado et al. 2012; Ohwaki, et al. 2009; Chen et al. 2013) and South Korea (Lee et al. 2014; Sohn et al. 2020). Secondly, the introduction of the public LTCI in 2000 helped families reduce economic welfare losses associated with members of families with disabilities (Yamada et al. 2009; Iwamoto et al. 2010;Washio et al. 2012;Kim& Lim, 2015; Choi et al. 2018). for example, the introduction of public LTCI in China has greatly reduced the length of stay, hospitalization costs and medical insurance costs in tertiary hospitals by 41.0, 17.7 and 11.4%, respectively (Feng et al. 2020).
Finally, LTCI system has experienced different degrees of difficulties and challenges in the development process of different countries, which will affect the long-term sustainability and stability of LTCI system development. Among them, the challenges from the sustainability of LTCI financing, which is a core issue for LTCI’s long-term development (Schut& van den Berg,2010; Tamiya et al. 2011; Kato,2018; Rothgang,2010; Nadash et al. 2018). Financing is one of the greatest challenges in the development of China’s LTCI system (Wang et al.2018; Zhang et al.2020).
The literature review of this paper gives us some policy implications. First of all, learning from the practical experience of LTCI system in the world, such as structural design and financing mode, will contribute to the in-depth development of China’s public LTCI system. However, the literature review also makes us realize that, restricted by different factors in different countries, the long-term care system is a long-term process, which needs continuous reform (Bakx et al. 2015;Chandoevwit&Wasi,2020) in order to truly meet the growing and changing long-term care needs, especially in China, which has the largest elderly population in the world. Secondly, it is always the core of the stable and sustainable development of public LTCI to solve the financing problem of public LTCI. However, the breakthrough of traditional social concept and family concept, the balance of fairness and efficiency, are very important factors that affect the sustainable development of public LTCI, especially Japan, South Korea, and China, which are deeply influenced by traditional culture (Costa-Font, 2010; Chon, 2012; Kim& Choi,2013; Ayalon, 2018). Perhaps, while steadily promoting public LTCI, it is wise to actively develop private LTCI market (Schmitz& Giese,2019).
In general, Germany, Japan, and other countries have their characteristics in the specific implementation policies of public LTCI, such as fundraising. For example, German LTCI law emphasizes two essential principles, namely, “in the home care priority” and “prevention and rehabilitation priority.” All medical insurance policyholders, as long as is an adult, regardless of men and women’s health and age, must attend the LTCI. On fundraising, the difference according to individual income level presses different proportions to execute personal pay costs. Spending on Long-term care services accounted for about 1% of GDP in 2018. Overall, there are two types of public LTCI (Long-Term Care Insurance) systems in different countries at present. The first is the Nordic “welfare state” model of the comprehensive general welfare, which is not suitable for China’s specific social conditions. The second is the “corporatist-welfare” mode of universal coverage, which emphasizes the combination of comprehensive coverage and mutual benefit, which is meet China’s current “peer-to-peer” rights and obligations of social insurance concept consistent, but there are some risks such as the cost burden. Therefore, China’s future public LTCI development should choose a unique path suitable for its social conditions.
Availability of data and materials
The original data that If the reader has a personal request, I will provide it to him.
Abbreviations
- LTC:
-
Long-Term Care
- LTCI:
-
Long-Term Care Insurance
- Public LTCI:
-
Public Long-Term Care Insurance
- Private:
-
LTCI Private Long-Term Care Insurance
- ADL:
-
Activities of daily living
- CASP:
-
Critical Appraisal Skills Programme
References
Xu X, Huang X, Zhang X, Chen L. Family economic burden of elderly chronic diseases: evidence from China. Healthcare. 2019;7(3):99. https://doi.org/10.3390/healthcare7030099.
Rhee JC, Done N, Anderson GF. Considering long-term care insurance for middle-income countries: comparing South Korea with Japan and Germany. Health Policy. 2015;119(10):1319–29.
Wei-dong D. Long term care insurance:a rational choice of old-age security in China. Popul J. 2016;2:72–81 [in Chinese].
Chen L, Zhang X, Xu X. Health insurance and long-term Care Services for the Disabled Elderly in China: based on CHARLS data. Risk Manag Healthcare Policy. 2020;13:155–62. https://doi.org/10.2147/RMHP.S233949.
Xu X, Zhang L, Chen L, Wei F. Does COVID-2019 have an impact on the purchase intention of commercial long-term care insurance among the elderly in China? Healthcare. 2020;8(2):126. https://doi.org/10.3390/healthcare8020126.
Xu X, Xu Z, Chen L, Li C. How does industrial waste gas emission affect health care expenditure in different regions of China: an application of Bayesian Quantile regression. Int J Environ Res Public Health. 2019;16(15):2748. https://doi.org/10.3390/ijerph16152748.
Huang X, Xu X, Wang Q, Zhang L, Gao X, Chen L. Assessment of agricultural carbon emissions and their spatiotemporal changes in China, 1997–2016. Int J Environ Res Public Health. 2019;16(17):3105. https://doi.org/10.3390/ijerph16173105.
Xu X, Huang X, Huang J, Gao X, Chen L. Spatial-temporal characteristics of agriculture green Total factor productivity in China, 1998–2016: based on more sophisticated calculations of carbon emissions. Int J Environ Res Public Health. 2019;16(20):3932. https://doi.org/10.3390/ijerph16203932.
Chen L, Xu X. Effect evaluation of the long-term care insurance (LTCI) system on the health Care of the Elderly: a review. J Multidiscip Healthcare. 2020;13:863–75. https://doi.org/10.2147/JMDH.S270454.
Islam MS, Hasan MM, Wang X, Germack HD, Noor-E-Alam M. A systematic review on healthcare analytics: application and theoretical perspective of data mining. Healthcare. 2018;6(2):54.
Meiners MR, Tave AK. Surveying interest in long-term care insurance among elderly consumers. Gerontologist. 1984;24:168.
Schechter M. Long-term care insurance. Hosp Pract. 1984;19(12):15.
Meiners MR, Trapnell GR. Long-term care insurance - premium estimates for prototype policies. Med Care. 1984;22(10):901–11. https://doi.org/10.1097/00005650-198410000-00003.
Brown JR, Finkelstein A. The interaction of public and private insurance: Medicaid and the long-term care insurance market. Am Econ Rev. 2008;98(3):1083–102. https://doi.org/10.1257/aer.98.3.1083.
Ariizumi H. Effect of public long-term care insurance on consumption, medical care demand, and welfare. J Health Econ. 2008;27(6):1423–35. https://doi.org/10.1016/j.jhealeco.2008.07.008.
Yamada M, Hagihara A, Nobutomo K. Family caregivers and care manager support under long-term care insurance in rural Japan. Psychol Health Med. 2009;14(1):73–85. https://doi.org/10.1080/13548500802068990.
Ohwaki K, Hashimoto H, Sato M, Tamiya N, Yano E. Predictors of continuity in home care for the elderly under public long-term care insurance in Japan. Aging Clin Exp Res. 2009;21(4–5):323–8.
Yoshioka Y, Tamiya N, Kashiwagi M, Sato M, Okubo I. Comparison of public and private care management agencies under public long-term care insurance in Japan: A cross-sectional study. Geriatr Gerontol Int. 2010;10(1):48–55. https://doi.org/10.1111/j.1447-0594.2009.00558.x.
Campbell JC, Ikegami N, Gibson MJ. Lessons From Public Long-Term Care Insurance In Germany And Japan. Health Affairs. 2010;29(1):87–95. https://doi.org/10.1377/hlthaff.2009.0548.
Seok JE. Public Long-Term Care Insurance for the Elderly in Korea: Design, Characteristics, and Tasks. Soc Work Public Health. 2010;25(2):185–209 Special Issue: SI. https://doi.org/10.1080/19371910903547033.
Iwamoto Y, Kohara M, Saito M. On the consumption insurance effects of long-term care insurance in Japan: Evidence from micro-level household data. J Japan Int Econ. 2010;24(1):99–115. https://doi.org/10.1016/j.jjie.2009.12.009.
Buscher A, Holle B, Emmert S, Fringer A. Home care counseling for recipients of cash payments in the German long-term care insurance. Zeitschrift Fur Gerontologie Und Geriatrie. 2010;43(2):103–10. https://doi.org/10.1007/s00391-010-0099-4.
Schut FT, van den Berg B. Sustainability of Comprehensive Universal Long-term Care Insurance in the Netherlands. Soc Policy Adm. 2010;44(4):411–35. https://doi.org/10.1111/j.1467-9515.2010.00721.x.
Rothgang H. Social Insurance for Long-term Care: An Evaluation of the German Model. Soc Policy Adm. 2010;44(4):436–60. https://doi.org/10.1111/j.1467-9515.201000722.x.
Zuchandke A, Reddemann S, Krummaker S, von der Schulenburg JMG. Impact of the Introduction of the Social Long-Term Care Insurance in Germany on Financial Security Assessment in Case of Long-Term Care Need. Geneva Papers Risk Insur Issu Pract. 2010;35(4):626–43. https://doi.org/10.1057/gpp.2010.26.
Costa-Font J. Family ties and the crowding out of long-term care insurance. Oxford Rev Econ Policy. 2010;26(4):691–712. https://doi.org/10.1093/oxrep/grq040.
Tomita N, Yoshimura K, Ikegami N. Impact of home and community-based services on hospitalisation and institutionalisation among individuals eligible for long-term care insurance in Japan. BMC Health Serv Res. 2010;10:345. https://doi.org/10.1186/1472-6963-10-345.
Tamiya N, Noguchi H, Nishi A, Reich MR, Ikegami N, Hashimoto H, Shibuya K, Kawachi I, Campbell JC. Japan: Universal Health Care at 50 years 4 Population ageing and wellbeing: lessons from Japan's long-term care insurance policy. Lancet. 2011;378(9797):1183–92. https://doi.org/10.1016/S0140-6736(11)61176-8.
Kang IO, Park CY, Lee Y. Role of Healthcare in Korean Long-Term Care Insurance. J Korean Med Sci. 2012;27:S41–6 Supplement: S. https://doi.org/10.3346/jkms.2012.27.S.S41.
Schwarzkopf L, Menn P, Leidl R, Wunder S, Mehlig H, Marx P, Graessel E, Holle R. Excess costs of dementia disorders and the role of age and gender - an analysis of German health and long-term care insurance claims data. BMC Health Serv Res. 2012;12:165. https://doi.org/10.1186/1472-6963-12-165.
Olivares-Tirado P, Tamiya N, Kashiwagi M. Effect of in-home and community-based services on the functional status of elderly in the long-term care insurance system in Japan. BMC Health Serv Res. 2012;12:239. https://doi.org/10.1186/1472-6963-12-239.
Washio M, Arai Y, Oura A, Miyabayashi I, Onimaru M, Mori M. Family Caregiver Burden and Public Long-Term Care Insurance System in Japan. Int Med J. 2012;19(3):229–33.
Chon Y. Long-term care reform in Korea: lessons from the introduction of Asia's second long-term care insurance system. Asia Pac J Soc Work Dev. 2012;22(4):219–27. https://doi.org/10.1080/02185385.2012.726422.
Chen WL, Fukutomi E, Wada T, Ishimoto Y, Kimura Y, Kasahara Y, Sakamoto R, Okumiya K, Matsubayashi K. Comprehensive geriatric functional analysis of elderly populations in four categories of the long-term care insurance system in a rural, depopulated and aging town in Japan. Geriatr Gerontol Int. 2013;13(1):63–9. https://doi.org/10.1111/j.1447-0594.2012.00859.x.
Chon Y. A Qualitative Exploratory Study on the Service Delivery System for the New Long-Term Care Insurance System in Korea. J Soc Serv Res. 2013;39(2):188–203. https://doi.org/10.1080/01488376.2012.744708.
Kim JW, Choi YJ. Farewell to old legacies? The introduction of long-term care insurance in South Korea. Ageing Soc. 2013;33:871–87 Part: 5. https://doi.org/10.1017/S0144686X12000335.
Kim H, Kwon S, Yoon NH, Hyun KR. Utilization of long-term care services under the public long-term care insurance program in Korea: Implications of a subsidy policy. Health Policy. 2013;111(2):166–74. https://doi.org/10.1016/j.healthpol.2013.04.009.
Umegaki H, Yanagawa M, Nonogaki Z, Nakashima H, Kuzuya M, Endo H. Burden reduction of caregivers for users of care services provided by the public long-term care insurance system in Japan. Arch Gerontol Geriatr. 2014;58(1):130–3. https://doi.org/10.1016/j.archger.2013.08.010.
Shen SYL, Tanui F. Long-Term Care Insurance in China: Public or Private? Soc Work Health Care. 2014;53(7):679–92. https://doi.org/10.1080/00981389.2014.925999.
Lee TW, Yim E, Cho E, Chung J. Cognitive Function, Behavioral Problems, and Physical Function in Long-Term Care Insurance Beneficiaries with Dementia in South Korea: Comparison of Home Care and Institutional Care Services. J Am Geriatr Soc. 2014;62(8):1467–75. https://doi.org/10.1111/jgs.12944.
Cremer, H; Pestieau, P. Social long-term care insurance and redistribution. Int Tax Public Finance. 2014.21 6 955–974. doi: https://doi.org/10.1007/s10797-013-9289-5.
Chon Y. The Expansion of the Korean Welfare State and Its Results - Focusing on Long-term Care Insurance for the Elderly. Soc Policy Adm. 2014;48(6):704–20. https://doi.org/10.1111/spol.12092.
Hyun KR, Kang S, Lee S. Does long-term care insurance affect the length of stay in hospitals for the elderly in Korea?: a difference-in-difference method. BMC Health Serv Res. 2014;14:630. https://doi.org/10.1186/s12913-014-0630-1.
Costa-Font, J; Courbage, C. Crowding out of long-term care insurance: evidence from european expectations data. Health Econ.2015.24 74–88 Supplement: 1. doi: https://doi.org/10.1002/hec.3148.
Kim HB, Lim W. Long-term care insurance, informal care, and medical expenditures. J Public Econ. 2015;125:128–42. https://doi.org/10.1016/j.jpubeco.2014.12.004.
Bakx P, De Meijer C, Schut F, Van Doorslaer E. Going formal or informal, who cares? the influence of public long-term care insurance. Health Econ. 2015;24(6):631–43. https://doi.org/10.1002/hec.3050.
Bakx P, Schut F, van Doorslaer E. Can universal access and competition in long-term care insurance be combined? Int J Health Econ Manag. 2015;15(2):185–213. https://doi.org/10.1007/s10754-015-9163-3.
Geyer, J; Korfhage, T. Long-term Care Insurance and Carers’ Labor Supply - A Structural Model. Health Econ. 2015 24 9 1178–1191. doi: https://doi.org/10.1002/hec.3200.
Park JM. Equity of access under Korean national long-term care insurance: implications for long-term care reform. Int J Equity Health. 2015;14:82. https://doi.org/10.1186/s12939-015-0210-y.
Strier R, Werner P. Tracing Stigma in Long-Term Care Insurance in Israel: Stakeholders’ Views of Policy Implementation. J Aging Soc Policy. 2016;28(1):29–48. https://doi.org/10.1080/08959420.2016.1111726.
Ha SC, Kim HJ, Palmer A. The Relationship between Public Long-Term Care Insurance Awareness and Preparation for Later Life in South Korea. J Soc Serv Res. 2017;43(4):510–26. https://doi.org/10.1080/01488376.2017.1324829.
Bascans JM, Courbage C, Oros C. Means-tested public support and the interaction between long-term care insurance and informal care. Int J Health Econ Manag. 2017;17(2):113–33. https://doi.org/10.1007/s10754-016-9206-4.
Geyer J, Haan P, Korfhage T. Indirect Fiscal Effects of Long-Term Care Insurance. Fiscal Stud. 2017;38(3):393–415 Special Issue: SI. https://doi.org/10.1111/j.1475-5890.2017.12140.
Fu R, Noguchi H, Kawamura A, Takahashi H, Tamiya N. Spillover effect of Japanese long-term care insurance as an employment promotion policy for family caregivers. J Health Econ. 2017;56:103–12. https://doi.org/10.1016/j.jhealeco.2017.09.011.
Wang Q, Zhou Y, Ding XR, Ying XH. Demand for Long-Term Care Insurance in China. Int J Environ Res Public Health. 2018;15(1):6. https://doi.org/10.3390/ijerph15010006.
Saito T, Kondo N, Shiba K, Murata C, Kondo K. Income-based inequalities in caregiving time and depressive symptoms among older family caregivers under the Japanese long-term care insurance system: A cross-sectional analysis. Plos One. 2018;13(3):e0194919. https://doi.org/10.1371/journal.pone.0194919.
Nadash P, Doty P, von Schwanenflugel M. The German Long-Term Care Insurance Program: Evolution and Recent Developments. Gerontologist. 2018;58(3):588–97. https://doi.org/10.1093/geront/gnx018.
Ayalon L. Between older adults’ needs and the law: The Israeli Long Term Care Insurance Law from the Perspectives of Service Users and Providers. Health Soc Care Commun. 2018;26(4):E514–22. https://doi.org/10.1111/hsc.12563.
Kato RR. The future prospect of the long-term care insurance in Japan. Japan World Econ. 2018;47:1–17. https://doi.org/10.1016/j.japwor.2018.02.002.
Choi JW, Park EC, Lee SG, Park S, Ryu HG, Kim TH. Does long-term care insurance reduce the burden of medical costs? A retrospective elderly cohort study. Geriatr Gerontol Int. 2018;18(12):1641–6. https://doi.org/10.1111/ggi.13536.
Schmitz A, Giese C. Is Insurance the Answer to the Long-Term-Care Financing Challenge? Generations-J Am Soc Aging. 2019;43(1):88–90.
Kim W, Chun SY, Lee JE, Lee TH, Park EC. Factors Related to the Institutionalization of Older Aged Individuals Using Home- and Community-Based Care Services: Data From the South Korea Long-Term Care Insurance Program, 2008–2013. J Aging Soc Policy. 2019;31(4):321–37. https://doi.org/10.1080/08959420.2019.1589890.
Zhu YM, Osterle A. China's policy experimentation on long-term care insurance: Implications for access. Int J Health Plan Manag. 2019;34(4):E1661–74. https://doi.org/10.1002/hpm.2879.
Kondo A. Impact of increased long-term care insurance payments on employment and wages in formal long-term care. J Japan Int Econ. 2019;53:101034. https://doi.org/10.1016/j.jjie.2019.101034.
Zhang YZ, Yu X. Evaluation of Long-Term Care Insurance Policy in Chinese Pilot Cities. Int J Environ Res Public Health. 2019;16(20):3826. https://doi.org/10.3390/ijerph16203826.
Sohn M, O'Campo P, Muntaner C, Chung H, Choi M. Has the long-term care insurance resolved disparities in mortality for older Koreans? examination of service type and income level. Soc Sci Med. 2020;247:112812. https://doi.org/10.1016/j.socscimed.2020.112812.
Yang W, Chang S, Zhang WB, Wang RB, Mossialos E, Wu X, Cui D, Li H, Mi H. An Initial Analysis of the Effects of a Long-Term Care Insurance on Equity and Efficiency: A Case Study of Qingdao City in China. Res Aging. 2020:0164027520907346. https://doi.org/10.1177/0164027520907346.
Zhang LW, Fu SJ, Fang Y. Prediction the Contribution Rate of Long-Term Care Insurance for the Aged in China Based on the Balance of Supply and Demand. Sustainability. 2020;12(8):3144. https://doi.org/10.3390/su12083144.
Courbage, C ; Montoliu-Montes, G ; Wagner, J. The effect of long-term care public benefits and insurance on informal care from outside the household: empirical evidence from Italy and Spain. Eur J Health Econ. 2020. doi: https://doi.org/10.1007/s10198-020-01215-7. Early Access: JUL 2020.
Chandoevwit, W ; Wasi, N. Incorporating discrete choice experiments into policy decisions: Case of designing public long-term care insurance. Soc Sci Med. 2020 258 .Article Number: 113044 .doi: https://doi.org/10.1016/j.socscimed.2020.113044.
Feng J, Wang Z, Yu YY. Does long-term care insurance reduce hospital utilization and medical expenditures? Evidence from China. Soc Sci Med. 2020;258:113081. https://doi.org/10.1016/j.socscimed.2020.113081.
Acknowledgements
We thank Professor Timothy Kyng and Professor Fei Guo at Macquarie University for their thoughtful guidance, and the help of the MOE Project of Key Research Institute of Humanities and Social Sciences of Research Center for Economy of Upper Reaches of the Yangtse River (CJSYTD201710).
Funding
This research is the stage research result of the National Social Science Fund of China: Research on the blocking mechanism of the critical poor households returning to poverty due to illness (NO:20BJY057).
Author information
Authors and Affiliations
Contributions
All authors have read and agree to the published version of the manuscript. Conceptualization, X.X.; methodology, L.C.; writing—original draft preparation, L.C.; writing—review and editing, L.Z.; visualization, X.X.; project administration, L.C.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. Ethical approval is not necessary as this study does not involve human or animal studies.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, L., Zhang, L. & Xu, X. Review of evolution of the public long-term care insurance (LTCI) system in different countries: influence and challenge. BMC Health Serv Res 20, 1057 (2020). https://doi.org/10.1186/s12913-020-05878-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-020-05878-z