Abstract
Background
The concept of quality in health care has evolved, placing greater importance on the patient’s needs, culture, and social context, as well as their participation in clinical decision-making, as highlighted by Mead and Bower’s Person-Centered Care Model. The aim of the present study was to design and validate an instrument to assess the extent to which healthcare services provided by PEMEX (Petróleos Mexicanos) offer person-centered care according to user perceptions.
Methods
The first phase comprised the development of 57 items based on the analysis of responses from an open-ended questionnaire administered to 30 users of Pemex healthcare services. This questionnaire was designed considering the four factors of the person-centered care model, however, the high correlation between the 4 factors (i.e., r ≥ .80) indicated an overfactoring effect and consequently an increase in the risk of overfitting. Therefore, an exhaustive analysis of the instrument was performed, starting with the review of the individual behavior of each item, and carrying out exploratory and confirmatory factor analysis. Using a sample of 330 individuals, an exploratory factor analysis was perfomed. Afterward, a confirmatory factorial analysis was carried out with 335 participants. Finally, a new confirmatory factorial analysis included 130 participants due to the refinements made in the previous phase. Internal consistency was assessed using Cronbach’s α and McDonald’s ω at every phase.
Results
The exploratory factor analysis retained 35 items in a single factor that accounted for 49% of the variance with an internal consistency of Cronbach’s α and McDonald’s ω = 0.97. Because the factorial structure by confirmatory factorial analysis was unsatisfactory, the initial model was refined, leading to the retention of 11 items and a final model with adjustment index of χ2 = 127.53, χ2/gl = 2.89, RMSEA = 0.07, IC RMSEA 0.06 to 0.09, TLI = 0.95 and CFI = 0.96, with an internal consistency of Cronbach’s α and McDonald’s ω = 0.93. Due to the refinements, a new confirmatory factorial analysis was conducted with suitable goodness-of-fit criteria in most items (χ2 = 151.44, χ2/gl = 3.43, RMSEA = 0.13, IC RMSEA 0.11 to 0.16, TLI = 0.93 and CFI = 0.94), resulting in a Cronbach’s α and McDonald’s ω = 0.98.
Conclusions
The instrument exhibits suitable psychometric properties to be employed to measure the degree to which medical care is patient centered. This instrument represents a strategy for promoting an innovative healthcare model.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Text box 1. Contributions to the literature |
|---|
•Patient-centered care is about seeing everyone as a unique human being, with needs, desires, and concerns of their own. It means listening carefully, showing empathy, and working collaboratively with our patients to provide them with the best care possible. The creation of an instrument that measures patient-centered care, will detect the need to empower patients to improve results related to health care and increase the medical services user´s satisfaction. |
•This innovative instrument was built from all the factors contemplated in patient-centered care: (1) biopsychosocial perspective, (2) patient as a person, (3) therapeutic alliance, and (4) sharing power and responsibilities, and although the statistical treatment resulted in a unifactorial instrument, by conserving items that initially represented 3 of the 4 fundamental factors of the theoretical model, we consider that it preserves the essence of the theoretical model proposed by Mead and Bower [4]. |
•The strength of having designed an instrument whose rationale, design and validation are based on the highest scientific rigor by mean of a robust statistical analyses, such as exploratory factor analysis to detect its structure and confirmatory factor analysis to validate such structure is fundamental to the public health literature. |
Introduction
The organization of healthcare service components aims to contribute to the collective function. In this sense, the analytical and descriptive representation of a series of goals, operational strategies, and healthcare objectives that meet the population needs and demands allows conceptualizing a healthcare delivery model. Drawing from the insights of Avedis Donabedian [1], the extent to which healthcare services provide the greatest benefit, with minimum risks and reasonable costs, will be proportional to the quality of healthcare delivered.
The concept of quality in healthcare applied to the healthcare sector has been evolving, primarily in terms of the patient‒doctor relationship, where the principle of autonomy has been established gradually. This principle emphasizes the patient as a decision-maker regarding their health status [2]. Prior to this, there was a prevailing approach in which doctors played an exclusive role in decision-making and action guidelines. Currently, healthcare professionals strive to incorporate patient´s preferences into decisions regarding their care and engage in shared decision-making between the patient and the healthcare provider. The goal is to involve those affected by clinical decision-making [3].
The involvement of the patient in their health care and clinical decision-making highlights the “person-centered” care model by Mead & Bower, which focuses on the approach and understanding of patient´s experience and the meaning that illness holds for them. This model comprises four dimensions: (1) biopsychosocial perspective, (2) patient as a person, (3) therapeutic alliance, and (4) sharing power and responsibilities [4]. Identifying and understanding the patient’s perspective enables their inclusion in decision-making and care evolution [4]. While this approach has been discussed since the 1980s, it was not until the 1990s that it gained recognition and began to be implemented with the aim of shaping healthcare delivery centered on patients rather than providers and health systems [5]. Providing person-centered care involves respecting the patients´ culture, social context, and needs. In addition, it expects the patient’s role in care to be active, participating in decisions around their health care [6]. Empowering the patient encourages a responsible attitude toward their health care and brings advantages compared to other care models [7,8,9,10,11].
If healthcare aims to provide person-centered care, it is then essential to understand quality from the patient´s perspective [12, 13], whose perception encompasses subjective and objective experiences and observations of healthcare staff behavior influenced by different variables. Therefore, the patient’s experience must be considered a reflection of the commitment adopted by healthcare providers and the quality of care [14]. Definitively, factors such as the healthcare system’s reputation, concern for health status, and previous interactions with the medical unit impact patient expectations and consequently the perception of healthcare [13].
Regarding instruments designed to assess person-centered care, most have focused only on some dimensions of the Mead & Bower model [4]. In a meta-analysis that examined instruments focused on specific dimensions of person-centered care, Pascual and colleagues [15] identified five questionnaires focused on the dimension “patient as a person” or “biopsychosocial perspective”. Fifteen questionnaires focus on the dimension “sharing power and responsibility,” and nineteen focus on the “therapeutic alliance” dimension. It is noteworthy that 65% of these instruments were validated in the United States and the United Kingdom, with 80% in English-speaking countries. Only 7.7% of the analyzed questionnaires were validated in Spanish, but none were focused on the Mexican population. These investigators conducted an analysis based on the COSMIN scale (Consensus-based Standards for the selection of health Measurement Instruments) [16], which measures the quality and design of instruments, detecting methodological issues.
Thus, the aim of the present study is to design and validate an instrument that assesses the extent to which PEMEX (Petróleos Mexicanos) healthcare services provide person-centered care according to user perceptions. In addition to employing a suitable methodology that enables instrument generalization, the design will be based on the four dimensions of the person-centered care model [4]. The purpose of this work is to apply an instrument to guide the practice of healthcare professionals, enabling them to attain the benefits of patient empowerment, facilitating shared responsibilities in healthcare, and enhancing the quality of medical care.
Methods
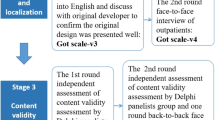
The present is an instrumental study [17], included in the category of studies that analyze the psychometric properties of psychological measurement instruments, including two phases (Fig. 1). In Phase 1, the instrument items were developed following the application of a questionnaire to a group of PEMEX healthcare service users on the care received. It is worth noting that the questionnaire was based on the dimensions of the Person-Centered Care Method [4]. Phase 2 involved the validation of the Person-Centered Care Instrument in Health Services.
Phase 1: Qualitative identification of potential questionnaire items and development of the Likert Scale
Participants
The participants consisted of 30 adult voluntary individuals [18], both men and women, who were users of PEMEX healthcare services at Mexico City, Mexico. Inclusion criteria required signing informed consent. The sole exclusion criterion was not completing the questionnaire.
Instrument
To explore indicators of perceived quality in medical care by PEMEX health users, an open questionnaire consisting of 9 questions was used, which was validated based on the agreement between 4 expert judges [19, 20]. This questionnaire was applied by the researcher to the 30 enrolled participants. The sample size was based on the principle of theoretical saturation contemplated by qualitative research [21], and a number of participants similar to that of previous studies was used [18]. The questions were grouped according to the dimensions of the theoretical person-centered care model: (1) patient as a person, (2) biopsychosocial perspective, (3) therapeutic alliance, and (4) sharing power and responsibility [4]. (Appendix C)
Procedure
Participants were recruited by investigators at the Medical Unit of Petróleos Mexicanos and the Central South Hospital, which are advertised to PEMEX. Subjects voluntarily responded to the questionnaire in August 2022. Emphasis was placed on confidentiality and personal data protection. After data collection, a content analysis was conducted to identify positive and negative indicators for each dimension, which collectively were the basis for a first Likert scale instrument with 71 items.
Development of the Likert Scale instrument
The scale items were evaluated by four experts in the field using the following criteria: clarity, wording, coherence, and relevance to each dimension. Based on expert opinions and due to a lack of congruence and relevance to the respective dimensions, 14 items were removed, resulting in 57 items: 19 for “patient as a person”, 13 for “biopsychosocial perspective,” 13 for “therapeutic alliance,” and 12 for the “sharing power and responsibility” dimension. Please, see the first instrument version in Appendix B.
Phase 2: Factorial analysis and validation
At the beginning of phase 2, a confirmatory factor analysis was performed including the 4 factors of Mead & Bower’s person-centered care model [4]. Inadequate fit indices or high correlations between factors implied an exploratory factor analysis to determine the initial structure of the instrument and a confirmatory factor analysis. In addition, the internal consistency of the instrument was assessed to determine the capability to measure person-centered care in a sample of Pemex healthcare service users.
Participants
Three groups of participants were recruited using a nonrandom convenience sampling technique. Sample A included 330 participants aged between 18 and 97 years (M = 51.38; SD = 15.57), 208 (63%) females and 122 (37%) males. Sample B consisted of 335 participants aged between 18 and 93 years (M = 51.06; SD = 14.13), 204 (60.9%) females and 131 (39.1%) males. Sample C included 130 participants aged between 18 and 88 years (M = 50.19; SD = 13.85), 89 (68.5%) females and 41 (31.5%) males. The personnel of the Health Services Quality Department of Petróleos Mexicanos invited users to participate and self-administer the instrument during the visit to any of Pemex’s medical facilities, including central and regional hospitals, clinics, and offices.
The confirmatory factor analysis was performed using the Group B to corroborate the 4-factor model, exceeding a minimum of 100 to 150 participants contemplated for SEM (structural equation modeling) models [22]. Given high correlations between factors, an overfactoring effect and a risk of overfitting [23], an exploratory factor analysis was carried out with this same group, assigning 5 participants per item, thus fulfilling with the minimum sample as previously described [24]. On the other hand, Groups B and C met the criteria required for conducting confirmatory factorial analysis [25] and the sample required to perform the confirmatory factorial analysis [22]. The inclusion criteria for all groups were the signing of informed consent and being adults (> 18 years); meanwhile, subjects who did not answer the instrument questions were excluded.
Instruments
A Likert scale was employed to evaluate the quality of health care, consisting of 57 items with 6 response options ranging from 1 (completely disagree) to 6 (completely agree). Items were divided into four dimensions: (1) Patient as a person; (2) Biopsychosocial perspective; (3) Therapeutic alliance; and (4) Sharing power and responsibility. The scale was scored by the arithmetic sum of each item’s score, with higher scores indicating higher quality of health care.
Design
Instrumental [17]. The construct validity of the scale was assessed through a factorial analysis, and internal consistency was assessed by using Cronbach’s α and McDonald’s ω.
Procedure
Samples A and B completed the instrument in November 2022, while Sample C completed the instrument in February 2023. Subjects were requested for voluntary participation by investigators who explained the study objectives and addressed any questions. Subjects eligible for being enrolled in the study signed an informed consent form and then answered the instrument.
Data analysis
Data were analyzed in four sequential steps. Step 1: the structure of the 4-factor model described by Mead & Bower model [4] was evaluated through a confirmatory factor analysis in the Group A. Step 2: Given high correlation between factors resulting from the evaluation of the 4-factor model, it was decided to start with an exploratory factor analysis to identify the initial structure of the instrument using data from sample A. Step 3: Here, data from Sample A were used to identify the initial structure of the instrument through exploratory factorial analysis. Step 2: The investigators used Sample B to verify the previously assessed instrument structure by confirmatory factorial analysis. In Step 4, confirmatory factorial analysis was performed using Sample C. This additional confirmatory factorial analysis was performed due to the number of refinements on the adjusted model during the previous steps.
In step 1, where the 4-factor model was evaluated to verify the goodness of fit of the model, the following indices were addressed: for absolute fit, the chi-square test (χ2) and the chi-square divided by degrees of freedom (χ2/df); for a parsimonious fit, the root mean square error of approximation (RMSEA) with the confidence interval (CI); and for incremental fit, the Tucker-Lewis index (TLI) and the comparative fit index (CFI). Acceptable fit values were considered as follows: χ2/df ≤ 5, RMSEA ≤ 0.08, TLI ≥ 0.90, CFI ≥ 0.90; and excellent fit values: χ2/df ≤ 2, RMSEA ≤ 0.05, TLI ≥ 0.95, CFI ≥ 0.95 [26, 27]; Likewise, the presence of independent factors was evaluated (i.e., r 0.80), which would allow an overfactoring effect to be avoided [23].
Afterward, an item analysis was performed, which involved identifying extreme responses within 90% or more of the choices, following this item elimination. The mean, standard deviation, and skewness and kurtosis coefficients were calculated. Univariate normality was assessed using the Shapiro‒Wilk test, while multivariate normality was assessed using the Mardia coefficient. Discriminative power for items was estimated using the extreme groups strategy, contrasting scores below the first quartile and above the third quartile of each item with one-tailed independent groups t tests. This test was selected due to its robustness and capability to handle deviations from normality [28]. The corrected item-total correlation was also calculated. Items with tests lacking discriminative capability or r values < 0.20 were removed [29]. To detect redundant items, a multicollinearity analysis was performed, and items with an interitem correlation of ≥ 0.80 were removed [30].
By correlation matrix determinant calculation, Bartlett’s test, and the Kaiser‒Meyer‒Olkin (KMO) index along with the confidence interval (CI), the sample adequacy of the data was assessed. In cases of inadequate KMO values (i.e., KMO ≤ 0.70), an individual adequacy analysis was performed based on the anti-image correlation matrix (AIM), and the item with the lowest value on the AIM’s main diagonal was eliminated. Following this, the sample adequacy tests were recalculated.
To mitigate factor overestimation, a parallel analysis was conducted, retaining factors that explained variance exceeding the 95th percentile random-generated factors. This strategy provides objective grounds for factor retention [31] as opposed to methods such as Kaiser’s criterion or scree plot analysis, which often overestimate the number of factors [32].
Subsequently, an exploratory factorial analysis was conducted using the polychoric correlation matrix by the robust diagonally weighted least squares (DWLS) method and oblique promax rotation. Retaining a factor required a minimum of 3 items, each with a factor loading ≥ 0.40 (i.e., simple factorial structure), a communality (h2) ≥ 0.32 [33], conceptual congruence between item and factor, and each factor showing a reliability ≥ 0.70 as calculated by Cronbach’s α and McDonald’s ω.
In Step 3, a confirmatory factorial analysis was performed using the maximum likelihood estimation method. The same criteria using in the step 1 were used to verify the goodness of fit of the model. During this process, both statistical criteria (modification indices and factor loading of each item) and theoretical considerations (conceptual coherence of item and factor) were considered to maintain the instrument’s conceptual value [34]. Internal consistency was evaluated using the final adjusted model. Items with a Cronbach’s α and McDonald’s ω > 0.94 were assessed for multicollinearity, and items with an interitem correlation ≥ 0.80 were removed.
Step 4 included a confirmatory factorial analysis and a multigroup confirmatory factorial analysis, both using the maximum likelihood method.
Data analysis was performed using SPSS v.23, AMOS v.21, and FACTOR v.12.03.02. When applicable, a significance level of p ≤ .05 was considered significant.
Results
Original model evaluation
Table 1 shows the results of the initial factorial model adjustment. Acceptable adjustment criteria were obtained by χ2/gl and RMSEA indices. Although the CFI and the TLI remain below the acceptable level, re-specification actions based on the analysis of the modification indices and the theoretical conception could achieve an acceptable model. However, the high correlations between the 4 factors (i.e., r ≥ .80) (Table 2) indicate an overfactoring effect and therefore the risk of overfitting [23] increases. Furthermore, these values suggest an uneconomical theoretical model, since with a smaller number of factors and/or reagents a more parsimonious instrument could be obtained. Due to this, an exhaustive analysis of the instrument was carried out, starting with the evaluation of each individual item behavior, and conducting an exploratory and confirmatory factor analysis.
Items diagnosis
No item concentrated ≥ 90% of choices in any of the extreme response options. The mean and standard deviation of item scores ranged from 3.76 to 5.19 and from 0.86 to 1.62, respectively. The skewness and kurtosis coefficients were ≤ |1.11| and ≤ |1.65|, respectively, with no evidence of univariate normality (p < .001) or multivariate normality (p < .001). All scale items discriminated (p < .05). Most items showed a corrected item-total correlation > 0.30, except for items 22, 31, and 56 (Table 3). Interitem correlation analysis identified an r ≥ .80 in 15 items, which were removed for subsequent analyses (i.e., 4, 5, 6, 20, 21, 27, 29, 35, 36, 38, 39, 41, 43, 45, 49).
Exploratory factorial structure
The polychoric matrix was initially nonpositive definite, so the sweet smoothing algorithms developed by [35] were implemented. Once the matrix was positive definite, tests of sample adequacy indicated that scale data were appropriate for conducting the factor analysis: KMO = 0.97, Bartlett’s test p < .01, and determinant of the correlation matrix < 0.000001. Parallel analysis identified a single factor that explained the variance exceeding the 95th percentile of variance by random factors. The exploratory factor analysis retained 35 items (Table 4), which met the previously specified criteria, organized into a single factor that explained 49% of the variance with an internal consistency α Cronbach and ω McDonald = 0.97. Items 9, 13, 48, and 51 were removed due to communality < 0.32.
Confirmatory factorial structure, sample B
The initial evaluation of factor structure was unsatisfactory, prompting a review of the modification indices aimed at model refinement to achieve at least acceptable fit indices. The analysis focused on the covariance value between items. With high values observed between item pairs, their conceptual relevance and wording were scrutinized. When items had similar semantic structures (e.g., “I receive respectful treatment at this medical unit” and “The rules and regulations are communicated and respected at the medical unit”) or referred to similar ideas (e.g., “There is good communication between doctors and me” and “The doctors’ good communication in this unit makes me feel committed to my health”), the item with the lower factor loading was removed. This process led to the removal of 24/35 items (1, 3, 7, 11, 12, 16, 17, 23, 24, 26, 28, 30, 33, 34, 37, 40, 42, 44, 47, 50, 52, 53, 54, 55), achieving acceptable (χ2/df, RMSEA) to high (TLI, CFI) fit criteria (Table 5). Sample B showed internal consistency of the 11-item model, as shown by Cronbach’s α and McDonald’s ω = 0.93.
Confirmatory factorial structure, sample C
Table 6 shows the results of the factorial model fit with 11 resulting items from Sample C (Fig. 2). Acceptable fit criteria are observed for χ2/gl, TLI, and CFI indices; however, the RMSEA index value was not acceptable.
The internal consistency of the 11-item model using Sample C was Cronbach’s α and McDonald’s ω = 0.98.
Factorial structure of the instrument to evaluate Person-Centered Care in Health Services. Values shown on the lines that join the factor with the reactants represent the factor loadings and those values placed on one side of the rectangle that represents the reactants are the R2. Hair et al. [36] argues that standardized factor loadings should ideally be 0.7, which implies a variance of 49%, that is, R2 = 0.49
The final items of the instrument are shown in Table 7, indicating to which factor of the original instrument they belonged (Appendix C).
Discussion
Patients’ positive experiences regarding medical care and low complication rates have been proposed as essential components of healthcare quality, encompassing patient-centered care. While some authors debate whether there is a correlation between technical care quality and interpersonal quality as reflected by patient satisfaction [37], facts have shown that reducing complications can lead to a better hospital experience. On the other hand, considering and addressing individuals’ needs promotes shared responsibility and increases success in health care, creating a virtuous circle that encompasses both technical and interpersonal aspects of quality. Hence, it is important to measure patient-centered care.
The instrument validation based on exploratory factorial analysis indicated a unifactorial structure with high overall internal consistency, explaining 49% of the variance.
The single-factor model is consistent with the fact that original model showed redundancy between factors [23]. In this way, with a smaller number of factors and items, redundant elements were eliminated, and a parsimonious instrument was obtained, adjusted from statistical estimates and a theoretical conception derived from the Patient-Centered Care model of Mead and Bower [4].
The inconsistency between the instrument structure and the conceptual framework (Mead and Bower’s Patient-Centered Care model [4]), which identifies four dimensions: (1) biopsychosocial perspective, (2) patient as a person, (3) therapeutic alliance, and (4) shared power and responsibilities might be supported by the close conceptual relationship among the dimensions considered in the model. For example, the “biopsychosocial perspective” of care implies healthcare staff’s willingness to engage with the range of difficulties raised by patients, not only with biomedical issues [38]. This is closely related to the concept of the “patient as a person” or individual experience illness as described by Armstrong [39], encompassing the difficulties expressed by patients beyond the biomedical issues. On the other hand, Balint [40] notes that healthcare providers should understand signs and symptoms not only in terms of diseases but also as expressions of the patient’s individuality, conflicts, and problems. This suggestion is in accordance with the “biopsychosocial factor” tightly related to the dimension “patient as a person”. On the other hand, the factor “shared power and responsibility”, described by Byrne and Long [41], refers to patients’ involvement in their health care and implies a symmetrical relationship, in line with what the “biopsychosocial” and “patient as a person” factors imply; this involves recognizing patients’ needs and preferences to encourage them to express ideas, listen, reflect, and collaborate. The quality of the doctor‒patient relationship, considering the above discussion, leads to the so-called “therapeutic alliance,” a factor that involves shared management of illness and decision-making. Crow et al. [42] point out that friendly and understanding attitudes from the patient improve their conditions, as affection impacts the outcome of medical treatment-mediated health. Thus, the selected items generally encompass the concept of patient-centered care, where factors beyond the biomedical model are considered, focusing on patients’ individualities and fostering an affectionate and equal relationship between doctor and patient. In summary, the abovementioned factors suggest that exploratory structure is conceptually and empirically consistent.
The parallel analysis carried out for exploratory factor analysis provides this study with assurance on the instrument factorial structure [31]. Furthermore, the use of oblique rotation increases the likelihood that psychological constructs are correlated with each other, as opposed to an orthogonal case [43]. Additionally, employing confirmatory factorial analysis allowed us to evaluate the initial identified structure more strictly, enabling the model to be respecified until achieving at least acceptable fit indices. Model refinement involved the removal of items based on high covariance between pairs with similar semantic structures. This procedure, together with the establishment of fit criteria ranging from acceptable to high, resulted in a brief instrument with high internal consistency (Cronbach’s alpha = 0.93).
Finally, a new confirmatory factorial analysis was performed with the 11-item scale after the phase 2 refinement, achieving adequate goodness-of-fit criteria on most of the considered items, thus confirming the previously proposed model. The sample size in the final confirmatory factor analysis could affect the values obtained by RMSEA. According to Morata-Ramírez [44], the percentage of acceptance of the models through RMSEA increases as the sample size increases, with mean values of 0.133 for samples of 100 subjects decreasing to 0.043 for samples of 850 subjects. An unacceptable RMSEA indicates that there may be an inconsistency between the estimated theoretical model and the real behavior of the populations, suggesting the evaluation and/or the review of the items wording or the re-specification of the model itself. However, the suggested cut-off points such as RMSEA, CFI and TLI are largely based on intuition and experience rather than statistical justification [45]. In this regard, although Hu and Bentler [46] suggested a RMSEA less than 0.06 and a CFI and TLI greater than 0.95, these authors point out that such criteria only refer to continuous data that are analyzed using the maximum likelihood (ML) of the normal theory. These authors warn that the suggested cut-off values may not generalize to conditions that were not addressed in their study, nor to estimation methods other than ML.
One of the study limitations is that only patients from PEMEX healthcare service users were considered, making it difficult to generalize to other populations. Furthermore, other types of validity testing are needed, such as discriminant and predictive validation. Future studies should address these limitations.
The application of an instrument that measures the level of person-centered care allows for interventions or strategies to improve patient engagement during care and to optimize healthcare resources [47]. In this regard, Holt [12] points out that improving the quality of healthcare should involve understanding the nature and relationships between patient experience, history, and expectations. The instrument we designed and validated should be used for ongoing and systematic assessment, identifying the degree to which the care provided is patient-centered. When healthcare services fail to meet patients’ expectations of care, it is less likely for patients to engage responsibly, adhere to treatments, and share responsibility for their own health condition with physicians and healthcare institutions [48].
Conclusions
The instrument, validated with users of PEMEX healthcare services, demonstrates adequate psychometric properties to be used as a tool for measuring the degree of person-centered care. The use of this instrument could represent a strategy or means for promoting an innovative and functional healthcare model that encompasses both the interpersonal and technical dimensions, thus moving away from the exclusively biomedical model.
Data availability
and Materials.
The datasets of the current study are available from the corresponding author upon reasonable request.
Abbreviations
- MAS/ACM:
-
Anti-image Correlation Matrix
- CFI:
-
Comparative Fit Index
- CI:
-
Confidence Interval
- COSMIN:
-
Consensus-based Standards for the selection of health Measurement Instruments
- DWLS:
-
Diagonally weighted least squares
- KMO:
-
Kaiser-Meyer‐Olkin
- C/K:
-
Kurtosis
- M:
-
Mean
- PEMEX:
-
Petróleos Mexicanos
- rr-tc/ ri-tc:
-
Correction of item-total correlations
- RMSEA:
-
Root mean square error of approximation
- S:
-
Skewness
- SD:
-
Standard Deviation
- TLI:
-
Tucker‒Lewis Index
- S:
-
Skewness
References
Donavedian A. Evaluating the Quality of Medical Care. Milbank Quarterly. 2005; 83(4): 691–729. https://doi.org/10.2307/3348969.
Lorenzo S. Hacia nuevos planteamientos de calidad. El paciente como coprotagonista. Informe SESPAS 2008. Gaceta Sanitaria. 2008; 22(1): 186– 191. https://doi.org/10.1016/S0213-9111(08)76091-6.
Charles C, Whelan T, Gafni A. What do we mean by partnership in making decisions about treatment? BMJ. 1999; 319(7212): 780–782. https://doi.org/10.1136/bmj.319.7212.780.
Mead N, Bower P. Patient-centeredness: a conceptual framework and review of the empirical literature. Social Science & Medicine. 2000; 51(7): 1087–1110. https://doi.org/10.1016/S0277-9536(00)00098-8.
Pascual López JA, Gil Pérez T, Sánchez Sánchez JA, Menárguez Puche JF. Cuestionarios De atención centrada en la persona en atención primaria. Una revisión sistemática. Aten Primaria. 2020;52(10):738–49. https://doi.org/10.1016/j.aprim.2019.11.004.
Nolte E, Merkur S, Anell A, North J. Person-centredness: exploring its evolution and meaning in the health system context. In: Nolte E, Merkur S, Anell A, editors. Achieving person-centered Health systems: evidence, Strategies and challenges. Cambridge: Cambridge University Press; 2020. pp. 19–40. https://doi.org/10.1017/9781108855464.005.
Hartzband PH, Groopman J. Keeping the patient in the equation-humanism and health care reform. BMJ. 2009; 361: 554–555. https://doi.org/10.1056/NEJMp0904813.
Coulter A, Magee H. The European patient of the future. 1st ed. Maidenhead: Open University; 2003.
Kassirer JP. Incorporating patients’ preferences into medical decisions. The New England Journal of Medicine. 1994; 330(26): 1895–1896. https://doi.org/10.1056/nejm199406303302611.
Mira JJ, Aranaz JM, Vitaller J, Ziadi M, Lorenzo S, Rebasa P, Aibar-Remón C. Percepción de seguridad clínica tras el alta hospitalaria. Medicina clínica, 2008; 131(3): 26–32. https://doi.org/10.1016/S0025-7753(08)76458-3.
Beach MC, Sugarman J, Johnson RL, Arbelaez JJ, Duggan PS, Cooper LA. Do patients treated with dignity report higher satisfaction, adherence, and receipt of preventive care. Annals of Family Medicine. 2005; 3: 331– 338. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1466898/.
Holt J. An evolutionary view of patient experience in primary care: A concept analysis. Nursing Forum. 2018; 53(4): 555–566. https://doi.org/10.1111/nuf.12286.
Sofaer S, Firminger K. Patient perceptions of the quality of health services. Annual Review of Public Health. 2005; 26: 513–559. https://doi.org/10.1146/annurev.publhealth.25.050503.153958.
Martsolf GR, Alexander JA, Shi Y, Casalino LP, Rittenhouse DR, Scanlon DP. The patient-centered medical home and patient experience. Health Services Research. 2012; 47(6): 2273 2295. https://doi.org/10.1111/j.1475-6773.2012.01429.x.
Pascual JA, Gil T, Sánchez JA, Menárguez JF. Cuestionarios de atención centrada en la persona en atención primaria. Una revisión sistemática. Atención Primaria. 2020; 52(10): 738–749. https://doi.org/10.1016/j.aprim.2019.11.004.
Mokkink LB, de Vet HCW, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, Terwee CB. COSMIN Risk of Bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1171–9. https://doi.org/10.1007/s11136-017-1765-4. Available From:.
Ato M, López-García JJ, Benavente A. Un sistema de clasificación de los diseños de investigación en psicología. Anales de Psicología/Annals of Psychology. 2013; 29(3), 1038–1059. https://doi.org/10.6018/analesps.29.3.178511.
Lemos V. Construcción y validación de una Escala para la Evaluación de la Deseabilidad Social Infantil (EDESI). Interdisciplinaria. 2005; 22(1), 77–96. http://www.scielo.org.ar/pdf/interd/v22n1/v22n1a04.pdf.
Lynn M. Determination and quantification of content validity. Nursing Research. 1986; 35(6), 382–385. https://journals.lww.com/nursingresearchonline/citation/1986/11000/DeterminationandQuantificatonOfContent.17.aspx.
Gable RK, Wolf JW. Instrument development in the affective domain: measuring attitudes and values in corporate and school settings. Boston: Kluwer Academic; 1993.
Bertaux D. El Enfoque biográfico: su validez metodológica, sus potencialidades. En: Historia oral e historias de vida. Costa Rica: FLACSO, Cuadernos de Ciencias Sociales 18; 1988.
Kyriazos TA. Applied psychometrics: sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology. 2018; 9(8): 2207. https://doi.org/10.4236/psych.2018.98126.
Watkins MA. Step-by-step guide to Exploratory Factor Analysis with R and Rstudio. London: Routledge; 2023.
DeVon HA, Block ME, Moyle-Wright P, Ernst DM, Hayden SJ, Lazzara DJ, Savoy SM, Kostas-Polston E. A psychometric toolbox for testing validity and reliability. Journal of Nursing Scholarship. 2007; 39(2): 155–164. https://doi.org/10.1111/j.1547-5069.2007.00161.x.
Boomsma A, Hoogland JJ. The robustness of LISREL modeling revisited. In: Cudeck R, Du Toit S, Sörbom D, Jöreskog KG, editors. Structural equation modeling present and future: a festschrift in honor of Karl Jöreskog. Chicago: Scientific Software International; 2001. p 139 – 68.
Cheng CS. Theory of Factorial Design. Berkeley USA: Chapman and Hall/CRC; 2016.
Steppan M, Piontek D, Kraus L. The effect of sample selection on the distinction between alcohol abuse and dependence. International Journal of Alcohol and Drug Research. 2014; 3(2): 159 – 68. https://doi.org/10.7895/ijadr.v3i2.100.
De Winter JC. Using the Student’s t test with extremely small sample sizes. Practical Assessment, Research y Evaluation. 2013; 18(10): 1–12. https://doi.org/10.7275/e4r6-dj05.
Cortada de Kohan N. Teoría y métodos para la construcción de escalas de actitudes. 1st ed. Buenos Aires: Lugar Editorial; 2004.
Tabachnick BG, Fidell LS. Principal components and factor analysis. Using Multivar Stat. 2001;4(1):582–633.
Hayton JC, Allen DG, Scarpello V. (2004). Factor retention decisions in exploratory factor analysis: A tutorial on parallel analysis. Organizational research methods. 2004; 7(2):191–205. https://doi.org/10.1177/1094428104263675.
Baglin J. Improving your exploratory factor analysis for ordinal data: A demonstration using FACTOR. Practical Assessment. Research, and Evaluation. 2014; 19(1): 5. https://doi.org/10.7275/dsep-4220.
Tabachnick BG, Fidell LS. Using multivariate statistics. 3rd ed. Northridge Cal: Harper Collins; 1996.
Pérez E, Medrano LA, Sánchez RJ. (2013). El Path Analysis: conceptos básicos y ejemplos de aplicación. Revista Argentina de Ciencias del Comportamiento, 5(1), 52–66. https://www.redalyc.org/pdf/3334/333427385008.pdf.
Lorenzo-Seva U, Ferrando PJ. Manual of the program Factor. 2020. http://psico.fcep.urv.es/utilitats/factor/index.html.
Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis. 7th ed. London: Prentice-Hall; 2009.
Stein S, Day M, Karia R, Hutzler L, Bosco J. Patients’ Perceptions of Care Are Associated With Quality of Hospital Care. American Journal of Medical Quality. 2015; 30(4): 382–388. https://doi.org/10.1177/1062860614530773.
Stewart M, Brown J, Weston W, McWhinney I, McWilliam C, Freeman T. Patient-centered medicine: transforming the clinical method. London: Sage; 1995. https://doi.org/10.1136/bmj.311.7019.1580.
Armstrong D. The emancipation of biographical medicine. Social Science & Medicine. Part A: Medical Psychology & Medical Sociology. 1979; 13: 1–8. https://doi.org/10.1016/0271-7123(79)90002-6.
Balint M. The Doctor, his patient and the illness. 2nd edition. London: Pitman Medical Publishing Co;1964.
Byrne P, Long B. Doctors talking to patients. London: HMSO/Royal College of General Practitioners; 1976.
Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H. The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review. Health Technology Assessment. 1999; 3(3). https://pubmed.ncbi.nlm.nih.gov/10448203/.
Thurstone LL. Multiple factor analysis. Chicago: University of Chicago Press; 1947.
Morata-Ramírez M, HolgadoTello FP, Barbero-García I, Mendez G. Análisis factorial confirmatorio: recomendaciones sobre mínimos cuadrados no ponderados en función del error Tipo I de Ji-Cuadrado y RMSEA. Acción psicológica. 2015; 12(1), 79–90. https://doi.org/10.5944/ap.12.1.14362.
Xia Y, Yang Y, RMSEA, CFI. and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behavior Research Methods. 2019; 51, 409–428. https://doi.org/10.3758/s13428-018-1055-2.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999; 6(1), 1–55. https://doi.org/10.1080/10705519909540118.
Wolfe A. Institute of Medicine Report: Crossing the Quality Chasm: A New Health Care System for the 21st Century., Policy, Politics. & Nursing Practice. 2001; 2(3): 233–235. https://doi.org/10.1177/152715440100200312.
Kern LM, Dhopeshwarkar RV, Edwards A, Kaushal R. Patient experience over time in patient-centered medical homes. The American journal of managed care. 2013; 19(5): 403–410. https://pubmed.ncbi.nlm.nih.gov/23781893/.
World Medical Association. WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects. 2013. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
Sociedad Mexicana de Psicología. Código ético del psicólogo. México: Trillas; 2010.
American Psychological Association (APA). Ethical principles of psychologists and code of conduct. American Psychological Association. 2002; 57: 1060–1073. https://www.apa.org/ethics/code.
Acknowledgements
The authors want to acknowledge users of Pemex healthcare contributing to the Person-Centered Care Assessment Instrument in Healthcare Services. Additionally, the authors want to express gratitude to all the authorities who assisted during participant recruitment.
Funding
Authors declared that no internal or external funding was obtained.
Author information
Authors and Affiliations
Contributions
All authors have reviewed the manuscript and approve it for submission. Authors RLM and GYCM designed, drafted and edited the presented work, OSG and IGM drafted, edited and provided a critical review. Authors RPFE and DL were involved in the statistical analysis, results interpretation, critical review, and final approvals. Authors RCL, RAVD, and HAMA carried out the critical review and the final evaluation of the article.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The research protocol was submitted to the Regional Hospital of Salamanca Ethics Research Committee, obtaining the approval registration number HRSICIO74-03-2022. Prior to conducting the study, all participants were informed about their rights in accordance with the Declaration of Helsinki [49]. The study was conducted in compliance with current ethical regulations and ethical considerations for human research [50, 51].
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lehmann-Mendoza, R., Cortés-Moreno, G.Y., Sarabia-González, O. et al. Design and validation of an instrument to evaluate Person-Centered care in health services. Arch Public Health 82, 123 (2024). https://doi.org/10.1186/s13690-024-01324-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-024-01324-2