Abstract
Background
Electroencephalography (EEG) is recommended for the practical approach to the diagnosis and prognosis of encephalitis. We aimed to investigate the prognostic value of standard EEG (stdEEG) in adult patients with severe herpes simplex encephalitis.
Methods
We performed a retrospective analysis of consecutive ICU patients with severe herpes simplex encephalitis in 38 French centers between 2006 and 2016. Patients with at least one stdEEG study performed at ICU admission were included. stdEEG findings were reviewed independently by two investigators. The association between stdEEG findings (i.e., background activity, lateralized periodic discharges, seizures/status epilepticus, and reactivity to painful/auditory stimuli) and poor functional outcome, defined by a score on the modified Rankin Scale (mRS) of 3 to 6 (moderate to severe disability or death) at 90 days, were investigated.
Results
We included 214 patients with at least one available stdEEG study. The first stdEEG was performed after a median time of one (interquartile range (IQR) 0 to 2) day from ICU admission. At the time of recording, 138 (64.5%) patients were under invasive mechanical ventilation. Lateralized periodic discharges were recorded in 91 (42.5%) patients, seizures in 21 (9.8%) and status epilepticus in 16 (7.5%). In the whole population, reactivity to auditory/noxious stimuli was tested in 140/214 (65.4%) patients and was absent in 71/140 (33.2%) cases. In mechanically ventilated patients, stdEEG reactivity was tested in 91/138 (65.9%) subjects, and was absent in 53/91 (58.2%) cases. Absence of reactivity was the only independent stdEEG finding associated with poor functional outcome in the whole population (OR 2.80, 95% CI 1.19 to 6.58) and in the subgroup of mechanically ventilated patients (OR 4.99, 95% CI 1.6 to 15.59). Adjusted analyses for common clinical predictors of outcome and sedation at time of stdEEG revealed similar findings in the whole population (OR 2.03, 95% CI 1.18 to 3.49) and in mechanically ventilated patients (OR 2.62, 95% CI 1.25 to 5.50).
Conclusions
Absence of EEG reactivity to auditory/noxious stimuli is an independent marker of poor functional outcome in severe herpes simplex encephalitis.
Similar content being viewed by others
Background
Herpes simplex virus (HSV) is the leading cause of sporadic encephalitis in adult patients [1]. It is a life-threatening disease with a mortality rate of 6–10% [2], which can rise to 70% without appropriate treatment [3, 4]. However, despite early initiation of intravenous acyclovir, HSV encephalitis (HSE) remains associated with a poor neurological outcome, as half of the patients present moderate to severe disability at 1 year [5, 6]. The practical diagnostic approach to suspected HSE encephalitis requires an early multimodal evaluation including a clinical examination, brain imaging, HSV DNA detection in the cerebrospinal fluid (CSF) by polymerase-chain reaction (PCR), and standard electroencephalography (stdEEG) [7].
Standard EEG is often considered as an easily accessible, non-specific tool in the intensive care unit (ICU). It is recommended for initial evaluation of patients with suspected encephalitis to detect focal or diffuse changes suggestive of encephalitis and to rule out non-convulsive seizures [7]. Standard EEG patterns during HSE include changes in background activity in 46.4% of cases, focal or generalized slowing in 28.6%, seizures or status epilepticus in 17.8%, and periodic discharges in 11.5% [8,9,10,11,12]. However, the prognostic value of stdEEG changes in HSE has been little studied. In a single-center retrospective study conducted on 103 patients hospitalized for all-cause encephalitis, including 12 HSE, a normal stdEEG was independently associated with a lower relative risk of death [12]. In another retrospective series of 45 HSE, stdEEG abnormalities were not associated with functional outcome [13]. A retrospective cohort study of 42 patients with primary central nervous system (CNS) infections, including 27 viral infections, found that continuous EEG monitoring recorded seizures in about 33% of patients and periodic epileptiform discharges in 40%, both independently associated with poor outcome [14]. However, continuous EEG monitoring data in primary CNS infections has been scarcely reported.
In the present study, we aimed to investigate the prognostic value of common stdEEG findings observed in severe adult cases of HSE encephalitis requiring care in the ICU.
Methods
Design
We conducted a retrospective analysis of patients from the multicenter HERPETICS database, which included adult patients with HSV encephalitis between January 2006 and December 2016 in 38 ICUs in France [15]. The ethical committee of the French society of Intensive Care Medicine (FICS) approved the study and waived the requirement for informed consent. Inclusion criteria were: (a) a minimum age of 18 years; (b) admission to the ICU with possible or probable acute encephalitis, as defined by the Consensus Statement of the International Encephalitis Consortium; [7] (c) a positive CSF PCR for HSV DNA during hospitalization; (d) and at least one stdEEG recording performed at admission or during ICU stay. Exclusion criteria were: (a) missing data on clinical outcome at 90 days; (b) missing or incomplete stdEEG data. Standard EEG data was reviewed independently by 2 investigators, including a neurologist (LJ) and a neurophysiologist (GV).
Clinical biological and brain imaging data
We used the data previously collected for the HERPETICS database, including patients’ history, neurological symptoms and reason for ICU admission, clinical, biological and imaging data, and therapeutics [15].
Standard EEG studies
We collected the following data from stdEEG reports: date of study, indication, and ongoing sedative and/or antiseizure medication at the time of the recording. We followed the American Clinical Neurophysiology Society’s guidelines to describe findings collected from stdEEG reports [16]: background activity voltage, asymmetry, continuity and frequency (minimal and maximal), periodic discharges, interictal epileptic activities (e.g. sharp waves, spikes, spike-and-waves), electrographic or electroclinical seizures, status epilepticus, and reactivity to external stimuli. A background frequency in the alpha range is defined by a frequency > 7 Hz but < 13 Hz [16]. Status epilepticus was defined as an electroclinical seizure for ≥ 10 continuous minutes or for a total duration of ≥ 20% of any 60-min period of recording, or ≥ 5 continuous minutes in cases of a bilateral tonic–clonic activity [16]. Reactivity was defined as transient changes in the stdEEG voltage and/or frequency immediately after an auditory or noxious stimulus. Reactivity on stdEEG recordings was categorized as “present”, “absent”, or “not tested” (when no auditory/noxious stimulus was applied during the recording) [16].
Second stdEEG
If more than one stdEEG study was available, we collected data from the first and second recordings. We studied evolution of reactivity between subsequent stdEEG studies and classified patients as “preserved reactivity” when both stdEEG were reactive to external stimuli, “absent reactivity” when none of the two stdEEG was reactive, and “variable reactivity” in patients with discordant reactivity between stdEEG studies (presence of reactivity followed by absence of reactivity, or vice versa).
Outcomes
The primary outcome was a poor functional outcome at 90 days, defined by a score on the modified Rankin Scale (mRS) of 3 to 6, indicating moderate to severe disability or death.
Statistical analysis
Patients’ characteristics are expressed as counts and frequencies for categorical variables and medians (interquartile range, IQR) for quantitative variables. Comparisons were achieved using the Wilcoxon rank sum test for continuous variables and Fisher’s test for categorical variables. We investigated the association of the first stdEEG findings with poor functional outcome in the whole cohort by means of univariable and multivariable logistical regression analyses. First, variables associated with outcome in univariable analysis (p-value < 0.20) were entered in the multivariable model. Second, we applied a backward elimination to select variables for the final model. Secondary analyses included a subgroup analysis in patients under mechanical ventilation and adjusted analyses for common clinical predictors of outcome (i.e., age, coma, and body temperature) and sedation at the time of EEG recording. Missing data were treated with multiple imputations using PROC MI and PROC MIANALYZE (SAS Software). All tests were two-sided and a p-value < 0.05 was considered statistically significant. All analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, NC) and R statistical software version 3.5.2 (R Project for statistical computing).
Results
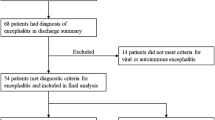
A total of 286 patients were screened, and 214 patients from 38 centers were included in the study (see patients flow chart, Additional file 1: Figure S1). There was no difference between characteristics of included patients who benefited from a stdEEG, and those of excluded patients who did not have a stdEEG recording or had missing stdEEG data (Additional file 1: Table S1). Baseline characteristics of patients are detailed in Table 1. The median age was 63 years (IQR 53–72) and 111 (51.9%) patients were male. A total of 105 (49.1%) patients were admitted to the ICU for altered mental status and 54 (25.2%) patients for seizures. 138 (64.5%) patients underwent mechanical ventilation.
Among the 214 patients, 140 (65.4%) subjects had one stdEEG, 42 (19.6%) had two stdEEGs, 14 (6.5%) had 3 and 18 (8.4%) had more than 3 stdEEGs. Data from the first available stdEEG is detailed in Table 1 and the correlation between EEG variables at the time of the recording is represented in Fig. 1. Median delays between ICU admission and the first stdEEG and between acyclovir administration and the first stdEEG were 1 (IQR 0–2) day, and 1 (IQR 1–3) day, respectively. Twenty-seven patients had their first stdEEG before admission to the ICU (with a median delay of 2 days (IQR 1–5) for these patients). Out of 192 stdEEG studies, 105 (54.7%) were performed for suspicion of encephalitis, 79/192 (41.1%) to rule out seizures and status epilepticus and 16/192 (8.3%) for both of these motives. Thirty-two patients out of 209 (15.3%) stdEEG recordings presented with a suppressed or low voltage, 25/213 (11.7%) were asymmetric in voltage and 65 (30.5%) were asymmetric in frequency. Thirteen out of 169 (7.7%) recordings had a maximal background rhythm frequency in the delta range. Lateralized periodic discharges (LPDs) were recorded in 91 (42.5%) patients. Sixty (28%) patients had interictal epileptic activities with spikes or sharp waves in 46 (21.5%) patients and spike-and-waves in 14 (6.5%) patients. Seizures were recorded in 21 (9.8%) patients and 16 (7.5%) presented with status epilepticus at the time of the first stdEEG. Reactivity was tested in 140/214 (65.4%) patients and was present in 69/140 (49.3%) recordings. No differences were found between the characteristics of patients for whom reactivity was tested, and those for whom it was not studied (Additional file 1: Table S1).
Overall, 157 (73.4%) patients had a poor functional outcome at 90 days, including 38 (17.8%) deaths. Results of the multivariable analyses of factors associated with poor functional outcome are presented in Table 2, and detail for the univariable and multivariable analyses can be found in Additional file 1: Table S2. The characteristics of stdEEG included in the multivariable model were maximal background frequency, and stdEEG reactivity. A stdEEG with “absent reactivity” was found to be the only variable independently associated with poor functional outcome (OR 2.80, 95% CI 1.19 to 6.58). A maximal background frequency recorded in the alpha range was found not to be independently associated with functional outcome (p = 0.187) in the multivariable analysis (Additional file 1: Table S2).
A secondary subgroup analysis performed in patients under mechanical ventilation (Table 2 and Additional file 1: Table S3) confirmed that absence of stdEEG reactivity was significantly associated with poor functional outcome in this population (OR 4.99, 95% CI 1.6 to 15.59). Secondary adjusted analyses for common clinical predictors of outcome and sedation at time of EEG revealed similar findings in the whole population (OR 2.03, 95% CI 1.18 to 3.49) and in patients under mechanical ventilation (OR 2.62, 95% CI 1.25 to 5.50).These analyses are presented in Table 2, Additional file 1: Tables S2bis and S3bis.
Seventy-four (35%) patients had at least a second stdEEG recording after a median time of 5 (IQR 2–12) days from the ICU admission. As for the first recording, the subsequent stdEEG were performed for seizures in 37/71 (52.1%) patients, for encephalitis suspicion in 14/71 (19.7%) patients, for both of these motives in 1/71 (1.4%) patients or to control the abnormalities shown on the first stdEEG in 16/71 (22.5%) patients. Sixteen (22%) patients had a first stdEEG with “present reactivity” and eight (50%) of them presented with preserved reactivity on the second stdEEG (Fig. 2). Of these eight patients with preserved reactivity in both stdEEGs, 5 (63%) had poor functional outcome at day 90. On the contrary, 58 (78%) patients had a first stdEEG with absence of reactivity, and among them 37 (50%) had a second stdEEG where reactivity was still absent. A persistent stdEEG with absent reactivity was associated with a poor functional outcome in 31/37 (84%) of these patients. Twenty-nine patients, classified as “variable reactivity”, had discordant reactivity between stdEEGs, and 21/29 (72%) patients had a poor functional outcome.
Association of EEG reactivity on the first and second stdEEGs with outcome. If more than one stdEEG study was available, we collected data from the first and second studies. We classified patients as “preserved reactivity” when both stdEEG were reactive to external stimuli, “absent reactivity” when none of the two stdEEG was reactive, and “variable reactivity” in patients with discordant reactivity between stdEEG studies (presence of reactivity followed by absence of reactivity, or vice versa). A poor outcome was defined by a score of 3–6 on the modified Rankin scale
Discussion
This retrospective study assembled 214 critically ill patients with HSE from 38 centers, with available stdEEG data and assessment of poor functional outcome (i.e., moderate to severe disability or death) at day 90. Our findings suggest that the lack of EEG reactivity to external stimuli in critically ill patients with HSE is independently associated with poor functional outcome. This result was confirmed in a subgroup analysis of mechanically ventilated patients, who can be considered as the most severely affected patients with HSE encephalitis. Moreover, the prognostic value of absent EEG reactivity was independent of common prognostic factors identified in this population (including age, coma, and fever at admission) [15] and was independent of sedation at time of EEG recording. Previous monocentric studies conducted in the non-ICU setting identified EEG patterns associated with outcome [8], such as Synek grades of I and II being predictive of good neurological prognosis. To our knowledge, our study is the largest cohort of patients with herpes simplex encephalitis requiring care in an ICU investigating stdEEG patterns associated with poor neurological prognosis.
The results from our study add to the recent body of evidence highlighting the prognostic role of EEG reactivity in critically ill patients with primary or secondary brain injury [17,18,19]. These results are consistent with a recent retrospective study of 121 unresponsive ICU patients with various diagnoses (e.g., respiratory, circulatory or neurologic failure), showing that the combination of the presence of reactivity on a stdEEG with a background frequency greater than 4 Hz was the only variable independently associated with a reduced risk of death [20]. Another study combined the same markers for assessing prognosis, and showed that a lower background frequency was independently associated with unfavorable outcome at 28 days in patients under venoarterial extracorporeal membrane oxygenation [21]. In our study, we could not easily combine markers such as background frequency and reactivity since minimal or maximal background frequencies were not reinterpreted as continuous variables and were not retained in the final multivariable model.
Standard EEG is of crucial importance for the positive diagnosis of herpes simplex encephalitis and its complications, notably seizures, status epilepticus and periodic discharges that can indicate parenchymal necrosis. Previous studies have mainly investigated the role of stdEEG in the positive diagnosis of HSE, especially in complex cases [11], and little data is available about prognostication. A retrospective, monocentric cohort of 29 patients, with stdEEG recordings performed in 25 patients, found stdEEG patterns (i.e. Synek III to V) to be associated with poor clinical outcome at 6 months [8]. However, stdEEG data only included Synek grade and the presence of LPDs, and reactivity to external stimuli was not reported.
The prognostic value of stdEEG recordings, however, has been studied in brain injuries of other kinds. In a large registry of cardiac arrest patients, absence of EEG reactivity was predictive of unfavorable outcome [18]. Preserved EEG reactivity was found to be associated with good clinical outcome after cardiac arrest in a post-hoc analysis of a prospective study, especially in patients with a discontinuous normal voltage stdEEG background pattern [22]. A recent review emphasized the link between preserved stdEEG reactivity and favorable clinical outcomes in consciousness impairments of various etiologies, but highlights the need for homogenous and consensual methods for reactivity assessment during stdEEG recordings [17].
Interestingly, the persistence of reactivity over time could be associated with neurological outcome. Indeed, when dividing the 74 patients who had at least two stdEEGs during hospitalization into three groups, we noted a worsening of the neurological prognosis when stdEEGs reactivity remained absent over time. Patients who had reactivity present on both stdEEGs (“preserved reactivity” group) had poor neurological prognosis in 63% of cases. Those who showed reactivity on neither stdEEG (“absent reactivity” group) had a poor prognosis in 84% of cases. The intermediate group (“uncertain reactivity”) with reactivity being present in only one of the two stdEEGs, seemed to evolve towards a poor prognosis in 72% of cases. Although our data was underpowered to allow proper analysis given the small number of patients who benefited from two stdEEGs or more, our study suggests that repeating stdEEG recordings as a follow-up for reactivity could be helpful during the ICU stay. This result requires confirmation by a prospective study with a standardized protocol (e.g. performing a stdEEG upon arrival to the ICU, followed by recordings at regular intervals).
Clinical elements for prognostication in HSE have been identified in previous studies, such as older age, coma, admission body temperature and indirect admission to an intensive care unit [15]. Our study did not find seizures or status epilepticus to be associated with poor clinical outcome in HSE. A retrospective study of 54 critical care unit patients with continuous stdEEG monitoring diagnosed with viral or auto-immune encephalitis found 22 (41%) patients who presented seizures [23]. Patients with seizures had significantly more LPDs, low voltage and focal slowing, but seizures were not associated with functional outcome at discharge, in accord with the present results. However, only 11 patients had HSV encephalitis and 12 had encephalitis of unknown etiology.
Since only two patients had a normal MRI at ICU admission in our cohort, MRI lesions were already present in the majority at the time of stdEEGs recording. Our data was therefore insufficient to determine whether stdEEG could show abnormalities before MRI signs can be detected. A recent multicenter cohort study investigated MRI data associated with poor functional outcome and found that MRI signal abnormalities involving more than 3 cerebral lobes were associated with poor functional prognosis [24]. Lateralized periodic discharges are often considered as an EEG marker of brain injury. However, in our study, we did not find the number of cerebral lobes impaired by lateralized periodic discharges to be associated with a poorer neurological prognosis. This could be explained by the poor spatial resolution of stdEEG, making the precise localization of lesions and their extension difficult to establish.
The strength of this study was to assemble a large multicenter cohort of 214 HSE patients recruited from 38 ICUs in reference centers and smaller hospitals, which decreases the risk of center bias. The large number of patients allowed to performed multivariable analyses adjusted for common clinical predictors of outcome in this population. Our study also has limitations: firstly, this study had a retrospective design, which implies missing data (e.g. missing stdEEG reports) and lack of reproducibility between subjects: some patients had a stdEEG upon arrival to the ICU, others were recorded a few days later for complications or delay in the recovery of consciousness. This retrospective design did not allow proper standardization of stdEEG recordings, or a systematic assessment of reactivity with a unique protocol (same stimuli and recording length). Many stdEEG reports reported scarce data, not always in accordance with the American Clinical Neurophysiology Society’s standardized critical care EEG terminology [16], which might have resulted in the loss of important information. For instance, assessing Synek grades, a scale using stdEEG patterns to establish prognosis in adult patients with diffuse anoxic and traumatic encephalopathies [25], was only possible for a small portion of individuals in our study. Analyzing full stdEEG tracings by two independent reviewers, instead of stdEEG reports of various origins, could be a way to determine stdEEG patterns in HSE in a more objective way, but such tracings were unfortunately unavailable for retrieval. Moreover, the reports did not mention detailed clinical data at the time of the stdEEG recording, such as Glasgow Coma Scale, FOUR score or response to command, and most of the stdEEG reports had no precisions about the duration of the recording and number of electrodes. For the patients under mechanical ventilation, we could find no precision about the presence and type of sedation at the time of the recording. Secondly, our study lacks continuous stdEEG recordings which could allow a better monitoring of neurophysiological status (e.g., evolution and duration of status epilepticus or seizures), as some brief epileptic events might not be recorded with discontinuous short-lasting stdEEGs. This might have underpowered our study in assessing neurological prognosis and mortality in some patients, especially for epileptic complications. Thirdly, our population was limited to patients from intensive care units, which makes it difficult to extrapolate our results to less severely affected populations, such as patients admitted to neurology or infectious diseases departments. Finally, we observed that out of the 286 patients of the Herpetics database, 13 had not benefited from a stdEEG recording, while electroencephalography is recommenced for any suspicion of encephalitis. This could be explained by the large amount of centers in the study, including smaller hospitals, with no on-site Neurophysiology department and a more difficult access to electroencephalography, reflecting real-life access to the usual standard of care.
A prospective study with a standardized protocol for the timing of stdEEG recordings and the assessment of reactivity would be useful to extend our results. The persistence of stdEEG abnormalities over time (e.g. lack of reactivity) could also be studied, rather than the immediate stdEEG abnormalities in the acute phase. Such a study would allow the assessment of long-term cognitive prognosis, quality of life and epilepsy sequelae. However, HSE cases remain scarce, making the construction of such a protocol difficult.
Conclusion
The absence of electroencephalographical reactivity to external stimuli is an independent indicator of poor functional outcome in adult patients with severe herpes simplex encephalitis, notably for mechanically ventilated patients. In addition to its use for the diagnosis of herpes simplex encephalitis and its complications, electroencephalography could help identify prognostic factors in often complex clinical situations.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Mailles A, De Broucker T, Costanzo P, Martinez-Almoyna L, Vaillant V, Stahl JP, et al. Long-term outcome of patients presenting with acute infectious encephalitis of various causes in France. Clin Infect Dis. 2012;54(10):1455–64.
Modi S, Mahajan A, Dharaiya D, Varelas P, Mitsias P. Burden of herpes simplex virus encephalitis in the United States. J Neurol. 2017;264(6):1204–8.
Sköldenberg B, Alestig K, Burman L, Forkman A, Lövgren K, Norrby R, et al. Acyclovir versus vidarabine in herpes simplex encephalitis. The Lancet. 1984;324(8405):707–11.
Whitley RJ, Soong SJ, Dolin R, Galasso GJ, Chien LT, Alford CA, et al. Adenine arabinoside therapy of biopsy-proved herpes simplex encephalitis: National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study. N Engl J Med. 1977;297(6):289–94.
Jouan Y, Grammatico-Guillon L, Espitalier F, Cazals X, François P, Guillon A. Long-term outcome of severe herpes simplex encephalitis: a population-based observational study. Crit Care. 2015;19(1):345.
Raschilas F, Wolff M, Delatour F, Chaffaut C, De Broucker T, Chevret S, et al. Outcome of and prognostic factors for herpes simplex encephalitis in adult patients: results of a multicenter study. Clin Infect Dis. 2002;35(3):254–60.
Venkatesan A, Tunkel AR, Bloch KC, Lauring AS, Sejvar J, Bitnun A, et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the International Encephalitis Consortium. Clin Infect Dis. 2013;57(8):1114–28.
Kim YS, Jung KH, Lee ST, Kang BS, Yeom JS, Moon J, et al. Prognostic value of initial standard EEG and MRI in patients with herpes simplex encephalitis. J Clin Neurol. 2016;12(2):224.
Illis LS, Taylor FM. The electroencephalogram in herpes-simplex encephalitis. The Lancet. 1972;299(7753):718–21.
Upton A, Gumpert J. Electroencephalography in diagnosis of herpes-simplex encephalitis. The Lancet. 1970;295(7648):650–2.
Bradshaw MJ, Venkatesan A. Herpes simplex virus-1 encephalitis in adults: pathophysiology, diagnosis, and management. Neurotherapeutics. 2016;13(3):493–508.
Sutter R, Kaplan PW, Cervenka MC, Thakur KT, Asemota AO, Venkatesan A, et al. Electroencephalography for diagnosis and prognosis of acute encephalitis. Clin Neurophysiol. 2015;126(8):1524–31.
Singh TD, Fugate JE, Hocker S, Wijdicks EFM, Aksamit AJ, Rabinstein AA. Predictors of outcome in HSV encephalitis. J Neurol. 2016;263(2):277–89.
Carrera E, Claassen J, Oddo M, Emerson RG, Mayer SA, Hirsch LJ. Continuous electroencephalographic monitoring in critically ill patients with central nervous system infections. Arch Neurol. 2008;65(12):7.
Jaquet P, de Montmollin E, Dupuis C, Sazio C, Conrad M, et al. Functional outcomes in adult patients with herpes simplex encephalitis admitted to the ICU: a multicenter cohort study. Intensive Care Med. 2019;45(8):1103–11.
Hirsch LJ, Fong MWK, Leitinger M, LaRoche SM, Beniczky S, Abend NS, et al. American Clinical Neurophysiology Society’s standardized critical care EEG terminology: 2021 version. J Clin Neurophysiol. 2021;38(1):1–29.
Azabou E, Navarro V, Kubis N, Gavaret M, Heming N, Cariou A, et al. Value and mechanisms of EEG reactivity in the prognosis of patients with impaired consciousness: a systematic review. Crit Care. 2018;22(1):184.
Benghanem S, Paul M, Charpentier J, Rouhani S, Ben Hadj Salem O, Guillemet L, et al. Value of EEG reactivity for prediction of neurologic outcome after cardiac arrest: Insights from the Parisian registry. Resuscitation. 2019;142:168–74.
Benghanem S, Cariou A, Diehl JL, Marchi A, Charpentier J, Augy JL, et al. Early clinical and electrophysiological brain dysfunction is associated with ICU outcomes in COVID-19 critically ill patients with acute respiratory distress syndrome: a prospective bicentric observational study*. Crit Care Med. 2022;50(7):1103–15.
Legouy C, Girard-Stein L, Wanono R, de Montmollin E, Vellieux G, Bouadma L, et al. Association of standard electroencephalography findings with mortality and command following in mechanically ventilated patients remaining unresponsive after sedation interruption. Crit Care Med. 2021;49(4):e423–32.
Magalhaes E, Reuter J, Wanono R, Bouadma L, Jaquet P, Tanaka S, et al. Early EEG for prognostication under venoarterial extracorporeal membrane oxygenation. Neurocrit Care. 2020;33(3):688–94.
Admiraal MM, Horn J, Hofmeijer J, Hoedemaekers CWE, van Kaam CR, Keijzer HM, et al. EEG reactivity testing for prediction of good outcome in patients after cardiac arrest. Neurology. 2020;95(6):e653–61.
Viarasilpa T, Panyavachiraporn N, Osman G, Parres C, Varelas P, Van Harn M, et al. Electrographic seizures in patients with acute encephalitis. Neurocrit Care. 2019;30(1):207–15.
Sarton B, Jaquet P, Belkacemi D, de Montmollin E, Bonneville F, Sazio C, et al. Assessment of magnetic resonance imaging changes and functional outcomes among adults with severe herpes simplex encephalitis. JAMA Netw Open. 2021;4(7):e2114328.
Synek VM. Prognostically important EEG coma patterns in diffuse anoxic and traumatic encephalopathies in adults. J Clin Neurophysiol. 1988;5(2):161–74.
Acknowledgements
ENCEPHALITICA study group (collaborators):
Pierre Jaquet, Department of Intensive Care Medicine and Infectious Diseases, Bichat-Claude Bernard University Hospital, AP-HP, Paris, France.
Etienne de Montmollin, Department of Intensive Care Medicine and Infectious Diseases, Bichat-Claude Bernard University Hospital, AP-HP, Paris, France.
Claire Dupuis, Medical Intensive Care Unit, CHU Gabriel Montpied, Clermont Ferrand, France.
Mikael Alves, Polyvalent Intensive Care Unit, Poissy–Saint-Germain-en-Laye Hospital, Poissy, France.
Laurent Argaud, Medical Intensive Care Unit, CHU Edouard Herriot, Lyon, France.
Pierre Bailly, Medical Intensive Care Unit, La Cavale Blanche University Hospital, Brest, France.
François Barbier, Medical Intensive Care Unit, La Source Hospital, Orléans, France.
Lila Bouadma, Department of Intensive Care Medicine and Infectious Diseases, Bichat-Claude Bernard University Hospital, AP-HP, Paris, France.
Noelle Brulé, Medical Intensive Care Unit, Nantes University Hospital, Nantes, France.
Fabrice Bruneel, Medical Intensive Care Unit, André Mignot Hospital, Versailles, France.
Russell Chabanne, Department of Perioperative Medicine, Clermont-Ferrand University Hospital, Clermont-Ferrand, France.
Marie Conrad, Medical Intensive Care Unit, CHU de Nancy, France.
Daniel da Silva, Medical Intensive Care Unit, Delafontaine Hospital, Saint-Denis, France.
Frederic Dailler, Department of Anesthesiology and Intensive Care Medicine, Hôpital Pierre Wertheimer, Lyon, France.
Delphine Daubin, Medical Intensive Care Unit, Montpellier university hospital, Montpellier, France.
Sophie Demeret, Neurological Intensive Care Unit, CHU Pitié Salpétrière, Paris, France.
Nicolas Lerolle, Medical Intensive Care Unit, CHU Angers, Angers University Hospital, Angers, France.
Julien Marechal, Medical Intensive Care Unit, Centre Hospitalier Universitaire de Poitiers, Poitiers, France.
Bruno Mourvillier, Medical Intensive Care Unit, CHU de Reims, Reims, France.
Ahmed El Kalioubi, Medical Intensive Care Unit, Roger Salengro University Hospital, Lille, France.
Benjamine Sarton, Intensive Care Unit, Purpan University Hospital, Toulouse, France.
Stein Silva, Intensive Care Unit, Purpan University Hospital, Toulouse, France.
Romain Sonneville, Department of Intensive Care Medicine and Infectious Diseases, Bichat-Claude Bernard University Hospital, AP-HP, Paris, France.
Vincent Susset, Polyvalent Intensive Care Unit, Chambery, France.
Jean Marc Tadié, Intensive Care Medicine, CHU Pontchaillou, Rennes, France.
Jean-Françoit Timsit, Department of Intensive Care Medicine and Infectious Diseases, Bichat-Claude Bernard University Hospital, AP-HP, Paris, France.
Michel Wolff, Neurological ICU, Hôpital Saint Anne, Paris.
Alexandre Lautrette, Medical Intensive Care Unit, Gabriel-Montpied University Hospital, Clermont-Ferrand, France.
Emmanuel Novy, Polyvalent Intensive Care Unit, Mercy Hospital CHR Metz-Thionville, Ars-Laquenexy, France.
Bertrand Guidet, Medical Intensive Care Unit, Hôpital Saint-Antoine, Paris, France.
François Mateos, Intensive care Unit, Centre hospitalier Saint-Brieuc, Saint-Brieuc, France.
Clément Brault, Department of Intensive Care Medicine, Amiens-Picardie University Hospital, Amiens, France.
Quentin Maestraggi, Medical Intensive Care Unit and UMR 1121, Hautepierre Hospital Strasbourg, France.
Keyvan Razazi, Medical Intensive Care Unit, Hopitaux Universitaires Henri Mondor, Créteil, France.
Jean-Pierre Quenot, Medical Intensive Care Unit, Centre Hospitalo-Universitaire de Dijon, Dijon, France.
Aurélie Joret, Medical Intensive Care Unit, CHU de Caen, Caen, France.
Albrice Levrat, Intensive care unit, Centre Hospitalier Annecy-Genevois, Annecy, France.
Alexandre Massri, Intensive Care Unit, Centre Hospitalier Francois Mitterand Pau, France.
Alexandre Robert, Medical Intensive Care Unit, Hôpital de l'Archet 1, CHU de Nice, Nice, France.
Damien Contou, Polyvalent Intensive Care Unit, Centre Hospitalier Victor Dupouy, Argenteuil, France.
Jean-Paul Mira, Medical Intensive Care Unit, Cochin University Hospital, Paris, France.
Gaudry Stephane, Polyvalent Intensive Care Unit, Louis Mourier University Hospital, Colombes, France.
Guillaume Voiriot, Polyvalent Intensive Care Unit, Centre Hospitalier Universitaire Tenon, Paris, France.
Asael Berger, Intensive Care Unit, Centre Hospitalier de Haguenau, Haguenau, France.
Vincent Das, Medical-Surgical Intensive Care Unit, Centre Hospitalier Intercommunal André Grégoire, Montreuil, France.
Nicolas Engrand, Neurosurgical Intensive Care Unit, Fondation ophtalmologique Adolphe Rotschild, Paris, France.
Martin Murgier, Intensive care unit, Saint-Etienne University Hospital, Saint-Etienne, France.
Shidasp Siami, Polyvalent Intensive care unit, Centre Hospitalier Sud Essone Dourdan-Etampes-Siège, Etampes, France.
Sami Hraiech, Medical Intensive Care Unit, Aix-Marseille Universite, Hopital Nord, Marseille, France.
Eric Mariotte, Medical Intensive Care Unit, Saint-Louis Hospital, Paris, France.
Claire Ragot, Medical-Surgical Intensive Care Unit, Robert Boulin Hospital, Libourne, France.
Annabelle Stoclin, Intensive Care Unit, Institut Gustave Roussy, Villejuif, France.
Pierre Trouiller, Intensive Care Unit, Antoine Béclère Hospital, Clarmart, France.
Mathieu Schmidt, Medical Intensive Care Unit, Hôpital Pitié – Salpêtrière, AP-HP, Paris, France.
Charline Sazio, Medical Intensive Care Unit, Bordeaux University Hospital, Bordeaux, France.
Funding
This study received no funding.
Author information
Authors and Affiliations
Consortia
Contributions
LJ participated in study conception, collected and interpreted the data, and wrote the manuscript. CD participated in study conception and performed statistical analysis. GV participated in data interpretation. PJ and EDM participated in data collection. JFT participated in study supervision and writing of the manuscript. RS participated in data interpretation, writing of the manuscript, and supervised the study. All authors contributed to critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethical committee of the French Society of Intensive Care Medicine (FICS) approved the study and waived the requirement for informed consent.
Consent for publication
Waived.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Patients flow chart. Table S1. Patients’ characteristics, according to the inclusion/exclusion in the study, and according to the testing of reactivity. Table S2. Results of the uni- and multivariable analyses for all patients (n = 214). Table S2bis. Results of the uni- and multivariable analyses for all patients, including clinical data and adjusted for sedation (n = 214). Table S3. Results of the uni- and multivariable analyses for patients under mechanical ventilation (n = 138). Table S3bis. Results of the uni- and multivariable analyses for patients under mechanical ventilation, including clinical data and adjusted for sedation (n = 138). Table S4. Complete case analysis for the whole cohort (n = 194), and among patients under mechanical ventilation (n = 122).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jeantin, L., Dupuis, C., Vellieux, G. et al. Electroencephalography for prognostication of outcome in adults with severe herpes simplex encephalitis. Ann. Intensive Care 13, 10 (2023). https://doi.org/10.1186/s13613-023-01110-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-023-01110-3