Abstract
Introduction
Despite attempts to prevent brain injury during the hyperacute phase of stroke, most sufferers end up with significant neuronal loss and functional deficits. The use of cell-based therapies to recover the injured brain offers new hope. In the current study, we employed human neural stem cells (hNSCs) isolated from subventricular zone (SVZ), and directed their differentiation into GABAergic neurons followed by transplantation to ischemic brain.
Methods
Pre-differentiated GABAergic neurons, undifferentiated SVZ-hNSCs or media alone were stereotaxically transplanted into the rat brain (n=7/group) 7 days after endothelin-1 induced stroke. Neurological outcome was assessed by neurological deficit scores and the cylinder test. Transplanted cell survival, cellular phenotype and maturation were assessed using immunohistochemistry and confocal microscopy.
Results
Behavioral assessments revealed accelerated improvements in motor function 7 days post-transplant in rats treated with pre-differentiated GABAergic cells in comparison to media alone and undifferentiated hNSC treated groups. Histopathology 28 days-post transplant indicated that pre-differentiated cells maintained their GABAergic neuronal phenotype, showed evidence of synaptogenesis and up-regulated expression of both GABA and calcium signaling proteins associated with neurotransmission. Rats treated with pre-differentiated cells also showed increased neurogenic activity within the SVZ at 28 days, suggesting an additional trophic role of these GABAergic cells. In contrast, undifferentiated SVZ-hNSCs predominantly differentiated into GFAP-positive astrocytes and appeared to be incorporated into the glial scar.
Conclusion
Our study is the first to show enhanced exogenous repopulation of a neuronal phenotype after stroke using techniques aimed at GABAergic cell induction prior to delivery that resulted in accelerated and improved functional recovery.
Similar content being viewed by others
Introduction
Stroke is an acute cerebrovascular disorder that remains a major cause of death and disability in the industrialized world [1]. Aside from thrombolysis, which is limited by a narrow therapeutic window, there is no effective therapeutic treatment proven to promote neurological recovery in the postischemic phase [2].
Regenerative events initiated following brain damage are active for weeks following stroke [3, 4], which potentially provides a second window for treatment. Although there are promising treatment strategies that target brain regeneration, including repetitive training, exercise, and physical therapy [5–7], many stroke survivors are often not able to participate in rehabilitation programs until many weeks after a stroke event and delayed rehabilitation results in worse outcomes [8].
Exogenous cell-based therapies to complement endogenous repair mechanisms are currently being trialed in humans following extensive meta-analysis of over 40 studies reporting significant improvements in function after cell transplantation in ischemic animal models [9–11]. Despite early reports of functional benefits in humans [12, 13], a cellular basis for neurological improvement still remains elusive [14]. Whilst neural cell replacement may be achieved, new research shows that neural stem cells (NSCs) can exert trophic effects through secretion of protein factors which induce change in the host tissue to promote functional improvements [15]. In addition to identifying how these cells work, it is equally important to isolate factors that influence stem cell survival and long-term integration within host tissue.
To date, all preclinical and clinical stem cell transplant studies for the treatment of stroke have been conducted using undifferentiated stem cells [10, 16, 17]. Survival of these cells ranges between 0.5 and 30 % [17–23], and although they are capable of forming neuronal populations after transplant in animal models, cells most predominantly differentiate into astrocytes [16, 17, 20]. Functional recovery in these studies has therefore been suggested to be due to trophic support [19, 24], but this effect has not been well characterized or documented.
Recent reports in other models of neurological disease suggest that predifferentiating stem cells into a neuronal phenotype prior to transplant might be a better approach [25–28]. Indeed, differentiated human neural progenitor cell-derived GABAergic neurons injected into the spinal cord following spinal cord injury result in long-term survival of GABAergic cells that generate glutamic acid decarboxylase, gamma-aminobutyric acid (GABA), and β-III tubulin, resulting in functional improvement [26]. We therefore see value in using a similar approach for promoting recovery after stroke. To this end, we have employed human neural stem cells (hNSCs) isolated from the subventricular zone (SVZ) [29] and directed their differentiation into GABAergic neuronal cells. In the present study we investigated the effect of transplanting undifferentiated SVZ-hNSCs versus predifferentiated SVZ-hNSCs into the rat brain 7 days after stroke. We determined the optimal phenotypic conditions that translate into best outcomes in terms of cell survival, histopathology, and functional recovery.
Materials and methods
The following experiments were conducted in adherence with current RIGOR guidelines [30, 31] and included randomization of treatments, blinding during assessment, inclusion of appropriate control groups, and full statistical analysis involving power calculations in consultation with the Statistical Consulting Centre, University of Melbourne, Victoria, Australia.
Ethics statement and animals
All experiments were performed in strict accordance with the guidelines of the National Health & Medical Research Council of Australia Code of Practice for the Care and Use of Animals for Experimental Purposes in Australia. The protocol was approved by the St Vincent’s Hospital animal ethics committee (AEC009/09). Surgeries were performed under general anesthesia and paracetamol (2 mg/kg in drinking water) was provided 24 hours prior to and after surgery to minimize distress. A total of 30 adult male Hooded Wistar rats weighing 300–360 g (Laboratory Animal Services, University of Adelaide, Australia) were used for experiments. Rats were group housed (four rats/cage) prior to stroke, whereupon they were individually housed on a 12-hour light/dark cycle with ad libitum access to food and water.
Surgical preparation
Rats were anesthetized with a mixture of ketamine/xylazine (75 mg/kg:10 mg/kg respectively intraperitoneally) and maintained throughout surgery by inhalation isoflurane (95 % O2 and 5 % isoflurane). A 23-gauge stainless steel guide cannula was stereotaxically implanted into the cortex 2 mm dorsal to the right middle cerebral artery (MCA) (0.2 mm anterior, –5.9 mm lateral, –5.2 mm ventral) as in previous studies [32, 33]. Rats were allowed to recover for 5 days prior to stroke induction.
Endothelin-1-induced stroke
Focal cerebral ischemia was induced in conscious rats (n = 30) by constriction of the right MCA with perivascular administration of endothelin-1 (ET-1, 60 ρmol in 3 μl saline over 10 minutes; American Peptide Company, Inc., CA, USA) [32, 33]. Characteristic behavioral changes indicative of stroke were scored 1–5 for stroke severity according to our previously established protocol, with 5 being the most severe [33]. Rats that did not display behavioral changes were considered not to have suffered a stroke and were excluded from further study. Only rats with an initial stroke severity score of 4, and with clear deficits of ≥3 according to the neurological deficit score at 7 days, were used for stem cell transplants so as to minimize sample variation associated with different stroke outcomes [32, 33].
In vitro cell preparation
hNSC expansion, medium preparation and handling
Experiments were conducted using hNSCs isolated from the SVZ of human fetal brain tissues (14–21 weeks) that were obtained following donor consent under the strict guidelines approved by the Singapore National Healthcare Group Domain Specific Review Board (reference: D/06/154) [29]. The hNSCs were cultured as free-floating neurospheres using protocols described previously.
Prior to transplant, cryopreserved SVZ-hNSCs were thawed, passaged 48 hours later, and expanded as described previously [29]. Briefly, cells were collected and mechanically dissociated by trituration, and approximately 0.7 × 106 cells/well were plated into low-adherence six-well plates (Corning Costar, Sigma-Aldrich, St. Louis, MO, USA). For expansion, cultures were maintained in complete media (Neurocult NS-A hNSC proliferation media and supplement; Stem Cell Technologies Inc., Tullamarine, VIC, Australia), human epidermal growth factor (EGF, 20 ng/ml; Peprotech, Rocky Hill, NJ, USA), human basic fibroblast growth factor (bFGF, 20 ng/ml; Peprotech), heparin (2 μg/ml; Sigma-Aldrich, St. Louis, MO, USA), and 1 % penicillin/streptomycin (Gibco, Thermo Fisher Scientific, Waltham, MA, USA) at 37 °C in a humidified incubator (5 % CO2 atmosphere) for a minimum of 14 days to reach appropriate numbers required for differentiation and transplantation. A 50 % media change was performed every second day. Cell density and viability (≥90 %) was determined using the standard 0.1 % trypan blue exclusion test [29].
In vitro differentiation of hNSCs
For differentiation of SVZ-hNSCs, neurospheres were first dissociated into single-cell suspensions with TryplE, and then cultured in differentiation media consisting of Dulbecco’s modified Eagle’s medium (DMEM)/F12 (Invitrogen, Thermo Fisher Scientific) and neurobasal media (1:1) supplemented with 1 % StemPro neural (Invitrogen), 0.5 % N2 (Gibco), and 50 ng/ml brain-derived neurotrophic factor (BDNF; Peprotech) to induce differentiation as described previously [29]. All cultures were maintained at 37 °C in a humidified culture incubator (5 % CO2 atmosphere) for 7 days, with a 50 % differentiation media change every second day.
In vitro immunocytochemistry
To determine the phenotype of undifferentiated (day 0) cells, SVZ-hNSC neurospheres were seeded onto poly-l-lysine-coated (Sigma-Aldrich, St. Louis, MO, USA) and laminin-coated (Sigma) eight-well chamber slides (Nunc Lab-Tek, Thermo Fisher Scientific) at a density of approximately 200,000 cells/ml. After seeding, for day 0 analysis, neurospheres were allowed to attach for 2 hours at 37 °C under 5 % CO2 before removal of media and fixation with 4 % paraformaldehyde (PFA) in 0.1 M phosphate-buffered saline (PBS) for 15 minutes for immunocytochemical analysis. For analysis of differentiated SVZ-hNSCs (day 7), hNSCs were seeded onto poly-l-lysine-coated (Sigma) and laminin-coated (Sigma) eight-well chamber slides as already described. SVZ-hNSCs were placed in differentiation media as described earlier and after 7 days the cells were fixed with 4 % PFA for 10 minutes at room temperature, washed (1 × 5 minutes in 0.1 M PBS), and processed for immunocytochemistry.
Immunofluorescence was performed on in vitro cell culture chamber slides to analyze phenotypic profiles as described previously [26]. Briefly, cells were blocked with 5 % normal goat serum (NGS) (or 1 % bovine serum albumin [BSA; Sigma-Aldrich, St. Louis, MO, USA] for all staining with goat anti-parvalbumin (PV) antibody) in 0.1 % Triton X-100 in 0.1 M PBS for 20 minutes before SVZ-hNSCs were identified using primary antibodies including mouse anti-human specific nuclear antigen (HuNu, 1:1000; Millipore, Billerica, MA, USA), rabbit anti-neuronal class III β-tubulin (Tuj1, 1:1000; Covance Inc., Sydney, NSW, Australia), rabbit anti-GABA (1:1000; Sigma), rabbit anti-Nestin (1:1000; Millipore), rabbit anti-glial fibrillary acidic protein (GFAP, 1:1000; DAKO, Glostrup, Hovedstaden, Denmark), guinea-pig anti-doublecortin (DCX, 1:500; Millipore), rabbit anti-neuronal nuclear antigen (NeuN, 1:1000; Millipore), rabbit anti-Ki67 (1:500; Thermo Fisher Scientific), rabbit anti-SOX2 (1:400; Millipore), rabbit anti-glutamate decarboxylase 65&67 (GAD, 1:1000; Millipore), rabbit anti-synaptophysin (SYN, 1:200; Sigma), chicken Tuj1 (1:200; Millipore), mouse anti-calbindin-D28k (CB, 1:1000; Swant, Marly, Fribourg, Switzerland), goat anti-PV (1:1000; Swant), and rabbit anti-calretinin (CR, 1:1000; Swant). All primary antibodies were diluted in 5 % NGS in 0.1 M PBS and cells were incubated for 2 hours at room temperature followed by washing in 0.1 M PBS.
Secondary fluorophore-conjugated antibodies (1:500 for all) included Alexa-568 goat anti-mouse, Alexa-488 goat anti-mouse, Alexa-568 goat anti-rabbit, Alexa-488 goat anti-rabbit, Alexa-488 goat anti-guinea pig, Alexa-555 goat anti-chicken, Alexa-647 goat anti-chicken, and Alexa-568 donkey anti-goat (Invitrogen). Antibodies were diluted in 5 % NGS in 0.1 M PBS and cells were incubated for 1 hour followed by washing in 0.1 M PBS.
In all experiments, DNA counterstain 4′,6-diamidino-2-phenylindole (DAPI; Molecular Probes, Thermo Fisher Scientific) was applied before coverslipping with ProLong gold anti-fade reagent (Invitrogen). Control experiments included either omission of each primary antibody from the protocol or the inclusion of the appropriate IgG control to verify the specificity of each antibody. Resulting sections were examined with a Nikon confocal laser scanning microscope (Nikon Instruments Inc., Melville, NY, USA).
Stereology for cultured cells was assessed by manually quantifying immunolabeled cells at a magnification of × 60 using the confocal microscope. Cells in two wells were analyzed for each immunocytochemical stain. Cell counts were performed at six randomly selected sites within each culture well. The total number of cells immunoreactive for Tuj1, GABA, Nestin, GFAP, SOX2, and Ki67 was determined and expressed as a percentage of the total number of HuNu-positive cells.
Preparation of cells for transplantation
SVZ-hNSCs were prepared for transplantation by treating neurospheres with 0.01 % DNase/DMEM for 20 minutes at 37 °C followed by rinsing in 0.01 % DNase/DMEM and centrifugation at 190 × g for 5 minutes, resuspension in 0.01 % DNase/DMEM, and gentle trituration into a single-cell suspension.
SVZ-hNSCs were predifferentiated in preparation for transplantation by culturing neurospheres in the presence of BDNF and neural supplements as described earlier. After 7 days, differentiated SVZ-hNSCs were collected and centrifuged at 190 × g for 5 minutes, and a single-cell suspension was made prior to transplantation.
Undifferentiated SVZ-hNSCs or predifferentiated cell suspensions comprised a final cell concentration of 400,000 cells/μl and ≥90 % viability for transplantation.
Experimental design
Surgical transplantation
Seven days after ET-1-induced stroke, rats were re-anesthetized as already described. A total of 800,000 cells in 2 μl were delivered to each graft site via a Hamilton syringe attached to a glass capillary (open diameter 50–70 μm). The glass capillary was left in place for a further 5 minutes after each dose before retrieval. A total of eight graft sites relative to the bregma were chosen across the striatum and cortex as follows: Site 1, 1.4 mm anterior, –4.9 mm lateral, –3 and –5 mm ventral; Site 2, 1.4 mm anterior, –2.8 mm lateral, –3.6 and –5.6 mm ventral; Site 3, 0.2 mm anterior, –3.8 mm lateral, –4.8 and –5.8 mm ventral; and Site 4, –2.16 mm anterior, –6 mm lateral, –3.3 and –4.3 mm ventral. All rats were immunosuppressed by daily intraperitoneal injections of cyclosporine (10 mg/kg intraperitoneally daily; Sandimmune, Novartis Pharmaceuticals, East Hanover, NJ, USA) commencing 2 days prior to cell transplantation.
Functional assessments
Neurological assessments were conducted on all rats prior to any surgical procedures (pre surgery), immediately prior to ET-1-induced stroke (0 hours post stroke), 24 and 48 hours post stroke, 7 days after stroke (day 0 post transplant), and again 7 and 28 days post transplant. Forelimb asymmetry was analyzed using a cylinder test and the percentage of forelimb placements made on the wall of the plexiglass cylinder during rearing was determined using the methods of Schallert et al. [34]. Animals were also tested for neurological abnormalities and assigned deficit scores based on abnormal posture and hemiplegia as described previously [32, 33, 35, 36]. All scores from each rat post stroke were compared with prestroke scores, and thus each rat acted as its own control.
Tissue processing and analysis
Rats were re-anesthetized 28 days post transplant and transcardially perfused with 300 ml ice-cold PBS (0.1 M, pH 7.4) followed by 300 ml cold 4 % PFA (in PBS, 0.1 M, pH 7.4) for 15 minutes. Forebrains were removed and post-fixed overnight in 4 % PFA in 0.1 M PBS at 4 °C followed by cryoprotection overnight in 0.1 M PBS with 30 % sucrose at 4 °C. Brains were then frozen and coronal sections (40 μm) prepared using a cryostat and processed as free-floating tissue sections.
In vivo immunohistochemistry
Immunofluorescence staining was performed on tissue sections to analyze and quantify graft survival, maturation, and differentiation as described previously [26]. Briefly, free-floating tissue sections were blocked using standard immunohistochemical techniques with 5 % NGS (or 1 % BSA [Sigma] for all staining with goat anti-PV antibody) in 0.3 % Triton X-100 in 0.1 M PBS before SVZ-hNSCs were identified using primary antibodies including mouse anti-HuNu (1:1000; Millipore), rabbit anti-Tuj1 (1:1000; Covance Inc.), rabbit anti-GABA (1:1000; Sigma), rabbit anti-Nestin (1:1000; Millipore), rabbit anti-GFAP (1:1000; DAKO), rabbit anti-NeuN (1:1000; Millipore), rabbit anti-Ki67 (1:500; Thermo Fisher Scientific), rabbit anti-SOX2 (1:400; Millipore), rabbit anti-GAD (1:1000; Millipore), rabbit anti-SYN (1:200; Sigma), chicken anti-Tuj1 (1:200; Millipore), mouse anti-CB (1:1000; Swant), goat anti-PV (1:1000; Swant), rabbit anti-CR (1:1000; Swant), rabbit anti-cleaved caspase-3 (Casp3, 1:500; Cell Signaling Technology, Boston, MA, USA), and rabbit anti-von Willebrand Factor (vWF, 1:200; Millipore).
Secondary fluorophore-conjugated antibodies (1:500 for all) included Alexa-568 goat anti-mouse, Alexa-488 goat anti-mouse, Alexa-350 goat anti-mouse, Alexa-488 goat anti-rabbit, Alexa-647 goat anti-rabbit, Alexa-555 goat anti-chicken, Alexa-647 goat anti-chicken, and Alexa-568 donkey anti-goat (Invitrogen). Antibodies were diluted in blocking solution.
For all experiments, DNA counterstain DAPI (Molecular Probes, Thermo Fisher Scientific ) was applied before coverslipping with ProLong gold anti-fade reagent (Invitrogen). Control studies included either omission of each primary antibody from the protocol or the inclusion of the appropriate IgG control to verify the specificity of each antibody. Staining for terminal transferase-mediated dUTP nick end-labeling (TUNEL) was performed using a TUNEL staining kit (Promega DeadEnd Colorimetric TUNEL system; Promega, Madison, WI, USA) according to the manufacturer’s instructions. Stained sections were examined with a Nikon confocal laser scanning microscope (Nikon Instruments, Melville, NY, USA). Orthogonal projections were performed using National Institute of Health ImageJ software (NIH).
Quantification and stereology
Infarct assessment
Eight predetermined coronal planes throughout the brain from 3.2 to –6.8 mm relative to the bregma [33] were collected for NeuN staining. Triplicate sections from each level were visualized with an Olympus (Albertslund, Denmark) microscope and stroke-damaged regions were identified as areas with distinct absence of NeuN stain, which was analyzed using ImageJ software (NIH, Bethesda, MD, USA) [37–39]. The infarct volume was determined by integrating the cross-sectional area of damage at each stereotaxic level and the distance between the levels [40], with edema corrected for as described previously [33, 41].
Stereological analysis
The optical fractionator stereological method was used to obtain unbiased estimates of the total number of HuNu-positive nuclei within undifferentiated and predifferentiated cell graft sites (n = 7/group) using Stereo Investigator software (MBF Bioscience, Williston, VT, USA) [20, 25, 42]. Briefly, every third section was analyzed using a fluorescence microscope (BH-2; Olympus, Tokyo, Japan) equipped with a QIClick scientific camera (QImaging, Surrey, BC, Canada) at a magnification of × 60, where a three-dimensional optical dissector counting probe (x, y, z dimensions of 30 μm × 30 μm × 10 μm respectively) was applied to a systematic random sample of sites within the cell graft [25]. Only HuNu-positive cells with clearly visible fluorescence were quantified.
Cell phenotyping
The number of HuNu-positive cells that expressed Tuj1, GABA, Nestin, GFAP, and Ki67 was manually counted for phenotypic analysis of cells in vivo within transplant sites. Cells were considered colocalized if labeling of markers was seen throughout the extent of the HuNu-positive nucleus or if a cytoskeletal/cytoplasmic marker surrounded the HuNu-positive nuclear marker. Quantitative analysis was performed in three tissue sections 280 μm apart per graft site (four graft sites/rat) using z-scan confocal microscopy at × 40 magnification for animals that received undifferentiated SVZ-hNSCs or predifferentiated cells (n = 7/group) as described previously [43–47]. Briefly, estimates of the total number of cells colocalizing with markers of interest were obtained using the following formula:
where E is the estimate of the total number of stained cells in each case, ∑N is the sum of n values in the three sections analyzed, and k indicates that every kth section was considered (k = 8). N was corrected according to Abercrombie’s formula:
where n is the number of cells counted in each section, t is the section thickness, and D is the mean diameter of the cells [48]. Colocalized cell counts were expressed as the percentage of the total number of HuNu-positive cells.
Because of the positioning of hNSC grafts, very few sections collected contained the exact same anatomical region within the SVZ for accurate comparisons of host neurogenesis across all rats. For this reason, only a qualitative assessment of the influence of exogenous transplants on host neurogenesis was made.
Statistical analysis
Data obtained in the cylinder test were analyzed by two-way repeated-measures analysis of variance (ANOVA) followed by the Bonferroni post-hoc test to compare differences between treatment groups over time. Data obtained for infarct area and volume assessments were analyzed by two-way ANOVA followed by the Bonferroni post-hoc test. Neurological deficit scores were analyzed by Kruskal–Wallis nonparametric ANOVA followed by Dunn’s post test. We performed a post-hoc power calculation to arrive at 73 % where P <0.01, in which deficits were considered improved by a score of 1 with a standard deviation of 0.87. All cell counts were analyzed by two-way ANOVA followed by the Bonferroni post-hoc test to compare treatment groups and graft sites. Data were analyzed with GraphPad Prism, version 6 (GraphPad Software Inc., San Diego, CA, USA) and presented as mean ± standard error of the mean (SEM). Statistical significance was defined as P <0.05.
Results
In vitro characterization of cells
Confocal analysis of immunolabeled undifferentiated SVZ-hNSCs in vitro revealed formation of neurospheres that were colocalized with HuNu and the undifferentiated cell marker SOX2 (98.9 ± 0.7 %) (Fig. 1a). These cells also colocalized with proliferation marker Ki67 (59.5 ± 3.1 %) and NSC marker Nestin (95.1 ± 0.7 %) (Fig. 1b), but did not express early neuronal marker Tuj1, inhibitory neurotransmitter GABA, GABA-producing enzyme GAD, or immature neuronal marker DCX (Fig. 1c–f). In contrast, predifferentiated SVZ-hNSCs labeled with HuNu were positive for Tuj1 (92.3 ± 1.4 %) (Fig. 1g), GABA (90.1 ± 2.7 %) (Fig. 1h), GAD (Fig. 1i), and DCX (Fig. 1j). Very few predifferentiated cells expressed Ki67 (9.6 ± 2.5 %) (Fig. 1k) or Nestin (28.5 ± 2.6 %, Fig. 1l) and SOX2 (12.1 ± 1.7 %, Fig. 1m). No expression of GFAP, SYN, or the intracellular calcium binding proteins (CBPs) CB, CR, or PV was detected in vitro.
Undifferentiated hNSCs and predifferentiated cell phenotypes in vitro. Immunofluorescent confocal images of undifferentiated SVZ-hNSCs in culture expressed HuNu (red) and SOX2 (green) (a), and Ki67 (red) and Nestin (green) (b), with colocalization giving a yellow appearance. Undifferentiated SVZ-hNSCs immunopositive for HuNu (red) (c–f) in culture were not observed to express Tuj1 (green) (c), GABA (green) (d), GAD (green) e, or DCX (green) f. Predifferentiated cells cultured for 7 days demonstrated immunoreactivity for HuNu (red) g–m and colabeled with Tuj1 (green) (g), GABA (green) (h), GAD (green) (i), and DCX (green) (j). Predifferentiated cells HuNu (red) cultured for 7 days demonstrated little immunoreactivity for Ki67 (green) (k), Nestin (green) (l), or SOX2 (green) (m). Scale bar: (a–f) 100 μm, (g–m) 50 μm. DCX doublecortin, GABA gamma-aminobutyric acid, GAD glutamate decarboxylase 65&67, HuNu human specific nuclear antigen, Tuj1 β-III tubulin
Transplant studies
Treatment groups
A total of 21 rats were included in this study. Seven rats were excluded prior to stem cell transplant based on low stroke severity scores and minimal functional deficits detected at 7 days [32, 33]. Only rats with a stroke rating of 4 and a clear functional deficit of ≥3 were randomly assigned to three experimental groups (n = 7/group): Group 1 received media without any cells (vehicle control); Group 2 received undifferentiated SVZ-hNSC transplants; and Group 3 received predifferentiated cells.
Functional outcomes
Cylinder test
No significant bias in forelimb use upon rearing was detected using the cylinder test prior to stroke induction in any treatment group. After stroke, all rats exhibited asymmetrical limb use indicative of stroke damage with preferential ipsilateral (unimpaired) forelimb use during rearing (Fig. 2a). While transplantation of either undifferentiated SVZ-hNSCs and predifferentiated SVZ-hNSCs appeared to decrease forelimb asymmetry after treatment, this effect was only statistically significant in rats receiving predifferentiated hNSCs at 7 and 28 days post transplant in comparison with vehicle control rats receiving media alone (Fig. 2a) (P <0.05, two-way ANOVA).
Functional outcome following transplantation. Effects of transplantation on contralateral limb use when rearing (a) in the cylinder test after ET-1-induced stroke. Data are mean ± standard error of the mean (SEM) expressed as a percentage of contralateral (impaired) forelimb use. Each rat acted as its own control; results following stroke were compared with 0-hour prestroke scores. ϕP <0.05, ϕϕP <0.01, ϕϕϕϕP <0.0001 relative to 0-hour poststroke baseline scores for vehicle-treated rats (n = 7); **P <0.01, ***P <0.001, ****P <0.0001 compared with 0-hour poststroke baseline scores for undifferentiated treated rats (n = 7); #P <0.05, ##P <0.01 relative to 0-hour poststroke baseline scores for predifferentiated treated rats (n = 7); δP <0.05, δδP <0.01 vehicle-treated rats compared with predifferentiated treated rats; φφP <0.01 vehicle-treated rats compared with undifferentiated treated rats; †P <0.05 predifferentiated treated rats compared with undifferentiated treated rats (two-way ANOVA followed by Bonferroni post test). Combined neurological deficit scores (b). Data presented as box plots include hinges extending from the 25th to 75th percentiles, the median line within the box and whiskers extending to the minimum and maximum values of the dataset (n = 7/group). *P <0.05, ***P <0.001, ****P <0.0001 relative to 0-hour poststroke baseline scores (n = 7/group); #P <0.05, ##P <0.01, ###P <0.001, ####P <0.0001 relative to pretransplant scores (Kruskal–Wallis ANOVA followed by Dunn’s test). Effect of transplanting vehicle, undifferentiated hNSCs, or predifferentiated cells on infarct area (c), (d) and total infarct volume (e) within the cortex and striatum. Data presented as mean ± SEM of infarct area measured at eight predetermined coronal planes through the brain (two-way ANOVA followed by Bonferroni post test)
Neurological deficit score
No neurological deficits were observed prior to ET-1-induced stroke. However, significant deficits were observed in all treatment groups between 24 hours and 7 days after stroke (day 0 post transplant) (P <0.001, nonparametric ANOVA) (Fig. 2b). By 28 days, rats receiving vehicle control or undifferentiated hNSCs showed significant recovery in their deficits when compared with pretransplant scores (P <0.01). Rats that received predifferentiated hNSCs demonstrated earlier recovery with significant improvements observed 7 days post transplant (P <0.001) when compared with pretransplant scores, with no significant deficits detected 28 days post transplant when compared with prestroke scores (P >0.05).
Infarct assessment
Absence of NeuN immunoreactivity revealed stroke-induced damage to the parietal, insular, and frontal cortex, as well as the striatum as reported previously [33]. Both infarct area (Fig. 2c, d) and infarct volume (Fig. 2e) within the cortex and striatum were consistent across treatment groups with no significant differences detected between groups (P >0.05, two-way ANOVA).
Characterization of cells within grafts
Cell counts
HuNu immunostaining revealed large numbers of SVZ-hNSCs within each graft site situated both within and outside the damaged regions 28 days post transplant. Although rats receiving undifferentiated hNSCs displayed evidence of cells within each transplant site, many HuNu-positive NSCs were also detected beyond the transplant regions and were also visible within the infarct border zone. Rats that received predifferentiated SVZ-hNSCs showed dense clustering of cells within each site. Stereological cell counting revealed significantly fewer undifferentiated SVZ-hNSCs within the cortex and striatum (64,712 ± 16,866 cells and 260,278 ± 14,112 cells respectively) compared with predifferentiated HuNu-positive cells in cortical and striatal graft regions (444,852 ± 22,181 and 508,098 ± 10,031 cells respectively) (P <0.0001; Fig. 3a). A greater number of predifferentiated (P <0.05) and undifferentiated (P <0.0001) SVZ-hNSCs remained within striatal grafts compared with cortical graft sites (Fig. 3a). However the overall percentage of transplanted predifferentiated cells remaining within cortical and striatal graft sites (27.8 ± 1.3 % and 31.8 ± 0.5 % respectively) was significantly higher than that of undifferentiated SVZ-hNSCs within the cortex and striatum (4.0 ± 1.0 % and 16.3 ± 0.9 % respectively) (P <0.0001; Fig. 3b).
Transplanted cells survive within the stroke affected brain. Total number (a) and percentage (b) of HuNu-positive cells remaining within cortical and striatal grafts from undifferentiated (n = 7) and predifferentiated (n = 7) treatment groups. Data presented as mean ± SEM. ****P <0.0001 relative to undifferentiated treated animals in the same region; ####P <0.0001 relative to undifferentiated grafts within the cortex; ϕP <0.05 relative to predifferentiated grafts within the striatum (two-way ANOVA followed by Bonferroni post test). Transplanted cells immunopositive for HuNu (red) (c, f) did not express apoptotic markers including Casp3 (green) (d), merged image (e), or TUNEL (g), with the level of TUNEL staining similar to the contralateral mirror image (h). Transplanted HuNu-positive (red) predifferentiated cells were associated with vWF-stained blood vessels (green) within infarcted brain regions (i). Many HuNu-positive undifferentiated hNSCs (red) were found within border regions consisting of GFAP-positive astrocytes (green) (j). Magnified immunofluorescent image (k) corresponds to box highlighted in (j) illustrating incorporation of undifferentiated hNSCs into the glial scar bordering the infarct. Scale bar: (c–e) 20 μm, (f–h) 100 μm, (i, k) 200 μm, (j) 100 μm. C contralateral hemisphere, Casp3 cleaved caspase-3, GFAP glial fibrillary acidic protein, HuNu human specific nuclear antigen, I ipsilateral hemisphere, TUNEL terminal transferase-mediated dUTP nick end-labeling, vWF von Willebrand factor
Survival of transplanted cells within graft sites was confirmed by immunohistochemical analysis for apoptotic marker Casp3 and TUNEL staining. Negligible Casp3 immunostaining (Fig. 3c–e) and TUNEL (Fig. 3f, g) staining was observed within cells 28 days post transplant. The low level of TUNEL staining within the graft was similar to that observed within the contralateral hemisphere (Fig. 3h). Many transplanted undifferentiated SVZ-hNSCs were associated within the glial scar and were GFAP-positive (Fig. 3i, j), whilst transplanted predifferentiated cells were clearly associated with blood vessels within the infarcted regions (Fig. 3k).
Cell phenotypes
Confocal image analysis 28 days post transplant revealed undifferentiated SVZ-hNSCs mainly expressed markers for GFAP and Nestin (Fig. 4a, b), with many cells also positive for Ki67 (Fig. 4c). Some undifferentiated SVZ-hNSCs were also found to express GABA and Tuj1 (Fig. 4d, e). In contrast, predifferentiated cells mainly expressed Tuj1 and GABA (Fig. 4f, g) with little colabeling with Nestin and Ki67 (Fig. 4h, i) and a distinct lack of GFAP expression (Fig. 4j).
Undifferentiated hNSCs and predifferentiated cell phenotypes in vivo. Confocal immunofluorescent photomicrographs of undifferentiated hNSCs at 28 days post transplant within cortical border regions with orthogonal reconstructions. Undifferentiated hNSCs maintained expression of HuNu (red) and colabeled mainly with GFAP (a), Nestin (b), and Ki67 (c), with little expression of GABA (d) and Tuj1 (e) (green). Immunofluorescent confocal images of predifferentiated cells 28 days post transplant within the stroke-damaged cortex maintained expression of HuNu (red) colabeled with Tuj1 (f), GABA (g), Nestin (h), and Ki67 (i) (green), with lack of colocalization with GFAP (green) (j). Orthogonal reconstructions from confocal z-series are presented as viewed in x–z (top) and y–z (right) planes. HuNu immunoreactivity of undifferentiated hNSCs was observed completely surrounded by GFAP and Nestin, while HuNu immunoreactivity of predifferentiated cells was observed completely surrounded by Tuj1 and GABA. Scale bar: (a–e) 50 μm, orthogonal images 5 μm; (f–j) 20 μm, orthogonal images 5 μm. GABA gamma-aminobutyric acid, GFAP glial fibrillary acidic protein, HuNu human specific nuclear antigen, Tuj1 β-III tubulin
Immunofluorescent NeuN staining was used to confirm positioning of graft sites within the infarcted region for stereological analysis across all groups receiving SVZ-hNSC transplants (Fig. 5a–h). Cell counts within each site revealed that there were significantly less cells that expressed Tuj1 (6.6 ± 1.3 %; P <0.0001) and GABA (5.4 ± 1.4 %; P <0.0001) for undifferentiated SVZ-hNSC grafts compared with predifferentiated cell grafts (Tuj1: 89.6 ± 1.9 %; GABA: 94.3 ± 1.6 %) across all transplant sites (Fig. 5i–l, ANOVA). Conversely, there was a significantly greater proportion of undifferentiated SVZ-hNSCs that expressed markers for GFAP (93.0 ± 1.9 %; P <0.0001), Nestin (88.1 ± 2.8 %; P <0.0001), and Ki67 (11.9 ± 1.6 %; P <0.05) compared with transplanted predifferentiated cells (GFAP: 4.7 ± 1.3 %; Nestin: 11.6 ± 3.3 %; Ki67: 4.6 ± 1.1 %) (Fig. 5i–l).
Phenotypic profile of transplanted undifferentiated hNSCs versus predifferentiated cells. Coronal sections immunostained with NeuN (green) highlight undamaged brain regions with lack of staining within stroke affected areas (white dotted line) at cortical graft sites +1.4 mm and –2.16 mm relative to the bregma (a, c) and striatal graft sites +1.4 mm and +0.2 mm relative to the bregma (e, g); white boxes depict graft location. Representative images of graft sites stained with HuNu (red) and NeuN (green) (b, d, f, h) from regions highlighted by white boxes (a, c, e, g). Numbers of HuNu-positive cells coexpressing Tuj1, GABA, Nestin, GFAP, and Ki67 from undifferentiated hNSC-treated (n = 7) and predifferentiated cell-treated (n = 7) animals from cortical graft sites; +1.4 mm (i) and –2.16 mm (j) relative to the bregma; and striatal graft sites +1.4 mm (k) and +0.2 mm (l) relative to the bregma. Numbers of cells are presented as a percentage of the total number of HuNu-positive cells counted. Data are mean ± SEM. ***P <0.001, ****P <0.0001 compared with undifferentiated hNSC counts (two-way ANOVA with Bonferroni post test). Scale bar: (a, c, e, g) 2000 μm, (b, d, f, h) 200 μm. GABA gamma-aminobutyric acid, GFAP glial fibrillary acidic protein, HuNu human specific nuclear antigen, NeuN neuron specific nuclear antigen, Tuj1 β-III tubulin
Further confocal analysis revealed that predifferentiated SVZ-hNSC grafts expressed GAD65/67 (Fig. 6a), as well as the intracellular CBPs CB (Fig. 6b), CR (Fig. 6c), and PV (Fig. 6d). In addition, predifferentiated SVZ-hNSCs were observed to express SYN that was mostly localized to the cell body of cells transplanted into the core infarct region (Fig. 6e), but was also additionally observed along the cytoskeleton of cells that were transplanted into sites outside of the infarct within the peri-infarct territory (Fig. 6f). Predifferentiated SVZ-hNSC grafts located within the peri-infarct territory appeared to extend long neurites revealed by HuNu and Tuj1 immunostaining (Fig. 6g). Grafts located within the core infarct were surrounded by the glial scar consisting of densely packed GFAP-positive astrocytes, with limited dispersion of SVZ-hNSCs in closest proximity to the scar (Fig. 7a–c). Parallel negative control experiments omitting primary antibodies depict a low level of autofluorescence within the core infarct (Fig. d–f).
Further maturation of predifferentiated cells 28 days post transplant. Confocal photomicrographs of predifferentiated cells 28 days post transplant within the stroke-damaged brain expressed HuNu (red) double labeled with either GAD65/67 (green) (a), calbindin-D28k (CB; green) (b), or calretinin (CR, green) (c). Predifferentiated cells expressing HuNu (blue) triple-labeled with parvalbumin (PV, green) and GABA (red) (d), or triple-labeled with Tuj1 (red) and presynaptic vesicle protein synaptophysin (SYN, green) within the cortical core (e) and border (f) regions. Some predifferentiated cells expressing HuNu (red) grafted to border regions appeared to extend long neurites expressing Tuj1 (green) (g). Orthogonal reconstructions from confocal z-series are presented as viewed in x–z (top) and y–z (right) planes. Scale bar: (a, b) 10 μm, orthogonal image 5 μm; (c, d) 40 μm, orthogonal image 5 μm; (e, f) 10 μm, orthogonal image 5 μm; (g) 20 μm, orthogonal image 5 μm. GABA gamma-aminobutyric acid, GAD glutamate decarboxylase 65&67, HuNu human specific nuclear antigen, Tuj1 β-III tubulin
Predifferentiated cells grafted to the core infarct in vivo. Predifferentiated cell graft (HuNu, red) (a) located within the infarcted core region was surrounded by GFAP-positive astrocytes on one side (green) (b) that form the glial scar border (arrow) and merge (c), with dispersion of HuNu-positive cells observed in the core furthest away from the scar (arrowheads). Negative control; omission of primary antibodies (d–f). Scale bar: (a–f) 100 μm. GFAP glial fibrillary acidic protein, HuNu human specific nuclear antigen
Effect of cell transplantation on the neurogenic niche
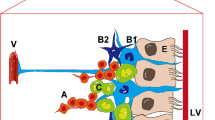
To investigate the effects of SVZ-hNSC transplant on endogenous recovery mechanisms we examined changes within the neurogenic niche in response to stem cell transplant. Confocal analysis revealed an apparent increase in the number of Ki67-positive proliferating cells within the ipsilateral SVZ of rats that received predifferentiated SVZ-hNSCs in comparison with rats that received undifferentiated SVZ-hNSCs or vehicle controls (Fig. 8a–f). In particular, immunofluorescent labeling of cells within the SVZ revealed an apparent increase in the number of newly generated DCX-positive neurons in rats with predifferentiated SVZ-hNSC transplants in comparison with the contralateral SVZ, and rats with undifferentiated hNSC transplants or vehicle controls (Fig. 8b, d, f). Further analysis of immunolabeled cells within the SVZ revealed an apparent increase in the number of GFAP-positive radial glial cells with long processes directed towards the infarct that did not colocalize with Nestin in animals that received predifferentiated SVZ-hNSC transplants compared with the contralateral SVZ, and compared with the other treatment groups (Fig. 8g–l). Furthermore, cells identified within the neurogenic niche of the SVZ were not immunopositive for HuNu, a marker of hNSCs.
Effect of treatment on endogenous neurogenesis and radial glial populations within the SVZ. Immunofluorescent images of proliferating cells (Ki67; red) and migrating immature neuroblasts (DCX; green) within the contralateral and ipsilateral SVZ of vehicle-treated (a, b), undifferentiated hNSC-treated (c, d), and predifferentiated cell-treated (e, f) animals. Nestin (green; arrowheads) and GFAP (red) immunopositive cells (coexpression giving a yellow appearance; arrows) within the contralateral and ipsilateral SVZ of vehicle-treated (g, h), undifferentiated treated (i, j), and predifferentiated treated (k, l) animals. All images were taken at the same anatomical location from animals with similar infarct volumes. Scale bar: (a–f) 500 μm, (g–l) 50 μm. CC corpus callosum, DCX doublecortin, GFAP glial fibrillary acidic protein, LV lateral ventricle, Prediff predifferentiated treated, Stm Striatum, Undiff undifferentiated hNSC treated
Discussion
The use of undifferentiated stem cells for treatment of neurological diseases including stroke have undergone intense investigation in preclinical models [49–51]. Undifferentiated stem cells are thought to provide trophic factor support to injured or “depressed” neural circuitry and respond to host microenvironmental cues by migrating and differentiating into various cell types to influence functional recovery. An alternative approach to cell-based therapies, however, includes predifferentiating hNSCs prior to transplant to improve functional outcomes in animal models of Huntington’s disease, Parkinson’s disease, and neuropathic pain models [25, 26, 28].
Here we report the first evidence in a model of stroke for accelerated improvement in motor function following transplantation of predifferentiated human GABAergic hNSCs compared with undifferentiated hNSCs. We demonstrate that GABAergic neuronal transplants survive within the stroke-affected rat brain, mature, and extend processes with evidence of synaptogenesis and calcium signaling events associated with neurotransmission. Moreover, rats receiving predifferentiated cells showed evidence of increased endogenous neurogenesis, with immature neurons seen extending from the SVZ towards the damaged striatum. In contrast, undifferentiated SVZ-hNSC transplants predominantly differentiated into astrocytes and appeared to contribute to scar formation within the peri-infarct border zone. Our results suggest that differentiation of hNSCs into a neuronal phenotype prior to transplant may be a favorable strategy for in vivo cell restoration and improved motor function after stroke.
In vitro cell phenotyping
In vitro differentiation of SVZ-hNSCs prior to transplantation at day 7 revealed a highly enriched population of GABAergic neurons that expressed Tuj1, GABA, and GAD [29]. The expression of both GAD isoforms (65 and 67) confirmed functional differentiation of these cells with an ability for neurons to produce and release GABA [52, 53] and excluded the possibility of GABA immunoreactivity resulting from in vitro uptake [28]. The decreased expression of markers Nestin, Ki67, and SOX2 with in vitro differentiation was consistent with phenotypic GABAergic conversion. Predifferentiated cell cultures comprised few Ki67-positive cells indicating the majority of cells had undergone differentiation. In contrast, examination of undifferentiated hNSCs revealed a larger population of Nestin, Ki67, and SOX2 immunopositive cells. Furthermore, previous in vitro analysis of predifferentiated hNSCs using our GABAergic predifferentiation protocol has already shown that differentiation does not result in the expression of markers for oligodendrocytes, D2 dopamine receptors, or postsynaptic glutamate receptors. It does, however, result in downregulation of precursor cell associated markers and leads to the majority of hNSCs expressing GABAergic neuronal phenotypic markers [28]. Taken together, differentiation in vitro results in downregulation of stem cell markers and an upregulation of neuronal markers where the majority of predifferentiated cells displayed a GABAergic neuronal phenotype [29].
Effect of cells on functional recovery
Treatment with differentiated GABAergic hNSCs accelerates functional recovery when compared with rats treated with undifferentiated hNSCs. In particular, neurological deficit scores were improved at earlier times after stroke in comparison with undifferentiated hNSC-treated rats. Recovery observed in GABAergic cell-treated rats 28 days post transplant was consistent with prestroke neurological scores. Unlike other treatments, GABAergic cell treatment resulted in statistically improved forelimb asymmetry, comparable with prestroke asymmetry. These results show that differentiation into a GABAergic cell lineage prior to transplant has beneficial effects on recovery for both the cortical and subcortical motor systems.
Transplant survival and migration
Only rats with the same stroke severity scores were included in these experiments, which resulted in little variation detected between infarct volumes across treatments. As such we were able to assess cell responses to the host microenvironment without having to take into account variations in brain injury between groups [32].
Despite the aforementioned findings, a comparison of cell survival 28 days post transplant between treatment groups was difficult due the apparent migration of undifferentiated cells away from the graft site. In our study, only 16 % of undifferentiated hNSCs were detected within striatal grafts and only 4 % within cortical grafts 28 days post transplant. Undifferentiated hNSCs favor less hostile environments and have previously been reported to migrate towards border regions [54, 55], which could account for the low cell numbers detected in the original grafts. For this reason, the peri-infarct territory is currently the target area for transplantation because it is thought to be less hostile and may provide a more supportive extracellular matrix for cell grafts to anchor [22, 37, 56]. In contrast, we now show for the first time that a greater percentage of cells can be retained in the target region if stem cells are predifferentiated. Approximately 30 % of GABAergic cell transplants were still detected in cortical and striatal graft sites even within the severely damaged brain 28 days post transplant. These cells were not in a state of decay since they did not stain positive for apoptotic markers Casp3 or TUNEL stain.
Previous reports suggest that between 0.5 and 15 % of exogenously grafted cells survive in the core infarct and only 20–30 % survive in locations distant to the infarct [18–22]. We now show that cell retention following transplant can be improved through predifferentiation, albeit some cell loss is probably necessary since pruning and refinement of cell numbers to facilitate development of efficient networks is an important process during development [57, 58]. Our findings may support the delivery of fewer cells while still achieving therapeutic outcomes.
The question remains: how do GABAergic cells survive within the severely damaged brain? The answer may relate to trophic factor support provided from blood vessels detected within and surrounding grafts [59–61]. Angiogenesis occurs as early as 3 days after ET-1 stroke [62] and is thought to provide a platform for brain repair. Cells grafted to sites of revascularization after stroke might be expected to do better [62–64]. Current clinical trials favor delaying cell-based treatments until behavioral deficits reach a steady plateau and the microenvironment is less aggressive [11, 65]. Unfortunately, delaying treatment also allows time for newly formed vasculature to regress [66]. Our results suggest that cell-based therapies may benefit from a developed microvascular bed for optimizing survival and influence of exogenous grafts on functional recovery. Timing cell-based therapy within weeks after stroke, when standard therapeutic procedures have been exhausted and relative stabilization of the infarct has occurred, may be a more suitable option for intervention.
Posttransplant histology
Immunohistochemical analysis revealed predominant differentiation of hNSCs into GFAP-positive astrocytes 28 days post transplant in all brain regions targeted. Astrocytes are becoming recognized as a restorative therapeutic target for brain injury, including stroke, because their phenotype can mediate aspects of brain integrity, neuronal cell death, and repair [67]. Astrocyte activation and reactive astrogliosis can result in both beneficial and deleterious responses, and is dependent on the intensity and hostility of the stroke-damaged environment [32, 67, 68]. In the ET-1 stroke model, reactive astrogliosis and glial scarring is established by 14 days [62] and is a major obstacle to brain repair and functional recovery [69, 70]. For this reason we chose not to transplant cells into an established glial scar, but rather targeted transplant prior to scar formation. Nonetheless, hNSCs that were not predifferentiated prior to transplant were found to be localized within the glial scar by 28 days and intensely stained with GFAP, indicating posttransplant differentiation. Undifferentiated hNSCs also displayed a significantly greater proliferative capacity as indicated by Ki67 immunoreactivity compared with predifferentiated cells, confirming their capacity for self-renewal and expansion after transplant. Interestingly, a small subpopulation of undifferentiated hNSCs spontaneously differentiated into Tuj1 and GABA-expressing neurons by 28 days, demonstrating their ability to enter a neuronal lineage despite a greater propensity towards glial cell formation [55, 56].
In contrast to the above, immunohistochemical analysis of predifferentiated GABAergic cell transplants revealed robust expression of Tuj1, GABA, and GAD within the cell bodies, confirming their GABAergic neuronal phenotype 28 days post transplant, even in the severely damaged brain. Predifferentiated cells displayed low levels of proliferative potential, without aberrant transdifferentiation. Furthermore, they did not revert back to an undifferentiated state, suggesting these cells could be a safe source for transplantation. As such, predifferentiating cells into neurons prior to transplant may provide a better treatment option by reducing the risk of contributing to glial scar and tumor formation [71]. Future studies investigating the effects of undifferentiated hNSC or predifferentiated cell transplants on non-neuronal host cells would be of great interest to determine the extent of their influence and thus provide a well-rounded perspective of their potential.
Neuronal repopulation and trophic support for functional recovery
How GABAergic transplants improve the recovering brain is yet to be fully determined. GABAergic neurons are the principal inhibitory cells of the mammalian central nervous system and occur throughout the brain, and GABA regulates the proliferation of neural progenitor cells [72, 73], migration [74], and other aspects of neurogenesis including differentiation [75, 76], neurite formation [77], and synaptogenesis [78]. Possible mechanisms of recovery following stroke injury therefore include neuronal repopulation to bridge the gap between damaged circuits, rescue or reactivation of dormant but surviving circuitry, and trophic influences on endogenous neurogenesis and neuronal reconstruction.
In our study, GABAergic cells transplanted into the striatum resulted in >30 % new neurons expressing immunohistochemical markers that are typically expressed by striatal GABAergic medium-sized spiny projection neurons and aspiny interneurons, being positive for GABA, GAD, Tuj1, and CBPs that are essential components for restoring neurotransmission [79–83]. Whilst grafts to the core infarct were clearly isolated by the glial scar barrier by 28 days, grafts within the border zone appeared to be better positioned to influence host circuitry and promote recovery. Future studies using anterograde and retrograde labeling would be required to substantiate connectivity of graft cells to host neural systems [84].
GABAergic cell transplants also upregulated markers that were absent at the time of transplant, indicating further maturation in vivo to potentially aid recovery. In our study, only predifferentiated cells expressed SYN, a presynaptic vesicle protein, suggesting increased synaptic vesicle formation with potential roles in neurotransmission and plasticity [85–87]. The localization of SYN to the cellular cytoskeleton of grafts within the peri-infarct territory could indicate a more advanced state of maturation compared with grafts within the core infarct. Furthermore, only predifferentiated cells were observed to express the intracellular CBPs CB, CR, and PV, potentially indicating calcium signaling events associated with neurotransmission, transmitter release, and plasticity [88, 89]. Overall, paracrine delivery of GABA, upregulated SYN, and CBP expression may restore neurotransmission and promote plasticity to improve behavioral outcomes.
Another possible outcome of GABAergic transplant is the awakening of depressed pathways known to lie dormant following stroke [90–92], either through restoration of neurotransmission or graft-induced enhancement of neurogenesis to stimulate pathways and influence repair. Trophic and chemoattractive functions exerted by interneurons during development through the release of depolarizing GABA may be recapitulated by GABAergic transplants to promote proliferation/migration of endogenous progenitor cells, provide positional cues to migrating cells including immature neurons, and influence synapse maturation [52, 93, 94]. This is concordant with the human GABAergic transplants in our study potentially being immature and therefore excitatory through release of depolarizing GABA as the switch to an inhibitory phenotype that only occurs late in the first postnatal year in humans [95]. Furthermore, within the ipsilateral SVZ, only predifferentiated cell-treated animals displayed GFAP-positive radial glial cells with long processes known to function in guiding immature neurons during neurogenesis [96]. Although the endogenous neurogenic response purportedly increases 7–14 days post stroke and returns to normal beyond this time [97], the apparent increase in activity within the neurogenic niche in our study 35 days post stroke suggests a trophic influence from transplanted GABAergic cells. In addition, the low neurogenic response observed in vehicle-treated animals 35 days post stroke supports previous reports demonstrating basal neurogenesis levels beyond 2 weeks post stroke in rats [97]. Trophic factors secreted from migrating endogenous progenitor cells and immature neurons, or GABAergic transplants themselves, could therefore act to stimulate rewiring or awakening of host circuits, enabling remaining healthy tissue to restore function of lost connections [92, 98, 99].
Conclusion
Findings from this study demonstrate predifferentiating SVZ-hNSCs prior to transplantation as a novel strategy to accelerate functional recovery after cerebral ischemia. In contrast, undifferentiated hNSC transplants have the potential to delay or hinder functional improvements through contributions to further scar formation. Neuronal repopulation through GABAergic neuronal transplants may achieve greater viability in a clinical setting by targeting a smaller ischemic region, as seen in lacunar strokes [100, 101]. However, GABAergic transplants also show promise for targeting severe stroke through production of GABA, synaptogenesis, and calcium signaling events associated with neurotransmission, to bridge the gap between damaged pathways, enhance plasticity, or rescue depressed circuitry to re-establish function. Alternatively, known trophic effects of depolarizing GABA during development may be recapitulated in our study to enhance endogenous neurogenesis, reactivate circuitry, and promote plasticity for functional recovery in severe strokes with widespread damage. The principles behind differentiation of hNSCs into a desired neuronal cell type may be a favorable alternative for treating stroke.
Abbreviations
- ANOVA:
-
Analysis of variance
- BDNF:
-
Brain-derived neurotrophic factor
- bFGF:
-
Basic fibroblast growth factor
- BSA:
-
Bovine serum albumin
- Casp3:
-
Cleaved caspase-3
- CB:
-
Calbindin-D28k
- CBP:
-
Calcium binding protein
- CR:
-
Calretinin
- DAPI:
-
4′,6-Diamidino-2-phenylindole
- DCX:
-
Doublecortin
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- EGF:
-
Epidermal growth factor
- ET-1:
-
Endothelin-1
- GABA:
-
Gamma-aminobutyric acid
- GAD:
-
Glutamate decarboxylase 65&67
- GFAP:
-
Glial fibrillary acidic protein
- hNSC:
-
Human neural stem cell
- HuNu:
-
Human specific nuclear antigen
- MCA:
-
Middle cerebral artery
- NeuN:
-
Neuron specific nuclear antigen
- NGS:
-
Normal goat serum
- NSC:
-
Neural stem cell
- PBS:
-
Phosphate-buffered saline
- PFA:
-
Paraformaldehyde
- PV:
-
Parvalbumin
- SEM:
-
Standard error of the mean
- SVZ:
-
Subventricular zone
- SYN:
-
Synaptophysin
- Tuj1:
-
β-III Tubulin
- TUNEL:
-
Terminal transferase-mediated dUTP nick end-labeling
- vWF:
-
Von Willebrand factor
References
Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, et al. Heart disease and stroke statistics—2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–e151.
Molina CA. Reperfusion therapies for acute ischemic stroke: current pharmacological and mechanical approaches. Stroke. 2011;42:S16–9.
Zhang RL, Zhang ZG, Chopp M. Ischemic stroke and neurogenesis in the subventricular zone. Neuropharmacology. 2008;55:345–52.
Dancause N, Barbay S, Frost SB, Plautz EJ, Chen D, et al. Extensive cortical rewiring after brain injury. J Neurosci. 2005;25:10167–79.
Nelles G. Cortical reorganization-effects of intensive therapy. Restor Neurol Neurosci. 2004;22:239–44.
Nudo R, Friel K. Cortical plasticity after stroke: implications for rehabilitation. Rev Neurol (Paris). 1998;155:713–7.
Pascual-Leone A, Amedi A, Fregni F, Merabet LB. The plastic human brain cortex. Annu Rev Neurosci. 2005;28:377–401.
Gauthier LV, Taub E, Perkins C, Ortmann M, Mark VW, et al. Remodeling the brain: plastic structural brain changes produced by different motor therapies after stroke. Stroke. 2008;39:1520–5.
Lees JS, Sena ES, Egan KJ, Antonic A, Koblar SA, et al. Stem cell-based therapy for experimental stroke: a systematic review and meta-analysis. Int J Stroke. 2012;7:582–8.
Sahota P, Savitz SI. Investigational therapies for ischemic stroke: neuroprotection and neurorecovery. Neurotherapeutics. 2011;8:434–51.
Kondziolka D, Wechsler L, Goldstein S, Meltzer C, Thulborn KR, et al. Transplantation of cultured human neuronal cells for patients with stroke. Neurology. 2000;55:565–9.
Wechsler LR. Stem cell transplantation for stroke. Cleve Clin J Med. 2004;71:S40.
Bliss T, Guzman R, Daadi M, Steinberg GK. Cell transplantation therapy for stroke. Stroke. 2007;38:817–26.
Stone LL, Grande A, Low WC. Neural repair and neuroprotection with stem cells in ischemic stroke. Brain Sci. 2013;3:599–614.
Acharya MM, Rosi S, Jopson T, Limoli CL. Human neural stem cell transplantation provides long-term restoration of neuronal plasticity in the irradiated hippocampus. Cell Transplant. 2015;24:691–702.
Chen J, Sanberg PR, Li Y, Wang L, Lu M, et al. Intravenous administration of human umbilical cord blood reduces behavioral deficits after stroke in rats. Stroke. 2001;32:2682–8.
Takahashi K, Yasuhara T, Shingo T, Muraoka K, Kameda M, et al. Embryonic neural stem cells transplanted in middle cerebral artery occlusion model of rats demonstrated potent therapeutic effects, compared to adult neural stem cells. Brain Res. 2008;1234:172–82.
Leong WK, Henshall TL, Arthur A, Kremer KL, Lewis MD, et al. Human adult dental pulp stem cells enhance poststroke functional recovery through non-neural replacement mechanisms. Stem Cell Translation Med. 2012;1:177–87.
Smith EJ, Stroemer RP, Gorenkova N, Nakajima M, Crum WR, et al. Implantation site and lesion topology determine efficacy of a human neural stem cell line in a rat model of chronic stroke. Stem Cells. 2012;30:785–96.
Hicks AU, Hewlett K, Windle V, Chernenko G, Ploughman M, et al. Enriched environment enhances transplanted subventricular zone stem cell migration and functional recovery after stroke. Neuroscience. 2007;146:31–40.
Hicks AU, Lappalainen RS, Narkilahti S, Suuronen R, Corbett D, et al. Transplantation of human embryonic stem cell-derived neural precursor cells and enriched environment after cortical stroke in rats: cell survival and functional recovery. Eur J Neurosci. 2009;29:562–74.
Saporta S, Borlongan CV, Sanberg PR. Neural transplantation of human neuroteratocarcinoma (hNT) neurons into ischemic rats. A quantitative dose-response analysis of cell survival and behavioral recovery. Neuroscience. 1999;91:519–25.
Chen J, Li Y, Wang L, Lu M, Zhang X, et al. Therapeutic benefit of intracerebral transplantation of bone marrow stromal cells after cerebral ischemia in rats. J Neurol Sci. 2001;189:49–57.
Chiu AY, Rao MS. Cell-based therapy for neural disorders—anticipating challenges. Neurotherapeutics. 2011;8:744–52.
Mukhida K, Hong M, Miles GB, Phillips T, Baghbaderani BA, et al. A multitarget basal ganglia dopaminergic and GABAergic transplantation strategy enhances behavioural recovery in parkinsonian rats. Brain. 2008;131:2106–26.
Mukhida K, Mendez I, McLeod M, Kobayashi N, Haughn C, et al. Spinal GABAergic transplants attenuate mechanical allodynia in a rat model of neuropathic pain. Stem Cells. 2007;25:2874–85.
Alvarez Dolado M, Broccoli V. GABAergic neuronal precursor grafting: implications in brain regeneration and plasticity. Neural Plast. 2011;2011:384216.
McLeod MC, Kobayashi NR, Sen A, Baghbaderani BA, Sadi D, et al. Transplantation of GABAergic cells derived from bioreactor-expanded human neural precursor cells restores motor and cognitive behavioural deficits in a rodent model of Huntington’s Disease. Cell Transplant. 2012;22:2237–56.
Kobayashi NR, Sui L, Tan PS, Lim EK, Chan J, et al. Modelling disrupted-in-schizophrenia 1 loss of function in human neural progenitor cells: tools for molecular studies of human neurodevelopment and neuropsychiatric disorders. Mol Psychiatry. 2010;15:672–5.
Landis SC, Amara SG, Asadullah K, Austin CP, Blumenstein R, et al. A call for transparent reporting to optimize the predictive value of preclinical research. Nature. 2012;490:187–91.
Lapchak PA. Recommendations and practices to optimize stroke therapy developing effective translational research programs. Stroke. 2013;44:841–3.
Abeysinghe HCS, Bokhari L, Dusting GJ, Roulston CL. Brain remodelling following endothelin-1 induced stroke in conscious rats. PLoS One. 2014;9, e97007.
Roulston CL, Callaway JK, Jarrott B, Woodman OL, Dusting GJ. Using behaviour to predict stroke severity in conscious rats: post-stroke treatment with 3′, 4′-dihydroxyflavonol improves recovery. Eur J Pharmacol. 2008;584:100–10.
Schallert T, Kozlowski DA, Humm JL, Cocke RR. Use-dependent structural events in recovery of function. Adv Neurol. 1997;73:229–38.
Yamamoto M, Tamura A, Kirino T, Shimizu M, Sano K. Behavioral changes after focal cerebral ischemia by left middle cerebral artery occlusion in rats. Brain Res. 1988;452:323–8.
De Ryck M, Van Reempts J, Borgers M, Wauquier A, Janssen PA. Photochemical stroke model: flunarizine prevents sensorimotor deficits after neocortical infarcts in rats. Stroke. 1989;20:1383–90.
Mine Y, Tatarishvili J, Oki K, Monni E, Kokaia Z, et al. Grafted human neural stem cells enhance several steps of endogenous neurogenesis and improve behavioral recovery after middle cerebral artery occlusion in rats. Neurobiol Dis. 2013;52:191–203.
Haelewyn B, Alix P, Maubert E, Abraini JH. NMDA-induced striatal brain damage and time-dependence reliability of thionin staining in rats. J Neurosci Methods. 2008;168:479–82.
Wolf HK, Buslei R, Schmidt-Kastner R, Schmidt-Kastner PK, Pietsch T, et al. NeuN: a useful neuronal marker for diagnostic histopathology. J Histochem Cytochem. 1996;44:1167–71.
Osborne KA, Shigeno T, Balarsky AM, Ford I, McCulloch J, et al. Quantitative assessment of early brain damage in a rat model of focal cerebral ischaemia. J Neurol Neurosurg Psychiatry. 1987;50:402–10.
Leach MJ, Swan JH, Eisenthal D, Dopson M, Nobbs M. BW619C89, a glutamate release inhibitor, protects against focal cerebral ischemic damage. Stroke. 1993;24:1063–7.
West MJ, Slomianka L, Gundersen HJ. Unbiased stereological estimation of the total number of neurons in thesubdivisions of the rat hippocampus using the optical fractionator. Anat Rec. 1991;231:482–97.
Corvino V, Marchese E, Podda MV, Lattanzi W, Giannetti S, et al. The neurogenic effects of exogenous neuropeptide Y: early molecular events and long-lasting effects in the hippocampus of trimethyltin-treated rats. PLoS One. 2014;9:e88294.
Corvino V, Geloso MC, Cavallo V, Guadagni E, Passalacqua R, et al. Enhanced neurogenesis during trimethyltin-induced neurodegeneration in the hippocampus of the adult rat. Brain Res Bull. 2005;65:471–7.
Geloso MC, Giannetti S, Cenciarelli C, Budoni M, Casalbore P, et al. Transplantation of foetal neural stem cells into the rat hippocampus during trimethyltin-induced neurodegeneration. Neurochem Res. 2007;32:2054–61.
Geloso MC, Vinesi P, Michetti F. Parvalbumin-immunoreactive neurons are not affected by trimethyltin-induced neurodegeneration in the rat hippocampus. Exp Neurol. 1996;139:269–77.
Geloso MC, Vinesi P, Michetti F. Calretinin-containing neurons in trimethyltin-induced neurodegeneration in the rat hippocampus: an immunocytochemical study. Exp Neurol. 1997;146:67–73.
Abercrombie M, Johnson ML. Quantitative histology of Wallerian degeneration: I. Nuclear population in rabbit sciatic nerve. J Anat. 1946;80:37–50.
Bjorklund A, Lindvall O. Cell replacement therapies for central nervous system disorders. Nat Neurosci. 2000;3:537–44.
Svendsen CN, Caldwell MA, Shen J, ter Borg MG, Rosser AE, et al. Long-term survival of human central nervous system progenitor cells transplanted into a rat model of Parkinson’s disease. Exp Neurol. 1997;148:135–46.
Martinez-Serrano A, Javier RF, Navarro B, Bueno C, Villa A. Human neural stem and progenitor cells: in vitro and in vivo properties, and potential for gene therapy and cell replacement in the CNS. Curr Gene Ther. 2001;1:279–99.
Le Magueresse C, Monyer H. GABAergic interneurons shape the functional maturation of the cortex. Neuron. 2013;77:388–405.
Soghomonian JJ, Martin DL. Two isoforms of glutamate decarboxylase: why? Trends Pharmacol Sci. 1998;19:500–5.
Okada S, Ishii K, Yamane J, Iwanami A, Ikegami T, et al. In vivo imaging of engrafted neural stem cells: its application in evaluating the optimal timing of transplantation for spinal cord injury. FASEB J. 2005;19:1839–41.
Kelly S, Bliss TM, Shah AK, Sun GH, Ma M, et al. Transplanted human fetal neural stem cells survive, migrate, and differentiate in ischemic rat cerebral cortex. Proc Natl Acad Sci U S A. 2004;101:11839–44.
Roitberg BZ, Mangubat E, Chen EY, Sugaya K, Thulborn KR, et al. Survival and early differentiation of human neural stem cells transplanted in a nonhuman primate model of stroke. J Neurosurg. 2006;105:96–102.
Iglesias J, Eriksson J, Grize F, Tomassini M, Villa AE. Dynamics of pruning in simulated large-scale spiking neural networks. Biosystems. 2005;79:11–20.
Craik FI, Bialystok E. Cognition through the lifespan: mechanisms of change. Trends Cogn Sci. 2006;10:131–8.
Leventhal C, Rafii S, Rafii D, Shahar A, Goldman SA. Endothelial trophic support of neuronal production and recruitment from the adult mammalian subependyma. Mol Cell Neurosci. 1999;13:450–64.
Shen Q, Goderie SK, Jin L, Karanth N, Sun Y, et al. Endothelial cells stimulate self-renewal and expand neurogenesis of neural stem cells. Science. 2004;304:1338–40.
Minger SL, Ekonomou A, Carta EM, Chinoy A, Perry RH, et al. Endogenous neurogenesis in the human brain following cerebral infarction. Regen Med. 2007;2:69–74.
Taylor C, Weston RM, Dusting GJ, Roulston CL. NADPH oxidase and angiogenesis following endothelin-1 induced stroke in rats: role for Nox2 in brain repair. Brain Sci. 2013;3:294–317.
Chopp M, Li Y. Treatment of stroke and intracerebral hemorrhage with cellular and pharmacological restorative therapies. In: Cerebral hemorrhage. Springer; 2008. p. 79–83.
Zhang ZG, Chopp M. Neurorestorative therapies for stroke: underlying mechanisms and translation to the clinic. Lancet Neurol. 2009;8:491–500.
Rabinovich SS, Seledtsov VI, Banul NV, Poveshchenko OV, Senyukov VV, et al. Cell therapy of brain stroke. Bull Exp Biol Med. 2005;139:126–8.
Yu SW, Friedman B, Cheng Q, Lyden PD. Stroke-evoked angiogenesis results in a transient population of microvessels. J Cereb Blood Flow Metab. 2007;27:755–63.
Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta Neuropathol. 2010;119:7–35.
Lau CL, Kovacevic M, Tingleff TS, Forsythe JS, Cate HS, et al. 3D Electrospun scaffolds promote a cytotrophic phenotype of cultured primary astrocytes. J Neurochem. 2014;130:215–26.
McGraw J, Hiebert GW, Steeves JD. Modulating astrogliosis after neurotrauma. J Neurosci Res. 2001;63:109–15.
Abeysinghe H, Bokhari L, Dusting GJ, Roulston CL. Cyclosporine A reduces glial scarring and facilitates functional recovery following transient focal ischemia J Neurol Neurophysiol. 2015; doi:10.4172/2155-9562.1000277.
Amariglio N, Hirshberg A, Scheithauer BW, Cohen Y, Loewenthal R, et al. Donor-derived brain tumor following neural stem cell transplantation in an ataxia telangiectasia patient. PLoS Med. 2009;6:e1000029.
LoTurco JJ, Owens DF, Heath MJ, Davis MB, Kriegstein AR. GABA and glutamate depolarize cortical progenitor cells and inhibit DNA synthesis. Neuron. 1995;15:1287–98.
Haydar TF, Wang F, Schwartz ML, Rakic P. Differential modulation of proliferation in the neocortical ventricular and subventricular zones. J Neurosci. 2000;20:5764–74.
Behar TN, Schaffner AE, Scott CA, O’Connell C, Barker JL. Differential response of cortical plate and ventricular zone cells to GABA as a migration stimulus. J Neurosci. 1998;18:6378–87.
Ganguly K, Schinder AF, Wong ST, Poo M-m. GABA itself promotes the developmental switch of neuronal GABAergic responses from excitation to inhibition. Cell. 2001;105:521–32.
Barbin G, Pollard H, Gaiarsa J, Ben-Ari Y. Involvement of GABA A receptors in the outgrowth of cultured hippocampal neurons. Neurosci Lett. 1993;152:150–4.
Maric D, Liu Q-Y, Maric I, Chaudry S, Chang Y-H, et al. GABA expression dominates neuronal lineage progression in the embryonic rat neocortex and facilitates neurite outgrowth via GABAA autoreceptor/Cl− channels. J Neurosci. 2001;21:2343–60.
Ben-Ari Y. Excitatory actions of GABA during development: the nature of the nurture. Nat Rev Neurosci. 2002;3:728–39.
Bennett B, Bolam J. Characterization of calretinin-immunoreactive structures in the striatum of the rat. Brain Res. 1993;609:137–48.
Cicchetti F, Beach TG, Parent A. Chemical phenotype of calretinin interneurons in the human striatum. Synapse. 1998;30:284–97.
Riedel A, Härtig W, Seeger G, Gärtner U, Brauer K, et al. Principles of rat subcortical forebrain organization: a study using histological techniques and multiple fluorescence labeling. J Chem Neuroanat. 2002;23:75–104.
Gerfen CR. The neostriatal mosaic: multiple levels of compartmental organization in the basal ganglia. Annu Rev Neurosci. 1992;15:285–320.
Gerfen CR, Baimbridge KG, Miller JJ. The neostriatal mosaic: compartmental distribution of calcium-binding protein and parvalbumin in the basal ganglia of the rat and monkey. Proc Natl Acad Sci. 1985;82:8780–4.
Lindvall O, Barker RA, Brustle O, Isacson O, Svendsen CN. Clinical translation of stem cells in neurodegenerative disorders. Cell Stem Cell. 2012;10:151–5.
Ujike H, Takaki M, Kodama M, Kuroda S. Gene expression related to synaptogenesis, neuritogenesis, and MAP kinase in behavioral sensitization to psychostimulants. Ann N Y Acad Sci. 2002;965:55–67.
Weimer RM, Jorgensen EM. Controversies in synaptic vesicle exocytosis. J Cell Sci. 2003;116:3661–6.
Hajjar T, Yong Meng G, Rajion MA, Vidyadaran S, Ai Li T, et al. Alterations in neuronal morphology and synaptophysin expression in the rat brain as a result of changes in dietary n-6: n-3 fatty acid ratios. Lipids Health Dis. 2013;12:113.
Yanez M, Gil-Longo J, Campos-Toimil M. Calcium binding proteins. Adv Exp Med Biol. 2012;740:461–82.
Felmy F, Schneggenburger R. Developmental expression of the Ca2+-binding proteins calretinin and parvalbumin at the calyx of held of rats and mice. Eur J Neurosci. 2004;20:1473–82.
Cramer SC. Repairing the human brain after stroke: I. Mechanisms of spontaneous recovery. Ann Neurol. 2008;63:272–87.
Benowitz LI, Carmichael ST. Promoting axonal rewiring to improve outcome after stroke. Neurobiol Dis. 2010;37:259–66.
Dancause N. Vicarious function of remote cortex following stroke: recent evidence from human and animal studies. Neuroscientist. 2006;12:489–99.
Represa A, Ben-Ari Y. Trophic actions of GABA on neuronal development. Trends Neurosci. 2005;28:278–83.
Lopez-Bendito G, Lujan R, Shigemoto R, Ganter P, Paulsen O, et al. Blockade of GABA(B) receptors alters the tangential migration of cortical neurons. Cereb Cortex. 2003;13:932–42.
Xu G, Broadbelt KG, Haynes RL, Folkerth RD, Borenstein NS, et al. Late development of the GABAergic system in the human cerebral cortex and white matter. J Neuropathol Exp Neurol. 2011;70:841–58.
Gubert F, Zaverucha-do-Valle C, Pimentel-Coelho PM, Mendez-Otero R, Santiago MF. Radial glia-like cells persist in the adult rat brain. Brain Res. 2009;1258:43–52.
Zhang RL, Zhang ZG, Zhang L, Chopp M. Proliferation and differentiation of progenitor cells in the cortex and the subventricular zone in the adult rat after focal cerebral ischemia. Neuroscience. 2001;105:33–41.
Wright LS, Li J, Caldwell MA, Wallace K, Johnson JA, et al. Gene expression in human neural stem cells: effects of leukemia inhibitory factor. J Neurochem. 2003;86:179–95.
Andres RH, Horie N, Slikker W, Keren-Gill H, Zhan K, et al. Human neural stem cells enhance structural plasticity and axonal transport in the ischaemic brain. Brain. 2011;134:1777–89.
Arboix A, Marti-Vilalta JL. Lacunar stroke. Expert Rev Neurother. 2009;9:179–96.
Carmichael ST. Rodent models of focal stroke: size, mechanism, and purpose. NeuroRx. 2005;2:396–409.
Acknowledgements
The authors thank Dr Yiping Fan for assisting in the procurement of primary human brain tissue utilized for this study. The authors would also like to thank Professor Robin McAllen for producing the glass capillaries that were used for conducting stem cell transplant procedures. In addition, the authors would like to acknowledge The O’Brien Institute for the use of their facilities to conduct experimental procedures within the first two years of commencing this study. This research was supported by the National Health and Medical Research Council Australia (NHMRC; project grant #628767) and a NHMRC Principal Research Fellowship to GJD (#1003113). All statistical analyses were conducted in consultation with statistical consultant Rachel Sore of the Statistical Consulting Centre University of Melbourne, Victoria, Australia. The authors would like to dedicate this paper to the late Dr Nao Kobayashi, a remarkable colleague and cherished friend. Nao’s passion and dedication to her scholarship was unparalleled and her friendship and caring spirit will be missed.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CLR was directly involved in the conception and design of the study, provision of study material, assembly of data, data analysis and interpretation, initial drafting and critical review of the manuscript, and financial support. NRK was involved in the conception of the study, maintenance of stem cells, design of the predifferentiation protocol and in vivo transplant procedure, and assembly of data. JMC was involved in the conception of the study, provision of study material, and financial support. GJD was involved in the conception of the study and financial support. MC and JC collectively made substantial contributions to the conception and design of this research project, and were directly responsible for seeking all human ethics approvals, procurement of primary human tissue, maintenance of stem cells, and design of the predifferentiation protocol. Both MC and JC were involved in securing research funding to support the collection and application of stem cells used in this project. AQ made substantial contributions to the conception and design of the in vitro immunocytochemistry experiments, preformed these studies independently, and was involved in the subsequent interpretation of data. LB was involved directly in data collection, assembly, and confocal microscopy analysis and interpretation. HCSA contributed to the design of the in vivo transplant procedure and was directly involved in the acquisition of data, analysis and interpretation of data, and initial drafting and critical review of the manuscript. All authors made substantive intellectual contributions to the study, were involved in the final preparation of the manuscript, and gave final approval of the version to be published. All authors agreed to be accountable for all aspects of the work and ensure, to the best of their abilities, that questions related to the accuracy or integrity of any part of the work have been appropriately investigated and resolved.
Nao R. Kobayashi is deceased
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Abeysinghe, H.C.S., Bokhari, L., Quigley, A. et al. Pre-differentiation of human neural stem cells into GABAergic neurons prior to transplant results in greater repopulation of the damaged brain and accelerates functional recovery after transient ischemic stroke. Stem Cell Res Ther 6, 186 (2015). https://doi.org/10.1186/s13287-015-0175-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-015-0175-1