Abstract
Background
Presacral myelolipomas form a rare disease and are often found incidentally in imaging diagnostics.
Case presentation
In this study, we report the case of a 71-year-old caucasian female with an incidental finding of a retroperitoneal tumor on magnetic resonance imaging scan. This report aimed at presenting the clinical course of this patient with emphasis on analysis of pathological, clinical, and epidemiological features in a meta-analysis of reported cases.
Conclusion
Presacral myelolipomas are rare and its etiology remains unclear. Surgical resection is indicated in symptomatic lesions and lesions > 4 cm. More clinical and pathological research on this rare entity is warranted.
Similar content being viewed by others
Background
Myelolipomas are benign tumors that are composed of mature adipose tissue and elements of extramedullary hematopoiesis with trilinear hematopoietic cells [1] with unknown etiology.
They were first described by Gierke in 1909 [2] and named by Oberling in 1929 [3]. Most commonly, myelolipomas are found as incidentalomas in adrenal glands [4]. Incidence ranges from 1:500 to 1:2500 in autopsy cases [4]. It is assumed that a high number of asymptomatic cases are undetected due to their benign behavior and slow growth [1]. With the widespread use of imaging diagnostics such as computed tomography (CT) and magnetic resonance imaging (MRI), the number of cases describing myelolipoma has increased in recent years [1].
About 15% of myelolipomas are found in extra-adrenal locations [5]. Most of them locate in presacral regions [4], although extra-adrenal myelolipomas have also been found in thorax [6], renal hilum [7], spleen [8], paravertebral regions [9], and the nasal cavity [10].
To date, presacral myelolipomas are described in fewer than 60 cases in English literature published on PubMed and form a rarity. The first patient was described by Blaisdell in 1933, concerning a case of extramedullary hematopoiesis found in a retroperitoneal tumor in an elderly woman [11].
This study aimed to systemically review and meta-analyze clinical, radiological, and epidemiological features of the presacral myelolipoma and present new case of a 71-year-old female with an incidentally detected tumor diagnosed by CT-guided biopsy.
Methods
Search strategy
All studies published until 30 September 2022 on the topic “presacral myelolipoma” was included in the current analysis with no restriction on age or language.
Systematic searches were performed using the term “presacral myelolipoma” on PubMed.
Articles were considered by reviewing title, abstract, and the full text if in doubt.
Selection criteria
Inclusion criteria was a confirmed diagnosis with presacral myelolipoma. Exclusion criteria were reported cases of extra-adrenal myelolipomas that were not located in the presacral region and all research articles on the topic myelolipoma without case presentation.
The PRISMA guidelines were followed.
Data extraction
The following information was extracted from each study: first author, year of publication, title, number of patients with presacral myelolipoma, gender, age, tumor size in diameter, reported symptoms, imaging technology used for diagnosis, and treatment.
All articles were analyzed, and a database was formed. In Table 1, all included articles are listed.
Statistical analysis
Descriptive data are presented as medians and interquartile range for non-normally distributed data, as appropriate. Categorical data are displayed as frequencies and percentages. Continuous data were tested for their normal distribution by Shapiro–Wilk analysis. Mann–Whitney U test was performed for continuous non-normally distributed variables. Categorical variables were compared using the chi-square test.
p < 0.05 was considered to indicate significance. All analyses were performed using SPSS Statistics Software version 28.0 (IBM, Armonk, New York) on macOS 12 Monterey.
Case presentation
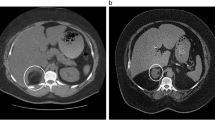
A 71-year-old caucasian female visited our outpatient clinic with an incidentally detected retroperitoneal tumor. An exophytic presacral mass of size 2.6 × 6 × 1.9 cm (Fig. 1) was found on MRI scan, which was performed during a regular gynecological check-up. The tumor located in the soft tissue adjacent to the level of S2. The tumor was clearly demarcated and inhomogeneously configurated, which was isodense to muscle tissue. Furthermore, the tumor showed moderate contrast enhancement and infiltrated both intervertebral foramina of S2.
The patient complained of weight loss of 6 kg in 6 months without fever or diarrhea. On physical examination, no neurological deficit was found. On laboratory workup, an elevated white blood cell count (WBC) of 11.900 was found. Further analysis revealed a normal distribution of white blood cells without abnormal cell proliferation.
A CT-guided biopsy confirmed the diagnosis of a presacral myelolipoma consisting of mature adipose cells with trilineage hematopoietic element. No ectopic adrenal tissues were observed (Fig. 2).
Histological image from the obtained fine-needle biopsy specimens of the presacral myelolipoma (hematoxylin and eosin staining). A Needle biopsy specimens (low magnification) showing monotonous histology consisting of hematopoietic cells and mature fat cells, which are intimately intermingled. No adrenal tissues are observed. B The hematopoietic cells show a normal trilineage from myeloid, erythroid, and megakaryocytic cells (high magnification)
In consent with the patient, a decision towards further follow-up by MRI imaging of the presacral myelolipoma was given, as the patient was asymptomatic when discharged from the clinic.
At 6 months follow-up, there was no evidence of tumor enlargement by MRI imaging and the patient remained asymptomatic. Further radiological reevaluations are scheduled at 6–12-month intervals.
Results
The PubMed database search identified 64 published articles. Through citation search, one more article was identified. Forty-seven publications with 54 reported cases were considered eligible for inclusion. Of the included articles, no longitudinal cohort studies were identified. A small number of included studies described more than one case. Lee et al. described five cases, whereas Grignon et al. and Andriandi et al. described three and two cases, respectively.
The earliest case included in the current analysis was from 1933, while the latest case was from 2021.
Figure 3 shows the PRIMA flow diagram for included articles.
Meta-analysis
The clinical characteristics of the 54 cases searched in literature are depicted in Table 2.
The mean age was 66.4 years (IQR 59.7–74.0 years), ranging from 1.5 to 85 years.
Three cases were found during an autopsy. Women form the majority of reported cases, with a female predominance of 3:1.
The mean size of the presacral tumor was 7.2 cm. More than half of the patients presented with symptoms (34/54, 63%). The most frequent symptom was abdominal pain (n = 12), followed by abdominal discomfort (n = 6) and urological complaints (n = 6). Other symptoms presented were neurological pain in the lower extremities, lower back pain, and bowel obstruction. About half of all cases were incidentally detected (48%).
In most cases, a combination of CT and MRI was used for tumor diagnosis (46%), followed by CT only (30%). Other cases were detected by clinical and ultrasound examinations and dynamic x-ray. The diagnosis was confirmed by a fine-needle biopsy in 28 patients (52%). Thirty patients (56%) received a resection.
There was no significant difference in the size of lesions between symptomatic and asymptomatic patients (p = n.s.). No metastasis or recurrence was reported after an R0 resection.
Discussion
Most presacral myelolipomas, including the one in our new case, occur in elderly female between 50 and 70 years of age [12, 13] with a mean age of 66.4 years.
Imaging features
About half of all reported presacral myelolipomas are found incidentally on CT and MRI in the current study.
Characteristically, the yellowish mature fatty tissue within the myelolipoma appears translucent on abdominal radiographs and echogenic on ultrasound examination [5]. On CT, the fatty elements can be diagnosed by using Hounsfield units, which reveals a low attenuated tissue with −10 to −100 HU [14], while an MRI would present a high-intensity signal in T1-weighted sequence and a corresponding low-intensity signal in fat-suppressed T2 weighted sequences [5].
The hematopoietic elements of myelolipoma interspersed in mature fatty tissue usually have a medium signal intensity similar to that of the spleen on MRI [5]. On T2-weighted images, the marrow-like elements result in areas of increased signal intensity within the inhomogeneous tumor [5].
Due to its superiority in soft-tissue contrast in comparison with CT, MRI represents the modality of choice in the diagnosis of myelolipoma [15]. Thus, the potential invasion of adjacent structures, such as neuroforamina with sacral nerve compression, as described in our case report, can be detected.
In our patient, the presacral myelolipoma has indeed infiltrated neuroforamina in two distinct areas, albeit without causing any symptoms.
Differential diagnosis and treatment recommendations
As a fat-containing soft tissue mass of the retroperitoneum, a spectrum of neoplastic conditions, such as lipoma, liposarcoma, neurogenic tumors, germ cell tumors, teratoma, and metastasis of cancer, must be considered in the differential diagnosis of myelolipoma [14].
In the current case report, Schwannoma was suspected on MRI, based on the finding of infiltration to neuroforamina. A definitive diagnosis can only be determined by fine-needle biopsy with consecutive histological examination or surgical resection. In previous cases, the diagnosis was made either in resection specimens (30 patients, 56%) or by a fine-needle biopsy (28 patients) including our patient.
According to American Association of Clinical Endocrinology (AACE)/American Association of Endocrine Surgeons (AAES) guideline from 2009 for adrenal incidentaloma, small and asymptomatic and hormonally inactive lesions < 4 cm are recommended for radiological reevaluation at 3–6 months and then annually for 1–2 years [16].
The patients may develop a variety of symptoms such as small bowel obstruction [17], urinary retention [18,19,20,21], abdominal pain and discomfort [22,23,24,25,26], and neurological pain [27,28,29,30], through mass effect by tumor enlargement. Tumors > 4 cm should be considered for surgical resection even without suspicion of malignancy [16].
Myelolipomas larger than 6 cm are prone to complications such as spontaneous rupture or rupture due to trivial trauma and hemorrhage with the probability of an acute abdomen [31]. Indeed, half of the patients with presacral myelolipomas, who were initially asymptomatic, later required resection of the tumor (Table 2). The biggest lesion so far reported was approximately 15 cm, described by Massey et al. in 1987, which caused urinary retention and azotemia associated with compression of urinary bladder neck, and the tumor was later completely resected [21].
Due to the rarity of the tumor, there are few comprehensive studies on the detailed clinical features. Han et al. retrospectively assessed a series of 12 patients with 13 myelolipomas in 1997 who received a conservative treatment [32] and followed up by serially conducted CT scans and reported that the tumor enlarged in 6 cases, decreased in 2 cases, and remained unchanged in 5 cases in a mean follow-up time of 3.2 years. Furthermore, most patients remained asymptomatic, and only 2 patients reported new-onset abdominal pain without life-threatening complications [32].
In our analysis, no malignant transformation or metastasis was, except for a rare infiltration secondary by other tumors (chronic lymphocytic leukemia), so far reported [17, 22].
Etiology
The etiology of myelolipoma of the adrenal glands as well as of the presacral counterpart remains unknown. Several hypotheses have been discussed, including metaplasia of reticuloendothelial cells in blood capillaries as a response to an event such as necrosis, infection, or inflammation [32, 33]. However, nonrandom X-chromosome inactivation suggests a clonal origin of the tumor [34].
Conclusion
Presacral myelolipoma is a rare disease with unknown etiology. In this study, we analyzed clinical, radiological features of previously reported 54 cases and reported the case of a 71-year-old woman with an incidentally detected presacral myelolipoma. For asymptomatic tumors, an observation with a regular imaging follow-up can be recommended after histological diagnosis by biopsy. Resection should be considered for bigger lesions > 4 cm and/or for symptomatic patients. Contrast-enhanced MRI and fine-needle biopsy are indicated to determine the definitive diagnosis.
Availability of data and materials
The dataset used in the current study is available from the corresponding author on reasonable request.
Abbreviations
- AACE:
-
American Association of Clinical Endocrinology
- AAES:
-
American Association of Endocrine Surgeons
- CT:
-
Computed tomography
- HU:
-
Hounsfield unit
- MRI:
-
Magnetic resonance imaging
- WBC:
-
White blood cell count
References
Decmann Á, Perge P, Tóth M, Igaz P. Adrenal myelolipoma: a comprehensive review. Endocrine. 2018;59(1):7–15.
Gierke E. Über Knochenmarksgewebe in der Nebenniere. Zieglers Beitr Path Anat 1905:311–25.
Oberling C. Les formations myélolipomateuses. Bull Assoc Fr Etud Cancer. 1929;18:234–46.
Olsson CA, Krane RJ, Klugo RC, Selikowitz SM. Adrenal myelolipoma. Surgery. 1973;73(5):665–70.
Rao P, Kenney PJ, Wagner BJ, Davidson AJ. Imaging and pathologic features of myelolipoma. Radiographics. 1997;17(6):1373–85.
Franiel T, Fleischer B, Raab BW, Füzesi L. Bilateral thoracic extraadrenal myelolipoma. Eur J Cardiothorac Surg. 2004;26(6):1220–2.
Bartumeus Martínez P, Ripollés González T. Mielolipoma extraadrenal retroperitoneal. [Extraadrenal retroperitoneal myelolipoma]. Actas Urol Esp. 2009;33(4):439–42.
Nitz JA, Huckleby J, Hwang EH, Medina MG, Pera SJ, Orcutt ST. Symptomatic extra-adrenal myelolipoma in the spleen. Case Rep Surg. 2020;2020:8839178.
Fonda P, Santiago E de, Guijarro M, Gamallo C. Mediastinal myelolipoma with leukocytosis. BMJ Case Rep. 2013;2013.
George SA, Manipadam MT, Thomas R. Primary myelolipoma presenting as a nasal cavity polyp: a case report and review of the literature. J Med Case Rep. 2012;6:127.
Blaisdell JL. Extramedullary hematopoiesis in a retroperitoneal tumor. Arch Pathol. 1933;16:643–8.
Chen KT, Felix EL, Flam MS. Extraadrenal myelolipoma. Am J Clin Pathol. 1982;78(3):386–9.
Gill KRS, Hasan MK, Menke DM, Wallace MB. Presacral myelolipoma: diagnosis by EUS-FNA and Trucut biopsy. Gastrointest Endosc. 2010;71(4):849.
Shaaban AM, Rezvani M, Tubay M, Elsayes KM, Woodward PJ, Menias CO. Fat-containing retroperitoneal lesions: imaging characteristics, localization, and differential diagnosis. Radiographics. 2016;36(3):710–34.
Kilcoyne RF, Richardson ML, Porter BA, Olson DO, Greenlee TK, Lanzer W. Magnetic resonance imaging of soft tissue masses. Clin Orthop Relat Res. 1988;228:13–9.
Zeiger MA, Thompson GB, Duh Q-Y, et al. The American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons medical guidelines for the management of adrenal incidentalomas. Endocr Pract. 2009;15(Suppl 1):1–20.
Gheith S, Boulay R, Cornfield D. Small lymphocytic lymphoma/chronic lymphocytic leukemia in a pelvic myelolipoma. Int J Clin Exp Pathol. 2009;2(1):95–8.
Orsola A, Raventós C, Trias I, Español I, Orsola I. Urinary retention secondary to presacral myelolipoma; first reported case diagnosed by prostate TUR and requiring a cystectomy. Int Urol Nephrol. 2005;37(4):717–9.
Adetiloye VA, Adejuyigbe O, Adelusola KA. Presacral myelolipoma: sonographic appearance. Pediatr Radiol. 1996;26(4):271–2.
Prahlow JA, Loggie BW, Cappellari JO, Scharling ES, Teot LA, Iskandar SS. Extra-adrenal myelolipoma: report of two cases. South Med J. 1995;88(6):639–43.
Massey GS, Green JB, Marsh WL. Presacral myelolipoma. Cancer. 1987;60(3):403–6.
Arora K, Sidhu J. Extra-adrenal myelolipoma containing small lymphocytic lymphoma/chronic lymphocytic leukemia: a case report and review of the literature. Case Rep Hematol. 2016;2016:7364951.
Chan YF, Yu SJ, Chan YT, Yik YH. Presacral myelolipoma: case report with computed tomographic and angiographic findings. Aust N Z J Surg. 1988;58(5):432–4.
Zanon C, Bortolini M, Bo P, et al. Un caso di mielolipoma presacrale. [A case of presacral myelolipoma]. Minerva Chir. 2000;55(7–8):559–63.
Grignon DJ, Shkrum MJ, Smout MS. Extra-adrenal myelolipoma. Arch Pathol Lab Med. 1989;113(1):52–4.
Hernández-Amate A, Ríos-Martín JJ, Díaz-Delgado M, García-Escudero A, Otal-Salaverri C, González-Cámpora R. Cytological diagnosis of a presacral myelolipoma: a case report diagnosed by fine-needle aspiration. Diagn Cytopathol. 2008;36(12):921–2.
Spizzirri A, Napolitano V, La Mura F, et al. Mielolipoma presacrale: case report. [Presacral myelolipoma: a case report]. G Chir. 2010;31(10):451–5.
Müller M, Schultheiss M, Feuerlein S. Myelolipom versus extramedulläre Hämatopoese–ungewöhnliche Differenzialdiagnose einer präsakralen Raumforderung. [Myelolipoma versus extramedullary hematopoiesis—an unusual differential diagnosis in the presacral region]. RoFo Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2009;181(2):169–70.
Lazarides AL, Scott EJ, Cardona DM, Blazer DG, Brigman BE, Eward WC. Simultaneous primary presacral myelolipomas: case report and review of the literature. J Gastrointest Cancer. 2016;47(3):331–5.
Sagarra Cebolla E, Díaz-Zorita Aguilar B, Del Rodriguez CJ, Ponce Dorrego MD, García Sabrido JL. Giant presacral myelolipoma. Cirugia espanola. 2014;92(9):628–9.
Shenoy VG, Thota A, Shankar R, Desai MG. Adrenal myelolipoma: controversies in its management. Indian J Urol IJU. 2015;31(2):94–101.
Han M, Burnett AL, Fishman EK, Marshall FF. The natural history and treatment of adrenal myelolipoma. J Urol. 1997;157(4):1213–6.
Bokhari MR, Zulfiqar H, Garla VV. StatPearls: Adrenal Myelolipoma. Treasure Island (FL) 2022.
Bishop E, Eble JN, Cheng L, et al. Adrenal myelolipomas show nonrandom X-chromosome inactivation in hematopoietic elements and fat: support for a clonal origin of myelolipomas. Am J Surg Pathol. 2006;30(7):838–43.
Cho J, Kinsey D, Kimchi ET, et al. Retroperitoneal extra-adrenal myelolipoma misdiagnosed as liposarcoma: a case report. Radiol Case Rep. 2021;16(2):364–8.
Andriandi, Cleven AHG, Hanff DF, Hartgrink H, Dijkstra PDS. Presacral myelolipoma, case report and literature review. Ann Med Surg. 2020;57:274–80.
Rizzo G, Coramusi C, Pietricola G, et al. Laparoscopic approach for a presacral myelolipoma resembling a liposarcoma. J Surg Case Rep. 2018;2018(7):rjy156.
Sethi S, Thakur S, Jacques S, Aoun HD, Tranchida P. Myelolipoma of the pelvis: a case report and review of literature. Front Oncol. 2018;8:251.
Sakamoto A, Nagamatsu I, Shiba E, Okamoto T, Hisaoka M, Matsuda S. Presacral myelolipoma as a possible parasymptom of cancer: a case report. Rare Tumors. 2018;10:2036361318772124.
Cho MH, Mandaliya R, Liang J, Patel M. A case report of symptomatic presacral myelolipoma. Medicine. 2018;97(15): e0337.
Oldrini G, Bron G, Renard-Oldrini S, Leroux A, Grignon B, Henrot P. À propos d’un myélolipome présacré. [About a presacral myelolipoma]. Presse Medicale. 2016;45(121):1194–6.
Lee JJ, Dickson BC, Sreeharsha B, Gladdy RA, Thipphavong S. Presacral myelolipoma: diagnosis on imaging with pathologic and clinical correlation. Am J Roentgenol. 2016;207(3):470–81.
Tokuyama N, Takeuchi H, Kuroda I, Aoyagi T. Incidental presacral myelolipoma resembling the liposarcoma: a case report and literature review. Case Rep Urol. 2016;2016:6510930.
Fourati H, Fourati M, Hentati Y, Daoud E, Mnif Z. Presacral myelolipoma: imaging features. Presse Medicale. 2015;44(11):1196–8.
Varone V, Ciancia G, Bracale U, et al. Multidisciplinary diagnostic approach combining fine needle aspiration, core needle biopsy and imaging features of a presacral myelolipoma in a patient with concurrent breast cancer. Pathol Res Pract. 2015;211(3):261–3.
Gagliardo C, Falanga G, Sutera R, et al. Presacral myelolipoma. A case report and literature review. Neuroradiol J. 2014;27(6):764–9.
Leite MI, Gonçalves A, Ferreira AC, Ortiz S, Esteves R, Távora I. An unusual fat-containing presacral tumor in an elderly patient. Case Rep Radiol. 2014;2014: 674365.
Baker KS, Lee D, Huang M, Gould ES. Presacral myelolipoma: a case report and review of imaging findings. J Radiol Case Rep. 2012;6(6):1–9.
Asuquo SE, Nguyen SQ, Scordi-Bello I, Divino CM. Laparoscopic management of presacral myelolipoma. J Soc Laparoendosc Surg. 2011;15(3):406–8.
Dann PH, Krinsky GA, Israel GM. Case 135: presacral myelolipoma. Radiology. 2008;248(1):314–6.
Liu Y-L, Wang M-L, Liu J-Y. Presacral myelolipoma. Taiwan J Obstet Gynecol. 2008;47(2):241–3.
Skorpil M, Tani E, Blomqvist L. Presacral myelolipoma in a patient with rectal cancer: diagnosis by magnetic resonance imaging and aspiration cytology. Acta Radiol. 2007;48(10):1049–51.
Gong Y, Sun X. Fine-needle aspiration of a presacral myelolipoma. Diagn Cytopathol. 2006;34(1):29–30.
Mariappan MR, Fadare O, Ocal IT. Pathologic quiz case: a 74-year-old man with an incidental retroperitoneal tumor found at autopsy presacral myelolipoma. Arch Pathol Lab Med. 2004;128(5):591–2.
Giuliani A, Tocchi A, Caporale A, et al. Presacral myelolipoma in a patient with colon carcinoma. J Exp Clin Cancer Res. 2001;20(3):451–4.
Saboorian MH, Timmerman TG, Ashfaq R, Maiese RL. Fine-needle aspiration of a presacral myelolipoma: a case presentation with flow cytometry and immunohistochemical studies. Diagn Cytopathol. 1999;20(1):47–51.
Gavelli A, Zachar D, Ambrosiani N, Mainguéné C, Huguet C. Myélolipome présacré. [Presacral myelolipoma]. Chirurgie memoires de l’Academie de chirurgie. 1998;123(3):297–9.
Yang GC, Coleman B, Daly JM, Gupta PK. Presacral myelolipoma. Report of a case with fine needle aspiration cytology and immunohistochemical and histochemical studies. Acta Cytol 1992;36 (6):932–6.
Sutker B, Balthazar EJ, Fazzini E. Presacral myelolipoma: CT findings. J Comput Assist Tomogr. 1985;9(6):1128–30.
Fowler MR, Williams RB, Alba JM, Byrd CR. Extra-adrenal myelolipomas compared with extramedullary hematopoietic tumors: a case of presacral myelolipoma. Am J Surg Pathol. 1982;6(4):363–74.
Labow SB, Hoexter B, Susin M. Presacral myelolipoma: report of a case and review of the literature. Dis Colon Rectum. 1977;20(7):606–7.
Benson PA, Janko AB. Pelvic myelolipoma (rare presacral tumor). Am J Obstet Gynecol. 1965;92(6):884–5.
Dodge OG, Evans DM. Haemopoiesis in a presacral fatty tumour (myelolipoma). J Pathol Bacteriol. 1956;72(1):313–7.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
CX conducted meta-analysis concerning reported cases of myelolipomas. HF and AN contributed equally to write the manuscript. AK provided histopathological workup and histological images and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Given the nature of case series of our manuscript, ethics approval is not required. Written informed consent was obtained from the patient to participate in the case report.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests. All authors read and approved the final manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, C., Kasajima, A., Novotny, A. et al. Meta-analysis of reported presacral myelolipomas, including a report of a new case. J Med Case Reports 17, 31 (2023). https://doi.org/10.1186/s13256-022-03746-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03746-4