Abstract
Mediastinal myelolipoma is a rare condition and has no obvious symptoms. In the past 20 years, some clinical cases have been documented. However, the literature has not systematically summarized its imaging features. The aim of this paper is to present a case of right posterior mediastinal myelolipoma and to review and summarize its imaging features. Twenty-six articles were included in our study, which included a total of 26 patients and 33 lesions; 90.9% of the lesions were located in the mediastinum at the level from the 8th thoracic vertebral body to the thoracic 12th vertebral body. Among the cases with unilateral mediastinum, 68.4% of the cases were located in the right posterior mediastinum. Bilateral lesions accounted for almost one-fourth of all lesions. After contrast medium was injected, 93.9% of the lesions had mild to moderate enhancement; 84.8% of the lesions contained fat density; and 75.8%, 69.7%, 87.9%, and 75.8% of the lesions showed clear boundary, regular shape, heterogeneity and were encapsulated, respectively. Only 12.1% of the lesions contained calcification. An inhomogeneous mass in the right posterior mediastinum near the spine, including fat density, is the predominant imaging marker of most mediastinal myelolipomas.
Similar content being viewed by others
Introduction
Although mediastinal myelolipoma is rare, it can occasionally be encountered in clinical work. Myelolipoma is a benign tumor composed of mature adipocytes and hematopoietic tissue, that most often occurs in the adrenal gland but can also occur outside the adrenal gland [1]. The incidence of extra-adrenal myelolipoma has been reported to be very low, with an incidence of 0.08%~0.2% [2]. The uncommon primary sites of myelolipoma include the presacral area, retroperitoneum, liver, spleen, stomach, omentum, pia mater, and mediastinum [3]. With the wide application of imaging examinations, the incidence rate of the disease has increased year by year. To date, most of the reports on mediastinal myelolipoma have been case reports, and there have been no reports in the literature that have summarized its imaging features. Our goal here is to present a case of right posterior mediastinal myelolipoma and to review and summarize its imaging findings.
Case report
The case is a 55-year-old female Han Chinese patient. Three years ago, the patient had no obvious cause; recurrent chest tightness and chest pain, aggravated after activity and relieved after rest; and felt slightly tired, accompanied by dizziness, headache, fatigue, palpitation, epigastric discomfort, acid reflux, and hiccups. Our laboratory results reported: no white blood cell elevation; glycosylated hemoglobin A1c,7.3%(4.1–6.1%); Type B natriuretic peptide precursor, 363.6 pg/ml(0-125pg/ml); creatinine,122.4 umol/l(31–97 umol/l); urea nitrogen, 9.52 mmol/L(2.9-8.2mmol/L); uric acid,551.0 umol/l(140–380 umol/l); endogenous creatinine clearance rate, 30.56 ml/min(70-200 ml/min); triglyceride, 3.14 mmol/l(0.2–1.7 mmol); blood glucose, 16.67 mmol/l(3.9-6.1mmol/l); neutrophil percentage, 77.00%(40–75%); whole course C-reactive protein, 8.42 mg/L(0–4.0 mg/L). There were no abnormalities found during a physical examination. The previous treatment was effective according to “coronary heart disease”, but the condition had returned. The patient had hypertension, type 2 diabetes, and hyperlipidemia but no anemia.
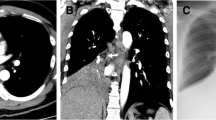
A CT image showed an irregular mass of mixed density on the right side of the 9th-10th thoracic vertebral bodies. The mass had a regular shape, clear boundaries and a capsule, some of which were fat density; and a size of approximately 2.8 × 2.5 cm, slightly enhanced after enhancement (Fig. 1). No pulmonary disease was found, no mediastinal lymph node enlargement was found, and no pleural effusion was found. The doctor first diagnosed schwannoma before surgery.
The video-assisted thoracic surgery (VATS) intraoperative findings showed a 2.5 cm x 2.0 cm tumor in the right posterior lower mediastinum near the 9th-10th thoracic vertebral bodies, with a clear boundary and complete capsule. It was adjacent to the thoracic sympathetic nerve chain, and the blood vessels on the surface of the lesion were dilated. Fish-like organisms were observed after cutting the capsule, with obvious bleeding. The pathological results showed myelolipoma (Figs. 2 and 3).
(A–D) Magnifications of 40x, 100x, 200x, and 400x of myelolipoma under the microscope, respectively(H&E). Microscopic examination showed that the tumor was composed of mature adipose tissue mixed with mature hematopoietic tissue. The white arrow indicates mature hematopoietic tissue. The green arrow indicates adipocytes
After the operation, we rechecked the patient’s chest CT image. We reviewed the patient’s chest CT images one month and four months after surgery. The patient recovered well after the operation, and no tumor recurrence was found in the area of the operation. The following figure shows the chest CT image of the patient, 4 months after surgery (Fig. 4).
Literature review
We searched the literature in PubMed, Web of Science, and the Cochrane Library databases using the subject words myelolipoma and mediastinal. From April 1984 to September 2023, 39 relevant articles were searched, and 26 articles were included according to the integrity of article information and data. For the included cases, the basic information was required to be complete, and the images of the cases had to be described in detail or detailed information could be obtained from the images. For example, cases where the location of the lesion could not be accurately obtained were excluded.
A total of 26 patients and 33 lesions were included in the study. The age ranged from 33 to 79 years (60.8 ± 12.2). There were 6(23.1%) females and 20(76.9) males. The sizes of the lesions were approximately 20–93 mm (44.4 ± 20.5); 30(90.9%) lesions were located at the level of the 8th–12th thoracic vertebral bodies. For cases with unilateral mediastinum, the lesions in 13(68.4%) cases were located in the right posterior mediastinum; the lesions in two(10.5%) cases were located in the left posterior mediastinum; the lesions in two(10.5%) cases were located in the right middle mediastinum; and the lesions in two(10.5%) cases were located in the left and right anterior mediastinum. Lesions were found in the bilateral posterior mediastinum in seven(26.9%) cases;31(93.9%) lesions showed mild to moderate enhancement; 28 (84.8%) lesions contained lipid density ; calcification was found in four(12.1%) lesions; 25 (75.8%) lesions had clear boundaries; the morphology of 23(69.7%) lesions was regular; 29 (87.9%) lesions were heterogeneous; and 25(75.8%) lesions were encapsulated (Table 1).
Discussion
Most myelolipomas have no clinical symptoms. Most of them are accidentally found during physical examination or imaging examination due to other diseases [4]. In addition, in most patients, mediastinal myelolipoma appears around the age of 60, and there has been no significant relationship reported between gender and tumors [5, 6]. Similarly, in our study, the highest incidence rate was approximately 60 years old. However, we found that the incidence rate in males was significantly higher than that of in females. This was inconsistent with previous studies and may have been related to the fewer cases and statistical errors in previous studies.
Mediastinum accounts for approximately 3% of all myelolipomas and is mainly located in the lower right posterior mediastinum [5]. In our study, 68.4% of the cases were located in the right posterior mediastinum. Mediastinal myelolipoma can be single or multiple and located on one or both sides of the posterior mediastinum [7, 8]. In rare cases, it has been located in the anterior mediastinum; however, the study did not mention the image features [9]. In our study, most cases were unilateral lesions and 26.9% of the cases were bilateral lesions.
According to one study, the CT value of the tumor, which included fat and bone marrow tissue, was 20–50 Hu. In the case of the contrast agent, tumor enhancement was not obvious. In addition, calcification in tumors is rare [10]. This is roughly consistent with our study. In our study, fat-like density could be seen in most lesions (84.8%). After contrast enhancement, most lesions (93.9%) had mild to moderate enhancement, and only a few lesions (12.1%) showed calcification. Most lesions were heterogeneous and encapsulated.
There is little information on MRI-related reports of mediastinal myelolipoma. Because tumors contain fat components, most tumors have high signal intensity on T1WI and T2WI [11]. According to the main content of the mass, MRI may show equal intensity or slightly higher intensity in T1- and T2-weighted images [6]. One researcher mentioned that the MRI signal of mediastinal myelolipoma could be divided into three types according to the tumor components: fat signal, adult cortex signal, and signal between fat and liver [12].
CT is a common diagnostic method for mediastinal myelolipoma. CT and MRI can effectively diagnose adrenal myelolipoma, but they cannot diagnose mediastinal myelolipoma [13]. Even if the disease cannot be accurately diagnosed, it can be judged whether the disease is benign or malignant by using imaging [11]. Different tumors can be distinguished by their occurrence in distinct locations and the different tissue components present within a tumor. In particular, mediastinal myelolipoma needs to be differentiated from teratoma, neurofibroma, schwannoma, malignant nonseminomatous germ cell tumors, thymolipoma, angiolipoma, and epidural lipomatosis [14].
Adrenal myelolipoma is relatively common. It often occurs unilaterally, with a small volume, clear boundary, circular homogeneous mass, and often contains fat [15, 16]. It is notable that the amount of fat is much less in mediastinal myelipoma than in adrenal myelipoma.
When a paraspinal posterior mediastinal mass is found, especially if the mass is located in the right posterior mediastinum, in addition to the clear boundary and regular shape of the benign tumor signs, if the mass contains fat density, the possibility of myelolipoma should be considered first. Except for special situation such as extremely large masses, internal bleeding, and compression symptoms, radiologists should recommend follow-up rather than biopsy or surgery [17, 18].
General laboratory tests for myelolipoma show no abnormalities, and CT and MRI are the most important preoperative diagnostic methods; CT is more commonly used than MRI. In this study, some radiographic signs were characteristic, with the main radiographic sign being a heterogeneous mass in the right posterior mediastinum near the spine, including fat density. When the imaging features of the lesions are not typical, they mainly need to be differentiated from neurogenic tumors, extramedullary hematopoiesis, lymphadenopathy, and pleural mesothelioma.
Data availability
These data and materials are available from corresponding authors for rational reasons.
References
Nakagawa M, et al. Bilateral video-assisted thoracoscopic surgery resection for multiple mediastinal myelolipoma: report of a case. Korean J Thorac Cardiovasc Surg. 2014;47(2):189–92.
Kim K, et al. Primary myelolipoma of mediastinum. J Comput Tomogr. 1984;8(2):119–23.
Xiong Y, Wang Y, Lin Y. Primary myelolipoma in posterior mediastinum. J Thorac Dis. 2014;6(9):E181–7.
Mohan K, Gosney JR, Holemans JA. Symptomatic Mediastinal Myelolipoma Respiration. 2006;73(4):552.
Alsayegh HA, et al. A case of bilateral posterior mediastinal myelolipoma. Radiol Case Rep. 2022;17(3):656–61.
Yao WQ, et al. Mediastinal myelolipoma/extramedullary hematopoiesis presenting as a mass: rare differential diagnosis among mediastinal tumors. Int J Clin Exp Pathol. 2018;11(5):2714–20.
Pulsoni A, et al. Mediastinal extramedullary hematopoiesis as first manifestation of hereditary spherocytosis. Ann Hematol. 1992;65(4):196–8.
Goel I, Kaushik P, Anand R. Bilateral posterior Mediastinal Primary Myelolipoma. Ann Thorac Surg. 2018;106(5):e235–7.
AlSaffar AH, et al. Anterior Mediastinal Myelolipoma: a Case Report and Review of the literature. Am J Case Rep. 2022;23:e936005.
Shi Q, et al. Primary mediastinal myelolipoma: a case report and literature review. J Thorac Dis. 2017;9(3):E219–25.
Cao J, et al. Surgical management and outcome of extra-adrenal myelolipomas at unusual locations: a report of 11 cases in a single center. J Bone Oncol. 2022;35:100438.
Kawanami S, et al. Mediastinal myelolipoma: CT and MRI appearances. Eur Radiol. 2000;10(4):691–3.
Hosaka T, et al. Mediastinal myelolipoma showing gradual enlargement over 9 years: a case report. J Cardiothorac Surg. 2016;11(1):91.
Migliore M, et al. An unsual symptomatic case of mediastinal myelolipoma treated by VATS approach. Ann Ital Chir. 2014;85(1):85–7.
Lattin GE Jr., et al. From the radiologic pathology archives: adrenal tumors and tumor-like conditions in the adult: radiologic-pathologic correlation. Radiographics. 2014;34(3):805–29.
Bracci B, De Santis D. Adrenal Lesions: A Review of Imaging. 2022;12(9).
Albano D, et al. Imaging features of adrenal masses. Insights Imaging. 2019;10(1):1.
Zeiger MA, et al. American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons Medical Guidelines for the management of adrenal incidentalomas: executive summary of recommendations. Endocr Pract. 2009;15(5):450–3.
Funding
Ziyang medical science project, KY2023067.
Author information
Authors and Affiliations
Contributions
Conceptualization: Y.S.F., X.W., L.X. made substantial contributions to the conception, design, acquisition/analysis of data and writing of the manuscript. L.X. and X.W. revised the manuscript and provided general supervision. L.X. acquired data. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Ziyang People’s Hospital. The patient included in this research agreed to participate in this study.
Consent for publication
We obtained written informed consent from the patient for the publication of this article. The individual person’s data contained in the manuscript have obtained consent for publication by patients.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, L., Wen, X. & Feng, S.Y. A case of posterior mediastinal myelolipoma and a literature review of its imaging manifestations. J Cardiothorac Surg 19, 458 (2024). https://doi.org/10.1186/s13019-024-02829-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02829-1