Abstract
At the European Society of Radiology (ESR), we strive to provide evidence for radiological practices that improve patient outcomes and have a societal impact. Successful translation of radiological research into clinical practice requires multiple factors including tailored methodology, a multidisciplinary approach aiming beyond technical validation, and a focus on unmet clinical needs. Low levels of evidence are a threat to radiology, resulting in low visibility and credibility. Here, we provide the background and rationale for the thematic series Translating radiological research into practice—from discovery to clinical impact, inviting authors to describe their processes of achieving clinically impactful radiological research. We describe the challenges unique to radiological research. Additionally, a survey was sent to non-radiological clinical societies. The majority of respondents (6/11) were in the field of gastrointestinal/abdominal medicine. The implementation of CT/MRI techniques for disease characterisation, detection and staging of cancer, and treatment planning and radiological interventions were mentioned as the most important radiological developments in the past years. The perception was that patients are substantially unaware of the impact of these developments. Unmet clinical needs were mostly early diagnosis and staging of cancer, microstructural/functional assessment of tissues and organs, and implant assessment. All but one respondent considered radiology important for research in their discipline, but five indicated that radiology is currently not involved in their research. Radiology research holds the potential for being transformative to medical practice. It is our responsibility to take the lead in studies including radiology and strive towards the highest levels of evidence.
Critical relevance statement For radiological research to make a clinical and societal impact, radiologists should take the lead in radiological studies, go beyond the assessment of technical feasibility and diagnostic accuracy, and—in a multidisciplinary approach—address clinical unmet needs.
Key points
• Multiple factors are essential for radiological research to make a clinical and societal impact.
• Radiological research needs to go beyond diagnostic accuracy and address unmet clinical needs.
• Radiologists should take the lead in radiological studies with a multidisciplinary approach.
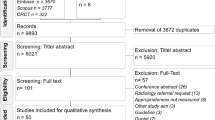
Graphical Abstract

Similar content being viewed by others
Introduction and rationale
Clinical research seeks to provide scientific evidence for diagnostic and therapeutic practices with the aim of improving patient outcomes and having a beneficial societal impact [1]. In their 2010 article on evidence-based medicine (EBM) for radiology, Sardanelli et al. reported the previously introduced hierarchy of studies on diagnostic tests, ranging from level 1 (technical performance) to level 6 (societal impact) [2, 3]. The authors were hopeful that radiological research, which was relatively slow in its uptake of EBM, would catch up. At the time, it was estimated that less than 10% of standard radiological procedures were supported by high-level evidence [4]. Indeed, over a decade later, many impactful radiological studies have now been published that truly changed clinical practice, including the management of suspected prostate cancer [5], treatment of stroke [6], and screening for breast cancer [7, 8] to name a few. What many of these highly impactful studies have in common is that they are the result of a fruitful collaboration of the various disciplines involved in the diagnosis and treatment of these particular diseases.
At the same time, a high rate of radiological research studies continues to focus on technical or diagnostic performance only, often using a retrospective study design including selected cohorts, without following on with the prospective validation [9, 10]. The assessment of technical and diagnostic performance should not be trivialised, as these are crucial first steps in assessing radiological performance and our focus on these is inherent to the technical nature of our profession [2]. Importantly, the safety of radiological procedures also needs to be assessed, as an initial step with technical performance (e.g. for CE marking) and thereafter as part of post-market surveillance. But the story does not end with technical and diagnostic performance. A clear distinction should be made between diagnostic benefit and benefit to the (individual) patient and eventually also to society, whether this is a change in management, outcome, and/or costs [3]. It is not a given that better technical or diagnostic performance actually changes patient management or outcome or has any impact on the societal level [11]. Also, prospective validation of the results of these studies is mandatory to fully evaluate the impact of the research on real-world practice, acknowledging that such work is highly challenging due to the costs and time required. As these domains are typically outside the general scope of diagnostic radiology, they receive (too) little attention in the radiological community.
The frequent lack of assessment of therapeutic and outcome impact by radiological studies not only hampers the penetration of new radiological developments into clinical practice and particularly into guidelines, but also impedes our strength, visibility, and impact as radiologists in the daily care of patients. An important indicator of this is the finding that out of 867 systematic reviews on diagnostic and interventional imaging between 2001 and 2010, only 330 (38%) were published by an imaging specialist as the first or last author. In other words, a large majority of systematic reviews on our specialty were led by non-imaging specialists [12]. What is more, the quality of those reviews not including imaging specialists among the authors was significantly lower than that of those including them [12]. This means that lower-quality systematic review publications dominated, which is detrimental to our credibility and impedes the introduction of advanced imaging techniques into clinical routine. In the recent NICE guideline on brain tumour management, for instance, all studies on perfusion MRI were considered low or very low-quality evidence [13]. Recommendations could therefore only be based on the committee’s clinical experience rather than scientific evidence, reducing their potential clinical impact.
There are multiple initiatives to assess and improve the quality of radiological research. Reporting guidelines such as STARD [14] or TRIPOD [15] specifically address diagnostic studies. But for radiological research to make a clinical impact, we also need to go beyond the assessment of technical and diagnostic performance, and address clinical unmet needs, connecting with referring/treating physicians to ensure their support and uptake into a clinical setting. In other words, our focus should not only be on the image, but on the full clinical setting, patient outcome, and eventually on society as a whole. The European Institute for Biomedical Imaging Research (EIBIR) established the European Network for the Assessment of Imaging in Medicine (EuroAIM) to systematically assess radiological technology and seek evidence for its best use in clinical practice. A number of EuroAIM initiatives were dedicated to critical appraisal of the quality of imaging guidelines using the AGREE II tool (see for example [16, 17]). Its application provides insight into the unmet radiological needs in clinical guidelines, for example, showing limitations in the “applicability” domain. It is imperative that we, as radiologists, truly take the lead in addressing these unmet needs by initiating and performing high-quality studies and ensuring their clinical implementation. More broadly, studies led by radiologists as principal investigators should approach difficult questions with original hypotheses and novel technologies, starting from fundamental questions in the field. This is not always self-evident from the commonly supportive role we have in a clinical setting, but even for aspects such as patient inclusion, we as radiologists can and should consider ourselves responsible to truly take the lead in such studies.
Objective
The objective of this article is to provide the background and rationale for the thematic series on Translating radiological research into practice—from discovery to clinical impact, which invites authors to describe the process of achieving clinically impactful radiological research as guidance and inspiration to the radiological research community. We will define impact and describe the specific challenges for relevant radiological research and those aspects that make diagnostic research unique in comparison to other clinical research. We will, furthermore, explain the various methodological aspects that result in impactful radiological research, specifically aiming to go beyond diagnostic accuracy. We will also highlight the importance of multidisciplinary research and provide examples of currently unmet clinical needs which provide potential areas of research where high impact could be achieved.
What is impact?
Each intervention undertaken in a patient’s care pathway will have an impact, which may be positive or negative, intended or unintended [18]. The impact of a radiological ‘intervention’ may be straightforward, such as influencing the start of treatment, for example, following the diagnosis of a pulmonary embolism, detection of osteoporosis, or screening for cancer. Impact evaluations may include a wide range of events, such as diagnosis, definition of or change in treatment plan, and selection of patients for trials. However, the impact of an imaging investigation may be difficult to tease out when considering complex scenarios affecting patient outcomes, due to multifactorial interacting events such as the patient’s performance status and differing treatment regimes.
Certainly, the exponential increase in requests for imaging investigations to guide treatment planning decisions is a form of evidence of the positive impact of imaging on patient pathways. Imaging investigations that are widely implemented into clinical practice are clearly valued by referring physicians for treatment planning. However, in order to measure impact more directly, it is necessary to formulate a clear question that will allow effective impact evaluation. For example, ‘what is the impact of MRI on patient selection for prostate biopsy?’. In this example, several kinds of impact may be considered, such as the following:
-
Did MRI increase the proportion of positive biopsies of significant tumours compared to ultrasound (US) alone?
-
Did MRI reduce the proportion of biopsies of non-significant tumours or abnormalities compared to US alone?
These questions allow measurable impact evaluation of the intervention. A clear positive impact of the imaging investigation has resulted in widespread change in clinical practice and adoption of the investigation into clinical guidelines. In addition, impact can be measured by the cost savings based on the reduction of the number of negative biopsies.
Clinical impact of radiological imaging may also be evaluated by patient preference, for example, in the case of MRI guiding fertility-preserving surgery in gynaecological cancer. In this case, the outcomes can be measured for both fertility events and cancer events. Patient preferences and the impact of imaging investigations on quality of life need to be addressed. Imaging findings can furthermore impact patient selection for clinical trials, where image-based eligibility criteria are used (e.g. presence of tumour above a certain size) and for stratification of patients into different study arms (for example, patients with or without metastatic disease on imaging). Large-scale imaging studies in non-patient populations can have an impact through providing insight into disease aetiology and risk factors such as stroke [19] or dementia [20].
Imaging to screen for relevant diseases may have a much wider societal impact, with a clear benefit to patient survival rates as in breast cancer-screened populations [21]. However, it is important to conduct appropriate large-scale screening trials; as the cost of population screening is high, there may be negative impacts on patient quality of life, and the impact on patient survival may not be present, as demonstrated in the UKCTOCs study in ovarian cancer screening [22].
Techniques to measure the value of imaging investigations, including health technology assessment, are even more important at this time of implementation of artificial intelligence (AI) in radiology [23]. The value of imaging in the patient experience is also an essential aspect of measuring our impact on value-based care [24, 25].
Importance of a multidisciplinary approach
Science and medicine are complex. No simple solution exists to understand the fundamentals of the biological processes and the use of current and future targeted treatments. To improve results, researchers also have to properly define the clinical pathway and outcomes to address, connect relevant technical and clinical aspects, access data repositories, understand other members’ skills, guarantee enough time to the research project, follow accepted checklists and guidelines, search for evidence-based knowledge, and develop common research skills. A multidisciplinary approach is mandatory not only between different specialties within medicine, but also with other disciplines such as data scientists, physicists, or computational engineers. Particularly in this era of precision medicine, where big data and AI are key to building robust predictive models integrating imaging and non-imaging data, a multidisciplinary approach is key also at the level of data collection. While there are multiple efforts to store and publicise such diverse datasets in the form of biobanks, only a minority have dedicated functionality for imaging data [26]. As an important effort to help imaging researchers to share or use imaging data, the ESR and EIBIR have set up an imaging biobank catalogue with descriptions of imaging biobanks and image collections in order to advertise them towards the research community (https://molgenis.eibir-edc.org/menu/main/app-molgenis-app-biobank-explorer#/).
Involving treating physicians is essential for the implementation and uptake of radiological advances in new guidelines. All relevant papers do have to finally address clinically relevant questions and unmet needs to improve how patients are diagnosed and treated. Even if the focus of a research work is technical, the foreseen clinical improvements must be highlighted, which can only be achieved by involving all relevant disciplines, each with their specific expertise. In a comparative study of various handbooks of guideline development, a multidisciplinary panel was considered a key aspect for issuing guidelines [27], to ensure input from all relevant stakeholders and timely identification of concerns with implementation [28]. It should be noted that developing guidelines (following the proper GRADE II methodology) requires a substantial time (1 year, minimum) and financial investment. Online meeting tools, however, have greatly facilitated cross-institutional/national and multidisciplinary collaboration and the ESR’s and subspecialty societies’ networks could provide an ideal starting point for such initiatives.
Unmet clinical needs
To assess the impact of radiological developments and the currently unmet imaging needs, a survey was sent to 23 non-radiological clinical societies and associations with whom the ESR has a memorandum of understanding or had any other formal contact in past years. The survey consisted of 5 open-answer questions (Table 1). Twelve responses were received from 11 societies (1 society provided 2 responses). The majority of respondents (6/11) were in the field of gastrointestinal/abdominal medicine; others were in the field of musculoskeletal (3/11), oncological (1/11), and diabetes (1/11) care. The implementation of CT or MRI techniques for disease characterisation, detection and staging of cancer, and surgical planning, together with radiological interventions were mentioned as the most important radiological developments in the past years (Table 2). The perception was that patients were not always aware of the impact of these developments, and when they were, the awareness was mostly modest (Table 2). Unmet clinical needs were mostly in the context of staging for various forms of (gastrointestinal) cancer, early and differential diagnosis, microstructural and/or functional assessment of tissues and organs, and the visualisation of implants (Table 3). All respondents but 1 considered radiology (very) important for clinical research and their discipline, but 5 indicated radiology was currently not involved in their clinical research (3 in gastrointestinal/abdominal medicine, 1 in diabetes care, and 1 in musculoskeletal disease).
Practical and methodological challenges and recommendations
There are several well-recognised challenges for radiologists trying to conduct imaging research as chief or principal investigators, rather than being in a supportive role, as is commonly the case in clinical trials with imaging used for measurement of treatment effect. Understanding these challenges may help to develop strategies to successfully undertake radiology-led research.
-
1.
Eligible patients may attend outpatient clinics led by referring clinicians who may not suggest taking part in an imaging study, leading to difficulties with recruitment, with patients slipping through. In addition, informed consent can be challenging if the research coordinator or referring clinician does not fully understand the suggested imaging intervention. Radiologists may not have sufficient flexibility to be present in the clinics to recruit and consent patients, especially when only few patients may be eligible per clinic. It becomes essential to employ a research coordinator to attend clinics for patient identification.
-
2.
The treating physician may not be fully supportive of imaging research, thus being an obstacle to present the study to the patient in a positive way to ensure recruitment. There may be competing studies led by treating physicians or indeed they may wish to lead the radiological research themselves, leading to a turf battle.
-
3.
There may not be sufficient flexibility on scanners to readily fit research examinations into a busy clinical schedule. If a research sequence is being added to a standard-of-care scan, there may not be sufficient flexibility in booking slots to allow for ad hoc extension to scan times.
-
4.
Even when setting up a prospective, quality-assured imaging protocol, there can be difficulties in ensuring uniformity of scan acquisition across multiple scanners, multiple sites, or multiple operators. Site training and quality assurance are essential but can be difficult, with so many radiographers involved in scanning patients over several years in multicentre prospective studies [29]. This may lead to difficulties with reproducibility and data variability across a study, negatively impacting the power of the study.
-
5.
Traditional study methodologies are not necessarily well-suited for conducting medical imaging research. A lack of awareness of methodological considerations regarding radiological research carries the risk of inappropriate study design by researchers on the one hand or—unjustified—rejection by reviewers in case a non-traditional yet appropriate method is applied.
Several methodological issues and challenges are specific and sometimes unique to radiological research. One first issue is the only indirect relationship between radiological imaging and treatment, with the obvious exception of interventional radiology. This means that between our diagnoses and patient outcomes, there is a large spectrum of options for confounding interventions and events, for instance, in oncology medical therapy, surgery, radiation therapy (and combinations thereof) and the personal biological status, including genetic and epigenetic factors. Thus, to measure the outcome effect of radiological imaging is the first big methodological challenge.
Well related to this point is the lack of awareness regarding the type of evidence needed for recommending radiological diagnostic procedures in multidisciplinary guidelines. The widely endorsed GRADE system for evaluating the quality of scientific evidence and strength of guideline recommendations [30] requires randomised controlled trials (RCTs) for obtaining the highest levels of evidence, while in fact, RCTs are not always needed [31]. According to EBM, physicians should choose the test showing the best compromise between sensitivity and specificity in the particular clinical scenario, e.g., for patients presenting with symptoms or signs of a disease high sensitivity may be desired to determine a treatable cause (e.g., identifying intracranial vessel occlusion in a patient with neurological symptoms); for staging of an already diagnosed disease, high specificity may be needed to avoid withholding treatment by inadvertent over-staging (e.g. excluding brain metastasis prior to start of systemic treatment) [32]. Sometimes, the entire story is forgotten: RCTs are a surrogate of intraindividual trials that are not possible for comparing different therapies. In fact, when intra-individual trials are possible, e.g. for ophthalmological disease (therapy 1 for the right eye, therapy 2 for the left eye) or dermatological disease (therapy 1 on the right arm, therapy 2 for the left arm), they are the best way, because of minimising the patients’ variability, so also reducing the sample size. Conversely, we—as radiologists—should always ask for RCTs to recommend new screening strategies, to avoid biases inherent to screening (length bias and lead time bias) [33] and to reach the highest level in the hierarchy of studies of diagnostic tests, up to the societal level (e.g. reduction of mortality as an effect of secondary disease prevention) [34].
A challenge is that the higher the levels of evidence we want to obtain, the higher the costs, the longer the time, and the more complex the research organisation we need. Radiology departments commonly do not have their own research nurses, data managers, or statisticians. The work is mostly done by clinical radiologists who also dedicate time to research or by radiology residents. The oft-reported burnout among radiologists due to excessive clinical workload could further impact research activities in radiology departments [35,36,37]. Even when PhD students are involved, we should consider that they frequently pursue a clinical rather than a scientific career after obtaining their PhD title. We need research professionals inside radiology departments, the same being true for data scientists and AI experts, to promote cross-fertilisation [38].
As a general advice to the radiological community, we should:
-
i.
Prefer multicentre over monocentric studies
-
ii.
Make preliminary calculations of statistical power and sample size
-
iii.
Use prospective and retrospective study designs appropriately
-
iv.
Address all potential sources of bias limiting applicability
-
v.
Promote systematic reviews and meta-analyses led by radiologists
-
vi.
Promote cost-effectiveness analysis with radiologists well represented in the authorship
-
vii.
Perform research in a multidisciplinary team with awareness of clinical unmet needs
-
viii.
Promote RCTs, especially for interventional radiology
The last recommendation is an absolute need. Radiologists often invented and proposed procedures that then became clinical practice in the hands of other professionals (e.g. ultrasound for obstetrics/gynaecology, neurology, vascular surgery, urology, gastroenterology [39]). In the era of overdiagnosis (also related to an increasingly ageing population), it is important to minimise the impact of invasive procedures for confirming diagnosis or initiating treatment. Interventional radiology, being minimally invasive and already playing an increasing role in oncology, can substantially contribute to this objective [40].
Conclusion
Successful translation of radiological research into clinical practice requires multiple factors including a sound but at the same time tailored methodology, a multidisciplinary approach aiming beyond technical validation, and a focus on unmet clinical needs. Low levels of evidence are a threat to radiology through limited impact and low uptake in guidelines, resulting in low visibility and low credibility of our profession. While radiologists are generally considered important for clinical research, they do not always have a formal role in research involving radiological examinations performed by non-radiological clinical societies. It is our responsibility as radiologists to take the lead in radiological studies and strive towards the highest levels of evidence and reproducibility for the added value of the advances of our discipline. Last but not least, research led by radiologists holds the potential to illuminate areas that go beyond the initial questions and impact medicine more broadly. In this thematic series, we present the factors, not always well-known, behind the success of impactful radiological studies to provide guidance for future radiological research.
Availability of data and materials
The survey results are in full and available with the first/corresponding author (MS) and the ESR office. For reasons of confidentiality and privacy, these are not made publicly available.
Abbreviations
- AI:
-
Artificial intelligence
- CESM:
-
Contrast-enhanced spectral mammography
- CT:
-
Computed tomography
- EBM:
-
Evidence-based medicine
- EIBIR:
-
European Institute for Biomedical Imaging Research
- ESR:
-
European Society of Radiology
- EuroAIM:
-
European Network for the Assessment of Imaging in Medicine
- IPMN:
-
Intraductal papillary mucinous neoplasm
- MRI:
-
Magnetic resonance imaging
- RCT:
-
Randomised controlled trial
- SICUS:
-
Small intestine contrast ultrasonography
- US:
-
Ultrasound
References
Brady AP, Bello JA, Derchi LE et al (2020) Radiology in the era of value-based healthcare: a multi-society expert statement from the ACR, CAR, ESR, IS3R, RANZCR, and RSNA. Insights Imaging 11:136
Sardanelli F, Hunink MG, Gilbert FJ, Di Leo G, Krestin GP (2010) Evidence-based radiology: why and how? Eur Radiol 20:1–15
Fryback DG, Thornbury JR (1991) The efficacy of diagnostic imaging. Med Decis Making 11:88–94
Kainberger F, Czembirek H, Fruhwald F, Pokieser P, Imhof H (2002) Guidelines and algorithms: strategies for standardization of referral criteria in diagnostic radiology. Eur Radiol 12:673–679
Kasivisvanathan V, Rannikko AS, Borghi M et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 378:1767–1777
Berkhemer OA, Fransen PS, Beumer D et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11–20
Heindel W, Weigel S, Gerss J et al (2022) Digital breast tomosynthesis plus synthesised mammography versus digital screening mammography for the detection of invasive breast cancer (TOSYMA): a multicentre, open-label, randomised, controlled, superiority trial. Lancet Oncol 23:601–611
Weigel S, Heindel W, Hense HW et al (2023) Breast density and breast cancer screening with digital breast tomosynthesis: a TOSYMA Trial Subanalysis. Radiology 306:e221006
Lim KJ, Yoon DY, Yun EJ et al (2012) Characteristics and trends of radiology research: a survey of original articles published in AJR and Radiology between 2001 and 2010. Radiology 264:796–802
Hong SJ, Yoon DY, Cho YK et al (2016) Characteristics and quality of radiologic randomized controlled trials: a bibliometric analysis between 1995 and 2014. AJR Am J Roentgenol 206:917–923
Hollingworth W, Jarvik JG (2007) Technology assessment in radiology: putting the evidence in evidence-based radiology. Radiology 244:31–38
Sardanelli F, Bashir H, Berzaczy D et al (2014) The role of imaging specialists as authors of systematic reviews on diagnostic and interventional imaging and its impact on scientific quality: report from the EuroAIM Evidence-based Radiology Working Group. Radiology 272:533–540
NICE (2921) Brain tumours (primary) and brain metastases in over 16s. NICE guideline [NG99]. Available via https://www.nice.org.uk/guidance/ng99. Accessed 4 Aug 2023
Bossuyt PM, Reitsma JB, Bruns DE et al (2015) STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. Radiology 277:826–832
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350:g7594
Brouwers MC, Kho ME, Browman GP et al (2010) AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ 182:E839-842
Brouwers MC, Kerkvliet K, Spithoff K, Consortium ANS (2016) The AGREE Reporting Checklist: a tool to improve reporting of clinical practice guidelines. BMJ 352:i1152
Clarke GM, Conti S, Wolters AT, Steventon A (2019) Evaluating the impact of healthcare interventions using routine data. BMJ 365:l2239
Akoudad S, Portegies ML, Koudstaal PJ et al (2015) Cerebral microbleeds are associated with an increased risk of stroke: the Rotterdam Study. Circulation 132:509–516
Akoudad S, Wolters FJ, Viswanathan A et al (2016) Association of cerebral microbleeds with cognitive decline and dementia. JAMA Neurol 73:934–943
Schunemann HJ, Lerda D, Quinn C et al (2020) Breast cancer screening and diagnosis: a synopsis of the European breast guidelines. Ann Intern Med 172:46–56
Menon U, Gentry-Maharaj A, Burnell M et al (2023) Mortality impact, risks, and benefits of general population screening for ovarian cancer: the UKCTOCS randomised controlled trial. Health Technol Assess. https://doi.org/10.3310/BHBR5832:1-81
Marti-Bonmati L, Koh DM, Riklund K et al (2022) Considerations for artificial intelligence clinical impact in oncologic imaging: an AI4HI position paper. Insights Imaging 13:89
European Society of Radiology (2021) Patient survey of value in relation to radiology: results from a survey of the European Society of Radiology (ESR) value-based radiology subcommittee. Insights Imaging 12:6
Bui KT, Liang R, Kiely BE, Brown C, Dhillon HM, Blinman P (2021) Scanxiety: a scoping review about scan-associated anxiety. BMJ Open 11:e043215
Gabelloni M, Faggioni L, Borgheresi R et al (2022) Bridging gaps between images and data: a systematic update on imaging biobanks. Eur Radiol 32:3173–3186
Turner T, Misso M, Harris C, Green S (2008) Development of evidence-based clinical practice guidelines (CPGs): comparing approaches. Implement Sci 3:45
Rosenfeld RM, Shiffman RN (2009) Clinical practice guideline development manual: a quality-driven approach for translating evidence into action. Otolaryngol Head Neck Surg 140:S1-43
Taylor SA, Mallett S, Miles A et al (2017) Streamlining staging of lung and colorectal cancer with whole body MRI; study protocols for two multicentre, non-randomised, single-arm, prospective diagnostic accuracy studies (Streamline C and Streamline L). BMC Cancer 17:299
Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A (2011) GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 64:380–382
Marti-Bonmati L (2021) Evidence levels in radiology: the insights into imaging approach. Insights Imaging 12:45
Centre for Evidence-Based Medicine. Oxford centre for evidence-based medicine: levels of evidence (March 2009) Availabe at https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009. Accessed 03 Oct 2023
Sardanelli F, Di Leo G (2009) Biostatistics for radiologists. Springer, Milan, pp 176–177
Colarieti A, Sardanelli F (2023) Clinical trials for evidence-based radiology: to randomize or not to randomize? This is the question. Radiol Med. https://doi.org/10.1007/s11547-023-01746-y
Wan Z, Tang J, Bai X et al (2023) Burnout among radiology residents: a systematic review and meta-analysis. Eur Radiol. https://doi.org/10.1007/s00330-023-09986-2
Molwitz I, Kemper C, Stahlmann K et al (2023) Work expectations, their fulfillment, and exhaustion among radiologists of all career levels: what can be learned from the example of Germany. Eur Radiol 33:5664–5674
Koo HJ, Do KH (2023) The manpower crisis and burnout in academic radiology: insights from a survey study in Korea. J Am Coll Radiol. https://doi.org/10.1016/j.jacr.2023.08.046
Sardanelli F, Colarieti A (2023) Open issues for education in radiological research: data integrity, study reproducibility, peer-review, levels of evidence, and cross-fertilization with data scientists. Radiol Med 128:133–135
European Society of Radiology (2014) International Summit 2014: organisation of clinical ultrasound in the world. Insights Imaging 5:641–644
Elsayed M, Solomon SB (2023) Interventional oncology: 2043 and beyond. Radiology 308:e230139
Acknowledgements
This is the founding article of the thematic series entitled Translating radiological research into practice—from discovery to clinical impact (guest editor: Marion Smits (Rotterdam/NL)).
It was endorsed by the ESR Executive Council in December 2023.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
MS drafted the manuscript outline and survey. All authors contributed to the writing of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
MS declares honoraria (paid to the institution) for consultancy from Bracco and for speaking from AuntMinnie, GE Healthcare, and Fondazione Internazionale Menarini.
AR declares Advisory Board and RoClub.
SNC is a co-founder of MyeloPro Diagnostics and Research GmbH and has been a consultant for GSK Belgium.
FS declares research grants from Bayer, Bracco, and General Electric.
LMB is a member of the non-profit Scientific Advisory Boards of Quibim SL, the Girona Biomedical Research Institute (IDIBGI), and the Instituto de Instrumentación para Imagen Molecular (CSIC-UPV). He is also Editor in Chief of Insights Into Imaging.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This is the founding article of the thematic series entitled Translating radiological research into practice—from discovery to clinical impact (guest editor: Marion Smits (Rotterdam/NL)).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Smits, M., Rockall, A., Constantinescu, S.N. et al. Translating radiological research into practice—from discovery to clinical impact. Insights Imaging 15, 13 (2024). https://doi.org/10.1186/s13244-023-01596-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-023-01596-2