Abstract
Background
Secondary prevention clinical trials for Alzheimer’s disease (AD) target amyloid accumulation in asymptomatic, amyloid-positive individuals, but it is unclear to what extent other pathophysiological processes, such as small vessel cerebrovascular disease, account for participant performance on the primary cognitive outcomes in those trials. White matter hyperintensities are areas of increased signal on T2-weighted magnetic resonance imaging (MRI) that reflect small vessel cerebrovascular disease. They are associated with cognitive functioning in older adults and with clinical presentation and course of AD, particularly when distributed in posterior brain regions. The purpose of this study was to examine to what degree regional WMH volume is associated with performance on the primary cognitive outcome measure in the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s Disease (A4) study, a secondary prevention trial.
Methods
Data from 1791 participants (59.5% women, mean age (SD) 71.6 (4.74)) in the A4 study and the Longitudinal Evaluation of Amyloid Risk and Neurodegeneration (LEARN) companion study at the screening visit were used to quantify WMH volumes on T2-weighted fluid-attenuated inversion recovery (FLAIR) MR images. Cognition was assessed with the preclinical Alzheimer cognitive composite (PACC). We tested the association of total and regional WMH volumes with PACC performance, adjusting for age, education, and amyloid positivity status, with general linear models. We also considered interactions between WMH and amyloid positivity status.
Results
Increased frontal and parietal lobe WMH volume was associated with poorer performance on the PACC. While amyloid positivity was also associated with lower cognitive test scores, WMH volumes did not interact with amyloid positivity status.
Conclusion
These results highlight the potential of small vessel cerebrovascular disease to drive AD-related cognitive profiles. Measures of small vessel cerebrovascular disease should be considered when evaluating outcome in trials, both as potential effect modifiers and as a possible target for intervention or prevention.
Similar content being viewed by others
Background
Pathogenic models of Alzheimer’s disease (AD) emphasize a biological cascade that begins with amyloid accumulation, followed by tau pathology, neurodegeneration, and subsequent cognitive decline and dementia [1, 2]. While this “amyloid cascade hypothesis” remains quite controversial, it has defined both diagnostic frameworks [3] and strategies for disease treatment and prevention [4]. Observational research from individuals with autosomal dominant, fully penetrant, mutations for AD suggests that amyloid accumulation initiates years, perhaps decades, prior to the onset of clinical symptoms [5]. With the development of neuroimaging and fluidic diagnostic biomarkers for AD, it is now possible to characterize AD pathophysiology in these early, presymptomatic phases of the disease.
Monoclonal antibodies that target the accumulation of amyloid protein remain the primary experimental approach towards disease treatment. Two distinct views have resulted from several clinical antibody trials that failed to show clinical efficacy or modest effects despite evidence of target engagement [6]. The first argues that amyloid pathology is not linked causally to the development and progression of clinical symptoms in AD and questions the fundamental basis of the amyloid cascade hypothesis [7]. The second argues that amyloid removal is still a viable treatment for AD but will only be effective in very early stages of disease pathogenesis [8]. Indeed, among myriad failed trials, three phase 3 trials that included patients with very mild or presymptomatic disease suggest some degree of clinical efficacy in primary [9, 10] or post hoc [11] analyses, which led to FDA approval of lecanemab and aducanumab. Despite the unambiguous ability to clear amyloid from the brain based on changes in biomarker profiles, these medications provide only the mildest clinical benefit to patients, suggesting that amyloid may be one of the factors implicated in AD pathophysiology, but its removal is not a panacea.
Most treatment or secondary prevention clinical trials for AD that target beta-amyloid require that participants have pathophysiological evidence of AD via positron emission tomography (PET) or cerebrospinal fluid biomarkers and have exclusion criteria for significant comorbidities, including suspected cerebrovascular disease. Although there are often other practical or methodological justifications for excluding one pathology in a trial to study another, the primary argument is that in order to determine whether a medication is helpful to individuals suffering from or at risk for a disease, only those with the “purest” forms should be included in trials to ensure that the potential therapeutic outcome of target engagement is not confounded or masked by another disease process. This approach has likely contributed to systematic exclusion of minoritized groups from clinical trials for AD because of differential base rates in comorbidities [12] and otherwise might not be a valid strategy towards evaluating treatment efficacy. Indeed, pathological and neuroimaging data confirm that the majority of symptomatic individuals with AD have evidence of cerebrovascular disease, which cerebrovascular disease precedes symptom onset in AD even in autosomal dominant forms, and that cerebrovascular disease contributes to symptom onset and progression [13,14,15,16,17,18]. Taken together, the evidence suggests that cerebrovascular disease is a core feature of AD, and imposing exclusion criteria in clinical trials that leave out individuals with suspected or peripheral risk factors for cerebrovascular disease may attenuate but not eliminate its impact on clinical outcomes.
In the current study, we tested the hypothesis that small vessel cerebrovascular disease, operationally defined as white matter hyperintensity (WMH) volume on T2-weighted magnetic resonance imaging (MRI), contributes to primary cognitive outcome performance in a secondary prevention trial for AD. We used screening data from the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s (A4) study, a secondary prevention trial of solanezumab in preclinical AD, and the Longitudinal Evaluation of Amyloid Risk and Neurodegeneration (LEARN) companion study. A unique aspect of A4 and LEARN is that individuals with vascular risk factors were not systematically excluded from participation, allowing us to examine the role of a range of cerebrovascular disease severity in typical prospective AD trial participants.
Methods
Participants
Data for the current analyses came from participants who were included in the screening visit for the A4 study, a multicenter clinical trial enrolling cognitively unimpaired older adults (ages 65 to 85) with evidence of increased amyloid accumulation in the brain [8, 19]. This secondary prevention trial evaluated the impact of solanezumab, a monoclonal antibody targeting beta amyloid’s mid-peptide domain, on cognitive progression in individuals characterized as having preclinical AD [19]. Major inclusion criteria for participants in the A4 study were the evidence of elevated brain amyloid levels determined by amyloid PET imaging, the classification of cognitively unimpaired at study enrollment, and access to a study partner willing to participate and provide information on participants’ daily life cognitive function. Major exclusion criteria included receiving treatment for AD with acetylcholinesterase inhibitors; serious or unstable medical, psychiatric, or neurological conditions; suicidality; or recent history of alcohol or substance abuse or dependence [8]. The screening procedure involved an initial cognitive assessment followed by PET imaging to determine amyloid status. After amyloid status was determined, participants with elevated amyloid received structural MRI. Participants determined to be amyloid negative were referred to the Longitudinal Evaluation of Amyloid Risk and Neurodegeneration (LEARN) study [8]. The LEARN study was run in parallel with the A4 clinical trial to act as a comparison group and further characterize preclinical AD vis-à-vis normal aging. LEARN participants received the same longitudinal imaging and clinical assessments as participants in the A4 clinical trial. Imaging data for a total of 1791 screening participants were included in these analyses; Table 1 displays the demographic characteristics of these participants. The enrollment outcome for these participants was not known at the time of our analysis, but all participants underwent cognitive assessment, amyloid PET imaging, and MRI scanning and met inclusion criteria for either the A4 or LEARN studies.
Cognitive assessment
Cognitive testing took place before PET imaging eligibility was determined. The primary cognitive outcome measure used in the A4 study is the preclinical Alzheimer cognitive composite (PACC) [20]. The PACC is derived from four cognitive measures: Free and Cued Selective Reminding Test [21], Logical Memory Test delayed recall (LMDR-IIa) [22], Digit Symbol Substitution Test [23], and Mini-mental State Examination (MMSE) [24]. Scores from each of the four components were normalized using the mean and standard deviation of the sample group; the standardized z scores were then summed to give the composite score used in these analyses [20]. Participants scoring very high (1.5 SD above the norm) or very low (1.5 SD below the norm) on LMDR-IIa were excluded after the first screening visit, before imaging data were collected, in hopes of increasing the likelihood of enrolling participants with a higher risk of imminent cognitive decline associated with AD pathophysiology and removing those with mild cognitive impairment (MCI) [8]. Participants with MMSE scores of 25 to 30, LMDR-IIa scores of 6 to 18, and a Clinical Dementia Ratings of 0 were eligible for further screening with an amyloid PET scan.
Amyloid PET imaging
Florbetapir PET imaging was used to assess amyloid burden. Images were acquired 50 to 70 min post-injection of 10 mCi of florbetapir F18 and analyzed using a mean cortical standardized uptake value ratio (SUVR) calculated with the whole cerebellum as a reference region [25]. A subset of participants’ amyloid eligibility assessments was verified by two-reader visual consensus before the decision to implement automatic inclusion of participants meeting a composite SUVR of 1.15 or greater at screening [8]. This change led to amyloid positive eligibility assessment outcomes for some individuals with a composite summary SUVR below the threshold (137 subjects, 11%, of the amyloid positive group included in these analyses). Amyloid positivity status for the analyses included here is based on the eligibility assessment outcomes.
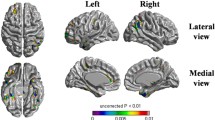
MRI acquisition and WMH quantification
Axial T2-weighted fluid-attenuated inversion recovery (FLAIR) MRI images (resolution, 0.86 mm, 0.86 mm, 5 mm; field of view, 256 × 256 × 35) were acquired for a majority of A4 and LEARN screening participants on study-approved 3T scanners with harmonized protocols after PET eligibility was determined. White matter hyperintensity volume was quantified with an automated algorithm with manual corrections (Fig. 1) [26]. Briefly, the method involves preprocessing the FLAIR images to remove non-brain tissue, correcting for intensity bias, and implementing a high-pass filter to remove voxels with intensity values equal to or below the mode. Intensity values of the preprocessed FLAIR images are then log transformed and fit to a half-Gaussian mixture model, in which the histogram containing an upper Gaussian curve captures image voxels within the distribution of WMH. The voxels within this range are labeled, and the mask is visually inspected and manually edited to remove any false-positive errors. We calculated total WMH volume and regional (frontal, temporal, parietal, and occipital lobe) WMH volumes in cm3. Regional WMH volumes were derived by co-registering a lobar atlas [27] to the FLAIR scans. Voxels within each of those regions are added and multiplied by the voxel dimensions to derive the regional WMH volumes.
Statistical analysis
Demographic characteristics and total and regional WMH volumes were compared between participants in A4 and in LEARN with t-tests for continuous variables and chi-squared tests for proportional data. A series of general linear models tested the association of total and regional WMH volumes with PACC scores; these analyses included age, number of years of education, and amyloid status (elevated or not elevated) as additional predictor variables. In subsequent models, we added a term capturing the interaction between total or regional WMH and amyloid status to test whether the association of WMH volumes with PACC score differed in individuals with and without elevated amyloid. Akaike information criterion (AIC), a log-likelihood metric penalized for the number of model parameters (lower is better), was used to determine the most parsimonious model (i.e., model containing only main effects versus a model containing a WMH × amyloid interaction term). Adjusted R2 values, also penalized for the number of model parameters (higher is better), were used to compare the total variance in the outcome that was explained by the model. The square of the partial correlation was used to determine the proportion of the variance attributable to each covariate within the models. Note that because all participants included from the A4 trial had elevated amyloid levels and all participants in the LEARN study did not have elevated amyloid levels, main effects and interactions with amyloid status reflect the effects of substudy as well.
Results
Table 1 displays the demographic characteristics of A4 and LEARN participants, corresponding to those with and without elevated amyloid levels, respectively. As is typical of clinical therapeutic trials in symptomatic or preclinical AD, participants were predominantly women, were in their early 70 s, were predominantly non-Latinx white, and had high levels of education. Participants in A4 (elevated amyloid levels) were older than those in LEARN (non-elevated amyloid) but were otherwise similar in sex/gender, race, ethnicity, and education. The two groups also did not differ in total WMH volumes; however, those enrolled in A4 had lower temporal lobe WMH volumes but greater occipital lobe WMH volumes.
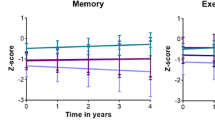
As seen in Table 2 and in Fig. 2, higher total, frontal, and parietal WMH volumes were associated with lower PACC scores. As expected, elevated amyloid was also associated with poorer PACC performance. The AIC, adjusted R2, and the interaction effect size (interaction effects = − 0.0049–0.003, p-values = 0.48–0.95) converged to indicate that total and regional WMH volumes did not interact with amyloid status on PACC scores, suggesting that the association of total and regional WMH with cognitive outcomes is similar in those with and without elevated amyloid. The total variance accounted for in PACC scores was small to moderate for each model. In models with a significant WMH effects, total, frontal, and parietal WMH volumes accounted for 1.4%, 2.7%, and 1.6% of the total variance, respectively, while amyloid accounted for 3.5% in each model.
Discussion
We found that regionally distributed WMH, an indicator of small vessel cerebrovascular disease, are associated with cognitive functioning in a group of participants being considered for enrollment in a secondary prevention trial for AD targeting beta amyloid. As expected, the PET biomarker reflecting beta amyloid pathology was strongly related to cognition, but WMH additionally contributed independently and significantly to the amount of variance in the cognitive outcome. The findings have important implications for our understanding of sources of cognitive impairment in preclinical AD, for strategies to analyze and interpret AD clinical trial data, and for planning of future prevention or intervention trials in AD.
It is now well-established that regional cerebrovascular disease is associated with cognition, cognitive decline, and risk of and progression of both late onset and autosomal dominant AD [15,16,17,18]. This observation is recapitulated in the current study, which included older adults considered for a secondary prevention trial. We confirmed an association of total WMH with cognitive outcomes. In terms of impact of regional WMH distribution, we previously showed consistent associations between posterior distribution, typically parietal lobe, WMH, and outcomes related to AD [28]. Here, we observed the same regional effect but also found that frontal lobe WMH, which are typically attributed to age- and risk factor-related ischemic changes [29], are also related to cognitive outcomes. It is unclear what factors mediate the regional distribution of AD-associated WMH, but it is interesting to note that several pathophysiology features of AD converge in posterior areas relatively early in the disease process, including cerebral microbleeds, amyloid and tau pathology, atrophy, and glucose hypometabolism [30,31,32,33]. We speculate that upstream blood flow abnormalities in posterior regions may mediate some of this convergence. As in previous studies [34, 35], WMH volume was independent of and did not interact with amyloid status in its relationship with cognitive outcomes. Some work suggests that amyloid pathology does interact with small vessel cerebrovascular disease to affect rates of cognitive decline [36], so despite the independent effects we observed of the two markers cross-sectionally, they may have a synergistic impact on change in cognitive outcomes. Additionally, our previous work demonstrates an effect of small vessel cerebrovascular disease on tau pathology [37], raising the possibility of direct downstream consequence of cerebrovascular disease on AD pathophysiology. The findings in the current study confirm that even in typical prospective AD clinical trial participants, cerebrovascular disease contributes to the clinical profile. Notably, the impact of cerebrovascular disease on cognition was not trivial; whereas amyloid positivity status accounted for 3.5% variance in PACC scores, frontal lobe WMH accounted for 2.7%.
The relationship between regional WMH volume and performance on the PACC, which was the primary clinical efficacy outcome of the trial, suggests that WMH should be considered explicitly in the design and analysis of clinical trial data. We are unaware of trials that have examined baseline WMH as potential effect modifiers or factors that would need statistical adjustment when considering efficacy. However, the relationship we observed indicates WMH as a source of variance in trial outcomes that could potentially obscure treatment effects. The results of the A4 trial showed that solanezumab did not slow cognitive decline compared with placebo [34]; an important post hoc analysis should examine whether WMH affected the efficacy outcomes in this trial. Similarly, it is now well established that brain edema and hemorrhage, the so-called amyloid-related imaging abnormalities (ARIA-E and ARIA-H, respectively), are common side effects of monoclonal antibody treatments that target amyloid [38]. The presence of baseline microbleeds is one predictor of these adverse outcomes [38], but future analyses should consider whether small vessel disease manifesting as WMH may also signal who might be at risk for adverse events. Cerebral microbleeds may be difficult to detect, and their visualization is dependent on MRI scan protocols, resolution, and operator expertise; on the other hand, WMH are easily visualized and quantifiable and may provide similar or better indicators of risk. Future trials should consider analyses involving WMH for both efficacy and safety outcomes.
Limitations
There is considerable debate about whether WMH in the context of AD represent a purely vascular phenomenon or whether they are consequences of AD-related neurodegeneration [39, 40]. We have argued against the latter based on animal studies, anatomical distribution, temporality, and dissociations between vascular risk factors and WMH severity [41]. In the A4 trial, which includes individuals who are presymptomatic or have very mild symptoms, we would also not expect there to be significant white matter degeneration secondary to AD pathophysiology at such early disease stages. Additionally, while the A4 trial was designed to be more inclusive of race and ethnicity groups than previous AD trials [8], there was still bias [42], and the target numbers for inclusion of enrolled participants from racially and ethnically minoritized backgrounds were not reached. We [43, 44] and others [45] have documented differences in WMH volume across race/ethnicity minoritized groups and in the impact of WMH on cognitive outcomes. As recruitment and enrollment strategies of AD trials continue to improve with respect to more inclusive participation, the potential impact of cerebrovascular disease on the efficacy, and possibly safety, of trial outcomes will become more relevant.
Conclusions
Given the multifactorial etiology of cognitive decline in AD, efforts towards risk reduction and prevention via multidomain interventions that include management of cerebrovascular disease [46, 47], combination therapies [48], or explicit inclusion of individuals with cerebrovascular disease will continue to emerge as important strategies. Our study confirms the importance of multiple etiological factors in cognitive outcomes even among individuals considered for single mechanism secondary prevention AD trials.
Availability of data and materials
A4 trial data are available through the Laboratory of Neuroimaging, Image & Data Archive.
Abbreviations
- A4:
-
Anti-amyloid in asymptomatic alzheimer’s disease
- AD:
-
Alzheimer’s disease
- AIC:
-
Akaike information criterion
- FLAIR:
-
Fluid-attenuated inversion recovery
- LEARN:
-
Longitudinal evaluation of amyloid risk and neurodegeneration
- LMDR:
-
Logical memory delayed recall
- MCI:
-
Mild cognitive impairment
- MMSE:
-
Mini-mental state examination
- MRI:
-
Magnetic resonance imaging
- PACC:
-
Preclinical Alzheimer cognitive composite
- PET:
-
Positron emission tomography
- SUVR:
-
Standardized uptake value ratio
- WMH:
-
White matter hyperintensities
References
Jack CR, Knopman DS, Jagust WJ, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207–16.
Hardy JA, Higgins GA. Alzheimer’s disease: the amyloid cascade hypothesis. Science. 1992;256:184–5.
Jack CR, Bennett DA, Blennow K, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14:535–62.
Golde TE. The Aβ hypothesis: leading us to rationally-designed therapeutic strategies for the treatment or prevention of Alzheimer disease. Brain Pathol. 2006;15:84–7.
Bateman RJ, Xiong C, Benzinger TLS, et al. Clinical and biomarker changes in dominantly inherited Alzheimer’s disease. N Engl J Med. 2012;367:795–804.
Ackley SF, Zimmerman SC, Brenowitz WD, et al. Effect of reductions in amyloid levels on cognitive change in randomized trials: instrumental variable meta-analysis. BMJ. 2021;372: n156.
Kepp KP, Sensi SL, Johnsen KB, et al. The anti-amyloid monoclonal antibody lecanemab: 16 cautionary notes. JAD. 2023;94:497–507.
Sperling RA, Rentz DM, Johnson KA, Karlawish J, Donohue M, Salmon DP, Aisen P. The A4 study: stopping ad before symptoms begin? Sci Transl Med. 2014. https://doi.org/10.1126/scitranslmed.3007941.
van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388:9–21.
Sims JR, Zimmer JA, Evans CD, et al. Donanemab in early symptomatic Alzheimer disease: the TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA. 2023;330:512.
Knopman DS, Jones DT, Greicius MD. Failure to demonstrate efficacy of aducanumab: an analysis of the EMERGE and ENGAGE trials as reported by Biogen, December 2019. Alzheimer’s Dementia. 2021;17:696–701.
Manly JJ, Glymour MM. What the aducanumab approval reveals about Alzheimer disease research. JAMA Neurol. 2021;78:1305–6.
Kapasi A, DeCarli C, Schneider JA. Impact of multiple pathologies on the threshold for clinically overt dementia. Acta Neuropathol. 2017;134:171–86.
Prins ND, Scheltens P. White matter hyperintensities, cognitive impairment and dementia: an update. Nat Rev Neurol. 2015;11:157–65.
Brickman AM, Provenzano FA, Muraskin J, Manly JJ, Blum S, Apa Z, Stern Y, Brown TR, Luchsinger JA, Mayeux R. Regional white matter hyperintensity volume, not hippocampal atrophy, predicts incident Alzheimer disease in the community. Arch Neurol. 2012;69:1621–7.
Lee S, Viqar F, Zimmerman ME, et al. White matter hyperintensities are a core feature of Alzheimer’s disease: evidence from the dominantly inherited Alzheimer network. Ann Neurol. 2016;79:929–39.
Lao PJ, Gutierrez J, Keator D, et al. Alzheimer-related cerebrovascular disease in Down syndrome. Ann Neurol. 2020;88:1165–77.
Brickman AM, Honig LS, Scarmeas N, Tatarina O, Sanders L, Albert MS, Brandt J, Blacker D, Stern Y. Measuring cerebral atrophy and white matter hyperintensity burden to predict the rate of cognitive decline in Alzheimer disease. Arch Neurol. 2008;65:1202–8.
Sperling RA, Donohue MC, Raman R, et al. Trial of solanezumab in preclinical Alzheimer’s disease. N Engl J Med. 2023;389:1096–107.
Donohue MC, Sperling RA, Salmon DP, Rentz DM, Raman R, Thomas RG, Weiner M, Aisen PS. The preclinical Alzheimer cognitive composite. JAMA Neurol. 2014;71:961–70.
Grober E, Buschke H. Genuine memory deficits in dementia. Dev Neuropsychol. 1987;3:13–36.
Wechsler D. WMS-R: Wechsler Memory Scale--Revised : manual. Psychological Corporation. 1987
Wechsler D. WAIS-R manual: Wechsler Adult Intelligence Scale-Revised. Psychological Corporation. 1981
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Joshi AD, Pontecorvo MJ, Lu M, Skovronsky DM, Mintun MA, Devous MD. A semiautomated method for quantification of F 18 florbetapir PET images. J Nucl Med. 2015;56:1736–41.
Igwe KC, Lao PJ, Vorburger RS, Banerjee A, Rivera A, Chesebro A, Laing K, Manly JJ, Brickman AM. Automatic quantification of white matter hyperintensities on T2-weighted fluid attenuated inversion recovery magnetic resonance imaging. Magn Reson Imaging. 2022;85:71–9.
Admiraal-Behloul F, Olofesen H, Van den Heuvel D, Schmitz N, Reiber J, Van Buchem M. Fully automated lobe delineation for regional white matter lesion load quantification in a large scale study. Proc Int Soc Magnet Res Med. 2004
Brickman AM, Zahodne LB, Guzman VA, et al. Reconsidering harbingers of dementia: progression of parietal lobe white matter hyperintensities predicts Alzheimer’s disease incidence. Neurobiol Aging. 2015;36:27–32.
Pålhaugen L, Sudre CH, Tecelao S, et al. Brain amyloid and vascular risk are related to distinct white matter hyperintensity patterns. J Cereb Blood Flow Metab. 2021;41:1162–74.
Graff-Radford J, Botha H, Rabinstein AA, et al. Cerebral microbleeds: prevalence and relationship to amyloid burden. Neurology. 2019. https://doi.org/10.1212/WNL.0000000000006780.
Ossenkoppele R, Zwan MD, Tolboom N, et al. Amyloid burden and metabolic function in early-onset Alzheimer’s disease: parietal lobe involvement. Brain. 2012;135:2115–25.
Tanner JA, Iaccarino L, Edwards L, et al. Amyloid, tau and metabolic PET correlates of cognition in early and late-onset Alzheimer’s disease. Brain. 2022;145:4489–505.
Whitwell JL. Progression of atrophy in Alzheimer’s disease and related disorders. Neurotox Res. 2010;18:339–46.
Garnier-Crussard A, Bougacha S, Wirth M, et al. White matter hyperintensity topography in Alzheimer’s disease and links to cognition. Alzheimers Dement. 2022;18:422–33.
Koncz R, Sachdev PS. Are the brain’s vascular and Alzheimer pathologies additive or interactive? Curr Opin Psychiatry. 2018;31:147–52.
Ali DG, Abner EL, Bahrani AA, El Khouli R, Gold BT, Jiang Y, Wilcock DM, Jicha GA. Amyloid-PET and white matter hyperintensities have independent effects on baseline cognitive function and synergistic effects on longitudinal executive function. Brain Sci. 2023;13:218.
Laing KK, Simoes S, Baena-Caldas GP, et al. Cerebrovascular disease promotes tau pathology in Alzheimer’s disease. Brain Commun. 2020;2:fcaa132.
Hampel H, Elhage A, Cho M, Apostolova LG, Nicoll JAR, Atri A. Amyloid-related imaging abnormalities (ARIA): radiological, biological and clinical characteristics. Brain. 2023;146:4414–24.
Garnier-Crussard A, Cotton F, Krolak-Salmon P, Chételat G. White matter hyperintensities in Alzheimer’s disease: beyond vascular contribution. Alzheimers Dement. 2023;19:3738–48.
Shirzadi Z, Schultz SA, Yau W-YW, et al. Etiology of white matter hyperintensities in autosomal dominant and sporadic Alzheimer disease. JAMA Neurol. 2023;80:1353–63.
Brickman AM, Rizvi B. White matter hyperintensities and Alzheimer’s disease: an alternative view of an alternative hypothesis. Alzheimer’s Dementia. 2023;19:4260–1.
Deters KD, Napolioni V, Sperling RA, Greicius MD, Mayeux R, Hohman T, Mormino EC. Amyloid PET imaging in self-identified non-Hispanic Black participants of the anti-amyloid in asymptomatic Alzheimer’s disease (A4) study. Neurology. 2021;96:e1491–500.
Brickman AM, Schupf N, Manly JJ, et al. Brain morphology in older African Americans, Caribbean Hispanics, and Whites from northern Manhattan. Arch Neurol. 2008;65:1053–61.
Zahodne LB, Manly JJ, Narkhede A, Griffith EY, DeCarli C, Schupf NS, Mayeux R, Brickman AM. Structural MRI predictors of late-life cognition differ across African Americans, Hispanics, and Whites. Curr Alzheimer Res. 2015;12:632–9.
Morrison C, Dadar M, Manera AL, Collins DL. Racial differences in white matter hyperintensity burden in older adults. Neurobiol Aging. 2023;122:112–9.
Kivipelto M, Mangialasche F, Ngandu T, World Wide Fingers Network. World Wide FINGERS will advance dementia prevention. Lancet Neurol. 2018;17:27.
Kivipelto M, Mangialasche F, Snyder HM, et al. World-Wide FINGERS network: a global approach to risk reduction and prevention of dementia. Alzheimers Dement. 2020;16:1078–94.
McDade E, Llibre-Guerra JJ, Holtzman DM, Morris JC, Bateman RJ. The informed road map to prevention of Alzheimer disease: a call to arms. Mol Neurodegener. 2021;16:49.
Acknowledgements
The A4 study is a secondary prevention trial in preclinical Alzheimer’s disease, aiming to slow cognitive decline associated with brain amyloid accumulation in clinically normal older individuals. The A4 study is funded by a public-private-philanthropic partnership, including funding from the National Institutes of Health-National Institute on Aging, Eli Lilly and Company, Alzheimer’s Association, Accelerating Medicines Partnership, GHR Foundation, an anonymous foundation, and additional private donors, with in-kind support from Avid and Cogstate. The companion observational Longitudinal Evaluation of Amyloid Risk and Neurodegeneration (LEARN) study is funded by the Alzheimer’s Association and GHR Foundation. The A4 and LEARN studies are led by Dr. Reisa Sperling at Brigham and Women’s Hospital, Harvard Medical School, and Dr. Paul Aisen at the Alzheimer’s Therapeutic Research Institute (ATRI), University of Southern California. The A4 and LEARN Studies are coordinated by ATRI at the University of Southern California, and the data are made available through the Laboratory for Neuro Imaging at the University of Southern California. The participants screening for the A4 Study provided permission to share their de-identified data in order to advance the quest to find a successful treatment for Alzheimer’s disease. We would like to acknowledge the dedication of all the participants, the site personnel, and all of the partnership team members who continue to make the A4 and LEARN Studies possible. The complete A4 study team list is available on the following: a4study.org/a4-study-team.
Funding
This work was supported in part by grants from the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
CDM: design of the work; analysis and interpretation of data; drafted the work. DC-S: analysis of data. PJL: interpretation and analysis of data; interpretation of data; substantial revision. JFC: Analysis of data. JDP: Analysis of data; interpretation of data. MJA: Analysis of data; creation of software used in the work. RL: Analysis of data. KB: Analysis of data. CH: Design of the work. NCE: Analysis of data; interpretation of data. KCI: Analysis of data; creation of software used in the work. KD: Conception of work; interpretation of data. MEZ: Conception of work; interpretation of data. AMB: Conception and design of work; interpretation of data; drafted the work. All authors have approved the submitted version and have agreed to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which they were not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is a secondary data analysis of a publicly available dataset from the screening visit of the A4 trial. The A4 trial received ethics approval by Institutional Review Boards in accordance with International Council for Harmonisation Good Clinical Practice guidelines at each of the 67 trial sites in Australia, Canada, Japan, and the USA, and all participants gave written informed consent.
Consent for publication
Not applicable.
Competing interests
Dr. Brickman is an inventor on a patent for quantification of white matter hyperintensities. He is a scientific advisor for Cognition Therapeutics, Inc; CogState; and Cognito Therapeutics, Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Morales, C.D., Cotton-Samuel, D., Lao, P.J. et al. Small vessel cerebrovascular disease is associated with cognition in prospective Alzheimer’s clinical trial participants. Alz Res Therapy 16, 25 (2024). https://doi.org/10.1186/s13195-024-01395-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-024-01395-x