Abstract
Background
Identifying individuals with mild cognitive impairment (MCI) who are likely to progress to Alzheimer’s disease and related dementia disorders (ADRD) would facilitate the development of individualized prevention plans. We investigated the association between MCI and comorbidities of ADRD. We examined the predictive potential of these comorbidities for MCI risk determination using a machine learning algorithm.
Methods
Using a retrospective matched case-control design, 5185 MCI and 15,555 non-MCI individuals aged ≥50 years were identified from MarketScan databases. Predictive models included ADRD comorbidities, age, and sex.
Results
Associations between 25 ADRD comorbidities and MCI were significant but weakened with increasing age groups. The odds ratios (MCI vs non-MCI) in 50–64, 65–79, and ≥ 80 years, respectively, for depression (4.4, 3.1, 2.9) and stroke/transient ischemic attack (6.4, 3.0, 2.1). The predictive potential decreased with older age groups, with ROC-AUCs 0.75, 0.70, and 0.66 respectively. Certain comorbidities were age-specific predictors.
Conclusions
The comorbidity burden of MCI relative to non-MCI is age-dependent. A model based on comorbidities alone predicted an MCI diagnosis with reasonable accuracy.
Similar content being viewed by others
Background
Mild cognitive impairment (MCI) is a condition associated with memory loss and cognitive deficits beyond what is expected with normal aging and may be a transitional stage before Alzheimer’s disease and related dementias (ADRD) [1]. For individuals with MCI, the likelihood of progression to any form of dementia is estimated to occur at a rate three to five times higher than among those without MCI [2,3,4,5]. The prevalence of MCI in the United States (US) increases with age, ranging from about 7% of people aged 60 to 64 to about 25% of people aged 80 to 84 [6].
While MCI could be identified as part of regular care by primary care physicians (PCPs), studies have found that the detection of MCI is limited and published identification rates of MCI by PCPs are as low as six to 15% [7, 8]. PCPs’ perceived barriers to detection include patients who do not disclose symptoms and family members assuming that symptoms are a natural part of aging [9]. Additional reasons for missed opportunities to identify MCI individuals include the lack of widely used cognitive assessment tools, lack of training on cognitive assessments, inconsistent opportunities for screening, lack of easily accessible biomarkers and imaging tests, and limited time during patient visits [10, 11].
Timely identification of MCI is important to facilitate an individualized management plan that addresses underlying conditions and possibly slows the progression to ADRD [12, 13]. The Food & Drug Administration (FDA) has recently approved two drugs that target the underlying pathology of AD by aiming to remove amyloid-beta plaques from the brain. These medicines are indicated for treatment in the early stages of disease [14, 15]. Cummings et al. analyzed information on clinicaltrials.gov and found that among the 143 agents in development for AD treatment, more than half of the phase 3 studies included participants with preclinical AD, MCI, or mild AD [16].
The barriers to early identification point to the utility and value of a tool that could help PCPs detect warning signs of MCI, in particular in younger age groups with a lower prevalence. Such a tool could use electronic health records (EHR) data to estimate the risk of developing MCI based on the presence of comorbidities. Such a tool would facilitate the detection of MCI, leading to potential treatment. Other studies have focused on identifying medical risk factors for developing AD [17] or ADRD [18,19,20,21,22,23,24]. Machine learning models using a large dataset of medical claims and EHR data have been shown to be effective in predicting the onset of dementia [25]. Our study expands previous research by using traditional statistical and machine learning models to explore the risk for MCI in individuals with established ADRD comorbidities by age group.
Methods
Data source and study design
This non-interventional retrospective matched case-control study used the Merative MarketScan Commercial and Medicare Databases and had an observation period from January 01, 2014, through December 31, 2019. These databases represent the health services of employees, dependents, and retirees in the US with primary or Medicare coverage through privately insured fee-for-service, point-of-service, or capitated health plans. The Commercial and Medicare Databases are generally representative of the population in the US in terms of gender. All enrollment records and inpatient, outpatient, ancillary, and drug claims were collected and used for study population identification as well as outcomes measurements.
As the study did not involve interactions with or interventions among human subjects and all data were de-identified per US federal regulations (45 CFR 46, 102(f))20, it was exempt from institutional review board (IRB) review, consent requirements and registration.
Study population
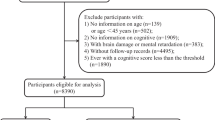
This study compared a cohort of individuals with an MCI diagnosis, but without an ADRD diagnosis at entry, to a cohort without an MCI or ADRD diagnosis. The index date for each individual in the MCI cohort was the date of the first MCI diagnosis. Individuals in the non-MCI cohort were matched three to one to an individual in the MCI cohort using age, sex, geographic region, and the year in which the individual had data entered into the MarketScan databases via the propensity score method. The index dates for non-MCI individuals were the index dates of their matched MCI individuals.
The pre-index period was defined as 2 years before the index date, and the follow-up period was defined as the time from the index date to the last visit recorded (minimum of one year of follow-up required). All individuals in the study were required to be at least 50 years old in the year of the index date. An MCI diagnosis was defined by an International Classification of Disease (ICD) code, either ICD-9 code 331.83 or ICD-10 code G31.84. To be included in the non-MCI cohort, individuals could not have an MCI or ADRD diagnosis throughout their inclusion in the MarketScan databases. All individuals were excluded if they (1) received a diagnosis of Parkinson’s disease at any time or (2) received donepezil, memantine, memantine/donepezil, galantamine, or rivastigmine during the pre-index period [26].
Study measures
Individuals in the MCI and non-MCI cohorts were categorized by age group (50 to 64 years, 65 to 79 years, 80+ years). Most individuals are eligible for Medicare at age 65, so 15-year increments were chosen to define age groups. Baseline demographic and clinical characteristics assessed included age at index, sex, region, Charlson Comorbidity Index (CCI), Elixhauser Comorbidity Index (ECI), ADRD comorbidities, and baseline treatments for non-AD-related conditions [27].
A literature review was conducted to identify ADRD comorbidities [28,29,30]. Twenty-seven ADRD comorbidities were identified, which will be simply referred to as comorbidities. These were categorized and included cardiovascular diseases (hypertension, stroke/transient ischemic attack [TIA], ischemic heart disease, congestive heart failure, myocardial infarction, atherosclerosis, atrial fibrillation), metabolic disorders (diabetes, hyperlipidemia, obesity, metabolic syndrome, weight loss), psychiatric disorders (depression, insomnia, bipolar, schizophrenia, psychosis, alcohol abuse, drug abuse), and other diseases (chronic kidney disease, chronic periodontitis, chronic pulmonary disease, hearing loss, obstructive sleep apnea, disturbances of sensation of smell and taste, hypothyroidism, traumatic brain injuries/concussion). Indices of these comorbidities and their treatments within 2 years before the index date were derived using ICD-9 and ICD-10 codes from both inpatient and outpatient visits [27]. Chronic periodontitis and traumatic brain injuries/concussion were excluded from the analysis because less than 0.3% of individuals with MCI had either condition.
Statistical analysis
Continuous variables were reported as mean (standard deviation [SD]) and median (lower quartile [Q1]–upper quartile [Q3]) and range by cohort, and subgroups in the MCI and non-MCI cohorts were compared using an independent t-test. Categorical variables were reported as frequencies and percentages, and cohorts, and subgroups in the MCI and non-MCI cohorts were compared using a chi-square test.
Odds ratios (ORs, MCI vs non-MCI) and two-sided 95% confidence intervals (CIs) were calculated based on percentages for each comorbidity for all patients and each age group. If the lower bound of the 95% CI was greater than one, it would indicate a statistically significant association between MCI and comorbidity. Furthermore, the ORs of each comorbidity among age groups were compared using a logistic regression model that included the age by comorbidity interaction term, including one comorbidity at a time. If a p-value for the age by comorbidity interaction term was less than 0.05, the ORs between the age groups would be considered statistically significantly different.
To predict the risk for MCI, several machine learning approaches (Bayesian logistic lasso regression [BLLR] with a mixture of double-exponential prior [31], stochastic gradient boosting machine, extreme gradient boosting [XGBoost], and regularized random forests) were applied. The area under the curve (AUC) of the receiver operating characteristic (ROC) curve, which was referred to as ROC-AUC, was used to evaluate each model. For machine-learning approaches, the model included age, sex, and 25 comorbidities as predictors; a subset of ADRD comorbidities was automatically selected by these algorithms, with the appropriate weight given based on their relative influence on the prediction. Training and test sets were created via a random 70–30% split, stratified by MCI/non-MCI status and by age. The MCI/non-MCI imbalance was accounted for in the prediction modeling algorithm by using the prevalence rate as the probability cutoff. Prediction performance was first evaluated within the 70% training set via ten iterations of ten-fold stratified cross-validation followed by evaluation in the 30% test set via the AUC of the ROC (ROC-AUC) [32]. Results from the best-performing algorithm are reported. The ROC-AUCs were compared via a bootstrap testing procedure [33].
All descriptive analyses were performed using SAS statistical software (version 9.4). The machine learning approaches were performed using R (version 4.2.2) [34].
Results
Demographics and clinical characteristics of the two cohorts at baseline
A total of 5185 individuals with an MCI diagnosis and 15,555 matched non-MCI individuals met the eligibility criteria. The mean age at index was 67 years for both the MCI and non-MCI cohorts, and 57.7% of individuals were female (Table 1). Mean CCI and ECI were higher in the MCI cohort compared to the non-MCI cohort (1.5 vs. 1.0 and 2.6 vs. 1.8, respectively; p < .001) (Table 1).
Twenty-five ADRD comorbidities were found to occur in statistically significantly higher proportions in MCI individuals vs. non-MCI individuals, with the lower 95% CI limits of the ORs greater than one (Table 1). The MCI cohort had a statistically significantly higher frequency of patients with one or more of the 25 comorbidities (95.6% vs. 81.4%) with OR (MCI vs non-MCI, 95% CI) of 4.9 (4.3, 5.7) (Table 1).
The 15 comorbidities with the largest frequency in the MCI cohort were as follows: hyperlipidemia (66.0%), hypertension (65.2%), depression (31.3%), obstructive sleep apnea (27.8%), diabetes (25.2%), hypothyroidism (25.0%), chronic pulmonary disease (24.2%), ischemic heart disease (21.9%), stroke/TIA (21.0%), hearing loss (21.0%), obesity (17.9%), insomnia (14.6%), atherosclerosis (10.0%), atrial fibrillation (9.6%), and congestive heart failure (8.0%) (Table 1).
The 15 comorbidities with the largest OR (MCI vs. non-MCI) were as follows: psychosis with an OR (95% CI) of 8.2 (5.3, 12.8), bipolar 6.7 (4.8, 9.2), schizophrenia 4.9 (2.4, 9.7), disturbances of sensation of smell and taste 4.4 (2.6, 7.4), depression 3.8 (3.5, 4.1), stroke/TIA 3.3 (3.0, 3.6), drug abuse 3.1 (2.4, 3.9), obstructive sleep apnea 2.9 (2.7, 3.1), weight loss 2.8 (2.4, 3.2), insomnia 2.7 (2.4, 2.9), alcohol abuse 2.6 (2.1, 3.3), hearing loss 2.1 (1.9, 2.3), metabolic syndrome 2.1 (1.8, 2.5), ischemic heart disease 1.7 (1.6, 1.8), and hyperlipidemia 1.6 (1.5, 1.7) (Table 1).
Seven comorbidities appeared on both lists of the highest frequency and highest OR. These seven were presented in the order of OR as follows: depression, stroke/TIA, obstructive sleep apnea, insomnia, hearing loss, ischemic heart disease, and hyperlipidemia.
When compared by age group, the OR (MCI vs non-MCI) decreased significantly with increasing age groups across the 25 comorbidities (Fig. 1). For depression, the OR was statistically significantly higher for the age 50 to 64 age group (4.4 [4.0, 4.9]) compared with the 65 to 79 age group (3.1 [2.7, 3.6]) and 80+ age group (2.9 [2.4, 3.6]) (p < .05). For stroke/TIA, the OR was significantly greater in the 50 to 64 years age group (6.4 [5.4, 7.5]) compared with 65 to 79 years (3.0 [2.6, 3.5]) and 80+ years (2.1 [1.8, 2.5]) with p < .05.
Forest plot of the prevalence odds ratio of ADRD comorbidities at baseline by age group. Note. ORs and 95% confidence intervals were calculated directly from percentages and frequencies for MCI and non-MCI cohorts in each age group. The p-values were for testing the equality of ORs among age groups and obtained by assessing comorbidity by age group interaction in the logistic regression model with cohort as response variable and the comorbidity, age group, and the interaction of the comorbidity by age group
MCI risk prediction models
As the other machine-learning algorithms such as stochastic gradient boosting and random forests yielded similar prediction performance with the ROC-AUCs ranging from 74 to 76% and were not significantly different from the BLLR algorithm (p > 0.05, based on bootstrap test) [33], the results from only the BLLR algorithm are reported in this paper due to its simplicity and ease of interpretation. The BLLR had ROC-AUC 0.72 (Table 2) for the analysis of all individuals; age was a significant (p <.001) predictor while sex was not.
Performance of the model for MCI risk prediction varied widely across the three age groups with ROC-AUC 0.75, 0.70, and 0.66 for the age groups 50 to 64 years, 65 to 79 years, and 80+ years, respectively (Table 2). The ROC-AUC value for the 50 to 64 years age group was statistically significantly higher than both the 65 to 79 age group (p < .05) and the 80+ age group (p < .05). However, the difference between the ROC-AUC values for the 65 to 79 age group and the 80+ age group was not statistically significantly different (p = .1299). The sensitivity and specificity are presented in Table 2. The 50 to 64 years group had the best performance with a sensitivity of 61.9% and a specificity of 77.4%; the 65–79 years group had a sensitivity of 59.3% and a specificity of 71.7%; the 80+ years had the least performance with a sensitivity of 55.3% and a specificity of 66.8%.
The BLLR identified the comorbidities that were significant predictors of MCI for each age group (Fig. 2). For age group 50 to 64 years, 12 comorbidities were significant predictors of MCI diagnosis in the multivariate model with p-values < 0.05: depression, stroke/TIA, obstructive sleep apnea, hearing loss, bipolar, psychosis, hypothyroidism, insomnia, weight loss, chronic pulmonary disease, alcohol abuse, and drug abuse. For the age group 65 to 79 years, five comorbidities significantly impacted the model with p-values < 0.05: stroke/TIA, depression, obstructive sleep apnea, hearing loss, and weight loss. For the age group 80+ years, four comorbidities significantly impacted the model with p-values < 0.05: depression, hearing loss, stroke/TIA, and weight loss.
Discussion
The results of this retrospective study of the MarketScan Commercial and Medicare Databases suggest that ADRD comorbidities are also comorbidities for MCI. The BLLR algorithm was selected due to its simplicity and interpretability and because it yielded similar prediction performance as the other machine-learning algorithms.
The 25 ADRD comorbidities identified by our literature search were also significant risk factors for MCI in this population. Individuals in the MCI cohort had a higher frequency of comorbidities compared with the non-MCI cohort. The differences between cohorts for depression and stroke/TIA were the largest. Depression, stroke/TIA, obstructive sleep apnea, insomnia, hearing loss, ischemic heart disease, and hyperlipidemia appeared on both the list of the highest frequency comorbidities and the list of comorbidities with the highest ORs, suggesting these seven comorbidities may be predictive of MCI. Considering that MCI is a prodromal stage for ADRD, the connection between ADRD comorbidities and MCI comorbidities is not unexpected; however, identifying the comorbidities with the strongest connections and quantifying the relationships can help inform the development of a screening tool to identify high-risk individuals.
Secondly, the ORs (MCI vs. non-MCI) decreased with increasing age group for all comorbidities. The differences were statistically significantly higher for the age 50 to 64 group compared with both older age groups. As a result, the potential for ADRD comorbidities to predict MCI risk also declined with increasing age group. The BLLR results in this study demonstrated better model predictivity in the younger age group. Depression, stroke/TIA, hearing loss, and weight loss were significant predictors across all age groups; however, obstructive sleep apnea was significant only for the two youngest age groups. Furthermore, hypothyroidism, insomnia, bipolar, chronic pulmonary disease, psychosis, alcohol abuse, and drug abuse were only significant for the youngest age group.
Changes in the likelihood of observing a particular comorbidity in different age groups may be related to the epidemiology of the specific condition. For cardiovascular and metabolic diseases, frequencies increased by age group in both the MCI and non-MCI cohorts; thus, ORs decreased. This aligns with the literature because people are more likely to develop cardiovascular and metabolic diseases with increasing age [35,36,37]. The association between hypertension in midlife, which aligns with the youngest age group for this study, and cognitive decline has been well established [38, 39]. The relationship between hypertension developing in late life and dementia is less clear. A 24-year prospective study found that in addition to hypertension in midlife and late life, a history of hypertension followed by late-life hypotension was also associated with an increased risk of dementia [40]. Our study evaluates hypertension over a shorter time period but confirms the importance of considering the temporal effects of comorbidities.
The frequency of psychiatric disorders, including depression and bipolar, decreased in the oldest age group in both cohorts. This aligns with the literature because the prevalence of psychiatric disorders decreases with age, in part because of the reduction in life expectancy of people with depression [41].
The observed differences in the oldest and youngest age groups in this study may have been impacted by survivorship bias. To reach the oldest age group, individuals likely maintained good health during the prior years. The number of years with comorbidity is likely to impact the onset of dementia and longevity [42].
Another possible contributor to lower ORs in the older age groups in this study may be the effect of undiagnosed MCI in the non-MCI cohort. The proportion of undiagnosed MCI individuals is likely similar to MCI prevalence at the population level, which increases with age. For people aged 50 to 64 years, the MCI prevalence is about 6.7% [4]. If our cohorts are similar to the general population, the non-MCI cohort may include a similar percentage of undiagnosed MCI individuals, which should have little impact on the frequencies for comorbidities in the non-MCI cohort and the ORs. However, for the 80+ years group, the MCI prevalence in the general population is about 25.2% [4]; the impact of undiagnosed MCI on ORs in this age group may not be ignored.
Our findings suggest that chronic pulmonary disease is a predictor of MCI; however, reports of the association between chronic obstructive pulmonary disease and ADRD outcomes are conflicting and limited [35, 36]. Thus, additional research on the association between chronic pulmonary disease and MCI and ADRD is recommended, as well as further evaluation to quantify the impact of smoking on MCI.
Chronic periodontitis and head injury were excluded from this analysis because fewer than 0.3% of individuals received a diagnosis. For chronic periodontitis, this may be because dentists were most likely to diagnose and treat that condition. MarketScan data do not capture dental records. A diagnosis of chronic periodontitis would only be captured in the dataset if it were noted in a medical office setting. For head injury, a longer baseline period may be required to quantify the relationship.
According to the package inserts for aducanumab and lecanemab-irmb, treatment should be initiated in patients with MCI or at the mild dementia stage of disease [14, 15]. With the availability of new treatments and screening tools for mild and early-stage ADRD, clinical guidelines will need more frequent updates that describe best practices for people with ADRD [1, 43]. Diagnosis of MCI due to AD is important to patients and their families, providing opportunities for treatment and future preparations. To have the greatest impact, predictive models should focus on identifying individuals at elevated risk for MCI.
A predictive model for MCI risk based on EHRs could include demographic characteristics (e.g., age, sex, race/ethnicity), biometric data (e.g., blood pressure, body mass index), health-related behavior (e.g., smoking status), laboratory results (e.g., lipids, HbA1c), and the presence of ADRD comorbidities and other data that are accessible in the PCP setting. The model will not include biomarkers, and thus, it will not be a diagnostic tool. However, an easily implemented screening tool for PCPs can greatly improve their ability to identify individuals at elevated risk of MCI. Alerting the PCPs of the possibility of undetected risks could provide an entry point for triage when an individual is flagged for elevated risk. Depending on the maturity of blood-based biomarkers, PCPs could use those results as part of their initial work-up and to decide whether and with what urgency to initiate specialist referrals.
One of the linchpins in the pursuit of the early detection of MCI by PCPs in age-eligible patients is the Medicare Annual Wellness Visit (AWV). Beginning in 2011, the AWV includes the detection of cognitive impairment for Medicare Part B beneficiaries [44]; however, by 2018 uptake of the AWV was still only at 32% [45]. Medicare is primarily available to people aged 65 years or over and this age group is considered the most at risk for MCI and dementia [46]. Being able to identify individuals at risk for MCI before they reach 65 years would enable physicians to treat and track them even earlier, thus potentially limiting the clinical and economic burden of the progression to ADRD.
Limitations
The results of this study must be considered in the context of several limitations. Firstly, there are those inherent to all claims data: claims data do not allow for proper assessment of potentially relevant clinical variables such as body mass index, smoking status, and the severity, rather than mere presence, of comorbid conditions. Additionally, the generalizability to populations other than the commercially and Medicare supplementally insured, also referred to as Medigap, is unknown. Data from MarketScan is sourced from employers; findings may not be generalizable to the uninsured or underinsured populations. Claims data are collected for reimbursement and not research purposes. This limitation can be addressed by future studies using EHR data, which contains a broader range of predictors and covers an “all-comers” population. An additional benefit to conducting a similar study using EHR data would be the ability to separate individuals with MCI due to AD from the general MCI population, something that was not possible in this study. As mentioned above, because of the underdiagnosis of MCI, this analysis may underestimate the true burden of MCI. The pattern of odds ratio decreasing with increased age may be partially attributed to the expectation that the highest percentage of undiagnosed MCI individuals in the non-MCI cohort is likely to be in the oldest age group. While longitudinal, our observational study design precludes the assessment of causality. Increased diagnoses related to complications as patients near an AD dementia diagnosis have been documented in the literature, which may reflect increased use of health care services as cognitive impairment worsens [47]. Studies that advance our understanding of the diagnostic process, as well as the natural history of the AD continuum, may further elucidate the relationship. In order to address these limitations, studies that compare individuals with diagnosed MCI to individuals with clinically verified normal cognition are needed. In addition, the potential temporal bias could be introduced by using a case-control study design, e.g., patients who saw a doctor more often are more likely to be diagnosed with MCI.
Conclusions
The ultimate goal of this research is to develop a triage tool to help PCPs identify those with elevated risk of MCI. The 25 ADRD comorbidities were also MCI comorbidities. The comorbidity burden of MCI is likely age-dependent. Based on routinely collected data in the PCP setting, we hope to achieve even better prediction of MCI risk for triage in primary care. This work could enable PCPs to focus on high-risk individuals to initiate further assessment and/or identification of possible MCI and improve the detection of pre-existing MCI in patients who are not voicing concerns about cognitive impairment and initiating an individualized and suitable treatment plan.
Availability of data and materials
The data that support the findings of this study are available from the Merative Corporation, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Merative.
Abbreviations
- ADRD:
-
Alzheimer’s disease and related dementia disorders
- AUC:
-
Area under the curve
- AWV:
-
Annual Wellness Visit
- BLLR:
-
Bayesian logistic lasso regression
- CCI:
-
Charlson Comorbidity Index
- CI:
-
Confidence intervals
- ECI:
-
Elixhauser Comorbidity Index
- FDA:
-
Food & Drug Administration
- EHR:
-
Electronic health records
- ICD:
-
International Classification of Disease
- IRB:
-
Institutional review board
- MCI:
-
Mild cognitive impairment
- OR:
-
Odds ratio
- PCP:
-
Primary care physicians
- Q:
-
Quartile
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation
- TIA:
-
Transient ischemic attack
- US:
-
United States
- XGBoost:
-
Extreme gradient boosting area
References
Hampel H, Au R, Mattke S, Van Der Flier WM, Aisen P, Apostolova L, et al. Designing the next-generation clinical care pathway for Alzheimer’s disease. Nature Aging. 2022;2(8):692–703.
Mitchell AJ, Shiri-Feshki M. Temporal trends in the long-term risk of progression of mild cognitive impairment: a pooled analysis. J Neurol Neurosurg Psychiatry. 2008;79(12):1386–91.
Yaffe K, Petersen RC, Lindquist K, Kramer J, Miller B. Subtype of mild cognitive impairment and progression to dementia and death. Dement Geriatr Cogn Disord. 2006;22(4):312–9.
Petersen RC, Roberts RO, Knopman DS, Boeve BF, Geda YE, Ivnik RJ, et al. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66(12):1447–55.
Ward A, Tardiff S, Dye C, Arrighi HM. Rate of conversion from prodromal Alzheimer’s disease to Alzheimer’s dementia: a systematic review of the literature. Dement Geriatr Cogn Dis Extra. 2013;3(1):320–32.
Petersen RC, Lopez O, Armstrong MJ, Getchius TSD, Ganguli M, Gloss D, et al. Practice guideline update summary: mild cognitive impairment. Neurol. 2018;90(3):126–35.
Borson S, Scanlan JM, Watanabe J, Tu S-P, Lessig M. Improving identification of cognitive impairment in primary care. Int J Geriatr Psychiatry. 2006;21(4):349–55.
Savva GM, Arthur A. Who has undiagnosed dementia? A cross-sectional analysis of participants of the aging, demographics and memory study. Age Ageing. 2015;44(4):642–7.
Judge D, Roberts J, Khandker R, Ambegaonkar B, Black CM. Physician perceptions about the barriers to prompt diagnosis of mild cognitive impairment and Alzheimer’s disease. Int J Alzheimers Dis. 2019;2019:3637954.
Sabbagh MN, Boada M, Borson S, Doraiswamy PM, Dubois B, Ingram J, et al. Early detection of mild cognitive impairment (MCI) in an at-home setting. J Prev Alzheimers Dis. 2020;7(3):171–8.
Sabbagh MN, Boada M, Borson S, Chilukuri M, Doraiswamy PM, Dubois B, et al. Rationale for early diagnosis of mild cognitive impairment (MCI) supported by emerging digital technologies. J Prev Alzheimers Dis. 2020;7(3):158–64.
Hampel H, Lista S. Dementia: the rising global tide of cognitive impairment. Nat Rev Neurol. 2016;12(3):131–2.
Galvin JE. Screening for mild cognitive impairment: there is the will but is there a way? J Prev Alzheimer's Dis . 2020;7(3):144–5. https://doi.org/10.14283/jpad.2020.16.
Leqembi (lecanemab-irmb) injection. Prescribing information. Eisai Inc. and Biogen; 2023. Accessed 3 May 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/761269s000lbl.pdf.
Aduhelm (aducanumab-avwa) injection. Prescribing information. Biogen and Eisai, Inc; 2021. Accessed 3 May 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761178s000lbl.pdf.
Cummings J, Lee G, Nahed P, Kambar M, Zhong K, Fonseca J, et al. Alzheimer’s disease drug development pipeline: 2022. Alzheimers Dement (N Y). 2022;8(1):e12295.
Tjandra D, Migrino RQ, Giordani B, Wiens J. Cohort discovery and risk stratification for Alzheimer’s disease: an electronic health record-based approach. Alzheimers Dement (N Y). 2020;6(1):e12035.
Ben Miled Z, Haas K, Black CM, Khandker RK, Chandrasekaran V, Lipton R, et al. Predicting dementia with routine care EMR data. Artif Intell Med. 2020;102:101771.
de Bruijn RFAG, Bos MJ, Portegies MLP, Hofman A, Franco OH, Koudstaal PJ, et al. The potential for prevention of dementia across two decades: the prospective, population-based Rotterdam study. BMC Med. 2015;13(1):132.
Liang Y, Ngandu T, Laatikainen T, Soininen H, Tuomilehto J, Kivipelto M, et al. Cardiovascular health metrics from mid- to late-life and risk of dementia: a population-based cohort study in Finland. PLoS Med. 2020;17(12):e1003474.
Marra DE, Miller AH, Li Q, Yang X, Smith GE, Wu Y, et al. Utilizing electronic medical record data to predict onset of Alzheimer’s disease and related dementias. Alzheimers Dement. 2020;16(S10):e041233.
Boustani M, Perkins AJ, Khandker RK, Duong S, Dexter PR, Lipton R, et al. Passive digital signature for early identification of Alzheimer’s disease and related dementia. J Am Geriatr Soc. 2020;68(3):511–8.
Barnes DE, Zhou J, Walker RL, Larson EB, Lee SJ, Boscardin WJ, et al. Development and validation of eRADAR: a tool using EHR data to detect unrecognized dementia. J Am Geriatr Soc. 2020;68(1):103–11.
Li Q, Yang X, Xu J, Guo Y, He X, Hu H, et al. Early prediction of Alzheimer’s disease and related dementias using real-world electronic health records. Alzheimer's Dement. 2023:19:3506–18. https://doi.org/10.1002/alz.12967.
Nori VS, Hane CA, Crown WH, Au R, Burke WJ, Sanghavi DM, et al. Machine learning models to predict onset of dementia: a label learning approach. Alzheimers Dement: TRCI. 2019;5(1):918–25.
Albrecht JS, Hanna M, Kim D, Perfetto EM. Predicting diagnosis of Alzheimer’s disease and related dementias using administrative claims. J Manag Care Spec Pharm. 2018;24(11):1138–45.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Tjandra D, Migrino RQ, Giordani B, Wiens J. Use of blood pressure measurements extracted from the electronic health record in predicting Alzheimer’s disease: a retrospective cohort study at two medical centers. Alzheimers Dement. 2022;18(11):2368–72.
Rabinovici GD, Carrillo MC, Hillner BE, Siegel BA, Dilworth-Anderson P, Whitmer RA, et al. New IDEAS: imaging dementia—evidence for amyloid scanning study. ClinicalTrials.gov identifier: NCT02420756 2021 [updated August 2, 2021] Available from: https://www.ideas-study.org/-/media/Ideas/Files/New-IDEAS-Study-Protocol.pdf. Accessed 27 Jan 2023.
Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, et al. Dementia prevention, intervention, and care. Lancet. 2017;390(10113):2673–734.
Tang Z, Shen Y, Zhang X, Yi N. The spike-and-slab lasso generalized linear models for prediction and associated genes detection. Genetics. 2017;205(1):77–88.
Shi L, Campbell G, Jones WD, Campagne F, Wen Z, et al. The MicroArray Quality Control (MAQC)-II study of common practices for the development and validation of microarray-based predictive models. Nature Biotech. 2010;28(8):827–38.
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez J-C, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 2011;12(1):77.
R Software. 2022 [Available from: https://www.r-project.org/].
Edson EJ, Sierra-Johnson J, Curtis B. Diabetes and obesity in older adults: a call to action. Rev Clin Gerontol. 2009;19(2):135–47.
Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circ J. 2023;147(8):e93–621.
Bechtold M, Palmer J, Valtos J, Iasiello C, Sowers J. Metabolic syndrome in the elderly. Curr Diab Rep. 2006;6(1):64–71.
Swan GE, DeCarli C, Miller BL, Reed T, Wolf PA, Jack LM, et al. Association of midlife blood pressure to late-life cognitive decline and brain morphology. Neurol. 1998;51(4):986–93.
Daugherty AM. Hypertension-related risk for dementia: a summary review with future directions. Semin Cell Dev Biol. 2021;116:82–9.
Walker KA, Sharrett AR, Wu A, Schneider ALC, Albert M, Lutsey PL, et al. Association of midlife to late-life blood pressure patterns with incident dementia. JAMA. 2019;322(6):535–45.
Blue Cross Blue Shield. Major depression: The impact on overall health. 2018. Last access on December 2, 2023 at: https://www.bcbs.com/the-health-of-america/reports/major-depression-the-impact-overall-health#:~:text=The%20Impact%20of%20Major%20Depression%20on%20Overall%20Health&text=The%20overall%20health%20of%20people,(see%20Exhibit%201)6.
Zilkens RR, Davis WA, Spilsbury K, Semmens JB, Bruce DG. Earlier age of dementia onset and shorter survival times in dementia patients with diabetes. Am J Epidemiol. 2013;177(11):1246–54.
Tahami Monfared AA, Phan NTN, Pearson I, Mauskopf J, Cho M, Zhang Q, et al. A systematic review of clinical practice guidelines for Alzheimer’s disease and strategies for future advancements. Neurol Therapy. 2023.
Thunell JA, Jacobson M, Joe EB, Zissimopoulos JM. Medicare’s Annual Wellness Visit and diagnoses of dementias and cognitive impairment. Alzheimers Dement: DADM. 2022;14(1):e12357.
Jacobson M, Thunell J, Zissimopoulos J. Cognitive assessment at Medicare’s annual wellness visit in fee-for-service and Medicare advantage plans. Health Aff (Millwood). 2020;39(11):1935–42.
2020 Alzheimer’s disease facts and figures. Alzheimers Dement. 2020;16(3):391-460. https://doi.org/10.1002/alz.12068. Accessed 1 Sept 2023.
Abbass IM, Choi D, Wallick C, Assunção SS. Trends in healthcare resource use preceding diagnosis of Alzheimer’s disease dementia. Int J Alzheimers Dis. 2023;2023:8154701.
Acknowledgements
The authors would like to acknowledge the contributions of Timothy Juday of Eisai, Inc., and Yingjie Ding of Genesis Research for their helpful discussions. Kristen Downs of Genesis Research provided medical writing and editorial assistance. The authors would like to thank two anonymous reviewers for constructive comments that greatly improved the clarity of the presentation.
Funding
This study was funded by Eisai Inc.
Author information
Authors and Affiliations
Contributions
G.L. made substantial contributions to the conception and design of the work; was involved in the acquisition, analysis, and interpretation of the patient data; was involved in the software programming for the analysis; and was a major contributor in writing the manuscript. N.T. was involved in the interpretation of the patient data, was involved in the software programming for the analysis, and was a major contributor in writing the manuscript. V.D. was involved in the acquisition, analysis, and interpretation of the patient data; was involved in the software programming for the analysis; and was a major contributor in writing the manuscript. R.B. was involved in the interpretation of the patient data and was a major contributor in writing the manuscript. T.B. and M.F. were involved in the acquisition, analysis, and interpretation of the patient data and were involved in the software programming for the analysis. M.C. and F.F. were involved in the acquisition, analysis, and interpretation of the patient data and were major contributors in writing the manuscript. J.E.G. made substantial contributions to the conception and design of the work; was involved in the acquisition, analysis, and interpretation of the patient data; and was a major contributor in writing the manuscript. D.H. was involved in the acquisition, analysis, and interpretation of the patient data and was a major contributor in writing the manuscript. S.M., S.D, and H.H. made substantial contributions to the conception and design of the work; were involved in the acquisition, analysis, and interpretation of the patient data; and were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
As the study did not constitute human subjects research per US federal regulations (45 CFR 46, 102(f))20, it was exempt from institutional review board (IRB) review, consent requirements, and registration.
Consent for publication
This study involved analyses of MarketScan Commercial and Medicare Databases; thus, no informed consent was feasible or necessary.
Competing interests
G.L. is an employee of Eisai Inc. N.T. has no declarations of interest. V.D. is an employee of Eisai Inc. R.B. is an employee of Eisai Inc. T.B. has no declarations of interest. M.C. is an employee of Eisai Inc. M.F. has no declarations of interest. F.F. is an employee of Eisai Inc. J.E.G. has provided consultation to Alpha Cognition, Biogen, Cognition Therapeutics, CND Life Sciences, EIP Pharma, Eisai, Eli Lilly, GE Healthcare, Genentech, Otsuka, and Roche. J.G. is the Chief Scientific Officer for Cognivue. J.E.G. is the creator of the Quick Dementia Rating System and holds copyright with the New York University Grossman School of Medicine. J.E.G. is supported by NIA grants R01AG071514, R01AG701514S1, R56AG074889, R01AG071643, R01AG069765, R01AG057681, P01AG066584, and P30AG059295; NINDS grants R01NS101483 and R01NS101483S1. D.H. is an employee of Janssen R&D and a shareholder in Johnson and Johnson. S.M. serves on the board of directors of Senscio Systems, Inc., and the scientific advisory board of AiCure Technologies, Alzpath, and Boston Millennia Partners. S.M. has received consulting and speaker fees from Biogen, C2N, Eisai, Novartis, Novo Nordisk and Roche/Genentech. S.D. is an employee of Eisai Inc. H.H. is an employee of Eisai and serves as reviewing editor for the Journal Alzheimer’s & Dementia. H.H. is inventor of 11 patents and has received no royalties for: In Vitro Multiparameter Determination Method for The Diagnosis and Early Diagnosis of Neurodegenerative Disorders patent no. 8916388; In Vitro Procedure for Diagnosis and Early Diagnosis of Neurodegenerative Diseases patent no. 8298784; Neurodegenerative Markers for Psychiatric Conditions publication no. 20120196300; In Vitro Multiparameter Determination Method for The Diagnosis and Early Diagnosis of Neurodegenerative Disorders publication no. 20100062463; In Vitro Method for The Diagnosis and Early Diagnosis of Neurodegenerative Disorders publication no. 20100035286; In Vitro Procedure for Diagnosis and Early Diagnosis of Neurodegenerative Diseases publication no. 20090263822; In Vitro Method for The Diagnosis of Neurodegenerative Diseases patent no. 7547553; CSF Diagnostic in Vitro Method for Diagnosis of Dementias and Neuroinflammatory Diseases publication no. 20080206797; In Vitro Method for The Diagnosis of Neurodegenerative Diseases publication no. 20080199966; Neurodegenerative Markers for Psychiatric Conditions publication no. 20080131921; Method for diagnosis of dementias and neuroinflammatory diseases based on an increased level of procalcitonin in cerebrospinal fluid: US patent no. 10921330.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplemental Table. ICD-9 and ICD-10 Codes for Identifying ADRD Comorbidities.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, G., Toschi, N., Devanarayan, V. et al. The age-specific comorbidity burden of mild cognitive impairment: a US claims database study. Alz Res Therapy 15, 211 (2023). https://doi.org/10.1186/s13195-023-01358-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-023-01358-8