Abstract
Background
Cardiovascular factors and low education are important risk factors of dementia. We provide contemporary estimates of the proportion of dementia cases that could be prevented if modifiable risk factors were eliminated, i.e., population attributable risk (PAR). Furthermore, we studied whether the PAR has changed across the last two decades.
Methods
We included 7,003 participants of the original cohort (starting in 1990) and 2,953 participants of the extended cohort (starting in 2000) of the Rotterdam Study. Both cohorts were followed for dementia until ten years after baseline. We calculated the PAR of overweight, hypertension, diabetes mellitus, cholesterol, smoking, and education. Additionally, we assessed the PAR of stroke, coronary heart disease, heart failure, and atrial fibrillation. We calculated the PAR for each risk factor separately and the combined PAR taking into account the interaction of risk factors.
Results
During 57,996 person-years, 624 participants of the original cohort developed dementia, and during 26,177 person-years, 145 participants of the extended cohort developed dementia. The combined PAR in the original cohort was 0.23 (95 % CI, 0.05–0.62). The PAR in the extended cohort was slightly higher at 0.30 (95 % CI, 0.06–0.76). The combined PAR including cardiovascular diseases was 0.25 (95 % CI, 0.07–0.62) in the original cohort and 0.33 (95 % CI, 0.07–0.77) in the extended cohort.
Conclusions
A substantial part of dementia cases could be prevented if modifiable risk factors would be eliminated. Although prevention and treatment options of cardiovascular risk factors and diseases have improved, the preventive potential for dementia has not declined over the last two decades.
Similar content being viewed by others
Background
In recent years, it has become clear that cardiovascular factors and low education are risk factors of dementia [1–3]. As advocated by the recent World Alzheimer report [3], most of these factors are potentially modifiable, which provides an opportunity for prevention of dementia. The magnitude of this potential for prevention can be estimated via the population attributable risk (PAR) [4].
Few studies have estimated PAR for modifiable risk factors of dementia [5–10]. However, results have been inconsistent due to methodological variation. For instance, some studies estimated PAR using data from multiple different sources, which precludes proper adjustment for risk factors and only yields indirect approximations of PAR [6, 8, 10]. Nevertheless, the combined PAR of potentially modifiable risk factors of dementia has been estimated to range from 8.4–50.7 % [6–9].
At the same time, converging evidence, including from our own study, suggests that the incidence of dementia has declined over the last decades [11–15]. Presumably, this decline has been triggered by a better control of cardiovascular risk and improved education [11–15]. If this is indeed the case, it is conceivable that previously published PARs of modifiable risk factors for dementia have now become an overestimation. There is thus an urgent need for contemporary data on PAR of modifiable risk factors of dementia, because such updated knowledge can better inform public health priorities on preventive strategies against dementia. In this study, we provide direct and contemporary estimates of PAR of modifiable risk factors of dementia. Additionally, we investigate how this PAR has changed across the last two decades.
Methods
Setting and study population
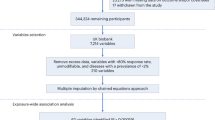
This study was embedded within the Rotterdam Study, a prospective population-based cohort study. In 1990, all residents aged 55 and older residing in Ommoord, a district of Rotterdam, the Netherlands, were invited. Of the 10,215 invited inhabitants, 7,983 agreed to participate in the baseline examinations. In 2000, the cohort was extended: again all residents aged 55 and older of the same district were invited, except for the participants that were already participating in the original cohort. Of the 4,472 invitees, 3,011 agreed to participate. Follow-up examinations take place every 3 to 4 years [16].
From the original cohort, we excluded 455 participants because they were not properly screened for dementia, 482 participants because they had prevalent dementia, and 43 participants for lack of follow-up information on the dementia diagnosis. Finally, 7,003 participants were included in the analyses. In the extended cohort, we excluded 29 participants because they had prevalent dementia and 29 for lack of follow-up information on the dementia diagnosis. Finally, 2,953 participants were included in the analysis. Even though a part of the original cohort still participated in 2000, those participants were only included in the original, and not in the extended cohort. We aimed to avoid overlapping individuals, since such a correlation would limit the assessment of cohort effects.
The Rotterdam Study has been approved by the medical ethics committee according to the Population Study Act Rotterdam Study and written informed consent was obtained.
Selection and measurement of risk factors
Potentially causal and modifiable risk factors for dementia were chosen on the basis of previous literature [1–3]. The following risk factors were selected: overweight and obesity, hypertension, diabetes mellitus, unfavorable cholesterol levels, smoking, and low educational level.
All risk factors were measured at baseline. Weight and height were measured at the research center visit and body mass index (BMI) was calculated as weight in kilograms divided by length in meters squared. BMI was categorized into four categories: underweight (<18.5), normal weight (18.5–25), overweight (25–30), and obesity (>30). Blood pressure was measured in sitting position on the right arm and calculated as the average of two measurements using a random-zero sphygmomanometer. Hypertension was defined as a blood pressure ≥140/90 mmHg or use of blood pressure lowering medication, prescribed for the indication of hypertension. Diabetes mellitus was defined as a fasting serum glucose level ≥7.0 mmol/L, non-fasting serum glucose level ≥11.1 mmol/L, or use of anti-diabetic medication. Serum glucose, total cholesterol, and high-density lipoprotein (HDL)-cholesterol levels were acquired by an automated enzymatic procedure (Boehringer Mannheim System). Medication use, educational level, and smoking habits were assessed by interview. For people not taking lipid-lowering medication, total cholesterol/HDL-cholesterol ratio was divided in quartiles using the lowest category as the reference category. People using lipid-lowering medication were added as the fifth category and also compared to the reference category. Educational level was categorized as low (primary education or lower vocational education), intermediate (secondary education or intermediate vocational education), and high educational level (higher vocational education or university). Smoking habits were categorized as current, former, and never smoking.
Although stroke, coronary heart disease, heart failure, and atrial fibrillation are cardiovascular diseases that may result from cardiovascular risk factors and can be modified only via secondary prevention, several studies have shown that these diseases are related to dementia or cognitive impairment, independently of cardiovascular risk factors [17–20]. We therefore assessed the PAR of these factors in an additional analysis. A history of stroke, coronary heart disease (myocardial infarction or revascularization procedure), heart failure, and atrial fibrillation was evaluated using home interviews and confirmed by reviewing medical records [21, 22].
Assessment of dementia
Participants were screened for dementia at baseline and at follow-up examinations using a three-step protocol [11]. Screening was done using the Mini-Mental State Examination (MMSE) and the Geriatric Mental Schedule (GMS) organic level. Screen-positives (MMSE <26 or GMS organic level >0) subsequently underwent an examination and informant interview with the Cambridge Examination for Mental Disorders in the Elderly [11]. Participants who were suspected of having dementia underwent extra neuropsychological testing if necessary. Additionally, for persons not visiting the research center, the total cohort was continuously monitored for dementia through computerized linkage of the study database and digitized medical records from general practitioners and the Regional Institute for Outpatient Mental Health Care. When information on neuroimaging was required and available, it was used for decision making on the diagnosis. Ultimately, a consensus panel, led by a neurologist, decided on the final diagnosis in accordance with standard criteria for dementia (DSM-III-R) [11]. Both the original and the extended cohort were followed for dementia until 10 years after baseline examinations: until 2000–2003 for the original cohort and until 2010–2012 for the extended cohort. Follow-up for dementia was complete for 99.5 % of potential person-years in the original cohort and for 98.5 % of potential person-years in the extended cohort.
Statistical analyses
We imputed missing data on the investigated risk factors (3.3 % in the original cohort and 6.7 % in the extended cohort) using the mean of five imputations. Missing data were imputed on age, sex, and all other investigated risk factors. Differences between the original and the extended cohort were calculated using logistic regression models, adjusting for age and sex where appropriate. Analyses were performed using statistical software package SPSS 20.0.
We calculated PARs and corresponding 95 % confidence intervals (CIs) using the Interactive Risk Attributable Program (US National Cancer Institute) [23]. This metric is also referred to as population attributable fraction, or PAR%. We provide logit transformed 95 % CIs accompanying the PARs as these are better interpretable and more stringent with regard to our combined PAR estimates [24]. The PAR was estimated and adjusted for confounding factors according to the following formulae:
where
and
with D = 1 denoting presence of disease, X denoting exposure with i levels, and C denoting a confounder with j levels. Participants were censored at date of dementia, date of death, or last date of follow-up, whichever came first. The relative risk was estimated from a multivariable Poisson model [23]. First, we calculated the PAR for overweight and obesity, hypertension, diabetes mellitus, unfavorable cholesterol levels, smoking, and low educational level. Second, we calculated the PAR of stroke, coronary heart disease, heart failure, and atrial fibrillation. We calculated the PAR for each risk factor separately as well as the combined PAR per cohort. Many risk factors have a coinciding effect on the etiology of dementia. Therefore, the combined PAR cannot be estimated by the sum of the separate PARs as this would lead to an overestimation. The advantage of the statistical program used in this study is that it takes into account that a disease case can simultaneously be attributed to more than one risk factor. Hence, it takes into account the overlap between the PARs of each risk factor when estimating the combined PAR. The combined PAR included the PARs of modifiable risk factors which were associated to dementia in the expected direction in our study, meaning the relative risk was above one. PARs cannot be calculated using a relative risk below one as this will result in a PAR which cannot be interpreted [25].
Every PAR was adjusted for age, sex, and all other risk factors included in the model. Age was added per 5-year categories into the models. Because of a small number of people in the oldest age categories, the oldest age category of both cohorts comprised people 85 years of age and older.
Results
Baseline characteristics
Baseline characteristics of the two study populations are provided in Table 1. During a mean follow-up of 8.3 years (standard deviation (SD) 2.9), 624 participants of the original cohort developed dementia and 1,756 participants died. During a mean follow-up of 8.9 years (SD 2.3), 145 participants of the extended cohort developed dementia and 429 participants died. Cut-offs for quartiles of total cholesterol/HDL cholesterol ratio were: 4.1, 5.0, and 6.1 in the original cohort and 3.6, 4.3, and 5.2 in the extended cohort. Participants in the extended cohort were younger and had higher educational levels than those in the original cohort. Overweight and obesity, hypertension, diabetes mellitus, use of lipid-lowering medication, former smoking, and stroke were more prevalent in the extended cohort. Additionally, people had lower total cholesterol levels, higher HDL-cholesterol levels, and less heart failure and coronary heart disease in the extended cohort than in the original cohort (Table 1).
Population attributable risk (PAR)
In the original cohort, smoking (PAR, 0.07; 95 % CI, 0.02–0.23) and lower educational level (PAR, 0.07; 95 % CI, 0.00–0.90) had the largest PARs, followed by diabetes mellitus (PAR, 0.04; 95 % CI, 0.01–0.09), hypertension (PAR, 0.04; 95 % CI, 0.00–0.44) and higher total cholesterol/HDL cholesterol ratio (PAR, 0.03; 95 % CI, 0.00–0.73). Overweight and obesity were not related to dementia in the expected direction. The combined PAR in the original cohort was 0.23 (95 % CI, 0.05–0.62; Table 2).
In the extended cohort, hypertension (PAR, 0.16; 95 % CI, 0.02–0.62), lower educational level (PAR, 0.12; 95 % CI, 0.00–0.89), and diabetes mellitus (PAR, 0.06; 95 % CI, 0.02–0.19) had the largest PARs. Overweight and obesity, higher total cholesterol/HDL-cholesterol ratio, and smoking were not related to dementia in the expected direction. The combined PAR in the extended cohort was 0.30 (95 % CI, 0.06–0.76; Table 2).
When cardiovascular diseases were included into the model, the combined PAR was 0.25 (95 % CI, 0.07–0.62) in the original cohort and 0.33 (95 % CI, 0.07–0.77) in the extended cohort. Atrial fibrillation and stroke had the largest PARs in the original cohort, whereas coronary heart disease and stroke had the largest PARs in the extended cohort (Table 3).
Discussion
Within the population-based Rotterdam Study, we found that about one quarter to one third of dementia cases could potentially be prevented through optimal prevention or treatment of cardiovascular risk factors and diseases and improvement of educational level. This proportion has not declined between the original cohort of 1990–2000 and the extended cohort of 2000–2010, although we did observe a shift in the relative importance of individual factors.
Before these results can be interpreted, some methodological issues need to be mentioned. The strengths of the present study are the prospective, population-based design and almost complete dementia case finding. Additionally, information on a relatively wide range of risk factors was assessed, allowing the calculation of PARs on various potentially modifiable risk factors. Furthermore, a statistical approach, which takes into account the interaction between risk factors when estimating the combined PAR, was used.
We recognize that our study also has limitations. PAR calculations should always be interpreted with caution as they rely on assumptions which may be improbable in practice [26, 27]. For instance, the model assumes that a risk factor can be successfully treated in every person and that removing one risk factor would not induce changes in the other factors, which is unlikely. Furthermore, PAR calculations assume that, when a risk factor is successfully treated, the harming effect of the risk factor completely disappears, which too is unlikely as risk factors might have already caused irreversible damage before treatment is started. Moreover, if we prevent a dementia case caused by these cardiovascular risk factors, this person might still suffer from dementia caused by other factors. Therefore, the proportion that can actually be prevented in practice might be lower than suggested by the PAR [26, 27]. We selected potentially causal and modifiable risk factors of dementia based on previous literature [1–3]. However, it should be noticed that, within this study, this causal relationship could not be established. In particular, findings related to cardiovascular diseases should be interpreted with caution as these may have an association with dementia through shared risk factors. Paradoxically, treatment might even increase the occurrence of dementia, if the people that are treated live longer.
In our study, we did not find many statistically significant associations between these risk factors and the risk of dementia. This might have various explanations. First, dementia is a multifactorial disease and the effect of a single risk factor can therefore be relatively small and non-significant. However, the preventive potential of all risk factors combined can still be substantial. Second, the sample size was limited, which might have prevented the finding of statistically significant results because of low power and because smaller subgroups for the risk factors, such as untreated and treated hypertension, could not be formed. Third, baseline risk factors were used, whereas the risk factor profile might have changed during follow-up. This may have weakened the associations. Fourth, the effect of cardiovascular risk factors might be small because of the competing risk of cardiovascular mortality. People might die due to those risk factors before dementia occurs. Fifth, it has been suggested that the effect of several cardiovascular risk factors on the risk of dementia changes with increasing age. Studies have shown that obesity, hypertension, and high cholesterol levels were only related to an increased risk of dementia when assessed at midlife [28–30]. Since the participants in our study populations were older, we were not able to assess such midlife effects, possibly leading to an underestimation of our results. Although our data collection was extensive, we did not have information on some important modifiable risk factors, such as physical activity, dietary habits, depression, and social engagement, which might have led to an underestimation of our results. We imputed missing data on investigated risk factors, which may have introduced some misclassification. However, we hypothesized that excluding participants with missing data from our analyses would have resulted in more bias, given that missing data usually does not occur at random. A final limitation is that most participants of the Rotterdam Study are Caucasians and live in a middle-income district of Rotterdam, which limits the generalizability of our results.
We found that the PAR of modifiable risk factors of dementia was about one quarter to one third and has not declined across the last two decades. These findings have several implications. First, from a public health point of view, this suggests that despite the seemingly declining incidence of dementia, the potential for further reduction of dementia is still substantial. Second, it remains pivotal to find novel risk factors that can explain the remaining two thirds of dementia cases. Third, even though the combined PAR did not decline, we did find that the contribution of individual risk factors had changed across the two decades. For example, the PARs of hypertension and to a lesser extent of diabetes were higher in the extended cohort. Although treatment and preventive options for cardiovascular risk factors have improved over the past decades, the prevalence of various cardiovascular risk factors, such as hypertension, diabetes, and obesity has increased [31–33]. Correspondingly, we found that participants in the extended cohort had a higher prevalence of these risk factors, partly explaining the higher PARs. Conversely, we found a decline in the PARs of other cardiovascular risk factors, such as smoking and unfavorable cholesterol levels. Smoking had a large effect on the burden of dementia in the original cohort, which decreased dramatically in the extended cohort. Successful anti-smoking campaigns are an obvious explanation for these findings. A counterargument, however, is that the prevalence of current smokers was comparable between the two cohorts. The reduction of the effect of unfavorable cholesterol levels might be explained by the large increase in use of lipid-lowering medication in the extended cohort. Another interesting observation was the effect of educational level, which was higher in the extended cohort than in the original cohort. Conventionally, educational attainment is considered a reflection of cognitive reserve built up earlier in life. However, this has not always been the case in older Dutch generations, where many people were unable to achieve their educational potential due to the Second World War. This might have led to a discrepancy between educational attainment and corresponding cognitive reserve. In the original cohort of the Rotterdam Study, this phenomenon might have been more pronounced, explaining the higher prevalence but lower PAR of low educational level compared to the extended cohort.
As for cardiovascular diseases, atrial fibrillation had an effect on the burden of dementia in the original cohort, but not in the extended cohort. These results might be explained by improved prevention of ischemic stroke in patients with atrial fibrillation [34]. In contrast, we found a stronger effect of stroke and coronary heart disease in the extended cohort than in the original cohort. This might seem counter-intuitive, since preventive and treatment options for these diseases have improved in the same time-period. However, these findings could be explained by the fact that because of improved treatments, people with cardiovascular disease live longer and therefore are at an increased risk of developing dementia [35].
The combined PAR we found is very much in line with a recent report that was based on meta-analyses of studies, which mostly used data from the nineties [8]. We calculated PARs directly using original data from 1990–2000 and 2000–2010 and, more importantly, took into account interaction between risk factors. Our study therefore adds important veracity to the estimates of PAR. However, given that PAR calculations rely on theoretical assumptions, future research is necessary to observe the actual effect of risk factor improvement on the risk of dementia. Furthermore, other studies should also focus on identifying novel modifiable risk factors for dementia.
Conclusions
We found that the potential of prevention of dementia through proper control of modifiable risk factors is about one quarter to one third and has not declined over the last two decades. As this is currently one of the main options to diminish the burden of dementia, public health interventions are urgently needed.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- HDL:
-
High-density lipoprotein
- PAR:
-
Population attributable risk
- SD:
-
Standard deviation
References
Qiu C, Xu W, Fratiglioni L. Vascular and psychosocial factors in Alzheimer’s disease: epidemiological evidence toward intervention. J Alzheimers Dis. 2010;20:689–97.
Middleton LE, Yaffe K. Targets for the prevention of dementia. J Alzheimers Dis. 2010;20:915–24.
Alzheimer’s Disease International. World Alzheimer Report 2014. Dementia and Risk Reduction: an analysis of protective and modifiable factors. http://www.alz.co.uk/research/world-report-2014.
Rothman K, Greenland S. Modern epidemiology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1998.
Lipnicki DM, Sachdev PS, Crawford J, Reppermund S, Kochan NA, Trollor JN, et al. Risk factors for late-life cognitive decline and variation with age and sex in the Sydney Memory and Ageing Study. PLoS One. 2013;8, e65841.
Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10:819–28.
Dodge HH, Chang CC, Kamboh IM, Ganguli M. Risk of Alzheimer’s disease incidence attributable to vascular disease in the population. Alzheimers Dement. 2011;7:356–60.
Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer’s disease: an analysis of population-based data. Lancet Neurol. 2014;13:788–94.
Ritchie K, Carriere I, Ritchie CW, Berr C, Artero S, Ancelin ML. Designing prevention programmes to reduce incidence of dementia: prospective cohort study of modifiable risk factors. BMJ. 2010;341:c3885.
Kloppenborg RP, van den Berg E, Kappelle LJ, Biessels GJ. Diabetes and other vascular risk factors for dementia: which factor matters most? A systematic review. Eur J Pharmacol. 2008;585:97–108.
Schrijvers EM, Verhaaren BF, Koudstaal PJ, Hofman A, Ikram MA, Breteler MM. Is dementia incidence declining? Trends in dementia incidence since 1990 in the Rotterdam Study. Neurology. 2012;78:1456–63.
Qiu C, von Strauss E, Backman L, Winblad B, Fratiglioni L. Twenty-year changes in dementia occurrence suggest decreasing incidence in central Stockholm, Sweden. Neurology. 2013;80:1888–94.
Matthews FE, Arthur A, Barnes LE, Bond J, Jagger C, Robinson L, et al. A two-decade comparison of prevalence of dementia in individuals aged 65 years and older from three geographical areas of England: results of the Cognitive Function and Ageing Study I and II. Lancet. 2013;382:1405–12.
Lobo A, Saz P, Marcos G, Dia JL, De-la-Camara C, Ventura T, et al. Prevalence of dementia in a southern European population in two different time periods: the ZARADEMP Project. Acta Psychiatr Scand. 2007;116:299–307.
Langa KM, Larson EB, Karlawish JH, Cutler DM, Kabeto MU, Kim SY, et al. Trends in the prevalence and mortality of cognitive impairment in the United States: is there evidence of a compression of cognitive morbidity? Alzheimers Dement. 2008;4:134–44.
Hofman A, Darwish Murad S, van Duijn CM, Franco OH, Goedegebure A, Ikram MA, et al. The Rotterdam Study: 2014 objectives and design update. Eur J Epidemiol. 2013;28:889–926.
Savva GM, Stephan BC, Alzheimer’s Society Vascular Dementia Systematic Review Group. Epidemiological studies of the effect of stroke on incident dementia: a systematic review. Stroke. 2010;41:e41–6.
Roberts RO, Knopman DS, Geda YE, Cha RH, Roger VL, Petersen RC. Coronary heart disease is associated with non-amnestic mild cognitive impairment. Neurobiol Aging. 2010;31:1894–902.
Qiu C, Winblad B, Marengoni A, Klarin I, Fastbom J, Fratiglioni L. Heart failure and risk of dementia and Alzheimer disease: a population-based cohort study. Arch Intern Med. 2006;166:1003–8.
Dublin S, Anderson ML, Haneuse SJ, Heckbert SR, Crane PK, Breitner JC, et al. Atrial fibrillation and risk of dementia: a prospective cohort study. J Am Geriatr Soc. 2011;59:1369–75.
Wieberdink RG, Ikram MA, Hofman A, Koudstaal PJ, Breteler MM. Trends in stroke incidence rates and stroke risk factors in Rotterdam, the Netherlands from 1990 to 2008. Eur J Epidemiol. 2012;27:287–95.
Leening MJ, Kavousi M, Heeringa J, van Rooij FJ, Verkroost-van Heemst J, Deckers JW, et al. Methods of data collection and definitions of cardiac outcomes in the Rotterdam Study. Eur J Epidemiol. 2012;27:173–85.
Interactive Risk Attributable Program, version 2.2. http://dceg.cancer.gov/tools/risk-assessment/irap. Date last accessed: May 28, 2014.
Leung HM, Kupper LL. Comparisons of confidence intervals for attributable risk. Biometrics. 1981;37:293–302.
Benichou J. Biostatistics and epidemiology: measuring the risk attributable to an environmental or genetic factor. C R Biol. 2007;330:281–98.
Dehghan A, van Hoek M, Sijbrands EJ, Stijnen T, Hofman A, Witteman JC. Risk of type 2 diabetes attributable to C-reactive protein and other risk factors. Diabetes Care. 2007;30:2695–9.
Bos MJ, Koudstaal PJ, Hofman A, Ikram MA. Modifiable etiological factors and the burden of stroke from the Rotterdam study: a population-based cohort study. PLoS Med. 2014;11, e1001634.
Tolppanen AM, Ngandu T, Kareholt I, Laatikainen T, Rusanen M, Soininen H, et al. Midlife and late-life body mass index and late-life dementia: results from a prospective population-based cohort. J Alzheimers Dis. 2014;38:201–9.
Qiu C, Winblad B, Fratiglioni L. The age-dependent relation of blood pressure to cognitive function and dementia. Lancet Neurol. 2005;4:487–99.
Anstey KJ, Lipnicki DM, Low LF. Cholesterol as a risk factor for dementia and cognitive decline: a systematic review of prospective studies with meta-analysis. Am J Geriatr Psychiatry. 2008;16:343–54.
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–50.
Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med. 2014;370:1514–23.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Lakshminarayan K, Solid CA, Collins AJ, Anderson DC, Herzog CA. Atrial fibrillation and stroke in the general medicare population: a 10-year perspective (1992 to 2002). Stroke. 2006;37:1969–74.
Schmidt M, Jacobsen JB, Johnsen SP, Botker HE, Sorensen HT. Eighteen-year trends in stroke mortality and the prognostic influence of comorbidity. Neurology. 2014;82:340–50.
Acknowledgements
The Rotterdam Study is supported by the following: Erasmus MC, University Medical Center and Erasmus University Rotterdam; the Netherlands Organisation of Scientific Research (NWO); the Netherlands Organisation for Health Research and Development (ZonMW); The Research Institute for Diseases in the Elderly; the Ministry of Education, Culture, and Science; the Ministry of Health, Welfare, and Sports; the European Commission (DG-XII); and the Municipality of Rotterdam. Grants include NWO ZonMW 916.13.054; Netherlands Heart Foundation 2012 T008; MRACE grant from the Erasmus MC, and Internationale Stichting Alzheimer Onderzoek (grant number #12533). Further support was obtained from the Netherlands Consortium for Healthy Ageing (NCHA); and by a grant from the NWO (ZonMw) [grant 80-82500-98-10208].
AH received grants from the Netherlands Organisation for Scientific Research, the Netherlands Genomics Initiative, the Netherlands Ministry of Health and the European Commission; and remuneration as editor of the European Journal of Epidemiology. OF works in ErasmusAGE, a center for ageing research across the life course funded by Nestlé Nutrition (Nestec Ltd.), Metagenics Inc., and AXA. Nestlé Nutrition (Nestec Ltd.), Metagenics Inc., and AXA had no role in design and conduct of the study and preparation, review or approval of the manuscript. PJK received royalties for two textbooks of neurology, Reed Elsevier, the Netherlands. MAI received grants from the Netherlands Heart Foundation (2009B102 and 2012 T008), Netherlands Organization for Health Research and Development (ZonMW: 916.13.054), Internationaal Parkinson Fonds, and Internationale Stichting Alzheimer Onderzoek (#12533).
None of the funding organizations or sponsors were involved in the design and conduct of the study, collection, management, analysis and interpretation of the data, or preparation, review or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors have made substantial intellectual contributions to conception and design (RdB, MB, AH, OF, PJK, MAI), acquisition of data (RdB, MB), analysis and interpretation of data (RdB, MB, MP, AH, OF, PJK, MAI), drafting the article or revising it critically for important intellectual content (RdB, MB, MP, AH, OF, PJK, MAI), gave final approval of the version to be published (RdB, MB, MP, AH, OF, PJK, MAI), and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved (RdB, MB, MP, AH, OF, PJK, MAI). All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
de Bruijn, R.F., Bos, M.J., Portegies, M.L. et al. The potential for prevention of dementia across two decades: the prospective, population-based Rotterdam Study. BMC Med 13, 132 (2015). https://doi.org/10.1186/s12916-015-0377-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-015-0377-5