Abstract
Coronary heart disease (CHD) is a type of cardiovascular disease (CVD) that affects the coronary arteries, which provide oxygenated blood to the heart. It is a major cause of mortality worldwide. Various prediction methods have been developed to assess the likelihood of developing CHD, including those based on clinical features and genetic variation. Recent epigenome-wide studies have identified DNA methylation signatures associated with the development of CHD, indicating that DNA methylation may play a role in predicting future CHD. This narrative review summarises recent findings from DNA methylation studies of incident CHD (iCHD) events from epigenome-wide association studies (EWASs). The results suggest that DNA methylation signatures may identify new mechanisms involved in CHD progression and could prove a useful adjunct for the prediction of future CHD.
Similar content being viewed by others
Background
Coronary heart disease (CHD) is the most common cardiovascular disease (CVD) and a leading cause of death worldwide, with an estimated 8.88 million deaths from CHD in 2019 globally [1]. Atherosclerosis, a long-term inflammatory process in the arteries, is the common basis for CHD [2]. Atherosclerosis leads to the build-up of atherosclerotic plaques, and involves lipid deposition, inflammatory cells migration, smooth muscle cell proliferation and fibrosis. Eventually, the formation of an advanced atherosclerotic plaque narrows the artery, causing blood clots at the site of the lesion. Alternatively, the plaque may rupture and lead to blood clots in downstream arteries. CHD takes place when blood flow in coronary arteries is reduced or blocked due to the impact of atherosclerosis. The outcomes of CHD can be classified according to the severity of blockage of the vessel, from mild outcomes such as stable angina to severe acute coronary syndrome. The former is caused by a temporary insufficiency of blood flow supplying the heart during physical activity or stress. The latter refers to a sudden occurrence of more severe forms of coronary heart events which happen at rest, for example, in unstable angina and in myocardial infarction (MI), caused by complete blockage of coronary arteries.
The development of CHD is a long-term process, and certain risk factors can accelerate or worsen coronary atheroma development and the chance of a severe CHD event. Risk factors considered here include lifestyle factors and phenotypes that have a causal relationship with the increased risk of developing CHD. Acknowledged risk factors for CHD include smoking, hypertension, type 2 diabetes, and hyperlipidaemia, which corresponds to elevated levels of triglycerides (TG) and low-density lipoprotein (LDL) cholesterol, or low levels of high-density lipoprotein (HDL) cholesterol. Other risk factors also include high levels of C-reactive protein (CRP), lipoprotein-A, haemoglobin A1c (HbA1c), obesity, family history of CHD, and others [3]. Assessment of risk factors can be used to identify asymptomatic individuals at increased risk of CHD, especially in primary health care settings, and this in turn can lead to different levels of interventions. For low- and moderate-risk individuals, interventions are normally lifestyle modifications, while for high-risk individuals pharmacological intervention may be necessary. To reduce the risk of severe outcomes, individuals with high cardiovascular risk, or mild CHD symptoms, or high-risk coronary atherosclerosis conditions diagnosed by direct plaque imaging often receive medical treatment to slow down the formation of atherosclerotic plaques. However, a large number of asymptomatic individuals with a potential risk of developing a future CHD event remain undiagnosed in primary care settings [4].
In recent years, genome-wide association studies (GWASs) of CHD have also identified genetic risk factors. So far, over 150 single nucleotide polymorphisms (SNPs) have been identified to associate with CHD [5]. These include loci located in genes related to lipid metabolism, inflammation, transcriptional regulation, blood pressure, cell proliferation, neovascularization angiogenesis, NO-signalling, and vascular remodelling [5]. However, signals emerging from GWASs of CHD explain less than 10% of the heritability of CHD [6], prompting investigation into effects that may contribute to the ‘missing heritability’ in CHD [7].
Considering that CHD results in high mortality, it is crucial to develop accurate predictors for future CHD events, such as acute coronary syndrome, to enable early and effective interventions. At present, risk assessment of CHD events and other atherosclerosis-based cardiovascular events primarily relies on the use of different types of validated cardiovascular risk scores, for example the Framingham Risk Score, originally proposed over two decades ago [8]. Currently recommended risk scores include the SCORE risk prediction algorithms in Europe [9, 10], the QRISK risk prediction algorithms in the UK [11,12,13], and the pooled cohort equation atherosclerotic cardiovascular disease (ASCVD) risk score in the US [14]. These predict the risk of a 10-year first cardiovascular event, including CHD events. However, cardiovascular risk scores can also have limitations, for example, the ASCVD risk score can over- or under-estimate the risk of developing ASCVD in external samples [14,15,16]. These risk scores also do not consider further CHD risk factors, for example, genetic variants associated with the development of CVD.
Several studies have aimed to incorporate genotype information, often as a polygenic risk score (PRS) for CVD, into conventional CVD risk scores aiming to predict future or incident CHD (iCHD) events [17,18,19,20]. The majority of these integrated approaches do not report an improved discriminative capacity over use of conventional risk functions alone. However, most studies observe an improved reclassification of individuals in risk categories after PRS inclusion. At present, the clinical utility of integrating genetic information into conventional CVD risk prediction is under discussion. Current guidelines do not yet recommend the use of PRS in clinical practice to improve risk stratification [21].
These findings suggest that genetic variation may not significantly increase the performance of prediction in CHD, even though disease-associated genetic variants offer insights into the underlying biological mechanisms of disease. The relationship between genetic variation and disease may be mediated by epigenetic mechanisms. Epigenetic mechanisms are key regulators of gene function that can change in response to internal and external stimuli, including risk factors for CHD such as smoking [22]. Therefore, predictors of iCHD may benefit from considering additional layers of information, such as epigenetic variation.
Epigenetic mechanisms regulate gene expression and include DNA methylation, histone modification, RNA-associated silencing, and others. Among these, DNA methylation is the most studied epigenetic mark partly due to the development of multiple approaches to assay it including micro-arrays and bisulfite sequencing, as well as due to its relative stability allowing for profiling of previously collected stored DNA samples. Similar to GWAS, the association between phenotype and DNA methylation changes across the genome is assessed through epigenome-wide association studies (EWASs). Multiple EWASs have linked DNA methylation changes in certain 5′-cytosine-phosphate-guanine-3′ dinucleotides (CpGs) to CHD events. The majority of EWAS of CHD to date have considered retrospective CHD events at a single time-point, that is, in cross-sectional studies without longitudinal follow-up [23, 24]. Most studies have applied the Infinium HumanMethylation450 BeadChip (450k array) to explore blood DNA methylation variation at > 450,000 CpG-sites in primarily gene-centric regions across the human genome. However, unlike GWAS, CHD-associated DNA methylation changes may not be necessarily causal to CHD, but they may also be consequences of previous CHD events. To assess if epigenetic changes at individual CpG sites may help with the prediction of CHD, EWASs of iCHD and CHD risk factors are needed. Recently several EWAS of iCHD have been carried out, along with multiple EWAS of CHD risk factors. This narrative review explores DNA methylation signatures of iCHD, with a focus on EWAS findings from large-scale studies, to explore the potential of utilizing DNA methylation information for the risk assessment of iCHD, as well as to improve our understanding of how DNA methylation changes may contribute to iCHD.
Epigenome-wide findings for iCHD
Several studies have assessed the association between iCHD and DNA methylation levels in the genome. Initial studies explored changes in global levels of DNA methylation in iCHD. Global DNA methylation levels can be assessed by using the methylation level of the repetitive long interspersed nuclear element-1 (LINE-1) as a proxy. Two studies have associated LINE-1 hypomethylation in blood with iCHD [25, 26]. Global DNA methylation levels have also been explored by using the DNA methylation level of the ALU and Satellite 2 (AS) repetitive element as a proxy. In contrast to the hypomethylation findings with LINE-1, Kim et al. [27] found that AS methylation in peripheral blood leukocytes was higher (hypermethylated) in males with iCHD. Overall, the relationship between iCHD and global DNA methylation levels shows contradictory results, as discussed by Fernández-Sanlés and colleagues [28] in a systematic review. Therefore, further studies are needed at greater DNA methylation resolution to assess if individual CpG-site DNA methylation levels associate with iCHD.
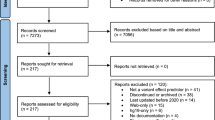
Recently several large-scale EWASs identified differential methylation signatures at specific genomic regions to be related to the development of iCHD outcomes. In all cases whole blood DNA methylation levels were profiled in healthy individuals at baseline. After a longitudinal follow-up, a subset of participants subsequently developed an iCHD event (iCHD cases). Comparison of baseline levels of DNA methylation in iCHD cases and controls identified differential methylation signals in iCHD. In this section, we focus on locus-specific results from recent large-scale EWASs of iCHD outcomes and from large-scale EWASs of CHD risk factors with iCHD follow-up.
EWASs of iCHD
Four recent large-scale EWASs have explored a range of iCHD outcomes. The most frequently studied outcome in EWASs of CHD is MI. An EWAS of incident MI was carried out by Guarrera et al. [26] using white blood cell DNA methylation profiles of 292 incident MI cases and 292 matched controls, with replication in 317 incident MI cases and 262 controls, both of European ancestry. The mean follow-up from baseline to iCHD outcome ranged between 5.64 (discovery cohort) to 6.9 years (replication cohort). The EWAS aggregated adjacent CpGs that have correlated methylation levels into 25,376 methylation regions, and identified one DNA methylation region consisting of 15 CpGs in the gene body of ZBTB12 to be significantly hypomethylated in incident MI at a genome-wide false discovery rate (FDR) < 5%, after replication. The ZBTB12 protein has a potential function in transcriptional regulation, and a recent study associated ZBTB12 gene body hypomethylation with faster blood coagulation triggered by tumour necrosis factor (TNF-α), as well as with increased white blood cell counts [29]. Guarrera et al. [26] then explored the relationship between ZBTB12 DNA methylation levels and expression levels at ZBTB12 and nearby genes in a separate sample set of approximately 80 healthy individuals, but no clear correlation was observed. The study also replicated previous findings of an iCHD association with LINE-1 DNA methylation levels as markers of global methylation. The authors next incorporated DNA methylation levels of the ZBTB12 15 CpGs with LINE-1 DNA methylation levels into a prediction model of MI based on age, sex, recruitment centre, smoking, body mass index (BMI), waist-to-hip ratio, lipid levels, blood pressure and menopausal status in women. Guarrera et al. found that by including DNA methylation in the model prediction of incident MI was improved in their replication cohort, as assessed by increased reclassification and discrimination (area under the receiver operating curves (AUC) improved from 0.66 to 0.69 for women and 0.7 for men) [26]. Overall, Guarrera et al.’s study discovered a novel blood DNA methylation signal for incident MI in ZBTB12 and provided evidence for the value of incorporating DNA methylation in MI prediction [26].
Angina, coronary insufficiency, coronary revascularization and CHD death are also commonly used outcomes for CHD and are occasionally grouped along with MI as a phenotype of interest in CVD EWASs. Furthermore, the group of phenotypes occasionally also includes stroke, which is often caused by atherosclerosis. Several studies have explored the association between DNA methylation and the incidence of these CVD outcome groups. Westerman et al. [30] performed an EWAS associating iCHD (incident MI, angina, revascularisation, stroke and CHD death) with blood DNA methylation profiles in 2023 discovery subjects of multiple ancestries (1009 iCHD cases) and 2587 replication subjects of European ancestry (305 iCHD cases). Overall, 3 DNA methylation regions were identified and replicated for iCHD association at a genome-wide Bonferroni multiple testing correction, in the SLC9A1, SLC1A5 and TNRC6C genes. Mendelian randomization analysis at 4 CpGs with methylation quantitative trait loci (meQTLs) in these regions identified one CpG (cg22304262) in SLC1A5 with moderate evidence for a putative causal effect on iCHD. Furthermore, the cis-meQTL SNP for cg22304262 (rs8105903) can also alter the expression level of SLC1A5 in blood in the GTEx (Genotype-Tissue Expression) data [31], suggesting that DNA methylation levels of cg22304262 may affect the expression of SLC1A5. SLC1A5 encodes a sodium-dependent cellular amino acid transporter, and this gene was found to facilitate glutaminolysis [32]. Suppression of SLC1A5 was demonstrated to impair glutamine homeostasis in failing myocardium [33]. In summary, this study not only explored novel blood DNA methylation regions associated with iCHD, but also demonstrated a putative causal effect for one of the discovered signals [30].
In the largest EWAS of iCHD outcomes to date, Agha et al. [34] conducted an EWAS meta-analysis of iCHD events including coronary insufficiency, angina, MI, coronary revascularization and CHD death. The study explored 11,461 blood leukocyte DNA methylation profiles (1895 iCHD cases, including 1183 MI-only cases) from 9 population-based cohorts of multiple ancestries, with a mean follow-up of 11.2 years. Altogether, 52 differentially methylated CpG sites in blood were shown to be associated with iCHD (multiple outcomes) or MI-only at a genome-wide FDR < 5%. The iCHD-associated CpGs were annotated to genes involved in calcium regulation and kidney function. The study also performed Mendelian randomization at 10 of the CpGs that also had meQTLs, identifying two CpGs (cg26470101 near to DLX2, and cg07289306 neighbouring MIR138-1) with putative causal effects on iCHD. The authors also explored if the meQTLs for these two signals overlap published expression-QTLs (eQTLs) [31] and observed overlapping eQTLs for nearby genes (meQTLs for cg26470101 are also eQTLs for ITGA6; and meQTLs for cg07289306 are also eQTLs for lncRNA RP4-555D20.2), indicating that DNA methylation levels at these two CpG sites may also influence the expression levels of nearby genes. Interestingly, one of the 52 CpG signals (cg05820312 in TRAPPC9), was shown to have a putative causal effect on systolic blood pressure in a recent Mendelian randomization study [35], therefore independently validating its relevance to cardiovascular health. To sum up, the results from the largest epigenetic study of iCHD to date highlight novel signals and potential new mechanisms whereby DNA methylation changes related to calcium regulation and renal function may play a role in the development of CHD.
In the most recent EWAS of iCHD to date Navas-Acien et al. [36] assessed the association between blood DNA methylation levels and fatal or non-fatal iCHD in a discovery cohort of American Indian ancestry, with replication in four cohorts from multiple ancestries. As one of the largest EWAS of iCHD the study included 2321 individuals (748 iCHD cases) in the discovery sample with a mean follow-up from baseline to iCHD outcome of 19.1 years, and 7047 individuals (1145 iCHD cases) in the replication cohorts with a mean follow-up of 15.6 years across the replication samples combined. The authors applied both standard linear models and Elastic-Net models in the EWAS to account for the inter-associations among CpG sites. While the standard iCHD EWAS did not detect significant results, the Elastic-Net EWAS identified 505 differentially methylated positions (DMPs) associated with iCHD in the discovery sample, where 4 signals replicated in all replication cohorts, and a further 29 replicated in three out of four replication cohorts. Ten of these 33 replicated DMPs showed significant pooled hazard ratios (p < 0.05) in a Cox regression model, such that changes in methylation showed an overall consistent directionality with iCHD across cohorts. The 10 DMPs map to genes related to coronary artery lesions, cardiometabolic traits, blood pressure, pulmonary hypertension, stroke, lipid levels, and cell adhesion, indicating high relevance to iCHD. However, cohort-specific analyses also identified distinct iCHD signals in each sample, suggesting that iCHD methylome signals can also exhibit population-specific effects.
These four EWASs of iCHD have altogether identified 66 DNA methylation signals of iCHD after genome-wide correction for multiple testing (Table 1), although the majority of signals have small effect sizes. The signals are located in a wide range of genes, including genes involved in lipid metabolism, amino acid transport, ion transport, transcriptional regulation, RNA processing, immune system processes and tissue-specific regulations. Furthermore, causal inference analyses indicate that 3 CpGs (cg22304262, cg26470101 and cg07289306) may have putative causal effects on iCHD, as well as potential impacts on gene expression. However, the four EWASs of iCHD do not show overlapping DNA methylation signatures for iCHD, possibly due to population and phenotype heterogeneity, and small effects at the differentially methylated sites.
EWASs of CHD risk factors with iCHD follow-up
Multiple large-scale studies have carried out EWASs of CHD risk factors and subsequently explored how the resulting signals relate to iCHD outcomes. This approach may identify novel iCHD-associated CpGs beyond the signals identified from EWASs of iCHD alone, and help to understand how specific CHD risk factors contribute to biological mechanisms underlying iCHD development. Methylation signals could further contribute towards the development of iCHD methylation risk scores that together with traditional iCHD risk equations may improve the performance of iCHD risk prediction.
TNF-α is a pro-inflammation cytokine that plays an important role in atherosclerosis, which underlies most CHD events. A cross-sectional EWAS meta-analysis in 4794 subjects, with replication in a further 816 subjects of European ancestry, linked blood DNA methylation profiles to circulating TNF-α levels [37]. The results identified differential methylation at 2 CpG sites in NLRC5 and 2 CpG sites in DTX3L and PARP9, where all three genes are involved in immune response. Upon exploring DNA methylation associations with gene expression in cis (cis-eQTMs), the authors found that all 4 CpGs were associated with expression of nearby genes in the discovery sample, but not in an external dataset. The authors then observed a significant association between DNA methylation levels of these 4 CpG sites and iCHD in 1895 iCHD cases (from Agha et al.’s study [34] with mean follow-up time of 11.2 years), which was a trans-ancestry population sample that overlapped with their discovery dataset. These results demonstrate that blood DNA methylation signatures of TNF-α may have biomarker potential for iCHD and towards methylation-based CHD risk prediction.
Lipids are important risk factors of CHD. Multiple EWASs have explored total cholesterol, LDL cholesterol and TG which are pro-atherogenic, and HDL cholesterol which is anti-atherogenic. Hedman et al. [38] performed an EWAS of lipids in whole blood samples from 2306 discovery subjects with replication in 2025 subjects of European ancestry. The study identified 33 associated CpGs after replication, of which one signal (cg27243685) in the ABCG1 gene was also significantly associated with iCHD in 8-year (115 cases) and 10-year (78 cases) clinical follow-ups in their discovery sample. ABCG1 encodes a cellular transporter protein that regulates lipid efflux, and ABCG1 methylation levels have also been associated with retrospective CHD in recent candidate gene DNA methylation studies [39, 40]. Hedman et al.’s study also explored the association between DNA methylation at candidate CpG signals and gene expression in a subset of samples, and observed that methylation levels of cg27243685 negatively associated with ABCG1 expression [38].
Obesity is another major risk factor of CHD [41]. Campanella et al. [42] carried out EWASs of obesity-related phenotypes (BMI, waist circumference, waist-hip and waist-height ratio) in peripheral blood leucocyte DNA methylation profiles from 1941 subjects with replication in 358 subjects from a European population, and where the peak methylation signals were then linked to future risk of MI (131 cases). Methylation levels at a CpG-site (cg12593793) in the LMNA gene identified from EWAS of waist-to-height ratio were inversely associated with risk of MI (follow-up time > 1 year) in the discovery sample. Polymorphisms and mutations in the LMNA gene are known to be related to abdominal adipocyte size [43], type 2 diabetes mellitus [43, 44] and cardiomyopathy [45]. The authors also assessed methylation associations with nearby gene expression levels, but no signals were found for cg12593793.
As previously discussed, risk scores are often used to aid the assessment of the likelihood of developing future CHD. Fernández-Sanlés et al. [46] developed an age-independent cardiovascular risk based on vascular age and multiple traditional cardiovascular risk factors including lipids, blood pressure, diabetes, smoking and obesity. They then investigated its association with genome-wide whole blood DNA methylation profiles in a discovery sample of 645 subjects, with replication in 2542 subjects of European ancestry. The results identified 8 CpGs in ALPPL2, AHRR, PPIF, CPT1A, SBNO2 and in 3 intergenic regions. Using these 8 CpGs the authors developed a DNA methylation risk score (MRS) for predicting future CVD events. This MRS demonstrated an association with incident CVD (222 cases, median follow-up time = 7.66 years) in their replication cohort.
To conclude, to date 14 blood DNA methylation CpG signals have been identified from EWASs of CHD risk factors (including TNF-α, lipids, waist-to-height-ratio and age-independent cardiovascular risk) to be directly linked to the development of iCHD with a 7-to-12-year follow-up (Table 2). Altogether, these results identify genes and mechanisms of disease progression that may be targeted therapeutically. For example, the CpG sites map to genes involved in lipid metabolism, phosphatase activity and transcription activity, and one of these signals in ABCG1 also associates with ABCG1 expression. Although the CpG sites identified in these EWASs of CHD risk factors with iCHD follow-up do not overlap with the signals identified from EWASs of iCHD to date (described in the previous section) multiple signals were previously detected in EWASs of CHD risk factors without direct iCHD follow-up, and are outlined below.
The emerging blood-based DNA methylation signatures of iCHD
The signals detected from EWASs of iCHD and EWASs of CHD-risk factors with iCHD follow-up map to genes that are enriched for several molecular functions and biological processes. Enriched annotations include ion binding activity, transcriptional regulation, and regulation of cellular macromolecule biosynthetic process. Many of the identified signals related to iCHD have been previously identified as signals in EWASs of CHD risk factors in cross-sectional studies, without iCHD follow-ups. This section discusses candidate DNA methylation signals of iCHD that have emerged from recent EWASs and that have also previously shown associations in independent studies of specific iCHD risk factors (Table 3).
Several biomarkers of smoking have been identified in EWASs of iCHD or EWASs with iCHD follow-ups, including signals in the AHRR and ALPPL2 genes. AHRR is a downstream target of the aryl hydrocarbon receptor (AHR) pathway, which facilitates the activation of enzymes and transporters involved in the elimination and biotransformation of toxins in the human body. AHRR helps mediate the transcription of AHR-dependent genes, functioning as a negative regulator in the AHR pathway [47]. DNA methylation of AHRR is the most consistent signature of tobacco smoking and has been shown to be a good biomarker for cardiovascular risk prediction [48], as well as being associated with serum CRP levels, a risk factor of CHD [49], and carotid intima-media thickness, an index of subclinical atherosclerosis [50]. ALPPL2 is another consistently replicated smoking-methylation locus, where the protein is a membrane-binding glycosylated enzyme and is considered to be a highly specific tumour cell surface antigen [51]. DNA methylation of ALPPL2 has also been associated with all-cause mortality [52]. Furthermore, a recent EWAS of CHD identified signals in AHRR (cg05575921) and near ALPPL2 (cg21566642) to be associated with retrospective CHD with validation in independent iCHD samples [53].
CpG-sites in lipid metabolism genes have also been identified in EWASs of iCHD or EWASs with iCHD follow-ups, including in the ABCG1 and CPT1A genes. ABCG1 is a transporter protein regulating lipid efflux that plays an important role in preventing the accumulation of excessive cholesterol, thus the build-up of atherosclerosis in the human body. DNA methylation signals in ABCG1 have previously been identified in a wide range of EWASs, including in EWASs of CHD risk factors such as HDL-cholesterol levels and TG levels [54], BMI, waist circumference, waist-hip and waist-height ratio [42], insulin levels and its assessment model HOMA-IR [55]. CPT1A encodes an important protein in lipid metabolism which mediates the transportation of long-chain fatty acid into the mitochondria. DNA methylation signals in CPT1A were previously reported in multiple EWASs of TG levels [38, 54, 56], BMI [57], and blood pressure [58].
Signals related to inflammation have also been identified in EWASs of iCHD or with iCHD follow up, including sites in the SBNO2 and ITGB2 genes. SBNO2 encodes a transcriptional coregulator considered to be an inflammatory response factor in the central nervous system [59]. Differential methylation of the SBNO2 gene was associated with serum CRP levels [49] and growth differentiation factor-15 (GDF-15) [60]. ITGB2 encodes a component of the integrin pathway which is involved in the leukocyte adhesion process [61]. DNA methylation in the ITGB2 gene has been associated with serum CRP levels [49], as well as variation in the atherosclerotic aorta [62].
Several EWASs of iCHD or with iCHD follow-up have carried out causal inference analyses of the peak signals. For example, DNA methylation levels in SLC1A5 were shown to have a putative causal effect on iCHD [30]. SLC1A5 encodes a sodium-dependent neutral amino acid transporter, which functions as a mediator of glutamine transport in cancer cell growth and survival [63]. CpG sites in SLC1A5 were also reported to be associated with TG levels [38] and blood pressure [58] in independent EWASs. Apart from SLC1A5, Mendelian randomisation analysis also identified DNA methylation levels of 2 CpGs in the transcription activator DLX2 and micro-RNA MIR138-1, respectively, which may have causal effects on iCHD. Although little is known about the exact links between these genes and CHD or CHD risk factors currently, these signals may be valuable for future research.
Altogether, EWAS of iCHD and EWAS of CHD risk factors with iCHD follow-ups have identified both novel DNA methylation signals, as well as signals with previously established relevance to cardiovascular health. These results give the opportunity for a better understanding of the development of CHD, as well as the potential for selecting new biomarkers of iCHD.
Towards methylation-based iCHD risk prediction
Several large-scale EWASs have identified DNA methylation signals associated with iCHD, including both novel signals and changes previously identified to associate with CHD or CVD risk. Although the iCHD signals do not overlap across iCHD studies, multiple signals show promising biomarker potential (Table 3), and a small subset exhibit evidence for putative causal effects on iCHD. However, the potential of DNA methylation signatures discovered in EWASs of iCHD for the prediction of iCHD has not yet been fully assessed.
A few studies have explored the use of epigenetics towards the prediction of iCHD. Guarrera et al. [26] assessed the predictive value of incorporating the peak iCHD EWAS signals to predict iCHD within their replication dataset, showing improved discrimination and reclassification compared to the use of traditional risk factors alone. Other methylation predictors have also been developed in recent years using peak signals from EWASs of retrospective CHD. Fernández-Sanlés et al. [53] developed a methylation risk score for the prediction of CHD and CVD based on a two-stage EWAS of cross-sectional acute MI in peripheral blood in a European population sample and the association of EWAS peak signals with iCHD follow-up. However, they did not observe an increase in discrimination and reclassification when incorporating the methylation risk score into the Framingham risk function [8]. Given the limited overlap across signals from different EWAS of iCHD alone, these results suggest that methylation risk scores should also consider population-specific aspects, potentially reflecting different CHD risk profiles across populations.
In addition to methylation risk score predictors alone, multiple layers of -omic information have also been combined with DNA methylation signals to develop multi-omic risk score classifiers and predictors for iCHD. A series of studies were conducted to integrate genetic and epigenetic (DNA methylation) information using machine learning for the classification of retrospective CHD cases and controls [64], as well as for prediction of incident CHD [65, 66]. All studies showed improved sensitivity for classification or prediction of incident CHD compared to conventional risk models [8, 14]. The most recent study by Dogan et al. [66] developed an integrated genetic-epigenetic model for predicting 3-year iCHD from a training set consisting of subjects of European ancestry. The model, which incorporated data from three methylation loci and five SNPs, showed superior sensitivity compared to the Framingham risk model [8] and the ASCVD risk model [14] in an external validation set. In the external validation set, the sensitivity of prediction increased from 31% for the Framingham risk model and 69% for the ASCVD risk model, to 75% for the new combined genetic and epigenetic CHD model. These results show better performance of integrated genetic and epigenetic models compared to conventional clinical risk models for prediction of individuals at greater risk for future CHD. Another recent multi-omic approach by Palou-Márquez et al. [67] integrated DNA methylation and gene expression data using multi-omic factor analysis (MOFA). Four factors based on methylation variability were associated with CVD incidence, and two of these improved the prediction performance of the Framingham risk function [8] in integrated analysis. The findings indicate that methylation and multi-omic risk score predictors have potential to improve the performance of conventional clinical risk score predictors for predicting future iCHD. Moreover, replication of the approach in an independent cohort identified DNA methylation signatures at three genes that also contributed to a factor associated with MI in the replication sample. These results together with findings from EWAS of iCHD suggest an extent of population specificity in the DNA methylation signature of iCHD, which supports future explorations of population specific DNA methylation predictors of iCHD.
One difficulty in interpreting the iCHD results described so far is that alterations in different molecular mechanisms can give rise to separate CHD events that could then be grouped together into a single iCHD outcome in EWASs. For instance, the mechanisms underlying troponin-negative unstable anginas will likely differ from those behind troponin-positive acute coronary syndromes [68]. In the EWASs of iCHD described above, a few studies consider more than one subtype of iCHD event as the phenotype of interest, which introduces phenotype heterogeneity. For example, in some studies stroke may be used together with CHD events as a CVD outcome [30], although the underlying mechanisms may differ. To tackle this, larger studies should be undertaken with more homogeneous phenotypes, for example, restricting the outcome to a single type of CHD event. Ideally, clinical case ascertainment should be carried out where possible to classify disease cases in more details.
Further limitations to the iCHD EWAS studies discussed here relate to aspects of methylome profiling. For example, most of the studies measured blood DNA methylation profiles with the 450 k array in the discovery samples. The 450 k array only measures less than 2% out of 28.3 million CpG sites across the human genome. More recent methylome profiling microarray technologies, such as the Infinium MethylationEPIC BeadChip (EPIC array), double this genome coverage, but still only profile less than 4% of CpG sites genome-wide. Ultimately, whole-genome bisulfite sequencing efforts will be needed to assess the methylome signature of iCHD at full resolution. Additionally, the EWASs of iCHD described so far were conducted in blood. Blood methylation levels are biologically relevant to iCHD because, for one, blood leukocytes were demonstrated to be responsible for the inflammation reaction which starts the formation of atheroma [69]. Blood samples are also easy to collect and access, which makes it convenient to measure DNA methylation in large well-powered samples and use it as a prediction tool in clinical setups. However, atherosclerosis plaques are distributed in different arteries and display focality. Therefore, DNA methylation of whole blood may not be representative for the development of individual atheromas.
Finally, experimental follow-ups that explore the functional impact of methylation changes are often difficult to conduct following the discovery of EWAS signals. Most EWASs of iCHD or with iCHD follow-ups assessed whether EWAS signals may be related to corresponding changes in gene expression at nearby genes. Guarrera et al. [26], Hedman et al. [38], and Campanella et al. [42] compared DNA methylation profiles with gene expression profiles in internal or external samples, whilst Westerman et al. [30], Agha et al. [34] and Aslibekyan et al. [37] explored the relationship between meQTLs and eQTLs from publicly available databases. However, none of the iCHD EWASs so far have carried out direct experiments to confirm the biological function of altered methylation levels of the identified CpG signatures.
To conclude, the rapid development of epigenome-wide technologies has enabled research efforts that provide an opportunity to add an epigenetic layer into the prediction of iCHD. Multiple epigenetic signals have been identified in iCHD, but a large-scale meta-analysis across these EWASs has yet to be carried out. In the future, further exploration of larger cohorts, ideally with a more detailed and homogeneous classification for iCHD cases, is needed. In addition to blood, DNA methylation profiling of heart tissue or vascular walls, which has been very limited to date [70,71,72], would provide highly relevant findings. Additionally, more functional follow-ups need to be carried out to characterise the function of the identified iCHD DNA methylation signatures, as this may provide insights for the development of iCHD events and their prevention. Finally, studies that assess the predictive ability of DNA methylation signatures of iCHD should be performed in larger cohorts incorporating the identified DNA methylation signatures of iCHD. These efforts may also aid clinical interventions, for example, providing more accurate iCHD prediction that leads to informed decisions regarding the choice of intervention.
Availability of data and materials
Not applicable.
Abbreviations
- 450k array:
-
Infinium HumanMethylation450 BeadChip
- ABCG1:
-
ATP binding cassette subfamily G member 1
- AHR:
-
Aryl-hydrocarbon receptor
- AHRR:
-
Aryl-hydrocarbon receptor repressor
- ALPPL2:
-
Alkaline phosphatase, placental-like 2
- AS:
-
ALU and Satellite 2
- ASCVD:
-
Atherosclerotic cardiovascular disease
- AUC:
-
Area under the receiver operating curves
- BMI:
-
Body mass index
- CHD:
-
Coronary heart disease
- cis-eQTMs:
-
DNA methylation associations with gene expression in cis
- CpG:
-
5′-Cytosine-phosphate-guanine-3′ dinucleotide
- CPT1A:
-
Carnitine palmitoyltransferase 1A
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular disease
- DLX2:
-
Distal-less homeobox 2
- DMPs:
-
Differentially methylated positions
- DNA:
-
Deoxyribonucleic acid
- DTX3L:
-
Deltex E3 ubiquitin ligase 3L
- EPIC array:
-
Infinium MethylationEPIC BeadChip
- EWAS:
-
Epigenome-wide association study
- FDR:
-
False discovery rate
- GDF-15:
-
Growth differentiation factor-15
- GTEx:
-
Genotype-Tissue Expression
- GWAS:
-
Genome-wide association studies
- HbA1c:
-
Haemoglobin A1c
- HDL:
-
High-density lipoprotein
- HOMA-IR:
-
Homeostatic model assessment for insulin resistance
- iCHD:
-
Incident coronary heart disease
- IDI:
-
Integrated discrimination improvement
- ITGA6:
-
Integrin sub-unit α 6
- ITGB2:
-
Integrin subunit beta 2
- LDL:
-
Low-density lipoprotein
- LINE-1:
-
Long interspersed nuclear element-1
- LMNA:
-
Lamin A/C
- meQTL:
-
Methylation quantitative trait locus
- MI:
-
Myocardial infarction
- MIR138-1:
-
MicroRNA 138-1
- MRS:
-
Methylation risk score
- NLRC5:
-
NLR family CARD domain containing 5
- NRI:
-
Net reclassification improvement
- PARP9:
-
Poly (ADP-ribose) polymerase family member 9
- PPIF:
-
Peptidylprolyl isomerase F
- PRS:
-
Polygenic risk score
- RNA:
-
Ribonucleic acid
- SBNO2:
-
Strawberry notch homolog 2
- SLC1A5:
-
Solute carrier family 1 member 5
- SLC9A1:
-
Solute carrier family 9 member A1
- SNP:
-
Single nucleotide polymorphism
- TG:
-
Triglyceride
- TNF-α:
-
Tumour necrosis factor
- TNRC6C:
-
Trinucleotide repeat containing adaptor 6C
- TRAPPC9:
-
Trafficking protein particle complex 9
- ZBTB12:
-
Zinc finger and BTB domain containing 12
References
World Health Organization. Global health estimates: leading causes of death. 2021. https://www.who.int/data/gho/data/themes/mortality. Accessed 01 Mar 2021.
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–95.
Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF. Braunwald’s heart disease e-book: a textbook of cardiovascular medicine. Amsterdam: Elsevier Health Sciences; 2018.
Turkay M, Senol Y, Alimoglu MK, Aktekin MR, Deger N. Missed opportunities for coronary heart disease diagnoses: primary care experience. Croat Med J. 2007;48:362–70.
Erdmann J, Kessler T, Munoz Venegas L, Schunkert H. A decade of genome-wide association studies for coronary artery disease: the challenges ahead. Cardiovasc Res. 2018;114:1241–57.
Björkegren JLM, Kovacic JC, Dudley JT, Schadt EE. Genome-wide significant loci: how important are they?: Systems genetics to understand heritability of coronary artery disease and other common complex disorders. JACC. 2015;65:830–45.
Eichler EE, Flint J, Gibson G, Kong A, Leal SM, Moore JH, et al. Missing heritability and strategies for finding the underlying causes of complex disease. Nat Rev Genet. 2010;11:446–50.
Wilson PWF, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47.
Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of 10-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003.
SCORE2 Working Group and ESC Cardiovascular Risk Collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42:2439–54.
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, May M, Brindle P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ. 2007;335:136.
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336:a332.
Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ. 2017;357:j2099.
Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. 2014;25(Suppl 2):S74–75.
Muntner P, Colantonio LD, Cushman M, Goff DC, Howard G, Howard VJ, et al. Validation of the atherosclerotic cardiovascular disease Pooled Cohort risk equations. JAMA J Am Med Assoc. 2014;311:1406–15.
Lee CH, Woo YC, Lam JKY, Fong CHY, Cheung BMY, Lam KSL, et al. Validation of the Pooled Cohort equations in a long-term cohort study of Hong Kong Chinese. J Clin Lipidol. 2015;9:640–646.e2.
Kathiresan S, Melander O, Anevski D, Guiducci C, Burtt NP, Roos C, et al. Polymorphisms associated with cholesterol and risk of cardiovascular events. N Engl J Med. 2008;358:1240–9.
Mosley JD, Gupta DK, Tan J, Yao J, Wells QS, Shaffer CM, et al. Predictive accuracy of a Polygenic Risk Score compared with a Clinical Risk Score for incident coronary heart disease. JAMA J Am Med Assoc. 2020;323:627–35.
Abraham G, Havulinna AS, Bhalala OG, Byars SG, De Livera AM, Yetukuri L, et al. Genomic prediction of coronary heart disease. Eur Heart J. 2016;37:3267–78.
Inouye M, Abraham G, Nelson CP, Wood AM, Sweeting MJ, Dudbridge F, et al. Genomic risk prediction of coronary artery disease in 480,000 adults: implications for primary prevention. J Am Coll Cardiol. 2018;72:1883–93.
Lambert SA, Abraham G, Inouye M. Towards clinical utility of polygenic risk scores. Hum Mol Genet. 2019;28:R133–42.
Breitling LP, Yang R, Korn B, Burwinkel B, Brenner H. Tobacco-smoking-related differential DNA methylation: 27K discovery and replication. Am J Hum Genet. 2011;88:450–7.
Rask-Andersen M, Martinsson D, Ahsan M, Enroth S, Ek WE, Gyllensten U, et al. Epigenome-wide association study reveals differential DNA methylation in individuals with a history of myocardial infarction. Hum Mol Genet. 2016;25:4739–48.
Li J, Zhu X, Yu K, Jiang H, Zhang Y, Deng S, et al. Genome-wide analysis of DNA methylation and acute coronary syndrome. Circ Res. 2017;120:1754–67.
Wei L, Liu S, Su Z, Cheng R, Bai X, Li X. LINE-1 hypomethylation is associated with the risk of coronary heart disease in Chinese population. Arq Bras Cardiol. 2014;102:481–7.
Guarrera S, Fiorito G, Onland-Moret NC, Russo A, Agnoli C, Allione A, et al. Gene-specific DNA methylation profiles and LINE-1 hypomethylation are associated with myocardial infarction risk. Clin Epigenetics. 2015;7:133.
Kim M, Long TI, Arakawa K, Wang R, Yu MC, Laird PW. DNA methylation as a biomarker for cardiovascular disease risk. PLoS ONE. 2010;5:e9692.
Fernández-Sanlés A, Sayols-Baixeras S, Subirana I, Degano IR, Elosua R. Association between DNA methylation and coronary heart disease or other atherosclerotic events: a systematic review. Atherosclerosis. 2017;263:325–33.
Noro F, Gianfagna F, Gialluisi A, de Curtis A, di Castelnuovo A, Napoleone E, et al. ZBTB12 DNA methylation is associated with coagulation- and inflammation-related blood cell parameters: findings from the Moli-family cohort. Clin Epigenetics. 2019;11:74.
Westerman K, Sebastiani P, Jacques P, Liu S, DeMeo D, Ordovás JM. DNA methylation modules associate with incident cardiovascular disease and cumulative risk factor exposure. Clin Epigenetics. 2019;11:142.
Aguet F, Brown AA, Castel SE, Davis JR, He Y, Jo B, et al. Genetic effects on gene expression across human tissues. Nature. 2017;550:204–13.
Huang MS, Chang JH, Lin WC, Cheng YH, Li FA, Suen CS, et al. SLC38A2 overexpression induces a cancer-like metabolic profile and cooperates with SLC1A5 in pan-cancer prognosis. Chem Asian J. 2020;15:3861–72.
Kennel PJ, Liao X, Saha A, Ji R, Zhang X, Castillero E, et al. Impairment of myocardial glutamine homeostasis induced by suppression of the amino acid carrier SLC1A5 in failing myocardium. Circ Heart Fail. 2019;12:12.
Agha G, Mendelson MM, Ward-Caviness CK, Joehanes R, Huan TX, Gondalia R, et al. Blood leukocyte DNA methylation predicts risk of future myocardial infarction and coronary heart disease. Circulation. 2019;140:645–57.
Huan T, Joehanes R, Song C, Peng F, Guo Y, Mendelson M, et al. Genome-wide identification of DNA methylation QTLs in whole blood highlights pathways for cardiovascular disease. Nat Commun. 2019;10:4267.
Navas-Acien A, Domingo-Relloso A, Subedi P, Riffo-Campos AL, Xia R, Gomez L, et al. Blood DNA methylation and incident coronary heart disease: evidence from the Strong Heart study. JAMA Cardiol. 2021;4:e212704.
Aslibekyan S, Agha G, Colicino E, Do AN, Lahti J, Ligthart S, et al. Association of methylation signals with incident coronary heart disease in an epigenome-wide assessment of circulating tumor necrosis factor. JAMA Cardiol. 2018;3:463–72.
Hedman ÅK, Mendelson MM, Marioni RE, Gustafsson S, Joehanes R, Irvin MR, et al. Epigenetic patterns in blood associated with lipid traits predict incident coronary heart disease events and are enriched for results from genome-wide association studies. Circ Cardiovasc Genet. 2017;10:e001487.
Guay SP, Légaré C, Houde AA, Mathieu P, Bossé Y, Bouchard L. Acetylsalicylic acid, aging and coronary artery disease are associated with ABCA1 DNA methylation in men. Clin Epigenetics. 2014;6:178–91.
Ghose S, Ghosh S, Tanwar VS, Tolani P, Kutum R, Sharma A, et al. Investigating coronary artery disease methylome through targeted bisulfite sequencing. Gene. 2019;721:144107.
Bastien M, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56:369–81.
Campanella G, Gunter MJ, Polidoro S, Krogh V, Palli D, Panico S, et al. Epigenome-wide association study of adiposity and future risk of obesity-related diseases. Int J Obes. 2018;42:2022–35.
Weyer C, Wolford JK, Hanson RL, Foley JE, Tataranni PA, Bogardus C, et al. Subcutaneous abdominal adipocyte size, a predictor of type 2 diabetes, is linked to chromosome 1q21–q23 and is associated with a common polymorphism in LMNA in Pima Indians. Mol Genet Metab. 2001;72:231–8.
Wegner L, Anthonsen S, Bork-Jensen J, Dalgaard L, Hansen T, Pedersen O, et al. LMNA rs4641 and the muscle lamin A and C isoforms in twins—metabolic implications and transcriptional regulation. J Clin Endocrinol Metab. 2010;95:3884–92.
Hermida-Prieto M, Monserrat L, Castro-Beiras A, Laredo R, Soler R, Peteiro J, et al. Familial dilated cardiomyopathy and isolated left ventricular noncompaction associated with lamin A/C gene mutations. Am J Cardiol. 2004;94:50–4.
Fernández-Sanlés A, Sayols-Baixeras S, Curcio S, Subirana I, Marrugat J, Elosua R. DNA methylation and age-independent cardiovascular risk, an epigenome-wide approach the REGICOR study (REgistre GIroní del COR). Arterioscler Thromb Vasc Biol. 2018;38:645–52.
Larigot L, Juricek L, Dairou J, Coumoul X. AhR signaling pathways and regulatory functions. Biochim Open. 2018;7:1–9.
Zhang Y, Schöttker B, Florath I, Stock C, Butterbach K, Holleczek B, et al. Smoking-associated DNA methylation biomarkers and their predictive value for all-cause and cardiovascular mortality. Environ Health Perspect. 2016;124:67–74.
Ligthart S, Marzi C, Aslibekyan S, Mendelson MM, Conneely KN, Tanaka T, et al. DNA methylation signatures of chronic low-grade inflammation are associated with complex diseases. Genome Biol. 2016;17:255.
Portilla-Fernández E, Hwang S-J, Wilson R, Maddock J, Hill WD, Teumer A, et al. Meta-analysis of epigenome-wide association studies of carotid intima-media thickness. Eur J Epidemiol. 2021. https://doi.org/10.1007/s10654-021-00759-z.
Su Y, Zhang X, Bidlingmaier S, Behrens CR, Lee NK, Liu B. ALPPL2 is a highly specific and targetable tumor cell surface antigen. Cancer Res. 2021;80:4552–64.
Abdulrahim JW, Kwee LC, Grass E, Siegler IC, Williams R, Karra R, et al. Epigenome-wide association study for all-cause mortality in a cardiovascular cohort identifies differential methylation in castor zinc zinger 1 (CASZ1). J Am Heart Assoc. 2019;8:e013228.
Fernández-Sanlés A, Sayols-Baixeras S, Subirana I, Sentí M, Pérez-Fernández S, Castro de Moura M, et al. DNA methylation biomarkers of myocardial infarction and cardiovascular disease. Clin Epigenetics. 2021;13:86.
Pfeiffer L, Wahl S, Pilling LC, Reischl E, Sandling JK, Kunze S, et al. DNA methylation of lipid-related genes affects blood lipid levels. Circ Cardiovasc Genet. 2015;8:334–42.
Hidalgo B, Irvin MR, Sha J, Zhi D, Aslibekyan S, Absher D, et al. Epigenome-wide association study of fasting measures of glucose, insulin, and HOMA-IR in the genetics of lipid lowering drugs and diet network study. Diabetes. 2014;63:801–7.
Irvin MR, Zhi D, Joehanes R, Mendelson M, Aslibekyan S, Claas SA, et al. Epigenome-wide association study of fasting blood lipids in the genetics of lipid-lowering drugs and diet network study. Circulation. 2014;130:565–72.
Demerath EW, Guan W, Grove ML, Aslibekyan S, Mendelson M, Zhou YH, et al. Epigenome-wide association study (EWAS) of BMI, BMI change and waist circumference in African American adults identifies multiple replicated loci. Hum Mol Genet. 2015;24:4464–79.
Richard MA, Huan T, Ligthart S, Gondalia R, Jhun MA, Brody JA, et al. DNA methylation analysis identifies loci for blood pressure regulation. Am J Hum Genet. 2017;101:888–902.
Grill M, Syme TE, Noçon AL, Lu AZX, Hancock D, Rose-John S, et al. Strawberry notch homolog 2 is a novel inflammatory response factor predominantly but not exclusively expressed by astrocytes in the central nervous system. Glia. 2015;63:1738–52.
Ek WE, Hedman ÅK, Enroth S, Morris AP, Lindgren CM, Mahajan A, et al. Genome-wide DNA methylation study identifies genes associated with the cardiovascular biomarker GDF-15. Hum Mol Genet. 2016;25:817–927.
Kijas JMH, Bauer TR, Gäfvert S, Marklund S, Trowald-Wigh G, Johannisson A, et al. A missense mutation in the β-2 integrin gene (ITGB2) causes canine leukocyte adhesion deficiency. Genomics. 1999;61:101–7.
Del Pilar V-M, Zaina S, Heyn H, Carmona FJ, Varol N, Sayols S, et al. The DNA methylation drift of the atherosclerotic aorta increases with lesion progression. BMC Med Genomics. 2015;8:7.
Hassanein M, Hoeksema MD, Shiota M, Qian J, Harris BK, Chen H, et al. SLC1A5 mediates glutamine transport required for lung cancer cell growth and survival. Clin Cancer Res. 2013;19:560–70.
Dogan MV, Grumbach IM, Michaelson JJ, Philibert RA. Integrated genetic and epigenetic prediction of coronary heart disease in the Framingham Heart Study. PLoS ONE. 2018;13:e0190549.
Dogan MV, Beach SRH, Simons RL, Lendasse A, Penaluna B, Philibert RA. Blood-based biomarkers for predicting the risk for 5-year incident coronary heart disease in the Framingham Heart Study via machine learning. Genes (Basel). 2018;9:641.
Dogan MV, Knight S, Dogan TK, Knowlton KU, Philibert R. External validation of integrated genetic-epigenetic biomarkers for predicting incident coronary heart disease. Epigenomics. 2021;13:1095–112.
Palou-Márquez G, Subirana I, Nonell L, Fernández-Sanlés A, Elosua R. DNA methylation and gene expression integration in cardiovascular disease. Clin Epigenetics. 2021;13:75.
Fuster V, Kovacic JC. Acute coronary syndromes: pathology, diagnosis, genetics, prevention, and treatment. Circ Res. 2014;114:1847–51.
Libby P, Tabas I, Fredman G, Fisher EA. Inflammation and its resolution as determinants of acute coronary syndromes. Circ Res. 2014;114:1867–79.
Nazarenko MS, Markov AV, Lebedev IN, Freidin MB, Sleptcov AA, Koroleva IA, et al. A comparison of genome-wide DNA methylation patterns between different vascular tissues from patients with coronary heart disease. PLoS ONE. 2015;10:e0122601.
Yamada Y, Nishida T, Horibe H, Oguri M, Kato K, Sawabe M. Identification of hypo- and hypermethylated genes related to atherosclerosis by a genome-wide analysis of DNA methylation. Int J Mol Med. 2014;33:1355–63.
Yamada Y, Horibe H, Oguri M, Sakuma J, Takeuchi I, Yasukochi Y, et al. Identification of novel hyper- or hypomethylated CpG sites and genes associated with atherosclerotic plaque using an epigenome-wide association study. Int J Mol Med. 2018;41:2724–32.
Zhang J, Liu Z, Umukoro PE, Cavallari JM, Fang SC, Weisskopf MG, et al. An epigenome-wide association analysis of cardiac autonomic responses among a population of welders. Epigenetics. 2017;12:71–6.
Gallego-Fabrega C, Carrera C, Reny JL, Fontana P, Slowik A, Pera J, et al. TRAF3 epigenetic regulation is associated with vascular recurrence in patients with ischemic stroke. Stroke. 2016;47:1180–6.
Mendelson MM, Marioni RE, Joehanes R, Liu C, Hedman ÅK, Aslibekyan S, et al. Association of body mass index with DNA methylation and gene expression in blood cells and relations to cardiometabolic disease: a Mendelian randomization approach. PLoS Med. 2017;14:e1002215.
Ahsan M, Ek WE, Rask-Andersen M, Karlsson T, Lind-Thomsen A, Enroth S, et al. The relative contribution of DNA methylation and genetic variants on protein biomarkers for human diseases. PLoS Genet. 2017;13:e1007005.
Zeilinger S, Kühnel B, Klopp N, Baurecht H, Kleinschmidt A, Gieger C, Weidinger S, Lattka E, Adamski J, Peters A, Strauch K, Waldenberger M, Illig T, Chen A. Tobacco smoking leads to extensive genome-wide changes in DNA methylation. PLoS ONE. 2013;8(5):e63812. https://doi.org/10.1371/journal.pone.0063812.
Kazmi N, Sharp GC, Reese SE, Vehmeijer FO, Lahti J, Page CM, et al. Hypertensive disorders of pregnancy and DNA methylation in newborns. Hypertension. 2019;74:375–83.
Acknowledgements
Not applicable.
Funding
This review received support from the JPI ERA-HDHL DIMENSION project and UK Biotechnology and Biological Sciences Research Council (BBSRC, BB/S020845/1 and BB/T019980/1 to JTB).
Author information
Authors and Affiliations
Contributions
YX and JB drafted the manuscript. JB and AB reviewed the manuscript and approved the final draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xia, Y., Brewer, A. & Bell, J.T. DNA methylation signatures of incident coronary heart disease: findings from epigenome-wide association studies. Clin Epigenet 13, 186 (2021). https://doi.org/10.1186/s13148-021-01175-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13148-021-01175-6