Abstract
Background
Despite the growing evidence of diabetic kidney disease (DKD) in adult patients with long-standing diabetes in sub-Saharan Africa, data on its burden and correlates in adult African patients with new-onset diabetes are limited. We, therefore, undertook this study to determine the burden and predictors of DKD in an adult population with new-onset diabetes in Uganda.
Methods
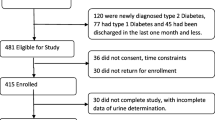
We collected data on the relevant sociodemographic, clinical, anthropometric, and metabolic characteristics in 519 participants with newly diagnosed diabetes recruited from seven tertiary hospitals. A spot mid-stream urine sample was collected for determination of the urine albumin creatinine ratio (UACR) using Clinitek® microalbumin strips and a point-of-care Clinitek® status analyser. The estimated glomerular filtration rate (e-GFR) was determined using the Chronic Kidney Disease Epidemiology formula. The presence of DKD was defined as a spot UACR ≥ 3 mg/mmol with or without an e-GFR < 60 ml/min/1.73m2.
Results
The median (IQR) age, UACR, and e-GFR of the participants were 48 years (39–57), 2.27 mg/mmol (1.14–3.41), and 121.8 ml/min/1.73m2 (105.4-133.9). UACR ≥ 3 mg/mmol and e-GFR < 60 ml/min/1.73m2 was noted in 175 (33.7%) and 7 (1.4%) participants, respectively. DKD was documented in 175 participants (33.7%). Compared with those without DKD, participants with DKD were more likely to be ≥ 50 years of age (53.7% vs. 43%, p = 0.02) and to have co-existing hypertension at the time of diagnosis (40.6% vs. 30.1%, p = 0.02). On multivariate analysis, self-reported hypertension comorbidity (OR 1.76 95% CI 1.24–2.48, p = 0.002) and body mass index (BMI) ≥ 30 kg/m2 (OR 0.61 95% CI 0.41–0.91, p = 0.02) were noted to independently predict DKD.
Conclusion
In this study population, DKD was relatively common and was independently associated with self-reported hypertension comorbidity and BMI ≥ 30 kg/m2.
Similar content being viewed by others
Introduction
Diabetic kidney disease (DKD) is a heterogeneous clinical condition characterised by the presence of persistent overt proteinuria (urine albumin creatinine ratio or UACR ≥ 300 mg/g or 3 mg/mmol) and declining renal function reflected by an estimated glomerular filtration rate (e-GFR) of < 60 ml/min/1.73 m2 [1]. Traditionally, the presence of albuminuria has been recognised as the hallmark of DKD (classical albuminuric DKD). However, recent studies have shown that, in addition to the classical albuminuric DKD phenotype, two new nonalbuminuric phenotypes of DKD exist, i.e., nonalbuminuric DKD and progressive renal decline, suggesting that progression of DKD can also occur through a non-albuminuric pathway [2, 3].
An increasing burden of DKD has been reported in adult patients with type 2 diabetes in sub-Saharan Africa (SSA) [4,5,6]. While there is reasonable data on the prevalence of DKD in African patients with long-standing diabetes, data on its burden and predictors in adult patients with newly diagnosed diabetes remains limited.
This study aimed to investigate the prevalence, phenotypes, and predictors of DKD in an adult Ugandan population with newly diagnosed diabetes.
Methods
Study settings, duration, and participants
The study participants were recruited from adult diabetes outpatient clinics of seven tertiary public and private mission hospitals located in Central and Southwestern Uganda between February 2019 and October 2020.
Participants were patients aged ≥ 18 years with new-onset diabetes (< 3 months preceding the diagnosis of diabetes), either treatment naïve or any glucose-lowering therapy. Participants with fever, any acute illness, and pregnancy were excluded.
A total of 519 participants were recruited for the study.
Socio-demographic, clinical, anthropometric, and metabolic characterisation
After providing written informed consent, a study questionnaire was used to collect the vital sociodemographic (age, sex, and smoking status) and clinical (self-reported history of co-existing hypertension) characteristics. Resting blood pressure and anthropometric measurements were then performed and the systolic and diastolic blood pressure, body mass index (BMI), waist circumference (WC), hip circumference (HC), and waist: hip circumference ratio (WHR) were recorded.
All participants had a fasting blood sample drawn for the measurement of fasting blood glucose (FBG), glycated haemoglobin (HbA1c), lipid profile, uric acid, a complete blood count (for estimation of the haemoglobin level), serum urea, and serum creatinine (for estimation of the e-GFR).
A spot mid-stream urine sample was also collected for the measurement of UACR. This was performed using the Siemens Healthcare Clinitek® microalbumin reagent test strips and a point-of-care Clinitek® status analyser. The Clinitek® status analyser also provided data on urine leucocytes, nitrites, glucose, blood, and pH.
All the above tests were performed at the Medical Research Council/Uganda Virus Research Institute and London School of Hygiene and Tropical Medicine Uganda Research Unit, Entebbe Uganda.
The e-GFR was determined using the Chronic Kidney Disease Epidemiology (CKD-EPI) formula [7]. The e-GFR and the UACR were classified according to the Kidney Disease: Improving Global Outcomes (KDIGO) 2020 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. The e-GFR was categorized as follows: G1: ≥90mL/min/1.73m2 (normal kidney function), G2: 60–89mL/min/1.73 m2 (mildly decreased), G3a: 45–59mL/min/1.73 m2 (mildly to moderately decreased), G3b: 30–44mL/min/1.73 m2 (moderately to severely decreased), G4: 15–29mL/min/1.73 m2 (severely decreased), and G5: <15mL/min/1.73m2 (kidney failure). Albuminuria categories based on the UACR were as follows: A1: <3 mg/mmol (normal to mildly increased), A2: 3–30 mg/mmol (moderately increased), and A3: >30 mg/mmol (severely increased) [1].
Definition of diabetic kidney disease and its phenotypes
DKD was defined as a spot UACR ≥ 3 mg/mmol (A2 and A3) with or without a reduced e-GFR of < 60 ml/min/1.73m2 (G3a-G5). Albuminuric and non-albuminuric DKD was defined as a spot UACR ≥ 3 mg/mmol (A2 and A3) regardless of the e-GFR and an e-GFR < 60 ml/min/1.73m2 with UACR < 3 mg/mmol (G3a-G5 and A1). No DKD was defined as an e-GFR ≥ 90 ml/min/1.73m2 and UACR < 3 mg/mmol (G1 and A1) [1].
Statistical analysis
To describe the characteristics of all study participants, we used proportions for the categorical variables and medians with inter-quartile range (IQR) for the continuous variables. Proportions were also used to express those with and without DKD, and the two DKD phenotypes (albuminuric and non-albuminuric DKD).
The differences in the socio-demographic, clinical, anthropometric, and metabolic characteristics of participants with and without DKD were analysed using the x2 test for categorical data and the Kruskal Wallis test for continuous data. Odds ratios (OR) and their corresponding 95% confidence intervals (CI) were estimated using logistic regression. Specific sociodemographic, clinical, and metabolic characteristics well-known to be associated with DKD were added to the logistic regression model to identify the independent predictors of DKD. All analyses were done using STATA statistical software version 15 College Station, TX: StataCorp LLC.
Results
The characteristics of all study participants and those with and without DKD separately are shown in Table 1.
The median (IQR) age, HbA1c, UACR, and e-GFR of the participants was 48 years (39–57), 10.6% (7.8–12.5) or 92 mmol/mol (62–114), 2.27 mg/mmol (1.14–3.41), and 121.8 ml/min/1.73m2 (105.4-133.9). A UACR of < 3 mg/mol (A1 category), 3–30 mg/mmol (A2 category), and > 30 mg/mmol (A3 category) were noted in 344 (66.3%) participants, 167 (32.2%) participants, and 8 (1.5%) participants, respectively. An e-GFR of ≥ 90 ml/min/1.73m2 (G1 category), 60–90 ml/min/1.73m2 (G2 category), 45–59 ml/min/1.73m2 (G3a category), 30–44 ml/min/1.73m2 (G3b category), and < 15 ml/min/1.73m2 (G5 category) was noted in 461 (88.8%) participants, 51 (9.8%) participants, 4 (0.8%) participants, 2 (0.4%) participants, and 1 (0.2%) participant, respectively. No participant had an e-GFR between 15 and 29 ml/min/1.73m2.
DKD was observed in 175 participants (33.7%) participants.
Socio-demographic, clinical, and metabolic characterisation of participants with and without DKD
Compared with those without DKD, participants with DKD generally were more likely to be ≥ 50 years of age (53.7% vs. 43%, p = 0.02) and have co-existing hypertension at the time of diagnosis (40.6% vs. 30.1%, p = 0.02). No significant differences in sex, anthropometric (BMI, WC, and WHR), and metabolic (glycaemic indices-FBG and HbA1c, lipid profile, and uric acid concentrations) characteristics were noted between the two groups.
Independent predictors of DKD
Table 2 shows the multivariate analysis to identify predictors of DKD.
On multivariate analysis, self-reported hypertension comorbidity (OR 1.76 95% CI 1.24–2.48, p = 0.002) and BMI ≥ 30 kg/m2 (OR 0.61 95% CI 0.41–0.91, p = 0.02) were noted to be independent predictors of DKD.
Discussion
In this study population, we report that DKD was relatively common, with the majority of participants presenting with the albuminuric phenotype. We also documented that pre-existing hypertension increased the odds of DKD while obesity reduced the risk.
A wide variation in the prevalence of DKD has been reported across African populations [4,5,6, 8, 9]. In one systematic review and meta-analysis of 21 medium- and high-quality studies performed in SSA to document the epidemiology of chronic kidney disease, the prevalence of DKD in the included studies was reported to range between 7.3% and 24%, with proteinuria being used as the main marker of the presence of DKD, in 96% of the studies [6]. In another systematic review of 32 studies (two population-based and 30 clinic-based) performed in Africa by Noubiap JJ et al., the prevalence of DKD varied from 11 to 83.7%, with about 63% of the studies diagnosing DKD based on urine protein measurement [4]. Another systematic review and meta-analysis that evaluated the burden of DKD and its association with hypertension in 27 studies performed in SSA reported a pooled prevalence of DKD of 35.3% [5], similar to what we documented in our study.
The reasons to explain these significant variations in the prevalence of DKD across the different African populations may be related to differences in diagnostic methods (urine protein and e-GFR measurement) and diagnostic thresholds used, populations studied (long-standing vs. newly diagnosed or type 1 vs. type 2 diabetes or combined), and study design (population-based vs. health facility-based or private vs. public health facilities).
In our study, pre-existing hypertension was documented to be associated with increased odds of having DKD. Hypertension is a well-recognised risk factor of DKD, regardless of phenotype, in African [5, 8, 10,11,12], white [13, 14], and Asian [15, 16] populations. The mechanisms to explain the association between hypertension and DKD are not well-understood but may be related to augmented sodium retention, pro-inflammatory cascade, renin-angiotensin-aldosterone, sympathetic nervous system, endothelial cell dysfunction, and oxidative stress, which ultimately result in glomerular damage [17, 18].
Obesity (BMI ≥ 30 kg/m2) was documented to reduce the odds of DKD in our study population, a finding conflicting with what has been observed in most studies investigating risk factors of DKD [19]. This underscores the heterogeneity in the pathogenesis of DKD across populations.
A similar protective effect of obesity towards having DKD was also reported in a retrospective study performed in rural South Africa in 253 adult patients with diabetes. Obesity and severe obesity defined as BMI > 27 kg/m2 and > 33 kg/m2 were present in 63% and 36.5% of the participants, respectively. On multivariate analysis, severe obesity was associated with reduced odds of having microalbuminuria (OR 0.27 95% CI 0.08–0.48, p = 0.002) [11]. A BMI > 25 kg/m2 was also noted to be associated with a reduced likelihood of chronic kidney disease, regardless of cause, in an urban and peri-urban community-based study performed in Uganda [20].
The reasons explaining the increased risk of DKD in individuals with normal or low BMI as reported in our study have not been investigated in great detail but could partly be explained by the developmental origins of health and disease (DOHaD) theory or developmental programming. Early-life environmental insults (in-utero or early childhood) like chronic infections, pre-eclampsia, and maternal malnutrition induce epigenetic changes that affect gene expression, development of critical body organs like the kidneys and pancreas, and function later in life resulting in several cardiometabolic conditions. Increased susceptibility to hypertension (a common predictor of kidney disease in African patients) and chronic kidney disease often develop due to an existing low nephron number or mass (Brenner hypothesis) which may be related to a pre-existing history of low BMI in the early stages of life [21]. This may explain why a high BMI, as reported in our study, is protective against DKD.
Study limitations
We used a single-spot UACR measurement to determine participants with DKD. This could have led to an over-representation of the burden of DKD in this study population. We were also unable to screen for diabetic retinopathy, as recommended, to correlate the diagnosis of DKD, especially in patients with the albuminuric phenotype.
Conclusion
DKD especially the albuminuric phenotype was relatively frequent in these adult Ugandan patients with newly diagnosed diabetes. A positive association was observed between hypertension comorbidity and DKD while obesity had an inverse association. Measurement of UACR as a measure of assessing for DKD should be encouraged in clinical care, especially in patients with co-existing hypertension and BMI < 30 kg/m2.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AOR:
-
Adjusted odds ratio
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology formula
- DKD:
-
Diabetic kidney disease
- e-GFR:
-
Estimated glomerular filtration rate
- FBG:
-
Fasting blood glucose
- HbA1c:
-
Glycated haemoglobin
- HC:
-
Hip circumference
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- SSA:
-
Sub-Saharan Africa
- UACR-:
-
Urine albumin creatinine ratio
- WC-:
-
Waist circumference
- WHR-waist:
-
Hip circumference ratio
References
KDIGO: KDIGO. 2020 clinical practice Guideline for Diabetes Management in chronic kidney disease. Kidney Int. 2020;98(4s):1–s115.
Persson F, Rossing P. Diagnosis of diabetic kidney disease: state of the art and future perspective. Kidney Int Suppl (2011) 2018, 8(1):2–7.
Chen Y, Lee K, Ni Z, He JC. Diabetic kidney disease: challenges, advances, and Opportunities. Kidney Dis (Basel). 2020;6(4):215–25.
Noubiap JJN, Naidoo J, Kengne AP. Diabetic nephropathy in Africa: a systematic review. World J Diabetes. 2015;6(5):759–73.
Wagnew F, Eshetie S, Kibret GD, Zegeye A, Dessie G, Mulugeta H, Alemu A. Diabetic nephropathy and hypertension in diabetes patients of sub-saharan countries: a systematic review and meta-analysis. BMC Res Notes. 2018;11(1):565.
Stanifer JW, Jing B, Tolan S, Helmke N, Mukerjee R, Naicker S, Patel U. The epidemiology of chronic kidney disease in sub-saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(3):e174–181.
Chronic Kidney Disease Epidemiology (CKD-EPI) collaboration equation. https://qxmd.com/calculate/calculator_251/egfr-using-ckd-epi (accessed on 1/06/2020).
Tolossa T, Fetensa G, Regassa B, Yilma M, Besho M, Fekadu G, Wakuma B, Bekele D, Mulisa D. Burden and determinants of chronic kidney Disease among Diabetic Patients in Ethiopia: a systematic review and Meta-analysis. Public Health Rev 2021, 42(3).
Abd ElHafeez S, Bolignano D, D’Arrigo G, Dounousi E, Tripepi G, Zoccali C. Prevalence and burden of chronic kidney disease among the general population and high-risk groups in Africa: a systematic review. BMJ Open. 2018;8(1):e015069.
Choukem SP, Dzudie A, Dehayem M, Halle MP, Doualla MS, Luma H, Kengne AP. Comparison of different blood pressure indices for the prediction of prevalent diabetic nephropathy in a sub-saharan african population with type 2 diabetes. Pan Afr Med J. 2012;11:67.
Rotchford AP, Rotchford KM. Diabetes in rural South Africa–an assessment of care and complications. S Afr Med J. 2002;92(7):536–41.
Kalyesubula R, Hau J, Asiki G, Ssebunya B, Kusemererwa S, Seeley J, Smeeth L, Tomlinson L, Newton R. Impaired renal function in a rural ugandan population cohort [version 3; peer review: 2 approved]. Wellcome Open Research 2019, 3(149).
Retnakaran R, Cull CA, Thorne KI, Adler AI, Holman RR. Risk factors for renal dysfunction in type 2 diabetes: U.K. prospective diabetes study 74. Diabetes. 2006;55(6):1832–9.
Penno G, Solini A, Bonora E, Fondelli C, Orsi E, Zerbini G, Trevisan R, Vedovato M, Gruden G, Cavalot F, et al. Clinical significance of nonalbuminuric renal impairment in type 2 diabetes. J Hypertens. 2011;29(9):1802–9.
Yoshida Y, Kashiwabara K, Hirakawa Y, Tanaka T, Noso S, Ikegami H, Ohsugi M, Ueki K, Mita T, Watada H et al. Conditions, pathogenesis, and progression of diabetic kidney disease and early decliner in Japan. BMJ Open Diabetes Res Care 2020, 8(1).
Unnikrishnan RI, Rema M, Pradeepa R, Deepa M, Shanthirani CS, Deepa R, Mohan V. Prevalence and risk factors of diabetic nephropathy in an urban south indian population: the Chennai Urban Rural Epidemiology Study (CURES 45). Diabetes Care. 2007;30(8):2019–24.
Van Buren PN, Toto R. Hypertension in diabetic nephropathy: epidemiology, mechanisms, and management. Adv Chronic Kidney Dis. 2011;18(1):28–41.
Lopes de Faria JB, Silva KC, Lopes de Faria JM. The contribution of hypertension to diabetic nephropathy and retinopathy: the role of inflammation and oxidative stress. Hypertens Res. 2011;34(4):413–22.
Zhao Q, Yi X, Wang Z. Meta-analysis of the relationship between abdominal obesity and Diabetic kidney disease in type 2 Diabetic patients. Obes Facts. 2021;14(4):338–45.
Kalyesubula R, Nankabirwa JI, Ssinabulya I, Siddharthan T, Kayima J, Nakibuuka J, Salata RA, Mondo C, Kamya MR, Hricik D. Kidney disease in Uganda: a community based study. BMC Nephrol. 2017;18(1):116.
Luyckx VA, Brenner BM. Clinical consequences of developmental programming of low nephron number. Anat Rec (Hoboken). 2020;303(10):2613–31.
Funding
This study was supported by the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordat agreement (Project Reference: MC_UP_1204/16), and the National Institute for Health Research (NIHR) Global Health Research Grant (17/63/131).
The study sponsors were not involved in the design of the study, the collection, analysis and interpretation of data, and the writing of the report.
Author information
Authors and Affiliations
Contributions
DK oversaw the entire data collection process, and data interpretation, and wrote the initial draft of the manuscript. IS performed the statistical analysis, and data interpretation, and reviewed all the versions of the manuscript. WL contributed to data collection and interpretation and reviewed all the versions of the manuscript. All the authors read and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethical approval from the research ethics committee of the Uganda Virus Research Institute (GC/127/18/05/650) and the Uganda National Council of Science and Technology (HS 2431). All participating study sites offered administrative approval before the initiation of the study. All study participants recruited into the study offered written informed consent. All methods were performed in accordance with the relevant guidelines and regulations or declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
All the authors report no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kibirige, D., Sekitoleko, I. & Lumu, W. Burden and predictors of diabetic kidney disease in an adult Ugandan population with new-onset diabetes. BMC Res Notes 16, 234 (2023). https://doi.org/10.1186/s13104-023-06500-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-023-06500-1