Abstract
Background
The varied clinical presentations of Helicobacter pylori (H. pylori) infection are most likely due to differences in the virulence of individual strains, which determines its ability to induce production of interleukin-8 (IL-8) in the gastric mucosa. The aim of this study was to examine association between cagA, vacA- s1 and vacA- s2 genotypes of H. pylori and severity of chronic gastritis and presence of peptic ulcer disease (PUD), and to correlate these with IL-8 levels in the gastric mucosa.
Methods
Gastric mucosal biopsies were obtained from patients during esophagogastroduodenoscopy. The severity of chronic gastritis was documented using the updated Sydney system. H. pylori cagA and vacA genotypes were detected by PCR. The IL-8 levels in the gastric mucosa were measured by ELISA.
Results
H. pylori cagA and/or vacA genotypes were detected in 99 patients (mean age 38.4-12.9; 72 males), of whom 52.5% were positive for cagA, 44.4% for vacA-s1 and 39.4% for vacA-s2; and 70.7% patients had PUD. The severity of inflammation in gastric mucosa was increased with vacA-s1 (p=0.017) and decreased with vacA-s2 (p=0.025), while cagA had no association. The degree of neutrophil activity was not associated with either cagA or vacA-s1, while vacA-s2 was significantly associated with decreased neutrophil activity (p=0.027). PUD was significantly increased in patients with cagA (p=0.002) and vacA-s1 (p=0.031), and decreased in those with vacA-s2 (p=0.011). The level of IL-8 was significantly increased in patients with cagA (p=0.011) and vacA-s1 (p=0.024), and lower with vacA-s2 (p=0.004). Higher levels of IL-8 were also found in patients with a more severe chronic inflammation (p=0.001), neutrophil activity (p=0.007) and those with PUD (p=0.001).
Conclusions
Presence of vacA-s1 genotype of H. pylori is associated with more severe chronic inflammation and higher levels of IL-8 in the gastric mucosa, as well as higher frequency of PUD. Patients with vacA-s2 have less severe gastritis, lower levels of IL-8, and lower rates of PUD. The presence of cagA genotype is not associated with the severity of gastritis or IL-8 induction in the gastric mucosa. The association of cagA with PUD may be a reflection of its presence with vacA-s1 genotype.
Similar content being viewed by others
Background
Helicobacter pylori (H. pylori) colonizes the mucosa of the human stomach and establishes a long-term infection [1]. It leads to the development of chronic gastritis, peptic ulcer disease (PUD), mucosal-associated lymphoid tissue (MALT) lymphoma and gastric carcinoma [2],[3]. The extent and severity of these associations depend on several elements, such as bacterial virulence factors, age of the host, genetic susceptibility, immune response and environmental factors [4-6].
The two key virulence markers of H. pylori are the cytotoxin associated A (cagA) and the vacuolating cytotoxin A (vacA) genes [6],[7]. The cagA gene is not present in every H. pylori strain, but is associated with more severe clinical results such as more severe inflammation of the gastric mucosa, as well as higher prevalence of PUD and gastric carcinoma [8-10]. The vacA gene is present in all H. pylori strains and is associated with PUD [11]. The vacA gene contains at least three variable regions, the signal (s) region, intermediate (i) region and middle (m) region. The s-region exists as s1 and s2 types [12],[13]. The vacA-s1 strains are associated with more severe gastric inflammation and PUD independently of cagA, while vacA-s2 strains are associated with lower ulcer prevalence and less severe inflammation [14].
H. pylori infection results in recruitment of neutrophils, lymphocytes and macrophages into the gastric mucosa through the induction of several cytokines such as TNF-?, IL-6 and IL-8 [15-17]. IL-8 is an important mediator in the immunopathogenesis of chronic gastritis caused by H. pylori[16]. It has been demonstrated that cagA and vacA-s1 positive strains of H. pylori induce production of IL-8 in the gastric mucosa, both in vivo and in vitro [16],[18],[19]. The vacA-s2 gene is not associated with IL-8 induction [18]. In addition, an association between the mucosal levels of IL-8 and severity of gastritis and presence of PUD has also been reported [19]. Most studies of association between genotypes of H. pylori and chronic gastritis, peptic ulcer disease and IL-8 levels have been conducted in the Western populations, and no previous study has examined these associations in the Middle East. Furthermore, the majority of published studies have only examined either a single or some of these associations.
The aim of this study was to determine the association between the presence of cagA, vacA-s1 and vacA-s2 genotypes in H. pylori and the severity of gastritis and PUD, and to correlate these with the levels of IL-8 in a group of patients from the Middle East. We have also attempted to examine all these inter-related associations in the same group of patients to validate the biologic plausibility that the bacterial virulence factors lead to induction of the cytokine IL-8, which in turn results in more severe inflammation or development of PUD.
Results
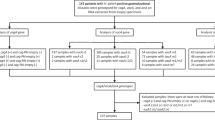
Esophagogastroduodenoscopy and gastric biopsies were performed in 120 adult patients. H. pylori were seen on histopathology in 98 of these patients, all of whom were positive for cagA and/or vacA. One patient had vacA on PCR but was not positive for H. pylori on histopathology was also included in the analysis. Therefore, further analysis was carried out in these 99 patients (72.7% males, 27.3% females; mean age 38.4 years) (Table 1). A history of PUD was present in 27.3% of the patients, and the most common indication for referral was dyspepsia (84.8%).
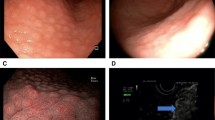
The most frequent abnormality seen on endoscopy was PUD (70.7%) (Table 2). Endoscopic evidence of mucosal inflammation of the stomach and duodenum was observed in 57.6% and 29.3% of the patients, respectively. Chronic inflammation was ‘None-Mild’ in 22.2% of the patients, and ‘Moderate-Marked’ in 77.8%. Neutrophil activity was ‘None-Mild’ in 60.6%, and ‘Moderate-Marked’ in 39.4% of the patients.
The presence of cagA, vacA-s1 and vacA-s2 genes was found in 52.5%, 44.4% and 39.4% of the patients, while 10.1% were positive for both vacA-s1 vacA- s2. The cagA gene was found in combination with vacA-s1 (cagA?+?vacA-s1) in 31.3% of the patients, with vacA-s2 (cagA?+?vacA-s2) in 8.1% and with both vacA-s1 and vacA-s2 (cagA?+?vacA-s1?+?s2) in 7.1% of the patients. The IL-8 levels were available in 77 patients with a median value of 1567.4 (IQR 1566.3) pg/mg protein.
Table 3 shows the association between the H. pylori genotypes and severity of chronic inflammation, neutrophil activity and presence of PUD. Patients who were infected with H. pylori containing both the cagA and vacA-s1 genes were most likely to have ‘Moderate-Marked’ degree of chronic inflammation (OR =?6.7, 95% CI: 1.4-31.4; p =?0.016). Patients with vacA-s1 gene alone also had a significantly more ‘Moderate-Marked’ degree of chronic inflammation (OR =?3.9, 95% CI: 1.2-12.0; p =?0.017), while those with vacA-s2 had significantly less chronic inflammation (OR =?0.3, 95% CI: 0.1-0.8; p =?0.025). The presence of cagA or vacA-s1 genes either independently or together did not affect the severity of neutrophil activity in the gastric biopsies. Patients with vacA-s2 gene had a significantly less ‘Moderate-Marked’ degree of neutrophil activity (OR =?0.3, 95% CI: 0.1-0.8; p =?0.027). The proportion of patients having PUD was highest in those with the cagA gene (OR =?4.8, 95% CI: 1.8-12.5; p =?0.002), followed by those with the vacA-s1 gene (OR =?2.8, 95% CI: 1.1-7.4; p =?0.031), while those with vacA-s2 had the lowest proportion of PUD (OR =?0.3, 95% CI: 0.1-0.7; p =?0.011). The presence of both cagA and vacA-s1 gene increased the risk of PUD more than the presence of these genotypes individually (OR =?6.3, 95% CI: 1.6-23.4; p =?0.006).
Table 4 shows the correlation between level of IL-8 in the gastric mucosa and H. pylori genotypes and histologic features and PUD. The median value for IL-8 was significantly higher in patients infected with H. pylori with cagA (p =?0.011) and vacA-s1 genes (p =?0.011 and 0.024, respectively); and significantly lower in those with vacA-s2 gene (p =?0.004) (Figure 1). The highest levels of IL-8 were found in patients who were positive for both cagA and vacA-s1 (Figure 2). Correlation of gastric mucosal IL-8 levels with the severity of chronic inflammation showed that patients who had ‘Moderate-Marked’ chronic inflammation had significantly higher median IL-8 level compared to those who had ‘None-Mild’ inflammation (p =?0.001) (Figure 3). Patients with ‘Moderate-Marked’ neutrophil activity on gastric biopsy also had significantly higher median IL-8 levels compared to those who had ‘None-Mild’ activity (p =?0.007). The median levels of IL-8 were also significantly elevated in the gastric biopsies of patients with PUD compared to those who did not have ulcers (p =?0.001). There was no significant difference in the density of H. pylori or degree of glandular atrophy or intestinal metaplasia with the IL-8 level in the gastric biopsies.
Levels of interleukin-8 in the gastric mucosa in patients with H. pylori with and without genotypes cagA , vacA -s1 and vacA -s2. These are expressed as box plots. The ends of the bars indicate the 25th and 75th percentiles. The 50th percentile is indicated with a line, and the 10th and 90th percentiles are indicated with error bars. The p-values were calculated using the Mann-Whitney U test. *indicates that the p-value is statistically significant.
Levels of interleukin-8 in the gastric mucosa in patients with H. pylori with and without genotypes cagA?+?vacA -s1, cagA?+?vacA -s2 and cagA?+?vacA -s1?+?vacA -s2. These are expressed as box plots. The ends of the bars indicate the 25th and 75th percentiles. The 50th percentile is indicated with a line, and the 10th and 90th percentiles are indicated with error bars. The p-values were calculated using the Mann-Whitney U test. *indicates that the p-value is statistically significant.
Levels of interleukin-8 in the gastric mucosa in patients with H. pylori and severity of chronic inflammation, neutrophil activity and peptic ulcer disease. These are expressed as box plots. The ends of the bars indicate the 25th and 75th percentiles. The 50th percentile is indicated with a line, and the 10th and 90th percentiles are indicated with error bars. The p-values were calculated using the Mann-Whitney U test. * indicates that the p-value is statistically significant.
A total of 58 (75.3%) patients who had ‘Moderate-Marked’ chronic inflammation in the gastric mucosa had PUD, compared to 12 (54.5%) with ‘None-Mild‘ while 31 (79.5%) patients with ‘Moderate-Marked’ neutrophil activity had PUD, compared to 39 (65.0%) of those with ‘None-Mild’ activity. However these differences were not statistically significant. There was also no association between the presence of PUD and severity of glandular atrophy, intestinal metaplasia or H. pylori density on gastric biopsies.
Discussion
To our knowledge, this is the first study to examine the association between the presence of cagA, vacA-s1 and vacA-s2 genotypes in H. pylori and the severity of chronic gastritis and PUD in a group of patients from the Middle East. We have also demonstrated the relationship of these factors with the levels of IL-8 in the gastric mucosa validating the biologic plausibility that these bacterial virulence factors lead to induction of the cytokine IL-8, which in turn results in more severe inflammation and/or development of PUD.
There appears to be a geographic variation in the association between H. pylori genotypes and gastric inflammatory response. Infection with cagA positive strains of H. pylori in Western countries is reported to cause more severe gastric inflammation compared to Asian countries, where the results have been inconsistent [7],[20-24]. In our study both the degree of chronic inflammation and neutrophil activity in the gastric mucosa were more severe in patients who were infected with H. pylori containing the cagA and vacA-s1 genes. The presence of both cagA and vacA-s1 appeared to have a synergistic role in increasing the severity of inflammation in our patients. On the other hand, the presence of vacA-s2 appeared to improve the severity of chronic inflammation as well as neutrophil activity regardless of the presence of cagA, vacA-s1 or both. These findings are consistent with previously published studies where vacA-s2 strains were found to be associated with less inflammation [25]. Both the cagA and vacA-s1 genes were also independently associated with an increased risk of PUD, while the vacA-s2 gene appeared to have a lesser effect. Patients who had both the cagA and the vacA-s1 gene had the highest risk of PUD. On the other hand, the presence of vacA-s2 decreased the risk of PUD, whether it was present alone or with cagA, vacA-s1, or both. These results are similar to those reported from the Western countries [20],[21],[24], even though the majority of the patients in our study were from the Middle East and the Indian Subcontinent [26]. A recent study conducted to determine the genetic affinities of H. pylori isolates from ethnic Arabs in Kuwait found that these strains are closely related to the Indo-European group of the organism and clearly distinct from the East Asian strains [27]. This could be the reason why the association of cagA, vacA-s1 and vacA-s2 and gastritis and PUD in our patients seems to be similar to that reported from the Western countries.
The pro-inflammatory cytokine IL-8 plays an important role in the regulation of mucosal neutrophil migration and activation. Our results show that the level of IL-8 in the gastric mucosa was increased in presence of cagA and vacA-s1 genotypes of H. pylori and the highest levels were seen in patients who were positive for both these genes. The presence of vacA-s2 was associated with lower levels of IL-8. Significantly higher levels of IL-8 in the gastric mucosa were also seen in patients who had more severe degree of chronic inflammation and neutrophil activity in the gastric biopsies, as well as those who had PUD. These results are in agreement with previous reports where the levels of gastric mucosal IL-8 levels have been correlated with the presence of virulence H. pylori genes such as cagA and ice A [28],[29]. However, some researchers have reported no difference in the IL-8 levels in patients with H. pylori infections with and without PUD [30], while others have higher levels in patients with PUD then those with only gastritis [31]. This inconsistency in the results of IL-8 production could be because of the differences in the methodologies used to measure the level of the cytokine in the gastric mucosa. We have used an ELISA based technique, which may be a more sensitive method of cytokine quantification.
With reference to other factors, we found no difference in the severity of gastritis, presence of PUD or levels of IL-8 between patients with or without history of smoking or alcohol consumption. The presence of PUD was however more frequent in this group of patients than has been reported previously from Kuwait as well as elsewhere [32]. The confounding effects of medications were minimized by only selecting those patients who had not been on any of the mentioned medications for at least 4 weeks prior to endoscopy. Several other H. pylori factors such as vacA-s1 subtypes (s1a and s1b), vacA middle region subtypes (m1 and m2), iceA and dupA genes can also affect the virulence of this organism and its effects on the gastric mucosa [33]. However, our study was not designed to determine these virulence factors, and this could be considered a limitation of this report. Besides bacterial factors, host genetics also contribute to the pathogenesis of gastroduodenal diseases [34],[35]. In addition, many cytokine gene polymorphisms reveal different risk in gastric and duodenal ulcer patients [36],[37].
Conclusions
This study which included patients from the Middle East shows that presence of H. pylori cagA and vacA-s1 genes results in induction of higher levels of the pro-inflammatory cytokine IL-8 in the gastric mucosa, which not only results in a more marked intensity of chronic inflammation and neutrophil activity in the gastric mucosa but also a higher occurrence of PUD. The presence of vacA-s2 results in lower levels of IL-8, as well as less severe inflammation and less PUD. In addition the presence of vacA-s2 appears to lessen the virulence effects of cagA and/or vacA-s1 genes.
Patients and methods
Patients and samples
The study population and the method of biopsy collection have been described previously [26],[32]. Briefly, 120 consecutive, unselected adult patients referred for esophagogastroduodenoscopy were invited to participate in the study. Patients with coagulation abnormalities, prior gastro-duodenal surgery were excluded from the study. Patients who had taken histamine type 2 receptor antagonists, proton pump inhibitors, antibiotics, bismuth salts, aspirin or non-steroidal anti-inflammatory agents in the preceding four weeks were also excluded. The prevalence of cagA and vacA genotypes in these patients has been reported earlier [26].
Upper gastrointestinal endoscopy was performed in a standard manner. All endoscopes underwent a cleaning and disinfection process with an automated washer-disinfector before each procedure according to guidelines of the European Society of Gastrointestinal Endoscopy [38]. For each patient, four biopsies were taken from the gastric antrum, within 2 cm of the pylorus, using sterilized biopsy forceps.
Two biopsy specimens were fixed in buffered formalin, processed to paraffin, sectioned and stained with H&E and the HpSS [39]. All biopsies were examined individually by a senior gastrointestinal pathologist who was blinded to the clinical information about the patients. A biopsy was scored positive for H. pylori if organisms were seen on light microscopy. The updated Sydney system was used to score the density of H. pylori and degree of chronic inflammation, neutrophil activity, glandular atrophy and intestinal metaplasia on the biopsies [40]. Patients who had no or mild chronic inflammation in the gastric biopsy were combined in one group (None-Mild group), while those with moderate or marked degree of inflammation were included in the other group (Moderate-Marked group). Similarly, patients were divided into two groups (i.e. None-Mild and Moderate-Marked) for neutrophil activity, as well as for intestinal metaplasia and glandular atrophy.
The QIA’ DNA mini kit (Qiagen, Hilden, Germany) was used to extract DNA from the biopsies. The purity of DNA was assessed calculating the ratio of optical density (OD) at 260-280 nm and the yield was quantified by absorbance at 260 nm.
PCR amplification of target DNA
Table 5 shows the primers used in this study. The cagA F and cagA R primers generate a fragment of 183 base pairs (bp) for the detection of cagA, while primers VA1F and VA1XRA yield a 176 bp fragment for vacA-s1 and 203 bp for vacA-s2 variants [41],[42]. A pre-aliquoted PCR master mix (Abgene, Surrey, UK) was used for PCR amplification of target DNA. The final reaction volume was 50L and contained 25pmol of each primer and 50 ng DNA [43]. PCR was performed after preincubation at 94°C for 5 minutes, followed by 35 cycles at 94°C , 50°C and 74°C for one minute each followed by a 5 minutes final extension step at 74°C. The amplified samples were analyzed by electrophoresis on 2% high-resolution agarose gel in Tris-Acetate-EDTA (TAE) buffer, which was then stained with ethidium bromide at 0.5μg/ml [44]. Ultraviolet light was used to visualize the bands of amplified DNA, which were then photographed.
Measurement of IL-8
Two biopsy specimens were frozen immediately in liquid nitrogen and stored at ?80°C. These samples were later homogenized with 1 mL phosphate buffered saline (pH 7.4) for 1 minute at 4°C. The homogenate was then centrifuged for 10 minutes at 14,000 rpm. The supernatant obtained was used for estimation of IL-8 level as well as total protein measurement [45-47]. The IL-8 concentration was measured by IL-8 ELISA kit (Immunotech, Hamburg, Germany) in a sandwich type assay using the procedure recommended by the manufacturer. The modified Lowry method was used to measure the total protein in the homogenate [48]. The amount of IL-8 in the gastric mucosal biopsies was expressed as pg/mg protein.
Statistical analysis
The Student’s t-test was used to compare the difference between two means. We evaluated the association of PUD and severity of inflammation with the three H. pylori genotypes (cagA, vacA-s1 and vacA-s2) and their combinations. As our outcome measures were binary variables, we used univariate logistic regression models to test if any of the genotypes or their combinations are related to presence of the PUD or severity of inflammation. The strength of the association between these variables obtained from the regression models was expressed as the odds ratio (OR) and 95% Confidence Interval (95% CI) along with p-values. Further multivariate logistic regression models were used to obtain age and gender adjusted estimates of these effects. We used Mann-Whitney U tests to evaluate if the levels of IL-8 correlated with varying genotypes or their combinations, severity of inflammation and presence of PUD. We used non-parametric method as the cytokines were not normally distributed. A p-value of <0.05 was considered statistically significant. All p-values presented are two sided. The data were analyzed using the SPSS software (SPSS Inc., Chicago, IL, USA).
The protocol for the study, and the statement of informed consent, was approved by the ethical committee of the Medical Research Council of the Health Sciences Center at Kuwait University and conforms to the provisions of the World Medical Association’s Declaration of Helsinki in 1995 (as revised in Tokyo 2004). All patients gave an informed consent prior to inclusion in the study.
Authors’ contributions
IS, AAQ, ASM and TAJ conceived and designed the study. IS, AAQ, ASM and TAJ collected the data. IS, AAQ, ASM and TAJ carried out experiments. IS, AAQ and AM statistically analyzed and interpreted the data. IS, AAQ, JAA and WA did literature research. IS generated the figures and tables. IS wrote the manuscript with help of AAQ, ASM, AM and TAJ. IS, AM. AAQ, ASM, TAJ, JAA and WA revised the paper. IS had full access to all of the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis. All authors had final approval of the submitted and published versions.
References
Eusebi LH, Zagari RM, Bazzoli F: Epidemiology of Helicobacter pylori Infection. Helicobacter. 2014, 19 (Suppl 1): 1-5. 10.1111/hel.12165.
Malnick SD, Melzer E, Attali M, Duek G, Yahav J: Helicobacter pylori: Friend or foe?. World J Gastroenterol. 2014, 20: 8979-8985.
Marshall BJ, Windsor HM: The relation of Helicobacter pylori to gastric adenocarcinoma and lymphoma: pathophysiology, epidemiology, screening, clinical presentation, treatment, and prevention. Med Clin North Am. 2005, 89: 313-344. 10.1016/j.mcna.2004.09.001.
O’Keeffe J, Moran AP: Conventional, regulatory, and unconventional T cells in the immunologic response to helicobacter pylori. Helicobacter. 2008, 13: 1-19. 10.1111/j.1523-5378.2008.00559.x.
Basso D, Plebani M, Kusters JG: Pathogenesis of Helicobacter pylori infection. Helicobacter. 2010, 15 (Suppl 1): 14-20. 10.1111/j.1523-5378.2010.00781.x.
de Bernard M, Josenhans C: Pathogenesis of Helicobacter pylori Infection. Helicobacter. 2014, 19 (Suppl 1): 11-18. 10.1111/hel.12160.
Umit H, Tezel A, Bukavaz S, Unsal G, Otkun M, Soylu AR, Tucer D, Otkun M, Bilgi S: The relationship between virulence factors of Helicobacter pylori and severity of gastritis in infected patients. Dig Dis Sci. 2009, 54: 103-110. 10.1007/s10620-008-0316-9.
Almeida N, Donato MM, Romãozinho JM, Luxo C, Cardoso O, Cipriano MA, Marinho C, Fernandes A, Sofia C: Correlation of helicobacter pylori genotypes with gastric histopathology in the central region of a south-European Country.Dig Dis Sci 2014, [Epub ahead of print].,
Kim JY, Kim N, Nam RH, Suh JH, Chang H, Lee JW, Kim YS, Kim JM, Choi JW, Park JG, Lee YS, Lee DH, Jung HC: Association of polymorphisms in virulence factor of Helicobacter pylori and gastroduodenal diseases in South Korea. J Gastroenterol Hepatol. 2014, 29: 984-991. 10.1111/jgh.12509.
Yamaoka Y, Graham DY: Helicobacter pylori virulence and cancer pathogenesis. Future Oncol. 2014, 10: 1487-1500. 10.2217/fon.14.29.
Memon AA, Hussein NR, Miendje Deyi VY, Burette A, Atherton JC: Vacuolating cytotoxin genotypes are strong markers of gastric cancer and duodenal ulcer-associated Helicobacter pylori strains: a matched case-control study. J Clin Microbiol. 2014, 52: 2984-2989. 10.1128/JCM.00551-14.
Atherton JC, Cao P, Peek RM, Tummuru MK, Blaser MJ, Cover TL: Mosaicism in vacuolating cytotoxin alleles of Helicobacter pylori. Association of specific vacA types with cytotoxin production and peptic ulceration. J Biol Chem. 1995, 270: 17771-17777. 10.1074/jbc.270.30.17771.
Rhead JL, Letley DP, Mohammadi M, Hussein N, Mohagheghi MA, Eshagh Hosseini M, Atherton JC: A new Helicobacter pylori vacuolating cytotoxin determinant, the intermediate region, is associated with gastric cancer. Gastroenterology. 2007, 133: 926-936. 10.1053/j.gastro.2007.06.056.
Matos JI, de Sousa HA, Marcos-Pinto R, Dinis-Ribeiro M: Helicobacter pylori CagA and VacA genotypes and gastric phenotype: a meta-analysis. Eur J Gastroenterol Hepatol. 2013, 25: 1431-1441. 10.1097/MEG.0b013e328364b53e.
Bodger K, Bromelow K, Wyatt JI, Heatley RV: Interleukin 10 in Helicobacter pylori associated gastritis: immunohistochemical localisation and in vitro effects on cytokine secretion. J Clin Pathol. 2001, 54: 285-292. 10.1136/jcp.54.4.285.
Hisatsune J, Nakayama M, Isomoto H, Kurazono H, Mukaida N, Mukhopadhyay AK, Azuma T, Yamaoka Y, Sap J, Yamasaki E, Yahiro K, Moss J, Hirayama T: Molecular characterization of Helicobacter pylori VacA induction of IL-8 in U937 cells reveals a prominent role for p38MAPK in activating transcription factor-2, cAMP response element binding protein, and NF-kappaB activation. J Immunol. 2008, 180: 5017-5027. 10.4049/jimmunol.180.7.5017.
Lee KE, Khoi PN, Xia Y, Park JS, Joo YE, Kim KK, Choi SY, Jung YD: Helicobacter pylori and interleukin-8 in gastric cancer. World J Gastroenterol. 2013, 19: 8192-8202. 10.3748/wjg.v19.i45.8192.
Audibert C, Janvier B, Grignon B, Salaün L, Burucoa C, Lecron JC, Fauchère JL: Correlation between IL-8 induction, cagA status and vacA genotypes in 153 French Helicobacter pylori isolates. Res Microbiol. 2000, 151: 191-200. 10.1016/S0923-2508(00)00139-X.
Bartchewsky W, Martini MR, Masiero M, Squassoni AC, Alvarez MC, Ladeira MS, Salvatore D, Trevisan M, Pedrazzoli J, Ribeiro ML: Effect of Helicobacter pylori infection on IL-8, IL-1beta and COX-2 expression in patients with chronic gastritis and gastric cancer. Scand J Gastroenterol. 2009, 44: 153-161. 10.1080/00365520802530853.
Soltermann A, Koetzer S, Eigenmann F, Komminoth P: Correlation of Helicobacter pylori virulence genotypes vacA and cagA with histological parameters of gastritis and patient’s age. Mod Pathol. 2007, 20: 878-883. 10.1038/modpathol.3800832.
Gunn MC, Stephens JC, Stewart JA, Rathbone BJ, West KP: The significance of cagA and vacA subtypes of Helicobacter pylori in the pathogenesis of inflammation and peptic ulceration. J Clin Pathol. 1998, 51: 761-764. 10.1136/jcp.51.10.761.
Demirtürk L, Ozel AM, Yazgan Y, Solmazgül E, Yildirim S, Gültepe M, Gürbüz AK: CagA status in dyspeptic patients with and without peptic ulcer disease in Turkey: association with histopathologic findings. Helicobacter. 2001, 6: 163-168. 10.1046/j.1523-5378.2001.00024.x.
Saruc M, Demir MA, Kücükmetin N, Kandiloglu AR, Akarca US, Yüceyar H: Histological and clinical predictive value of determination of tissue CagA status by PCR in Helicobacter pylori infected patients; results of the large population based study in western Turkey. Hepatogastroenterology. 2002, 49: 878-881.
Warburton VJ, Everett S, Mapstone NP, Axon AT, Hawkey P, Dixon MF: Clinical and histological associations of cagA and vacA genotypes in Helicobacter pylori gastritis. J Clin Pathol. 1998, 51: 55-61. 10.1136/jcp.51.1.55.
Atherton JC, Peek RM, Tham KT, Cover TL, Blaser MJ: Clinical and pathological importance of heterogeneity in vacA, the vacuolating cytotoxin gene of Helicobacter pylori. Gastroenterology. 1997, 112: 92-99. 10.1016/S0016-5085(97)70223-3.
Al Qabandi A, Mustafa AS, Siddique I, Khajah AK, Madda JP, Junaid TA: Distribution of vacA and cagA genotypes of Helicobacter pylori in Kuwait. Acta Trop. 2005, 93: 283-288. 10.1016/j.actatropica.2005.01.004.
Albert MJ, Al-Akbal HM, Dhar R, De R, Mukhopadhyay AK: Genetic affinities of Helicobacter pylori isolates from ethnic Arabs in Kuwait. Gut Pathog. 2010, 2: 6-10.1186/1757-4749-2-6.
Ma YJ, Duan GC, Zhang RG, Fan QT, Zhang WD: Mutation of iceA in Helicobacter pylori compromised IL-8 induction from human gastric epithelial cells. J Basic Microbiol. 2010, 50 (Suppl 1): S83-S88. 10.1002/jobm.200900410.
Naito M, Eguchi H, Goto Y, Kondo T, Nishio K, Ishida Y, Kawai S, Okada R, Hishida A, Wakai K, Hamajima N: Associations of plasma IL-8 levels with Helicobacter pylori seropositivity, gastric atrophy, and IL-8-T-251A genotypes. Epidemiol Infect. 2010, 138: 512-518. 10.1017/S0950268809990677.
Noach LA, Bosma NB, Jansen J, Hoek FJ, van Deventer SJ, Tytgat GN: Mucosal tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-8 production in patients with Helicobacter pylori infection. Scand J Gastroenterol. 1994, 29: 425-429. 10.3109/00365529409096833.
Peek RM, Miller GG, Tham KT, Perez-Perez GI, Zhao X, Atherton JC, Blaser MJ: Heightened inflammatory response and cytokine expression in vivo to cagA?+?Helicobacter pylori strains. Lab Invest. 1995, 73: 760-770.
Siddique I, Al-Mekhaizeem K, Alateeqi N, Memon A, Hasan F: Diagnosis of Helicobacter pylori: improving the sensitivity of CLOtest by increasing the number of gastric antral biopsies. J Clin Gastroenterol. 2008, 42: 356-360. 10.1097/MCG.0b013e31802b650d.
Alam J, Maiti S, Ghosh P, De R, Chowdhury A, Das S, Macaden R, Devarbhavi H, Ramamurthy T, Mukhopadhyay AK: Significant association of the dupA gene of Helicobacter pylori with duodenal ulcer development in a South-east Indian population. J Med Microbiol. 2012, 61: 1295-1302. 10.1099/jmm.0.038398-0.
Höcker M, Hohenberger P: Helicobacter pylori virulence factors-one part of a big picture. Lancet. 2003, 362: 1231-1233. 10.1016/S0140-6736(03)14547-3.
Varon C, Mosnier JF, Lehours P, Matysiak-Budnik T, Mégraud F: Gastric carcinogenesis and Helicobacter pylori infection. Methods Mol Biol. 2009, 511: 237-265. 10.1007/978-1-59745-447-6_10.
Wex T, Bornschein J, Malfertheiner P: Host polymorphisms of immune regulatory genes as risk factors for gastric cancer. Minerva Gastroenterol Dietol. 2009, 55: 395-408.
Lanas A, García-González MA, Santolaria S, Crusius JB, Serrano MT, Benito R, Pena AS: TNF and LTA gene polymorphisms reveal different risk in gastric and duodenal ulcer patients. Genes Immun. 2001, 2: 415-421. 10.1038/sj.gene.6363798.
Guidelines on cleaning and disinfection in GI endoscopy. Update 1999. Endoscopy. 2000, 32: 77-80.
Doglioni C, Turrin M, Macrì E, Chiarelli C, Germanà B, Barbareschi M: HpSS: a new silver staining method for Helicobacter pylori. J Clin Pathol. 1997, 50: 461-464. 10.1136/jcp.50.6.461.
Dixon MF, Genta RM, Yardley JH, Correa P: Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996, 20: 1161-1181. 10.1097/00000478-199610000-00001.
van Doorn LJ, Figueiredo C, Sanna R, Plaisier A, Schneeberger P, de Boer W, Quint W: Clinical relevance of the cagA, vacA, and iceA status of Helicobacter pylori. Gastroenterology. 1998, 115: 58-66. 10.1016/S0016-5085(98)70365-8.
van Doorn LJ, Figueiredo C, Rossau R, Jannes G, van Asbroek M, Sousa JC, Carneiro F, Quint WG: Typing of Helicobacter pylori vacA gene and detection of cagA gene by PCR and reverse hybridization. J Clin Microbiol. 1998, 36: 1271-1276.
De Gusmão VR, Nogueira Mendes E, De Magalhães Queiroz DM, Aguiar Rocha G, Camargos Rocha AM, Ramadan Ashour AA, Teles Carvalho AS: vacA genotypes in Helicobacter pylori strains isolated from children with and without duodenal ulcer in Brazil. J Clin Microbiol. 2000, 38: 2853-2857.
Mustafa AS, Ahmed A, Abal AT, Chugh TD: Establishment and evaluation of a multiplex polymerase chain reaction for detection of mycobacteria and specific identification of Mycobacterium tuberculosis complex. Tuber Lung Dis. 1995, 76: 336-343. 10.1016/S0962-8479(05)80033-4.
Yamaoka Y, Kita M, Kodama T, Sawai N, Kashima K, Imanishi J: Induction of various cytokines and development of severe mucosal inflammation by cagA gene positive Helicobacter pylori strains. Gut. 1997, 41: 442-451. 10.1136/gut.41.4.442.
Zhang QB, Etolhi G, Dawodu JB, Husain A, Gemmell CG, Russell RI: Relationship between mucosal levels of interleukin 8 and toxinogenicity of Helicobacter pylori. Inflammopharmacology. 1998, 6: 109-117. 10.1007/s10787-998-0028-y.
Yamamoto S, Kaneko H, Konagaya T, Mori S, Kotera H, Hayakawa T, Yamaguchi C, Uruma M, Kusugami K, Mitsuma T: Interactions among gastric somatostatin, interleukin-8 and mucosal inflammation in Helicobacter pylori-positive peptic ulcer patients. Helicobacter. 2001, 6: 136-145. 10.1046/j.1523-5378.2001.00020.x.
Noble JE, Bailey MJ: Quantitation of protein. Methods Enzymol. 2009, 463: 73-95. 10.1016/S0076-6879(09)63008-1.
Acknowledgements
The authors thank Dr. Lukman Thalib for providing statistical advice.
Disclaimer
This work has been presented as a poster at the Digestive Disease Week (DDW®) 2012, in San Diego, California, USA in May 2012 and the abstract was published in Gastroenterology (2012;142:S-472-S-473).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they hare no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Siddique, I., Al-Qabandi, A., Al-Ali, J. et al. Association between Helicobacter pylori genotypes and severity of chronic gastritis, peptic ulcer disease and gastric mucosal interleukin-8 levels: Evidence from a study in the Middle East. Gut Pathog 6, 41 (2014). https://doi.org/10.1186/s13099-014-0041-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13099-014-0041-1