Abstract
Background
Malnutrition and inflammation are associated with adverse clinical outcomes in patients with diabetes or coronary artery disease (CAD). Prognostic nutritional index (PNI) is a comprehensive and simple indicator reflecting nutritional condition and immunological status. Whether there is a crosstalk between nutritional-immunological status and diabetes status for the impact on the prognosis of coronary artery disease (CAD) is unclear.
Methods
A total of 9429 consecutive CAD patients undergoing percutaneous coronary intervention were grouped by diabetes status [diabetes (DM) and non-diabetes (non-DM)] and preprocedural PNI level [high PNI (H-PNI) and low PNI (L-PNI)] categorized by the statistically optimal cut-off value of 48.49. The primary endpoint was all-cause death.
Results
During a median follow-up of 5.1 years (interquartile range: 5.0–5.1 years), 366 patients died. Compared with the non-DM/H-PNI group, the DM/L-PNI group yielded the highest risk of all-cause death (adjusted hazard ratio: 2.65, 95% confidence interval: 1.97–3.56, p < 0.001), followed by the non-DM/L-PNI group (adjusted hazard ratio: 1.44, 95% confidence interval: 1.05–1.98, p = 0.026), while DM/H-PNI was not associated with the risk of all-cause death. The negative effect of L-PNI on all-cause death was significantly stronger in diabetic patients than in nondiabetic patients (p for interaction = 0.037). Preprocedural PNI category significantly improved the Global Registry of Acute Coronary Events (GRACE) risk score for predicting all-cause death in patients with acute coronary syndrome, especially in those with diabetes.
Conclusions
CAD patients with diabetes and L-PNI experienced the worst prognosis. The presence of diabetes amplifies the negative effect of L-PNI on all-cause death. Poor nutritional-immunological status outweighs diabetes in increasing the risk of all-cause death in CAD patients. Preprocedural PNI can serve as an assessment tool for nutritional and inflammatory risk and an independent prognostic factor in CAD patients, especially in those with diabetes.
Similar content being viewed by others
Backgroud
Malnutrition, manifested as altered body composition and diminished biological function, is not rare in patients with coronary artery disease (CAD) and has been reported to be associated with adverse clinical outcomes [1]. Inflammation has been recognized as a key mediator in the negative impact of malnutrition on the prognosis of cardiovascular disease [2]. Prognostic Nutritional Index (PNI) was first introduced by Buzby et al. in the context of gastrointestinal surgery [3] and modified by Onodera et al. [4]. Calculated from serum albumin levels and absolute lymphocyte counts, this simple and comprehensive index reflects not only protein stores but also the immunological status. Its prognostic value has been examined in malignancy [5], autoimmune disease [6], and heart failure [7,8,9,10,11,12] and has been reported in several small-scale studies for patients with acute coronary syndrome (ACS) or stable CAD [13,14,15,16].
Diabetes is a common cardiovascular risk factor and has been reported to be associated with increased risk of malnutrition [17]. Both malnutrition and diabetes affect systemic metabolism and exacerbate inflammation, driving the development of CAD. However, noModification of Diet in Renal Disease studies have examined how diabetes and coexisting malnutrition affect the prognosis of CAD. Only one study so far has reported the prevalence and prognostic value of malnutrition in CAD patients accompanied by diabetes [18]. Accordingly, this study aimed to investigate the joint effect and interaction between nutritional-immunological status assessed by PNI and diabetes status on the prognosis of the overall CAD population.
Methods
Study design, setting, and participants
From January 2013 to December 2013, the cohort study prospectively recruited 10,724 consecutive patients undergoing percutaneous coronary intervention (PCI) at Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences, Beijing, China. PCI was performed by experienced interventional cardiologists blinded to the study protocol. Details on catheterization procedures and periprocedural medication were in line with contemporaneous practice guidelines in China. At discharge, all patients without documented contraindications were prescribed statins and dual anti-platelet therapy with aspirin plus clopidogrel. Other cardiovascular medications, such as β-blockers, angiotensin-converting enzyme inhibitors, or angiotensin-receptor blockers, were prescribed according to patients' conditions and contemporaneous guidelines. Baseline and angiography data were extracted from the electronic medical record. Patients were followed up since the date of PCI. Follow-up and outcome information was obtained through clinic visits or telephone interviews by an independent group of clinical research coordinators at one, six, 12, 24 months, and 5 years after discharge. Investigator training and telephone recording were conducted to achieve high-quality results. Endpoint events were adjudicated by two independent cardiologists, and disagreement was resolved by consensus. This study complied with the Declaration of Helsinki. The Ethics Committee of Fuwai Hospital, National Center for Cardiovascular Diseases, approved the study protocol before enrolment (No. 2013–449). All participants provided written informed consent before intervention.
This post hoc analysis investigated the joint effect and interaction between PNI level and diabetes status on 5 year outcomes for CAD patients after PCI. Exclusion criteria were age less than 18 years, unsuccessful PCI, bare-metal stent implantation, end-stage liver or renal disease, systemic inflammatory disease, and missing preprocedural serum albumin and absolute lymphocyte counts data. Participants entering the final analysis were stratified by diabetes status (diabetes [DM] and non-diabetes [non-DM]) and further categorized by the optimal cut-off value of preprocedural PNI (high PNI [H-PNI] and low PNI [L-PNI]) into four groups.
Blood sampling and laboratory testing
Preprocedural blood samples were collected after emergency admission for unstable patients and after fasting for at least 12 h for stable patients. Postprocedural blood samples were collected within 24 h after PCI. Fasting blood glucose was assayed by an enzymatic hexokinase method. Glycated hemoglobin was assayed using a Tosoh Automated Glycohemoglobin Analyzer (HLC-723G8, Tokyo, Japan). Blood cell counts were measured by an automated blood cell counter. Serum albumin was measured using an automated chemistry analyzer (AU5400, Olympus, Japan) by the bromocresol green dye method. PNI was calculated as 10 × serum albumin (g/L) + 5 × absolute lymphocyte counts (109/L). Estimated glomerular filtration rate was calculated with the modified Modification of Diet in Renal Disease equation [19].
Outcomes and covariables
The primary endpoint was all-cause death. Secondary endpoints included cardiac death, non-fatal myocardial infarction (MI), non-fatal stroke, unplanned revascularization, and major adverse cardiovascular and cerebrovascular events. All deaths were considered cardiac unless an unequivocal non-cardiac cause could be established. MI was diagnosed based on the Third Universal Definition of Myocardial Infarction. Strokes included ischemic stroke, hemorrhagic stroke, and transient ischemic attack. Unplanned revascularization was defined as repeated coronary artery bypass grafting or PCI of any vessel driven by ischemic symptoms and events.
Body mass index ≥ 25 kg/m2 was considered obese based on the World Health Organization standard for Asian populations [20]. Diabetes was defined as fasting blood glucose ≥ 7.0 mmol/L, glycated hemoglobin ≥ 6.5%, oral antidiabetic medication or insulin use, or self-reported diabetes. Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, antihypertensive medication use, or self-reported hypertension. Dyslipidemia was diagnosed when at least one of the following criteria was met: total cholesterol ≥ 6.22 mmol/L, total triglyceride ≥ 2.26 mmol/L, low-density lipoprotein cholesterol ≥ 4.14 mmol/L, high-density lipoprotein cholesterol < 1.04 mmol/L, lipid-lowering medication use, or self-reported dyslipidemia [21].
Statistical analysis
Preprocedural PNI was categorized by the statistically optimal cut-off value for predicting all-cause death determined by recursive partitioning and log-rank tests. Baseline characteristics were compared using Mann–Whitney U tests, Kruskal–Wallis tests, or χ2 tests as appropriate. Categorical and continuous variables were expressed as numbers (percentages) and median [interquartile range], respectively. Correlation between preprocedural PNI and glycemic measures was assessed using Spearman rank correlation analysis.
Survival curves were plotted using Kaplan–Meier method and compared using log-rank tests. Association of preprocedural PNI category and diabetes status with clinical outcomes was examined using Cox proportional-hazards regression by estimating hazard ratios (HRs) and 95% confidence intervals (CIs). Covariables for adjustment included sex, age, hypertension, chronic obstructive pulmonary disease, previous revascularization, previous MI, previous stroke, high-sensitivity C-reactive protein, estimated glomerular filtration rate, and left ventricular ejection fraction, according to clinical plausibility and significance in univariate analysis. In addition, an inverse probability of treatment weighting analysis based on propensity score was undertaken. The propensity score was calculated by logistic regression with variables related to DM, PNI, and/or the outcomes.
Subgroup analysis for all-cause death was performed according to four variables of interest: age (≥ 65 years versus < 65 years), sex (women versus men), body mass index (≥ 25 kg/m2 versus < 25 kg/m2), and admission presentation (ACS versus chronic coronary syndrome). In sensitivity analysis for all-cause death, we applied five indexes: (1) preprocedural dichotomous PNI grouped by median; (2) preprocedural continuous PNI; (3) postprocedural PNI categorized by the optimal cut-off value; (4) the change in PNI before and after PCI (ΔPNI); (5) malnutrition defined based on the Global Leadership Initiative on Malnutrition (GLIM) criteria [10, 22]—an etiological criterion of inflammation (high-sensitivity C-reactive protein > 3.0 mg/L) plus any of the following phenotypic criteria: low body mass index (< 18.5 kg/m2 if < 70 years, or < 20.0 kg/m2 if ≥ 70 years) or reduced muscle mass (free fat mass index < 17.0 kg/m2 in men or < 15.0 kg/m2 in women). Association of preprocedural continuous PNI and ΔPNI with all-cause death was examined with restricted cubic splines with 4 knots.
The added value of the six indexes beyond the Global Register Acute Coronary Events (GRACE) risk score for the ACS population was evaluated by receiver operating characteristic curves and the decision curve analysis and was compared by the area under the curve (AUC), net reclassification improvement (NRI), and integrated discrimination improvement (IDI).
Statistical analyses were conducted with R version 4.2.0 (R Core Team 2022, Vienna, Austria. www.R-project.org). Figures were created by GraphPad Prism version 9.0.0 (GraphPad Software, San Diego, California, USA, www.graphpad.com). Two-tailed p-values of < 0.05 were considered statistically significant.
Results
Study population and baseline characteristics
The study population comprised 10,263 patients, of which 9429 (91.87%) patients with complete 5 year follow-up data were available for the final analysis. The number of participants at each stage is described in Additional file 1: Fig. S1. All baseline characteristics of patients followed up and lost to follow-up were comparable (Additional file 1: Table S1). During a median follow-up of 5.1 years (interquartile range: 5.0–5.1 years), 366 all-cause deaths, 219 cardiac deaths, 551 non-fatal MIs, 345 non-fatal strokes, 1371 unplanned revascularizations, and 2143 major adverse cardiovascular and cerebrovascular events were documented. No correlation was observed between preprocedural PNI and fasting blood glucose or glycated hemoglobin (r < 0.200) (Additional file 1: Table S2).
As shown in Table 1, the median age of the study population was 59 years (interquartile range: 51–66 years), 2163 (22.93%) were women, and 3956 (41.96%) had diabetes. The median value of preprocedural PNI was 52.60 for all participants. When patients were stratified by vital status, absolute lymphocyte counts, serum albumin levels, and PNI were significantly lower in patients who had died than in those still alive. Unsurprisingly, patients who survived to the end of5 year follow-up were younger, had fewer comorbidities (diabetes, hypertension, peripheral artery disease, and chronic obstructive pulmonary disease), were less likely to have a previous history of revascularization, MI and stroke, and had higher estimated glomerular filtration rate and left ventricular ejection fraction. The clinical presentation of CAD, cardiovascular medication use, and angiographic characteristics were well-balanced between the two groups.
The optimal cut-off value of preprocedural PNI for predicting all-cause death was 48.49. Table 2 shows baseline characteristics among four groups stratified by preprocedural PNI category and diabetes status. Patients with L-PNI accounted for 22.08% of all participants, 20.88% of the diabetes population, and 22.95% of the nondiabetic population. The DM/L-PNI group had more women and elderly patients than other groups. Patients in the DM/L-PNI group tended to have more comorbidities and previous adverse events and were more likely to have declined renal and cardiac function. The severity of coronary lesions sequentially increased from the non-DM/H-PNI group to the DM/L-PNI group, reflected by more left main or three-vessel disease and higher Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score.
Effect of preprocedural PNI category and diabetes status on clinical outcomes
Kaplan–Meier curves illustrate that patients in the DM/L-PNI group experienced more all-cause deaths than in other groups (log-rank p < 0.001; Fig. 1).
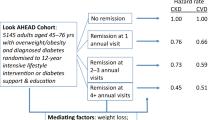
Univariate analysis for all-cause death is shown in Additional file 1: Table S3. Analyses before and after adjustment generated consistent results that the DM/L-PNI group yielded the highest risk of all-cause death (adjusted HR: 2.65, 95% CI 1.97–3.56, p < 0.001) compared with the non-DM/H-PNI group, followed by the non-DM/L-PNI group (adjusted HR: 1.44, 95% CI 1.05–1.98, p = 0.026), while DM/H-PNI was not associated with the risk of all-cause death (Table 3). The negative effect of L-PNI on all-cause death was significantly stronger in diabetic patients than in nondiabetic patients (p for interaction = 0.037; Fig. 2). The inverse probability of treatment weighting analysis produced similar results (Additional file 1: Table S4). Baseline characteristics after weighting were shown in Additional file 1: Table S5.
Association of PNI level and diabetes status with all-cause death. Forrest plots for all participants (A) and subgroups (B). Preprocedural PNI was categorized by the optimal cut-off value for all-cause death of 48.49. Subgroups were defined by age category, sex, BMI category, and admission presentation. ACS acute coronary syndrome, BMI body mass index, CCS chronic coronary syndrome, CI confidence interval, HR hazard ratio, other abbreviations as in Fig. 1.
No significant interaction between subgroups and preprocedural PNI category and diabetes status (all p for interaction > 0.05) was detected. DM/L-PNI remained associated with the highest risk of all-cause death, except in the subgroup aged < 65 years which limited statistical power with only 15 all-cause deaths and 438 individuals (Fig. 2, Additional file 1: Table S6).
Kaplan–Meier curves for secondary endpoints are shown in Additional file 1: SFigs. S2, S3, S4, S5, and S6. The same pattern of the association of preprocedural PNI category and diabetes status with all-cause death was observed for cardiac death. The non-DM/H-PNI group yielded a significantly lower risk of non-fatal stroke than the other three groups. DM/H-PNI was associated with an increased risk of unplanned revascularization. DM/H-PNI and DM/L-PNI were associated with an increased risk of major adverse cardiovascular and cerebrovascular events. No association of the four groups with non-fatal MI was observed.
Sensitivity analysis
Postprocedural PNI decreased in approximately 85% of patients. Analyses applying preprocedural dichotomous PNI and postprocedural PNI category generated robust results with the main analysis, whereas ΔPNI had no association with all-cause death. Only 471 patients were diagnosed with malnutrition based on the GLIM criteria, and the association with all-cause death remained similar to the main analysis (Additional file 1: Table S7).
On a continuous scale, elevated preprocedural PNI was associated with a decreased risk of all-cause death. For a 1-standard deviation increase in PNI, adjusted HRs and 95% Cis were 0.94 (0.92–0.96) in all participants, 0.92 (0.89–0.95) in diabetic patients, and 0.96 (0.93–0.99) in nondiabetic patients. When PNI was below 48.49, the risk of all-cause death decreased sharply with elevating PNI in both diabetic and nondiabetic patients, while a PNI above 48.49 yielded a trend toward a slight but steady reduction in the risk of all-cause death, which was only significant in diabetic patients (Fig. 3).
Association of preprocedural continuous PNI with all-cause death. Restricted cubic spline curves for all participants (A), diabetic (B), and nondiabetic (C) patients. A preprocedural PNI level of 48.49 was set as a reference. Adjusted for sex, age, hypertension, chronic obstructive pulmonary disease, previous revascularization, previous myocardial infarction, previous stroke, high-sensitivity C-reactive protein, estimated glomerular filtration rate, and left ventricular ejection fraction. SD, standard deviation; other abbreviations as in Figs. 1, 2.
Added value of nutritional indexes beyond the GRACE risk score
For the prediction of all-cause death in the entire ACS patients, the addition of preprocedural PNI category significantly improved discrimination (AUC and 95% CI 0.733 [0.698–0.768] vs. 0.688 [0.651–0.725], ΔAUC: 0.045, p < 0.001) and reclassification (NRI: 0.323, 95% CI 0.186–0.466, p < 0.001; IDI: 0.080, 95% CI 0.023–0.137, p = 0.006) of the GRACE risk score (Table 4). The decision curve illustrates that the GRACE + PNI category model outperformed the GRACE risk score, with a higher clinical net benefit within a threshold probability range from 0.05 to 0.25 (Fig. 4A). In diabetic ACS patients, the added value of preprocedural PNI category was more significant, with a higher clinical net benefit within a threshold probability range from 0.05 to 0.30 (Table 4; Fig. 4B). In nondiabetic ACS patients, the addition of preprocedural PNI category also achieved model improvement, whereas the decision curve reveals no clear increase in clinical net benefit (Fig. 4C).
Decision curve analysis for models predicting all-cause death. Decision curves for all participants (A), diabetic (B), and nondiabetic (C) patients. Preprocedural PNI was categorized by the optimal cut-off value for all-cause death of 48.49. GRACE, Global Register Acute Coronary Events; other abbreviations as in Fig. 1.
The addition of preprocedural dichotomous PNI, preprocedural continuous PNI, postprocedural PNI category, and malnutrition defined by the GLIM criteria to the GRACE risk score improved the AUC to varying extents. However, NRI and IDI indicate that these indexes were inferior to preprocedural PNI category. ΔPNI provided no improvement in the GRACE risk score (Table 4).
Discussion
This study presents the first evaluation of the joint effect and interaction between PNI level and diabetes status on 5 year outcomes after PCI in CAD patients. We found that patients with diabetes and L-PNI experienced the highest risk of all-cause death; the negative effect of L-PNI on all-cause death was significantly stronger in diabetic patients than in nondiabetic patients; the addition of preprocedural PNI category significantly improved model performance and clinical net benefit of the GRACE risk score for predicting all-cause death, especially in diabetic patients. These findings emphasize the prognostic significance of nutritional-immunological status and its interaction with diabetes status for CAD patients.
Previous small-scale studies have reported reduced coronary blood flow [15] and survival rate related to L-PNI in the ACS or stable CAD population [13,14,15,16]. This study demonstrated the adverse prognostic significance of low PNI for the overall CAD population. Hypoalbuminemia raises cardiovascular risk mainly related to weakened antioxidant, oncotic pressure-maintaining, and antithrombotic capacities of albumin [24]. In addition, decreased serum albumin indicates underlying inflammation, which provokes the progress of atherosclerosis [25]. Reduced absolute lymphocyte counts indicate impaired immune defenses due to malnutrition [26], reflecting increased susceptibility to infection and inflammation, which translate into atherosclerotic burden [2]. Additionally, different lymphocyte subsets are known to have opposite roles: T helper-1 and B2 cells can induce atherosclerosis, while regulatory T cells and B1 cells have atheroprotective properties [27]. Malnutrition may alter the proportions of lymphocyte subsets, causing an imbalance between proatherogenic and antiatherogenic immune microenvironments [26].
After considering diabetes status, we found that CAD patients accompanied by diabetes and L-PNI experienced the highest risk of all-cause death, the L-PNI-related risk outweighed the diabetes-related risk, while diabetes aggravated the negative impact of L-PNI (Additional file 1: Fig. S7). First, diabetic patients are often in a negative nitrogen balance due to increased protein catabolism and excretion and decreased protein anabolism. This raises the risk of malnutrition, [17] which in turn exacerbates insulin resistance, leading to a vicious cycle that impairs patients’ general conditions. Both diabetes and malnutrition can exacerbate the imbalance between cardioprotective immune response and inflammation, synergistically promoting the progression of CAD, resulting in worse prognosis in patients with combined traits [26, 28, 29]. Second, L-PNI/nondiabetic patients had a higher HR for all-cause death than H-PNI/diabetic patients, which is in line with previous research suggesting that the mortality risk related to malnutrition is higher than that associated with other chronic comorbidities [17], highlighting the value of PNI as a potent and general prognostic indicator. The differential impact of PNI and diabetes on all-cause death may be attributed to the fact that diabetes is typically subjected to active management, whereas subclinical malnutrition often goes undetected and therefore lacks intervention. Last, the adverse prognostic effect of L-PNI was aggravated in the presence of diabetes, which should be explained by the distinct pathophysiological state of diabetic patients. One possible example is that serum albumin might play a role in preventing autophagy; [30] however, the level of autophagy in diabetic heart tissue is significantly increased, [31] thereby amplifying the deleterious impact of hypoalbuminemia.
This study provides a comprehensive analysis of PNI. Except for ΔPNI, preprocedural PNI category, preprocedural dichotomous PNI, preprocedural continuous PNI, and postprocedural PNI category were all significantly associated with all-cause death in CAD patients and improved the AUC of the GRACE risk score. The finding is supported by previous studies [13, 16]. In this study, the GRACE + PNI category model showed the best performance, and only this model achieved significant improvement in both diabetes and nondiabetic patients. Restricted cubic spline for the association of preprocedural continuous PNI with the risk of all-cause death presents an inflection, illustrating that categorizing PNI by a certain cut-off value to identify malnourished patients is clinically realistic. The observed decrease in PNI after PCI may be attributable to the acute stress of catheterization. Therefore, preprocedural PNI is a more appropriate index of nutrition status than postprocedural PNI.
The GLIM has built a global consensus for malnutrition diagnosis with consideration of inflammation. However, the addition of malnutrition defined by the GLIM criteria had limited improvement in the GRACE risk score. This finding can be attributed to two reasons: first, we applied only one etiological criterion and two phenotypic criteria and thus failed to identify all malnourished patients; second, the GLIM still primarily considers body weight, thereby underestimating malnutrition in this study population. Moreover, GLIM criteria involve a multi-step diagnostic approach. In contrast, due to the wide availability of serum albumin and absolute lymphocyte counts, preprocedural PNI is a convenient and potent prognostic factor for CAD patients.
To our knowledge, this large-scale cohort study presents the first evaluation of the prognostic significance of PNI in the overall CAD population, the first investigation of the joint effect and interaction between PNI level and diabetes status on the prognosis of CAD patients, and the most comprehensive analysis for PNI.
This study also has some limitations. First, the observational nature raises concerns about residual confounding. Second, this single-center study was conducted only in Chinese population, which restricts the generalizability of our work. Large-scale studies in different countries and races are needed to determine a universal or race-specific cut-off value of PNI. Third, we did not follow up on nutritional status, which might have changed during the five-year follow-up period. Randomized trials are necessary to evaluate the value of PNI as an indicator of the efficacy of oral nutritional support in improving prognosis of CAD in a context of reduction of inflammatory drivers of both diabetes and CAD.
Conclusions
CAD patients with diabetes and L-PNI experienced the worst prognosis. The presence of diabetes amplifies the negative effect of status-PNI on all-cause death. Poor nutritional-immunological status outweighs diabetes in increasing the risk of all-cause death in CAD patients. Preprocedural PNI can serve as an assessment tool of nutritional and inflammatory risk and an independent prognostic factor in CAD patients, especially in those with diabetes.
Availability of data and materials
The data that support the findings of this study are available from the Information Center of Fuwai Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Information Center of Fuwai Hospital.
Abbreviations
- ACS:
-
Acute coronary syndrome
- AUC:
-
Area under the curve
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- GLIM:
-
Global leadership initiative on malnutrition
- GRACE:
-
Global register acute coronary events
- H:
-
High
- HR:
-
Hazard ratio
- IDI:
-
Integrated discrimination improvement
- L:
-
Low
- MI:
-
Myocardial infarction
- NRI:
-
Net reclassification improvement
- PCI:
-
Percutaneous coronary intervention
- PNI:
-
Prognostic nutritional index
References
Liu J, Huang Z, Huang H, He Y, Yu Y, Chen G, et al. Malnutrition in patients with coronary artery disease: prevalence and mortality in a 46,485 Chinese cohort study. Nutr Metab Cardiovasc Dis. 2022;32(5):1186–94.
Stenvinkel P, Heimburger O, Lindholm B, Kaysen GA, Bergstrom J. Are there two types of malnutrition in chronic renal failure? Evidence for relationships between malnutrition, inflammation and atherosclerosis (MIA syndrome). Nephrol Dial Transplant. 2000;15(7):953–60.
Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. 1980;139(1):160–7.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85(9):1001–5.
Yan L, Nakamura T, Casadei-Gardini A, Bruixola G, Huang YL, Hu ZD. Long-term and short-term prognostic value of the prognostic nutritional index in cancer: a narrative review. Ann Transl Med. 2021;9(21):1630.
Correa-Rodriguez M, Pocovi-Gerardino G, Callejas-Rubio JL, Fernandez RR, Martin-Amada M, Cruz-Caparros MG, et al. The prognostic nutritional index and nutritional risk index are associated with disease activity in patients with systemic Lupus Erythematosus. Nutrients. 2019;11(3):638.
Candeloro M, Di Nisio M, Balducci M, Genova S, Valeriani E, Pierdomenico SD, et al. Prognostic nutritional index in elderly patients hospitalized for acute heart failure. ESC Heart Fail. 2020;7(5):2479–84.
Cheng YL, Sung SH, Cheng HM, Hsu PF, Guo CY, Yu WC, et al. Prognostic nutritional index and the risk of mortality in patients with acute heart failure. J Am Heart Assoc. 2017;6(6):004876.
Narumi T, Arimoto T, Funayama A, Kadowaki S, Otaki Y, Nishiyama S, et al. Prognostic importance of objective nutritional indexes in patients with chronic heart failure. J Cardiol. 2013;62(5):307–13.
Chien SC, Chandramouli C, Lo CI, Lin CF, Sung KT, Huang WH, et al. Associations of obesity and malnutrition with cardiac remodeling and cardiovascular outcomes in Asian adults: a cohort study. PLoS Med. 2021;18(6): e1003661.
Prausmuller S, Heitzinger G, Pavo N, Spinka G, Goliasch G, Arfsten H, et al. Malnutrition outweighs the effect of the obesity paradox. J Cachexia Sarcopenia Muscle. 2022;13(3):1477–86.
Sze S, Pellicori P, Kazmi S, Rigby A, Cleland JGF, Wong K, et al. Prevalence and prognostic significance of malnutrition using 3 scoring systems among outpatients with heart failure: a comparison with body mass index. JACC Heart Fail. 2018;6(6):476–86.
Raposeiras Roubin S, Abu Assi E, Cespon Fernandez M, Barreiro Pardal C, Lizancos Castro A, Parada JA, et al. Prevalence and prognostic significance of malnutrition in patients with acute coronary syndrome. J Am Coll Cardiol. 2020;76(7):828–40.
Keskin M, Ipek G, Aldag M, Altay S, Hayiroglu MI, Borklu EB, et al. Effect of nutritional status on mortality in patients undergoing coronary artery bypass grafting. Nutrition. 2018;48:82–6.
Keskin M, Hayiroglu MI, Keskin T, Kaya A, Tatlisu MA, Altay S, et al. A novel and useful predictive indicator of prognosis in ST-segment elevation myocardial infarction, the prognostic nutritional index. Nutr Metab Cardiovasc Dis. 2017;27(5):438–46.
Wada H, Dohi T, Miyauchi K, Jun S, Endo H, Doi S, et al. Relationship between the prognostic nutritional index and long-term clinical outcomes in patients with stable coronary artery disease. J Cardiol. 2018;72(2):155–61.
Ahmed N, Choe Y, Mustad VA, Chakraborty S, Goates S, Luo M, et al. Impact of malnutrition on survival and healthcare utilization in Medicare beneficiaries with diabetes: a retrospective cohort analysis. BMJ Open Diabetes Res Care. 2018;6(1): e000471.
Wei W, Zhang L, Li G, Huang Z, Liu J, Wu Z, et al. Prevalence and prognostic significance of malnutrition in diabetic patients with coronary artery disease: a cohort study. Nutr Metab (Lond). 2021;18(1):102.
Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(10):2937–44.
World Health Organization. Regional Office for the Western Pacific. The Asia-Pacific perspective: redefining obesity and its treatment Sydney: Health Communications Australia 2000. https://apps.who.int/iris/handle/10665/206936.
Joint committee issued Chinese guideline for the management of dyslipidemia in a: 2016 Chinese guideline for the management of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi 2016. 44(10):833–53
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle. 2019;10(1):207–17.
Eckart A, Struja T, Kutz A, Baumgartner A, Baumgartner T, Zurfluh S, et al. Relationship of nutritional status inflammation, and serum albumin levels during acute illness a prospective study. Am J Med. 2020;133(6):713–22.
Manolis AA, Manolis TA, Melita H, Mikhailidis DP, Manolis AS. Low serum albumin: a neglected predictor in patients with cardiovascular disease. Eur J Intern Med. 2022;102:24–39.
Libby P. Inflammation in atherosclerosis-no longer a theory. Clin Chem. 2021;67(1):131–42.
Fock RA, Blatt SL, Beutler B, Pereira J, Tsujita M, de Barros FE, et al. Study of lymphocyte subpopulations in bone marrow in a model of protein-energy malnutrition. Nutrition. 2010;26(10):1021–8.
Hedrick CC. Lymphocytes in atherosclerosis. Arterioscler Thromb Vasc Biol. 2015;35(2):253–7.
Zeng C, Shi X, Zhang B, Liu H, Zhang L, Ding W, et al. The imbalance of Th17/Th1/Tregs in patients with type 2 diabetes: relationship with metabolic factors and complications. J Mol Med (Berl). 2012;90(2):175–86.
Rajamanickam A, Munisankar S, Dolla CK, Thiruvengadam K, Babu S. Impact of malnutrition on systemic immune and metabolic profiles in type 2 diabetes. BMC Endocr Disord. 2020;20(1):168.
Wu Y, Fan W, Huang D, Sun X. Possible intermediary role of autophagy in serum albumin decrease-associated cardiovascular events among patients with coronary heart disease. Int J Cardiol. 2018;250:64.
Munasinghe PE, Riu F, Dixit P, Edamatsu M, Saxena P, Hamer NS, et al. Type-2 diabetes increases autophagy in the human heart through promotion of Beclin-1 mediated pathway. Int J Cardiol. 2016;202:13–20.
Sciacqua A, Andreozzi F, Succurro E, Pastori D, Cammisotto V, Armentaro G, et al. Impaired clinical efficacy of aspirin in hypoalbuminemic patients with diabetes mellitus. Front Pharmacol. 2021;12: 695961.
Acknowledgements
We thank all the study participants and their families for their cooperation; the staff of Fuwai Hospital for data collection, management, and monitoring; Dr. Jining He of Fuwai Hospital for inspiring the idea to investigate the joint effect of PNI level and diabetes status; and Prof. Xinxu Wang of Gansu Medical College for helpful discussions. T.L thanks her sister, Yutong Wang for editing the figures.
Funding
This work was supported by the CAMS Innovation Fund for Medical Sciences [2020-I2M-C&T-B-049]; National Clinical Research Center for Cardiovascular Disease, Fuwai Hospital, Chinese Academy of Medical Sciences [NCRC2020013]; and China International Exchange and Promotion Association for Medical and Healthcare Investigator Sponsored Study [CN174125, DIREGL08735-DAPT].
Author information
Authors and Affiliations
Contributions
TL: Conceptualization, Methodology, Formal analysis, Writing—Original Draft DY: Formal analysis, Writing—Review and Editing PW: Formal analysis, Visualization GZ: Formal analysis, Visualization SJ: Data Curation CZ: Data Curation PZ: Data Curation YS: Data Curation XT: Data Curation RG: Supervision, Writing—Review and Editing BX: Investigation, Resources JY: Conceptualization, Investigation, Supervision, Project administration, Funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study complied with the Declaration of Helsinki. The Review Board of Fuwai Hospital approved the study protocol before enrolment (No. 2013–449). All participants provided written informed consents before intervention.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1: Table S1.
Baseline characteristics stratified by follow-up status. Table S2. Correlation between preprocedural PNI and glycemic measures in all participants and stratified by DM status. Table S3. Univariate and multivariate Cox proportional-hazard regression analysis for all-cause death. Table S4. Subgroup analysis for all-cause death. Figure S1. The study flowchart. Figure S2. Kaplan-Meier curves for cardiac death by diabetes status (A), PNI level (B) and both (C). Figure S3. Kaplan-Meier curves for non-fatal MI by diabetes status (A), PNI level (B) and both (C). Figure S4. Kaplan-Meier curves for non-fatal stroke by diabetes status (A), PNI level (B) and both (C). Figure S5. Kaplan-Meier curves for unplanned revascularization by diabetes status (A), PNI level (B) and both (C). Figure S6. Kaplan-Meier curves for MACCE by diabetes status (A), PNI level (B) and both (C). Figure S7. Central illustration.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, T., Yuan, D., Wang, P. et al. Association of prognostic nutritional index level and diabetes status with the prognosis of coronary artery disease: a cohort study. Diabetol Metab Syndr 15, 58 (2023). https://doi.org/10.1186/s13098-023-01019-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01019-8