Abstract
Aim
The hypothesis of the effect of the insulinogenic effects of diet on the development of cardiovascular diseases has been proposed, but the findings of previous studies are very contradictory. We investigated the association between dietary insulin index (DII) and dietary insulin load (DIL), and metabolic syndrome (MetS) risk. Another objective was to examine the extent to which lifestyle (physical activity, smoking status, and weight change) and sex influence the relationship between DII, DIL, and MetS risk.
Materials and methods
We followed 1915 participants in the Tehran Lipid and Glucose Study. DIL and DII were calculated based on a validated food frequency questionnaire. Weight change was measured, and participants were categorized into > 3% weight loss, weight stable (± 3%), and > 3% weight gain. By joint classification, the association between DII and DIL (< median and ≥ median) and risk of MetS was assessed according to weight change, sex, physical activity levels, and smoking status. Cox proportional hazards models were used to estimate the HRs (95% CI), adjusting for potential confounders.
Results
During 8.9 years of follow-up, among 1915 participants, we documented 591 new cases of MetS. DII and DIL were not associated with MetS risk in the crude and adjusted models. However, DIL and DII were associated with weight gain (≥ 3%). In the crude model, DIL and DII were associated with a higher risk of weight gain [HR: 1.74: 95% CI 1.50–2.03, and 1.70 (1.46–1.98), respectively]. These associations remained significant after further adjustment for confounders. The HRs were 1.61 (1.35–1.92) for DIL and 1.64 (1.39–1.93) for DII. Among men, women, participants with low physical activity levels, and smokers, the risk of MetS, independent of DIL and DII, only increased in a participant with weight gain. In women with weight stability, DIL and DII, higher than the median, were positively associated with MetS risk.
Conclusion
Our findings suggest that the association between MetS risk and a hyperinsulinemic diet depended on weight change.
Similar content being viewed by others
Introduction
Metabolic syndrome (MetS) is a multifactorial metabolic disease characterized by hypertension, dysglycemia, dyslipidemia, and central obesity. During the last two decades, the epidemic of MetS has been increasing at an alarming rate [1,2,3]. Its prevalence is increasing by more than 40% in some regions, in both developed and developing countries [1, 2]. Hyperinsulinemia and subsequent insulin resistance were well known to link the diet and MetS [4, 5]. Growing evidence suggests long-term exposure to insulin concentrations increases the risk of chronic disease [6, 7]. Although carbohydrate evokes postprandial insulin secretion and leads to hyperinsulinemia, the quantity, and quality of other macronutrients, including fat and protein, induce insulin secretion and hyperinsulinemia [8,9,10]. Two new dietary indices, the dietary insulin index (DII) and dietary insulin load (DIL), have been developed to assess the effect of insulinotropic factors of diet on insulin secretion and insulin exposure [11, 12]. The hypothesis of the effect of the insulinogenic effects of diet on the development of cardiovascular diseases (CVD) has been proposed, but the findings of previous studies are very contradictory. In cross-sectional studies, an insulinogenic diet has shown conflicting results with MetS and its components, including dyslipidemia, dysglycemia, and C-reactive protein concentrations [13,14,15,16]. Moreover, whether long-term consumption of diet-induced insulin secretion is associated with chronic diseases such as CVD and type 2 diabetes mellitus remain controversial in the general population [17, 18]. This discrepancy may be due to the modification effect of other lifestyle factors, such as physical activity and smoking status, particularly changes in body weight, on the association between DIL and DII and chronic diseases [13, 19, 20]. According to previous studies, following the consumption of insulinogenic food during the long term can increase the risk of weight gain [19, 21]. Changes in body weight have been shown to be associated with the incidence of chronic disease [22]. In addition, the development of chronic diseases such as MetS was influenced by two lifestyle factors, including physical activity and smoking status [23] and the interaction between DII and DIL with physical activity and smoking status on MetS was not evaluated yet. Few studies investigated the modification effect of weight change, physical activity, and smoking status on the relation between the potential insulinemic effect of diet on weight gain [13, 16, 19]. Therefore, the present study had multiple objectives. In this population-based prospective study, the first was to investigate the association between DII and DIL, weight change, and MetS risk. Another aim was to examine the extent to which lifestyle (physical activity, smoking status, and weight change) and sex influence the relationship between DII, DIL, and MetS risk.
Materials and methods
Study population
This study has been conducted within the framework of the Tehran Lipid and Glucose Study (TLGS), which is an ongoing prospective population-based study to prevent non-communicable diseases. The layout and other information on TLGS were provided elsewhere [24].
The TLGS was initiated in March 1999. A multistage, stratified cluster random sampling technique was used to enroll > 15,000 participants ≥ 3 years from district 13 of Tehran. The population of this district is representative of the urban population of Tehran, the capital city of Iran. Since 1999, the participants of TLGS underwent assessments for anthropometric measures, medication use, medical history of CVD risk factors, lifestyle factors, sociodemographic factors, socioeconomic status, and biochemical and blood pressure measurements. This information was documented through face-to-face interviews with the local research team every 3 years. Up to now, 6 phases of the examinations have been performed. Phases II, III, IV, V, and VI were prospective follow-up studies conducted during 2002–2004, 2005–2008, 2008–2011, 2012–2015, and 2016–2018, respectively.
The current study used the baseline examination data from phase III of the TLGS (2006–2008) because of the small sample size for dietary assessment in phases I and II of the study and using 24-h recall. The subjects were followed up to phase VI of TLGS (2016–2018).
During phase III of the TLGS (2006–2008), medical history and physical examination were collected for 12,523 participants. Owing to the cost, complexity, and time involved in the collection of dietary data in a large population, a representative sample of 4920 participants was randomly selected based on their age and gender. Of 4920 participants, 3462 agreed to complete a food frequency questionnaire (FFQ). The characteristics of participants who completed the FFQ were similar to those of the total population in phase III of TLGS [25]. For the current study, of 3462 participants, 3265 adults aged 19 years or older with complete data (demographic, anthropometric, biochemical, and dietary data) were selected from phase III (2006–2008). Moreover, individuals with MetS at baseline (n = 879), women who were pregnant or lactating at baseline and during follow-up (n = 28), and subjects with under- or over-reporting of energy intakes (daily energy intake < 500 and > 4200 kcal per day) (n = 115), participants following any specific diet as a result of their hyperlipidemia, hypertension, and hyperglycemia (n = 26), and subjects with missing biochemical and anthropometric measures related to diagnosis of MetS during follow up (n = 309) were excluded from the study. Final analysis was conducted on 1915 participants until 2018, with a response rate of 66%, during the 8.9 (Interquartile range: 7.98–9.69) year follow-up. The study protocol was approved by the Ethics Committee of the Research Institute for Endocrine Sciences (RIES) of Shahid Beheshti University of Medical Sciences, Tehran, Iran. Written informed consent was obtained from all participants.
Anthropometric measurements
Briefly, the participants’ weight, while being minimally clothed without shoes, was recorded using a digital scale (Seca 707; range: 0–150 kg; Seca GmbH, Germany) and recorded with accuracy of 100 g. Height was also measured in a standing position, without shoes, with shoulders in neutral alignment using a stadiometer (Seca 225; Seca GmbH, Germany) and recorded to the nearest 0.5 cm. Body mass index (BMI) was calculated as weight (kg) divided by the square of height (m2). Waist circumference (WC) was measured at the umbilical level using an un-stretched tape measure without any pressure to the body surface (accuracy, 0.5 cm).
Assessment of other variables
After participants rested in a sitting position for 15 min, blood pressure was measured using a standardized mercury sphygmomanometer (calibrated by the Iranian Institute of Standards and Industrial Research) on the right arm twice, at least 30 s apart, and the average of the two measurements was reported as the participant’s blood pressure. Demographic, lifestyle (smoking status and physical activity), socioeconomic status (education and employment), medication regimen (e.g., antihypertensive, lipid-lowering, and anti-diabetes drugs), and medical history were gathered using a questionnaire.
Physical activity was assessed using a modifiable activity questionnaire (MAQ) that included a list of all three forms of activities, including leisure time, job, and household activities. The frequency and amount of time spent per week on physical activity over the last year were recorded [26]. The physical activity levels were expressed as metabolic-equivalent (MET) hours per week (MET-h/week) [27]. The reliability and validity of the Persian version of the MAQ have been reported [28].
Dietary assessment
During face-to-face interviews with expert dietitians, a validated semi-quantitative FFQ was used to determine the frequency of daily, weekly, or monthly consumption of each food item during the previous year [29]. The Iranian food composition table (FCT) was used to calculate macro- and micronutrient intake [30].
From the initial number of 1915 participants at baseline, 592 participants completed all 4 FFQs (at baseline and during follow-up in phases IV, V, and VI), 804 participants completed 3 FFQs (at baseline and in two of the three phases of the follow-up study), 316 participants completed 2 FFQs (at baseline and in one of the three phases of the follow-up study), and 203 participants did not complete any FFQs during follow-up (only at baseline). To impute missing values, last observation carried forward method was used. In the present study, due to the crucial effect of recent dietary intakes on the association between diet and chronic disease, we used an alternative approach according to the Hu et al. formula [31]. This approach, which is more important than the baseline measures, adds more weight to the recent diet, reduces within-subject variability, and evaluates the long-term diet.
Definition of DIL and DII
Food insulin index (FII) refers to the incremental insulin area under the curve over 2 h in response to the consumption of a 1000-kJ (239 kcal) portion of the test food divided by the area under the curve after the ingestion of a 1000-kJ (239 kcal) portion of the reference food. The insulin index for 68 food items was obtained from studies by Bao et al. [12] (50 items), Bell et al. [32] (13 items), and Holt et al. [11] (5 items). The insulin index for three food items, including tea, coffee, and salt, was considered 0 because these foods’ energy, carbohydrate, protein, and fat content were close to 0. For the remaining 49 food items that were not available in the food lists of the mentioned studies, the FII of similar food items was used based on the correlation between their energy, fiber, carbohydrate, protein, and fat content. For example, both dates and raisins are dried fruits. The energy, carbohydrate, fat, protein, and fiber content of both fruits are similar. Therefore, we used the insulin index of raisins for dates. The 120 items of the FFQ, the source of the FII, and the FII value are presented in DII and DIL in Relation to MetS: The Shahedieh Cohort Study (available at www.jandonline.org). To determine DIL, first, the insulin load of each food was calculated using the following formula: Insulin load of a given food = insulin index of that food × energy content per 1 g of that food amount consumed (g/d). By summing the insulin load of each food, DIL was obtained for each person. DII was then calculated for each participant by dividing DIL by total energy intake.
Biochemical assessments
For biochemical measurements, after 12–14 h of overnight fasting, venous blood samples were collected in vacutainer tubes and centrifuged within 30–45 min of collection. The fasting plasma glucose (FPG), high-density lipoprotein-cholesterol (HDL-C), and triglyceride (TG) levels were measured in the TLGS research laboratory on the day of sample collection, using a Selectra 2 autoanalyzer (Vital Scientific, Spankeren, the Netherlands) and commercial kits (Pars Azmoon Inc., Tehran, Iran). FPG level was measured using an enzymatic colorimetric method with the glucose oxidase technique. The inter- and intra-assay coefficients of variation (CV) at baseline and after follow-up were both below 2.3%. TG was also assayed using an enzymatic colorimetric method with glycerol phosphate oxidase. HDL-C was measured after the precipitation of apolipoprotein B-containing lipoproteins with phosphotungstic acid. In baseline and follow-up assays, both intra- and inter-assay CVs were below 2.1% and 3.0% for TG and HDL-C. All samples were analyzed when the internal quality control met the acceptable criteria.
Definition of MetS
According to the Joint Interim Statement, a MetS diagnosis requires the presence of three or more criteria [33], including (1) elevated glucose concentrations (FPG concentration ≥ 100 mg/dL) or treatment with anti-hyperglycemic medications; (2) elevated serum TG concentration (≥ 150 mg/dL) or treatment with anti-hypertriglyceridemia medications; (3) reduced serum HDL-C (< 50 mg/dL in women and < 40 mg/dL in men); (4) elevated blood pressure (≥ 130/85 mmHg) or treatment with anti-hypertensive medications; and (5) enlarged abdominal circumference (≥ 95 cm according to the population- and country-specific cut-off points for Iranian adults of both genders [34].
Definition of weight change
Percentage weight change was calculated by subtracting the baseline weight from the follow-up one and multiplying it by 100. Participants were categorized as those who lost weight (≥ 3%), those with weight stability (± 3%), and those who gained weight (≥ 3%) [35].
Statistical analysis
Data are reported as mean (SD) and median (25th and 75th percentiles) for continuous variables or percentages for categorical variables. DII and DIL were categorized into tertiles. Baseline characteristics and energy-adjusted dietary variables were described across the tertiles of DII and DIL, using the general linear model and Chi-square test for continuous and categorical variables, respectively. Moreover, Cox proportional-hazards regression models were used to estimate the hazard ratios (HRs) and their 95% confidence intervals (CIs) for the incidence of MetS and weight gain ≥ 3% across the tertiles of DII and DIL. The first model was crude, while the second model was adjusted for age, gender, smoking, physical activity, education levels, occupation status, total energy intake, and family history of diabetes, dietary fiber and dietary cholesterol (all variable that adjusted was at baseline). The third model was additionally adjusted for BMI at baseline. The linearity of trends was determined by integrating the median values of tertiles as continuous variables into the Cox regression models. Based on the multivariable Cox regression model, by joint classification, we estimated the HRs and 95% CIs for MetS, according to the weight changes, sex, physical activity levels and smoking status. All statistical analyses were performed in SPSS version 15.0 (SPSS Inc., Chicago, IL, USA), and P-values less than 0.05 were considered statistically significant.
Result
During 8.9 years of follow-up, among 1915 participants, we documented 591 new cases of MetS. The mean (SD) age and BMI at baseline were 36.5 years (13.3) and 25.6 (4.5), respectively. 60% of the participants were men. The baseline characteristics of participants across tertiles of DII and DIL are presented in Table 1. Participants in the highest tertiles of DIL and DII were significantly younger, more likely to be smokers, less educated, and had weight gain. The intake of dietary variables of participants across tertiles of DII and DIL are presented in Table 2. Participants in the highest tertile of DII and DIL had a higher intake of energy, carbohydrate, total fiber, sugar-sweetened beverages, fruit, meats, processed meat, organ meat, whole grain, refined grain, nuts, and dairy products.
Table 3 presents multivariable-adjusted hazard ratio (95% confidence interval) for MetS and weight gain across tertiles of DII and DIL. DII and DIL were not associated with MetS risk in the crude and adjusted models. However, DIL and DII were associated with weight gain (≥ 3%). In the crude model, DIL and DII were associated with a higher risk of MetS (HR: 1.74: 95% CI 1.50–2.03, and 1.70 (1.46–1.98), respectively). These associations remained significant after further adjustment for confounders. The HRs were 1.61 (1.35–1.92) for DIL and 1.64 (1.39–1.93) for DII.
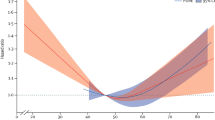
The combined effects of weight change and DIL and DII on MetS risk in the total population, as well as by gender, physical activity level, and smoking status, are shown in Figs. 1 and 2. In the total population, the risk of MetS, independent of DIL, increased in a participant with weight gain. However, participants with weight gain and DII ≥ median exhibited a significantly higher risk of MetS than the reference group. This association was not observed among subjects with DII lower than the median. In participants with weight stability and weight loss, DIL and DII, lower or higher than the median, were not associated with MetS risk compared to the reference group.
Hazard ratios of the combined. effect of dietary insulin load consumption (< median vs. ≥ median) and weight change (triangle, > 3% weight loss; square, weight stable (± 3%); and circle, > 3% weight gain) on risk MetS after adjustment for age, gender, smoking, physical activity, education levels, occupation status, total energy intake, and family history of diabetes, dietary fiber and dietary cholesterol and BMI at baseline
Hazard ratios of the combined. effect of dietary insulin index consumption (< median vs. ≥ median) and weight change (triangle, > 3% weight loss; square, weight stable (± 3%); and circle, > 3% weight gain) on risk MetS after adjustment for age, gender, smoking, physical activity, education levels, occupation status, total energy intake, and family history of diabetes, dietary fiber and dietary cholesterol and BMI at baseline
Further analyses on sex stratification revealed an association between weight gain and risk of MetS in men, independent of DIL and DII. The risk of MetS was not associated with DIL among men with weight stable and weight loss categories. Among women, the risk of MetS, independent of DIL and DII, increased with weight gain. In women with weight stability, DIL and DII, higher than the median, were positively associated with MetS risk. This association was not observed among subjects with DIL, and DII lower than the median.
Stratification based on physical activity level resulted in the increase of MetS risk among weight gained group with low physical activity, independent of DII and DIL. No association was found between DIL, DII, and risk of MetS in both weight-stable and weight-loss participants. Among participants in the medium and high category of PAL, DII and DIL were not associated with MetS, regardless of weight change, after adjustments for confounding factors.
Among smoking participants with weight gain, DIL > or < of the median increased risk of MetS compared to participants with weight loss. In these participants, DII > of the median increased risk of MetS compared to participants with weight loss. This association was not observed among subjects with DII lower of the median. The risk of MetS was not associated in a participant with weight stability and weight loss across DIL and DII lower or higher than the median intake. In non-smoking participants, DIL and DII were not associated with MetS, regardless of weight change, after adjustments for confounding factors.
Discussion
In this population-based prospective study, we found that DII and DIL were associated with weight gain but not the MetS. These associations survived after accounting for several confounders, including age, gender, and energy intake. After stratification of participants by weight changes, DII, lower or higher than the median intake, was positively associated with risk of MetS in the weight gain ≥ 3%, but not in the weight gain stable and loss weight groups. We also observed a higher risk of MetS with a diet high in DII and DIL, weight gain ≥ 3% and low physical activity level. Although weight gain, independent of DIL, increased the risk of MetS in both men and women, but in weight stable status, a higher dietary DII and DIL increased the risk of MetS in women.
Previous studies have investigated the association between DII and DIL, cardiometabolic risk factors, and chronic diseases, including MetS, type 2 diabetes mellitus, and CVD [3, 13, 14, 16,17,18, 36], but the conclusion of these studies has been controversial. This may be due to that BMI and insulin resistance status appeared to modify the association between DII, DIL, and metabolic diseases [13, 16, 17, 19, 36]. Sensitivity analysis based on dysglycemia [17], weight changes [19], and overweight/obese status [13] showed that the DII and DIL are related to cardiovascular risk factors and chronic diseases only in obese or overweight participants [13, 17, 20]. In cross-sectional studies, DII was significantly inversely associated with HDL-C, positively associated with high TG and unhealthy metabolic status in obese, but not in overweight or normal weight participants [13, 20]. In addition, DII and DIL were positively associated with the risk of CVD only among participants with dysglycemia [17]. Moreover, DII and DIL were positively associated with MetS and obesity risk among type 2 diabetes mellitus [36], but not in participants without diabetes [16]. In the current study, we also found a positive association between DII and DIL, and MetS existed in subjects with weight gain ≥ 3%. According carbohydrate-insulin model of obesity, a diet that induces insulin secretion through the anabolic effects of insulin cause weight gain and insulin resistance. In addition, an insulinogenic diet through decreasing satiety, increasing the total energy intake, and increasing insulin growth factor-1 (IFG-1) induce body fat accumulation and obesity [37, 38]. Following obesity and insulin resistance, insulin concentrations increase by reducing the clearance rate. In this condition, diets that stimulate insulin secretion to lead to long-term insulin exposure and the development of metabolic diseases such as type 2 diabetes mellitus and prediabetes [39]. In line with this evidence, in the current study, the positive association between DII and DIL, and MetS was observed only among subjects with weight gain ≥ 3%. These associations between DIL and MetS were stronger among participants with DIL ≥ median intake. These findings suggest that a high-insulinogenic diet, by causing obesity, leads to metabolic diseases such as type 2 diabetes mellitus, MetS, and CVD.
This study found no association between DII, DIL, and MetS in participants with weight loss. It seems that weight loss via decreased incidence of insulin resistance and insulin resistance remission [40], even with consumption of an insulinogenic diet, decreases circulating insulin levels by increasing the clearance rate. Following the low concentration of circulation insulin, the progress of metabolic diseases such as MetS can prevent.
In stratified analyses of DII and DIL and risk of MetS by weight change and physical activity level, we found that weight gain, independent of DIL and DII, low or higher than the median intake, increased the risk of MetS in participants with low physical activity levels. However, this association was stronger among participants with DIL ≥ median. In participants with medium/high physical activity levels, DII and DIL, lower or higher than the median intake, and weight gains > 3%, were not associated with the risk of MetS. In other words, if all adults have moderate/high physical activity levels, weight gain ≥ 3% and an insulinogenic diet would not be associated with the risk of MetS. Our findings are in line with a previous study that showed the associations between an insulinemic diet and 4-y weight gain were more substantial among participants who were less physical activity [19], and adjustment for physical activity disappeared the association between DII and DIL and health status [20]. In active participants, compared to sedentary individuals, low insulinemic diets were associated with a lower concentration of urinary and plasma C-peptide as a valid measurement of insulin resistance and insulin secretion [41, 42]. Previous studies reported that physical activity mediated the acute insulin response through improvement in insulin resistance [43], and in a participant with insulin resistance and type 2 diabetes mellitus, physical activity decreased insulin secretion and increased insulin clearance [44]. Physical activity is a key modifiable for reducing metabolic disease. To delay the onset of MetS, along with recommendations for consumption of a low insulinogenic diet and weight management, moderate/vigorous physical activity is also advised.
Recent meta-analyses of prospective studies found that sex modified the effects of dietary glycemic index and glycemic load on CVD outcomes [45,46,47]. In addition, high glycemic diets have shown an adverse effect on HDL-C and triglyceride concentrations in women compared to men [48]. Regarding the insulinogenic diet, cross-sectional studies have also reported that adherence to a diet with higher DII and DIL was positively associated with MetS and obesity only among women but not men [15, 21]. In the current study, we found that weight gain, independent of DIL, increased the risk of MetS in both men and women. But in the condition of weight stability, low DII and DIL diet in women appears to have a more beneficial effect than in men. Further research is warranted to assess the effect of modification of weight change on metabolic disease according to sex.
Cigarette smoking is associated with greater insulin concentration, hyperinsulinemia, insulin resistance, and MetS [49, 50]. In the current study, smokers who manage their weight had no risk of MetS, regardless of their diet. However, among smokers with a weight gain > 3%, the risk of MetS increased with the consumption of an insulinogenic diet. In contrast to the findings of our study, the association between Dietary Index for Hyperinsulinemia and weight gain is stronger among never-smoker participants [19]. The synergic effects of smoking and diet on the incidence of MetS and the effect modifier of weight change on this relationship need further investigation.
The strength of the current study was the population-based prospective design, use of validated FFQ, using alternative approaches for the assessment of dietary intake, and investigation of the mediatory effect of lifestyle factors on the association between DII and DIL and MetS risk. Nevertheless, the present study had some limitations. First and foremost, consuming foods together can affect the insulinemic response. However, assessment of dietary intake via FFQs cannot determine which foods are consumed together. The study was carried out in the metropolitan area of Tehran, which may limit the generalizability of our findings, especially in rural zones. Third, relatively low duration of follow-up (8.9 years) is another limitation of this study. Further prospective studies with a long follow-up period (≥ 20 year) are needed to better understand the association between DII and DIL and risk of MetS. Fourth, Lack of data on post load insulin and glucose concentrations to calculate insulin secretion indexes is another limitation of the current study. Additionally, even though data were adjusted for all confounding factors, residual or unmeasured confounding factors such as genetic factors that influence weight change in subjects with metabolic syndrome may also contribute to these association.
Conclusion
Our findings suggest that the association between MetS risk and a hyperinsulinemic diet depended on weight changes. Moreover, the combined effects of weight changes and insulinogenic diet on the incidence of MetS were different among men and women. Furthermore, medium/high physical activity levels may offset the detrimental effect of weight gain and insulinogenic diet on MetS risk in weight gain status.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due institution’s policy but are available from the corresponding author on reasonable request.
Abbreviations
- MetS:
-
Metabolic syndrome
- DII:
-
Dietary insulin index
- DIL:
-
Dietary insulin load
- CVD:
-
Cardiovascular diseases
- TLGS:
-
Tehran Lipid and Glucose Study
- FFQ:
-
Food frequency questionnaire
- RIES:
-
Research Institute for Endocrine Sciences
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- Met:
-
Metabolic-equivalent
- MAQ:
-
Modifiable activity questionnaire
- FCT:
-
Food composition table
- FII:
-
Food insulin index
- FPG:
-
Fasting plasma glucose
- HDL-C:
-
High-density lipoprotein-cholesterol
- TG:
-
Triglyceride
- CV:
-
Coefficients of variation
- IFG-1:
-
Insulin growth factor-1
References
Gurka MJ, Filipp SL, DeBoer MD. Geographical variation in the prevalence of obesity, metabolic syndrome, and diabetes among US adults. Nutr Diabetes. 2018;8(1):14.
Tabatabaei-Malazy O, Saeedi Moghaddam S, Rezaei N, Sheidaei A, Hajipour MJ, Mahmoudi N, et al. A nationwide study of metabolic syndrome prevalence in Iran; a comparative analysis of six definitions. PLoS ONE. 2021;16(3):e0241926.
Mirmiran P, Esfandiari S, Bahadoran Z, Tohidi M, Azizi F. Dietary insulin load and insulin index are associated with the risk of insulin resistance: a prospective approach in tehran lipid and glucose study. J Diabetes Metab Disord. 2015;15:23.
Stumvoll M, Goldstein BJ, van Haeften TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet. 2005;365(9467):1333–46.
Wang H, Tian Y, Chen Y, Shen X, Pan L, Li G. Hyperinsulinemia rather than insulin resistance itself induces blood pressure elevation in high fat diet-fed rats. Clin Exp Hypertens. 2020;42(7):614–21.
Rachdaoui N, Polo-Parada L, Ismail-Beigi F. Prolonged exposure to insulin inactivates akt and Erk(1/2) and increases pancreatic islet and INS1E β-cell apoptosis. J Endocr Soc. 2018;3(1):69–90.
Peeters PJ, Bazelier MT, Leufkens HG, Auvinen A, van Staa TP, de Vries F, et al. Insulin glargine use and breast cancer risk: associations with cumulative exposure. Acta Oncol. 2016;55(7):851–8.
Kahleova H, Hlozkova A, Fleeman R, Fletcher K, Holubkov R, Barnard ND. Fat quantity and quality, as part of a low-fat, vegan diet, are associated with changes in body composition, insulin resistance, and insulin secretion. A 16-Week randomized controlled trial. Nutrients. 2019;11(3):615.
Mager DR, Mazurak V, Rodriguez-Dimitrescu C, Vine D, Jetha M, Ball G, et al. A meal high in saturated fat evokes postprandial dyslipemia, hyperinsulinemia, and altered lipoprotein expression in obese children with and without nonalcoholic fatty liver disease. JPEN J Parenter Enteral Nutr. 2013;37(4):517–28.
Gulseth HL, Gjelstad IMF, Tiereny AC, McCarthy D, Lovegrove JA, Defoort C, et al. Effects of dietary fat on insulin secretion in subjects with the metabolic syndrome. Eur J Endocrinol. 2019;180(5):321–8.
Holt SH, Miller JC, Petocz P. An insulin index of foods: the insulin demand generated by 1000-kJ portions of common foods. Am J Clin Nutr. 1997;66(5):1264–76.
Bao J, de Jong V, Atkinson F, Petocz P, Brand-Miller JC. Food insulin index: physiologic basis for predicting insulin demand evoked by composite meals. Am J Clin Nutr. 2009;90(4):986–92.
Nimptsch K, Brand-Miller JC, Franz M, Sampson L, Willett WC, Giovannucci E. Dietary insulin index and insulin load in relation to biomarkers of glycemic control, plasma lipids, and inflammation markers. Am J Clin Nutr. 2011;94(1):182–90.
Mozaffari H, Namazi N, Larijani B, Surkan PJ, Azadbakht L. Associations between dietary insulin load with cardiovascular risk factors and inflammatory parameters in elderly men: a cross-sectional study. Br J Nutr. 2019;121(7):773–81.
Sadeghi O, Hasani H, Mozaffari-Khosravi H, Maleki V, Lotfi MH, Mirzaei M. Dietary insulin index and dietary insulin load in relation to metabolic syndrome: the Shahedieh cohort study. J Acad Nutr Diet. 2020;120(10):1672–86.
Ghorbaninejad P, Imani H, Sheikhhossein F, Tijani Jibril A, Mohammadpour S, Shab-Bidar S. Higher dietary insulin load and index are not associated with the risk of metabolic syndrome and obesity in Iranian adults. Int J Clin Prac. 2021;75(7):e14229.
Teymoori F, Farhadnejad H, Mirmiran P, Nazarzadeh M, Azizi F. The association between dietary glycemic and insulin indices with incidence of cardiovascular disease: Tehran lipid and glucose study. BMC Public Health. 2020;20(1):1496.
Teymoori F, Farhadnejad H, Moslehi N, Mirmiran P, Mokhtari E, Azizi F. The association of dietary insulin and glycemic indices with the risk of type 2 diabetes. Clin Nutr. 2021;40(4):2138–44.
Tabung FK, Satija A, Fung TT, Clinton SK, Giovannucci EL. Long-term change in both dietary insulinemic and inflammatory potential is associated with weight gain in adult women and men. J Nutr. 2019;149(5):804–15.
Hajhashemy Z, Mirzaei S, Asadi A, Akhlaghi M, Saneei P. Association of dietary insulin index and dietary insulin load with metabolic health status in Iranian overweight and obese adolescents. Front Nutr. 2022;9:821089.
Anjom-Shoae J, Keshteli AH, Sadeghi O, Pouraram H, Afshar H, Esmaillzadeh A, et al. Association between dietary insulin index and load with obesity in adults. Eur J Nutr. 2020;59(4):1563–75.
de Mutsert R, Sun Q, Willett WC, Hu FB, van Dam RM. Overweight in early adulthood, adult weight change, and risk of type 2 diabetes, cardiovascular diseases, and certain cancers in men: a cohort study. Am J Epidemiol. 2014;179(11):1353–65.
Mirmiran P, Farhadnejad H, Teymoori F, Parastouei K, Azizi F. The higher adherence to healthy lifestyle factors is associated with a decreased risk of metabolic syndrome in Iranian adults. Nutr Bull. 2022;47(1):57–67.
Azizi F, Zadeh-Vakili A, Takyar M. Review of rationale, design, and initial findings: Tehran lipid and glucose study. Int J Endocrinol Metab. 2018;16(4 Suppl):e84777.
Hosseinpour-Niazi S, Aghayan M, Mirmiran P, Azizi F. Does weight change modify the association between the consumption of sugar-sweetened beverages and 100% fruit juice and the risk of metabolic syndrome? Clin Nutr. 2021;40(10):5261–8.
Kriska AM, Knowler WC, LaPorte RE, Drash AL, Wing RR, Blair SN, et al. Development of questionnaire to examine relationship of physical activity and diabetes in Pima Indians. Diabetes Care. 1990;13(4):401–11.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl):498–504.
Momenan AA, Delshad M, Sarbazi N, Rezaei Ghaleh N, Ghanbarian A, Azizi F. Reliability and validity of the modifiable activity questionnaire (MAQ) in an Iranian urban adult population. Arch Iran Med. 2012;15(5):279–82.
Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 2010;13(5):654–62.
Esmaeili M, Hushiarrad A. Iranian food composition table. Tehran: Shahid Beheshti University of Medical Sciences Press; 2018.
Hu FB, Stampfer MJ, Rimm E, Ascherio A, Rosner BA, Spiegelman D, et al. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999;149(6):531–40.
Bell KJ, Petocz P, Colagiuri S, Brand-Miller JC. Algorithms to improve the prediction of postprandial insulinaemia in response to common foods. Nutrients. 2016;8(4):210.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5.
Azizi F, Khalili D, Aghajani H, Esteghamati A, Hosseinpanah F, Delavari A, et al. Appropriate waist circumference cut-off points among Iranian adults: the first report of the Iranian National Committee of obesity. Arch Iran Med. 2010;13(3):243–4.
Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. Int J Obes (Lond). 2006;30(3):391–9.
Anjom-Shoae J, Namazi N, Ayati MH, Darbandi M, Najafi F, Oasdar Y. Dietary insulin index and load in relation to cardiometabolic risk factors in patients with type 2 diabetes mellitus: a cross-sectional study on the RaNCD cohort study. Nutrition. 2022;105:111830.
Joslowski G, Halim J, Goletzke J, Gow M, Ho M, Louie JC, et al. Dietary glycemic load, insulin load, and weight loss in obese, insulin resistant adolescents: RESIST study. Clin Nutr. 2015;34(1):89–94.
Yari Z, Behrouz V, Zand H, Pourvali K. New insight into diabetes management: from glycemic index to dietary insulin index. Curr Diabetes Rev. 2020;16(4):293–300.
van Vliet S, Koh HE, Patterson BW, Yoshino M, LaForest R, Gropler RJ, et al. Obesity is associated with increased basal and postprandial β-cell insulin secretion even in the absence of insulin resistance. Diabetes. 2020;69(10):2112–9.
Chang Y, Sung E, Yun KE, Jung HS, Kim CW, Kwon MJ, et al. Weight change as a predictor of incidence and remission of insulin resistance. PLoS ONE. 2013;8(5):e63690.
Lee DH, Giovannucci EL, Tabung FK. Insulin-related dietary indices predict 24-h urinary C-peptide in adult men. Br J Nutr. 2020;19:1–8.
Tabung FK, Wang W, Fung TT, Hu FB, Smith-Warner SA, Chavarro JE, et al. Development and validation of empirical indices to assess the insulinaemic potential of diet and lifestyle. Br J Nutr. 2016;8:1–12.
Ku CY, Gower BA, Hunter GR, Goran MI. Racial differences in insulin secretion and sensitivity in prepubertal children: role of physical fitness and physical activity. Obes Res. 2000;8(7):506–15.
Tuominen JA, Ebeling P, Koivisto VA. Exercise increases insulin clearance in healthy man and insulin-dependent diabetes mellitus patients. Clin Physiol. 1997;17(1):19–30.
Mirrahimi A, de Souza RJ, Chiavaroli L, Sievenpiper JL, Beyene J, Hanley AJ, et al. Associations of glycemic index and load with coronary heart disease events: a systematic review and meta-analysis of prospective cohorts. J Am Heart Assoc. 2012;1(5):e000752.
Dong JY, Zhang YH, Wang P, Qin LQ. Meta-analysis of dietary glycemic load and glycemic index in relation to risk of coronary heart disease. Am J Cardiol. 2012;109(11):1608–13.
Ma XY, Liu JP, Song ZY. Glycemic load, glycemic index and risk of cardiovascular diseases: meta-analyses of prospective studies. Atherosclerosis. 2012;223(2):491–6.
Knopp RH, Paramsothy P, Retzlaff BM, Fish B, Walden C, Dowdy A, et al. Gender differences in lipoprotein metabolism and dietary response: basis in hormonal differences and implications for cardiovascular disease. Curr Atheroscler Rep. 2005;7(6):472–9.
Artese A, Stamford BA, Moffatt RJ. Cigarette smoking: an accessory to the development of insulin resistance. Am J Lifestyle Med. 2017;13(6):602–5.
Kim SW, Kim HJ, Min K, Lee H, Lee SH, Kim S, et al. The relationship between smoking cigarettes and metabolic syndrome: a cross-sectional study with non-single residents of Seoul under 40 years old. PLoS ONE. 2021;16(8):e0256257.
Acknowledgements
This study, as part of MSc. thesis of Bayyeneh khoshnoudi-Rad, was supported by the Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences and Qazvin University of Medical Sciences, Qazvin, Iran. We express our appreciation to the participants of this study for their collaboration.
Funding
This work was supported by Qazvin University of Medical Sciences, Qazvin, and Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Author information
Authors and Affiliations
Contributions
SHN and PM conceptualized and designed the study. SHN, and BK analyzed and interpreted the data; SHN, BK, MJ, PM and FA drafted the initial manuscript; PM and FA supervised the project. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of the Research Institute for Endocrine Sciences (RIES), Shahid Beheshti University of Medical Sciences, and written informed consent was acquired from participants prior to their inclusion in the study.
Consent for publication
Not applicable.
Competing interests
On behalf of all authors, the corresponding author hereby declares that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Khoshnoudi-Rad, B., Hosseinpour-Niazi, S., Javadi, M. et al. Relation of dietary insulin index and dietary insulin load to metabolic syndrome depending on the lifestyle factors: Tehran lipid and glucose study. Diabetol Metab Syndr 14, 198 (2022). https://doi.org/10.1186/s13098-022-00968-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00968-w