Abstract
Although physical activity is widely recommended for preventing and treating cardiovascular complications of type 2 diabetes mellitus (T2DM), the underlying mechanisms remain unknown. MicroRNA-126 (miR-126) is an angiogenetic regulator abundant in endothelial cells (ECs) and endothelial progenitor cells (EPCs). It is primarily involved in angiogenesis, inflammation and apoptosis for cardiovascular protection. According to recent studies, the levels of miR-126 in the myocardium and circulation are affected by exercise protocol. High-intensity interval training (HIIT) or moderate-and high-intensity aerobic exercise, whether acute or chronic, can increase circulating miR-126 in healthy adults. Chronic aerobic exercise can effectively rescue the reduction of myocardial and circulating miR-126 and vascular endothelial growth factor (VEGF) in diabetic mice against diabetic vascular injury. Resistance exercise can raise circulating VEGF levels, but it may have a little influence on circulating miR-126. The Several targets of miR-126 have been suggested for cardiovascular fitness, such as sprouty-related EVH1 domain-containing protein 1 (SPRED1), phosphoinositide-3-kinase regulatory subunit 2 (PIK3R2), vascular cell adhesion molecule 1 (VCAM1), high-mobility group box 1 (HMGB1), and tumor necrosis factor receptor-associated factor 7 (TRAF7). Here, we present a comprehensive review of the roles of miR-126 and its downstream proteins as exercise mechanisms, and propose that miR-126 can be applied as an exercise indicator for cardiovascular prescriptions and as a preventive or therapeutic target for cardiovascular complications in T2DM.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) is a metabolic disorder defined by serum glucose concentrations. The underlying pathophysiology is related to insulin resistance (IR), and β cell failure is required for diabetes to develop. It is characterized by hyperglycemia or hyperinsulinemia which would cause macrovascular and microvascular complications [1]. Epidemiological data have shown that cardiovascular disease (CVD) affects approximately 32.2% of patients with T2DM, accounting for over half of all fatalities recognized as a primary cause of mortality in them [2]. Glycemic control can decrease the glycated hemoglobin value and reduce macrovascular risks in patients with T1DM [3]. It seems that intensified glycemic therapy may reduce CVD risk in younger patients with recent-onset T2DM but not in high-risk older individuals with established disease [4]. A meta-analysis of data even shows that intensive glucose-lowering treatment has no benefits on death from cardiovascular causes in patients with T2DM [5]. Consequently, physical exercise as one of the first management strategies has been recommended to improve glycometabolism for cardiovascular benefits [6].
In one survey for over eight years, people with diabetes who walk at least 2 h per week have a 34% reduction in CVD mortality compared to those who do not exercise [7]. Exercise can reduce cardiovascular inflammation, blood pressure, and glucose metabolism. It has been reported to prevent the generation of reactive oxygen species (ROS) and ischemia damage, has anti-fibrosis and anti-apoptosis capabilities on diabetic myocardial and endothelial cells [8, 9]. The American Association of Clinical Endocrinologists and American College of Endocrinology recommend that each people with T2DM needs individualized exercise prescriptions to exert the maximum impact of exercise on the cardiovascular system [10]. Nevertheless, the underlying mechanisms of exercise in diabetic CVD are poorly understood.
MiRNAs are non-coding RNAs with a length of 20 ~ 24 nucleotides that can recognize the 3'-untranslated region of mRNA and inhibit the post-transcription target. They have been recognized as chemical messengers that regulate biological processes such as cell proliferation, differentiation, and survival [11]. Dysregulation of miRNAs leads to abnormal transcription of target mRNAs, which is believed to be related to various diseases. For example, circulating miR-126 is down-regulated throughout the pathophysiological processes of T2DM [12]. MiR-126 plays an essential role in the health of ECs, since mice with its deletion exhibit severe vascular leakage, dysfunction, and hemorrhaging [13]. Interestingly, aerobic exercise can partially rescue miR-126 abundance in diabetic cardiac muscle and stimulate myocardial angiogenesis by activating the vascular endothelial growth factor (VEGF) pathway [14]. Exercise can also increase circulating endothelial progenitor cell (EPC)-exosomes and their carried miR-126 for vascular repair in patients with T2DM [15].
In this review, we summarize the impact of diabetes and exercise on the abundance of miR-126, and highlight the role of miR-126 and its downstream targets that have been confirmed to participate in angiogenesis, vascular inflammation, cardiac autophagy and endothelial apoptosis. Current evidences suggest that miR-126 can be an exercise indicator for cardiovascular health and as a preventive or therapeutic approach for cardiovascular complications of T2DM.
Vascular pathophysiology in T2DM
Diabetic vascular disorders mainly include atherosclerosis, hypertension, and peripheral artery disease, which are developed by the abnormalities in ECs and vascular smooth muscle cells (VSMCs). ECs are located on the vasculature's inner lining for the regulation of blood flow and pressure, and the functions of leukocytes and platelets. Diabetes dramatically accelerates vascular inflammation and the formation of atherosclerotic plaques. Atherosclerotic plaque is formed by the accumulation of apoptotic ECs and macrophages, the migration and proliferation of VSMCs, and the deposits of lipid in the intima with fibrous tissue proliferation and calcinosis, which can result in severe vascular complications such as myocardial infarction or stroke [16]. The fundamental pathophysiology of diabetic macroangiopathy is depicted in Fig. 1. Furthermore, diabetes-related microvascular pathology is characterized primarily by sparse capillaries, excessive vascular permeability, and abnormal neovascularization, which eventually leads to local edema and microvascular inflammation [17, 18].
Vascular pathology in T2DM. T2DM induces macrovascular and microvascular dysfunction by hyperglycemia and hyperinsulinemia. Diabetic macroangiopathy (atherosclerosis) is made of intimal hyperplasia, foam cell infiltration, arterial wall calcification, and lumen stenosis. Capillary immature and increased permeability are features of diabetic microangiopathy. In diabetic cardiomyopathy, infiltrating inflammatory cells induce cardiac enlargement and fibrosis. All these pathological alters lead to diabetes-related heart failure. The arrow in the image means high permeability through apoptosis of ECs
Hyperglycemia, hyperinsulinemia, and insulin resistance/insufficiency are the primary reasons of vascular injury in diabetes. Hyperglycemia inhibits endothelial NO synthase (eNOS) and induces oxidative stress through polyol, advanced glycation end products (AGEs), hexosamine, and protein kinase C pathways [19]. Hyperinsulinemia caused by IR induces reduction of the translocation of glucose transporter 4 (GLUT4), the accumulation of diacylglycerol and cellular lipids, impairment of insulin signal pathway, and metabolism problems [20]. Therefore, these pathological changes in T2DM contributes to the incidence and development of macrovascular and microvascular complications.
MiR-126 expression in diabetic cardiovascular complications
Decreased miR-126 as a possible cardiac biomarker of T2DM
MiR-126 located in intron 7 of the EGFL7 gene, is exclusively expressed in ECs and EPCs. It can affect the translation of endothelial-specific proteins to maintain endothelial functions. Moreover, obesity [21], diabetes [22, 23] and exercise [14, 15] have been shown to regulate the miR-126 expression. In patients with T2DM, miR-126 is an independent predictor for long-term all-cause death and likely to be an epigenetic predictor/mediator of cardiovascular complications [24]. Low level of miR-126 in plasma and in the coronary venous sinus and aorta is significantly associated with left ventricular function and cardiac repair potential in heart failure patients [25]. In addition, several logistic regression analyses indicate that hyperglycemia decreases the concentration of miR-126 in the heart [22] and plasma [23], which contributes to diabetic macroangiopathy and microangiopathy [26, 27].
The two strands of pre-miR-126 develop into miR-126-3p and miR-126-5p. Unlike several other miRNAs, the pre-miR-126 passenger strand (miR-126-5p) is not degraded and substantially has functions as the guide strand (miR-126-3p). They have the ability to identify complementary mRNA molecules and significantly trigger target mRNA degradation or translation silencing [28]. The targets of miR-126-3p predicted by Targetscan and MiRanda analysis have been verified to play a role in cardiovascular mainly including phosphoinositide-3-kinase regulatory subunit 2 (PIK3R2) [29], sprouty-related EVH1 domain-containing protein 1 (SPRED1) [30], VCAM-1 [31], and tumor necrosis factor receptor-associated factor 7 (TRAF7) [32]. The targets of miR-126-5p include high-mobility group box 1 (HMGB1) [33], activated leucocyte cell adhesion molecule (ALCAM) [34] and Notch1 inhibitor delta-like1 homolog (Dlk1) [35]. As shown in Table 1, these targets are primarily involved in angiogenesis, vascular inflammation, and EC apoptosis, which might explain why circulating low levels of miR-126 have been regarded as a biomarker for diabetic cardiovascular diseases. Although miR-126-3p has many benefits on endothelial function, it can induce atherosclerosis by increasing VSMCs proliferation via insulin receptor substrate-1 (IRS-1) inhibition [36]. IRS-1 is considered to be a risk factor for coronary artery disease [37] and its activation in the hearts of patients with T2DM induces a lower myocardial glucose utilization [38]. Additionally, miR-126-3p also suppresses target gene insulin receptor substrate-2 (IRS-2) to inhibit β cell proliferation closely correlated with the IR [39]. Thus, miR-126 and their distinct targets provide new mechanistic insights into energy metabolism and diabetic vascular complications.
EPCs deficiency in diabetic vascular complications
Circulating EPCs derived from bone marrow cells contribute to vascular repair by incorporating them into ECs monolayers and secreting vascular growth factors [44]. A low concentration of circulating EPCs defineded with CD34 + and kinase insert domain-conjugating receptor (KDR) + cells independently predicts a fourfold increase in the incidence of cardiovascular events in coronary artery disease patients [45]. Moreover, in multivariate analysis, reduced circulating EPC levels are a significant, independent predictor of poor prognosis for established cardiovascular disease [45]. Diabetes impairs both the quantity and function of circulating EPCs [46]. Anti-diabetic drug ticagrelor could significantly increase circulating EPCs in diabetic patients with non-ST elevation acute coronary syndrome [47]. Besides, EPCs isolated from obese diabetic mice significantly have reduced the ability of angiogenesis in vitro and even an anti-angiogenesis phenotype [48].
MiR-126 is abundant in EPCs and increases the proliferation, migration and tube-like structures of EPCs by targeting VEGF pathway [49, 50]. Injection of EPCs with overexpressing miR-126 can induce reendothelialization and endothelial healing by promoting extracellular signal-regulated kinase (ERK)/VEGF and Akt/eNOS signaling pathways in non-obese diabetic rats with carotid artery injury [51]. Microvesicles (MVs) released from EPCs as a kind of extracellular vehicle (EV) can modulate cell migration, apoptosis, and oxidative stress [46]. The protective effects of EPC-MVs are compromised in diabetes due to the reduction of their carried miR-126 [46]. It is acknowledged that EV is an effective way to avoid miRNAs degradation during transport. MiRNAs carried by EVs can have a variety of physiologic and pathological functions by suppressing their post-transcription of target mRNAs [52]. For example, EV can protect against acute myocardial ischemia injury by lowering cell apoptosis and increasing cell survival via carrying miR‑126 -3p by PIK3R2/VEGF signaling pathway [53, 54]. Therefore, EPCs or their EV can provide a resource of miR-126 and promote vascular repair for diabetic vascular complications.
MiR-126 expression induced by exercise
Exercise can be classified into acute and chronic exercises according to exercise time, and aerobic and resistance exercise based on oxygen metabolism. Exhausted exercise, high-intensity interval training (HIIT), and high-, medium-, or low-intensity exercise are all classified by intensity. The current study shows that aerobic exercise is proposed to be more effective than resistance training (RT) in reducing endothelial activation markers and inflammatory cytokines [55]. Particularly, the expression of miR-126 can be comprehensively influenced by various exercise. Thus, we summarize the results of miR-126, VEGF, EPCs, and EPC-exosomes after different exercise protocols in myocardium and circulation in Table 2.
MiR-126 expression is increased by aerobic exercise
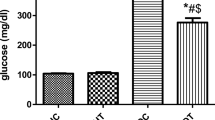
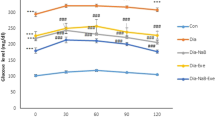
The expression profile of circulating miRNAs provides insight into the potential exercise mechanism of the cardiovascular system, in which miR-126 is one of these miRNAs that can be directly altered by exercise intervention [81]. Based on the few studies conducted so far, chronic aerobic exercise has been demonstrated to raise circulating and myocardial miR-126 levels in both healthy and diseased people. As shown in Table 2, four weeks of high-intensity exercises can elevate the level of circulating miR-126 in healthy individuals [62, 63]. Moreover, ten weeks of moderate-and high-volume swimming in Wister rats significantly increases the level of circulating miR-126 with exercise-induced cardiac angiogenesis in a dose–response manner [73]. Chronic running increases the myocardial expression of miR-126 in STZ rats and db/db mice [22, 72], but has no impact on circulating miR-126 [72]. Likewise, there is no change of miR-126 in the hypertensive rat’s plasma after ten-week swimming, but the level of its downstream target gene protein PIK3R2 reduces from an increase of 51% to normal [79]. The comparative study on chronic exercise of diabetic mice from 8-week-old and 16-week-old indicates that early exercise intervention can increase myocardial miR-126 and VEGF, and better improve the onset and progression of diabetic heart disease [72]. Combination of exercise and diet control for six weeks in obese adolescents increases serum miR-126 and vascular endothelial diastolic functions [82]. These findings suggest that miR-126 could be the essential molecule influenced by chronic aerobic exercise in a dose–response manner and might be involved in early protecting the cardiac function.
Acute aerobic exercise is a single bout of aerobic activity that usually uses % maximal oxygen uptake (V̇O2max) to measure the intensity of exercise. V̇O2max is the highest oxygen consumption attainable during maximal or exhaustive exercise per minutes. A single symptom-limited exercise test is a kind of exhaustion test. When a healthy subjects perform this test by bicycling, the circulating miR-126 will be increased [56]. After a 30-min aerobic exercise at 75% V̇O2max in obese adults, circulating miR-126 is also increased and is continued to increase 1 h [70]. A 42-km marathon can immediately increase plasma miR-126 by 1.9-fold in trained runners, and then decline to pre-race level within 24 h [60]. Uhlemann and colleagues believed that the rise of circulating miR-126 after an acute aerobic exercise as evidence of damage of the ECs layer [56]. However, the fact is that neither mature ECs exfoliation nor ECs monolayer injury occurs after exercise, even after 30 min of acute cycling at 85% peak power [57]. Tissue hypoxia induced by high-intensity exercise might be responsible for the increase of miR-126 expression. Hypoxia induces the expression of hypoxia-inducible factor -1α (HIF-1α) and its downstream Ets-1 which can regulate miR-126 in vascular ECs [83, 84]. In addition, EPCs promoted from the bone marrow into the bloodstream might be another reason for circulating miR-126 increase. However, the circulating EPCs do not change in T2DM patients following a 30 min-treadmill exercise at 60% V̇O2max [61] and increase in marathon athletes and in mice by eight week-aerobic exercise [15, 65]. Therefore, miR-126 expression/release can be different in different conditions of health, and after different protocols of aerobic exercise. It is recommended that exercise with moderate intensity or above can significantly increase circulating miR-126.
MiR-126 expression is increased by HIIT
HIIT consists of bouts of more than 90% V̇O2max followed by a brief rest period and seems to induce larger beneficial adaptation in the cardiovascular system [85]. Even a session of HIIT can completely prevent the normal postprandial reduction of endothelial function [86] and increase the circulating miR-126 levels including miR-126-3p and miR-126-5p in healthy individuals [57, 58]. In clinical experiments, the isolated high-density lipoprotein from chronic heart failure patients after moderate intensity exercise training rescues the miR-126 reduction in co-cultured ECs compared with no-exercise chronic heart failure patients [87]. In addition, the study finds that high volume training (HVT) with cycling for 130 min at 55% peak power output (PPO) could significantly elevate serum miR-126 level immediately [58]. One session of HVT with 90 min cycling at 60% PPO dramatically raises circulating miR-126 abundance in young male cyclists, but 4 × 4 min HIIT at 90–95% PPO had no influence [59]. Schmitz and colleagues also found that no acute elevation of circulating miR-126 was observed after HIIT with running 4 × 30 s at maximum speed in moderately trained students, but obviously elevated after four-week training sessions [63]. Therefore, HIIT can increase the abundance of serum miR-126, but it is influenced by training level of the subjects and the amount of exercise time.
MiR-126 expression is affected by resistance exercise
Resistance training (RT) has remarkable cardiovascular benefits. For example, a 12-week training program consisting of moderate-intensity resistance exercise improved cardiovascular fitness in overweight and obese participants [88]. RT is recommended to improve blood pressure, reduce arterial stiffness, and benefit for glycemic control as a complement to aerobic exercise programs [89]. It has been shown that the strength training intervention for one week has no impact on the circulating miR-126 among older diabetic patients and control subjects [71]. The researchers observe that decreased miR-126 in muscle biopsies could reliably distinguish between powerlifters and controls, implying that it might help define the powerlifter phenotype [69]. Although RT does not enhance the plasma level of miR-126, it still promotes a rise in serum VEGF and the level of circulating EPCs [66, 67]. The increase of plasma VEGF and HIF-1α after anaerobic RT is probably due to muscle ischemia during exercise [67]. Eccentric training is another strength training technique which is also confirmed to cause an increase of HIF-1α in untrained skeletal muscle and to up-regulate VEGF and eNOS expressions [90]. Therefore, RT has cardiovascular and muscular effects, but its mechanism may not be associated to miR-126.
The level of miR-126 in EPCs and EPC-EVs is increased by exercise
EPCs carried miR-126 may contribute to exercise-induced cardiovascular protection. After 12 h of a marathon, professional runners had a higher circulating percentage of EPCs which is accompanied by favorable effects on heart rate and blood pressure [65]. In diabetes patients, although circulating EPC-EVs are increased, their carried miR-126 and the expression of VEGF receptor 2(VEGFR-2) are decreased [46]. Surprisedly, exercise can significantly increase the number of circulating EPCs and EPC-exosomes and their carried miR-126 in mice, which protects ECs against from hyperglycemia-induced damage [15]. Our study showed that long-term moderate exercise mice promoted a higher circulating EPC-exosomes which could alleviate the dysfunction of injured ECs via SPRED1 downregulation and VEGF upregulation [15]. Furthermore, three years of regular endurance resistance exercise increased the circulating levels of EPCs and VEGF [66]. However, a 30-min running at 60% V̇O2max could not change the number of EPCs in the impaired glucose tolerance and T2DM subjects, only conversely increases in the control group [61]. Thus, chronic exercise may provide a potential approach to reduce diabetic vascular complications by elevating the number of EPCs, EPC-EV, and its carried miR-126.
Mechanism of exercise-induced miR-126 in improving cardiovascular function in diabetes
Exercise-induced miR-126 should be a valuable marker for optimizing individual training interventions based on its biological effects. MiR-126 has multiple functions such as glucose metabolism, neovascularization, inflammatory resistance, autophagy, and anti-apoptosis effects by modulating the expressions of its target genes. Figures 2 and 3 summarize the targets of miR-126 elicited by exercise for the beneficial effects on cardiovascular health in diabetes.
The mechanism of exercise in improving cardiovascular function in diabetes. Exosomes carried miR-126-3p/-5p plays an important role in control of angiogenesis, autophagy, anti-apoptosis, and glycogenesis, which together contribute to improve diabetic cardiovascular health in diabetes. SPRED1 and PIK3R2 suppress VEGF by separately inactivating the downstream Ras/Raf-1/ERK and PI3K/Akt signaling pathways. Akt phosphorylation is related to autophagy by affecting FoxO and mTOR, as well as anti-apoptosis by increasing Bcl-2. Akt can also phosphorylate glycogen synthase kinase-3β(GSK3β) for inactivation, which reduces inhibition of GS to increase glycogen
The molecular mechanisms of exercise-induced exosomal miR-126 for anti-inflammation in diabetes. Exercise-induced exosomes modify the downstream target genes IκBα, HMEB1, and VCAM-1 via their carried miR-126. The anti-inflammatory effects in diabetic cardiovascular system are achieved by inhibiting inflammatory substances, such as HMGB1 and TNF-a activate IKK to enhance phosphorylation of the NF-κB (p65 and p50) complex. Then NF-κB enters the nucleus via nuclear pore to stimulate IκBα genes and NF-κB target genes production, which can activate the NF-κB inflammatory pathway
Glycometabolism
Exercise has the potential to improve glycemic control in diabetes depending on the duration and intensity of physical activity. For example, a single bout of moderate-intensity aerobic exercise reduces fasting glucose (FG) level, but less effectively than HIIT in patients with T2DM [91]. Resistance exercise can lead to a modest reductions in FG [68, 92, 93]. RT enhances glucose uptake via increasing transport of glucose into skeletal muscle by GLUT4 translocation [94, 95]. The major molecular pathways of aerobic exercise are associated with insulin sensitivity improvement which can increase skeletal muscle glucose absorption by reducing adipokines, inflammation, and oxidative stress [96]. RT can also considerably lower the inflammatory biomarker C-reactive protein, total cholesterol, and low-density lipoprotein cholesterol to increase insulin sensitivity and decrease the risk of CVD [68, 92]. The expression of miR-126 can be surprisingly increased or maintained well in circulating EPC-MVs when the plasma glucose level is well-controlled in diabetic patients by drug management [46]. It assumes that exercise has a significant influence on the increase of miR-126, which might be mediated by blood glucose regulation, but this has yet to be verified.
MiR-126 is closely associated with glucose homeostasis. The study finds that the glycogen content is much more in the placentas of miR-126−/− mice [97]. Akt activation is a critical step to phosphorylate GSK3β in glycogen synthesis process. It is evidenced that miR-126 enhances the biological function of EPCs under oxidative stress via PI3K/Akt/GSK3β signaling pathways [98]. Interestingly, there is an increase in cardiac IRS1-PI3K activity and a reduction of GLUT4 in patients with T2DM [38]. MiR-126 is a negative regulator of IRS-1 [99] and can be increased by exercise which improves insulin sensitivity and the activation of Akt in diabetic heart [15, 100]. However, exercise does not enhance IRS-1-mediated PI3K activity, but up-regulate GLUT4 protein expression in diabetic skeletal muscle [101]. Moreover, exercise can decrease [102] or increase [103] myocardial glycogen synthesis. A report showed that 13-week swimming significantly reduced high blood glucose and cardiac glycogen in Zucker diabetic fatty rats via Akt/GSK3 signaling pathway [102]. Another study found that exercise did not correct abnormal cardiac glycogen accumulation in the db/db mice [103]. The mechanism of exercise induced glycogen production is complicated in diabetic heart. The AMP-activated protein kinase (AMPK) pathway also directly controls carbohydrate metabolism. Although AMPK activation enhances cellular glucose absorption and decreases glycogen production by inhibiting glycogen synthase activity, glucose-induced allosteric activation of glycogen synthase can mask the effect of AMPK to promote glycogen accumulation, contributing to metabolic disorders [104]. Whether miR-126 participates in the exercise-related glycogen alteration requires further investigation.
Angiogenesis
As shown in Table 1 and Fig. 2, SPRED1 and PIK3R2 are two essential miR-126-3p targets in the promotion of ECs growth and migration. SPRED1 is a member of the sprouty/spred protein family which can suppress VEGF by inactivating the downstream Ras/Raf-1/ERK signaling pathway [49]. By targeting the SPRED1 and PIK3R2, miR-126 regulates vascular endothelium permeability and angiogenesis [29]. Moreover, eNOS can be activated by PI3K/Akt/VEGF dependent pathway to control vasodilatation [105]. High glucose suppresses angiopoietin-1 (Ang-1) through the miR-126/PIK3R2 pathway in ECs [106]. This pathway not only fine-tunes VEGF-signaling on the formation of the initial vascular plexus but also strongly enhances the activity of Ang-1 on vessel stabilization and maturation. In addition, Notch1 inhibitor delta-like1 homolog (Dlk1) is the target gene of miR-126-5p that can inhibit Notch1 activation and limit G1-S phase progression to proliferation, up-regulation of miR-126-5p consequently can preventing the pathological process of atherosclerosis by inhibiting Dlk1 [35].
MiR-126/VEGF pathway is an essential exercise mechanism in diabetic cardiovascular protection. Exercise modulates miR-126 and its targets for physiological response and adaptation. Chronic and acute aerobic exercise promotes an increase in myocardial capillary/fiber ratio via miR-126/SPRED1 and PIK3R2 pathways in rats [73]. Particularly, acute HIIT can raise circulating VEGF, although its effect on circulating miR-126 is controversial [59, 62]. Therefore, based on the responses of miR-126 and VEGF, more consideration should be given to choosing appropriate intensity exercise for angiogenesis, such as HIIT or chronic aerobic exercise with moderate intensity.
Anti-inflammation
The vascular inflammation is a crucial cause of accelerating atherosclerosis and diabetic vascular disorder. Nuclear factor-kappa B (NF-κB) plays a central role in the induction of many pro-inflammatory cytokines to regulate cell stress, cell survival, and cell proliferation. Likewise, NF-κB in diabetic heart is medicated by tumor necrosis factor-α (TNF-α), interleukin-1(IL-1), and interleukin-6 (IL-6) contributing to IR development and cardiac dysfunction [107]. Exercise has significant benefits on the reduction of oxidative stress and vascular inflammation depending on the appropriate exercise protocols. Moderate endurance exercise always exerts an anti-inflammatory effect by inhibiting pro-inflammatory cytokines [108], reducing NF-κB activation [109], limiting IR [110] and reserving mitochondrial activity [111]. Even a single session of aerobic exercise also can lower postprandial lipemia, monocytic TNF, and NF-κB activity in peripheral blood mononuclear cells against high-fat diet-induced inflammation [112, 113]. Interestingly, IκBα is a physiological inhibitor protein of NF-κB, and its phosphorylation by IκB kinase (IKK) promoting ubiquitination and active NF-κB release [114]. NF-κB p65 and NF-κB p50 can be transferred into the nucleus, stimulating IκBα and pro-inflammatory cytokines gene expressions, and then moved from the nucleus via the nuclear pore to cytoplasm by binding with IκBα. MiR-126 is an important regulatory factor in the inflammatory response, because it can directly inhibit IκBα [115]. However, the study found that IκBα protein did not alter during moderate activity but considerably was reduced by exhaustive exercise [31]. It is suggested that the increased inflammation may be closely related to exercise load.
Patients with T2DM have a high incidence rate of CVD partly due to vascular inflammation that accelerates atherosclerosis and diabetic endothelial dysfunction. Many inflammatory mediators are involved in this process, such as increased IL-6, VCAM-1, and monocyte chemoattractant protein [116]. As the downstream target of NF-κB, VCAM-1 targeted by miR-126-3p can be up-regulated by hyperinsulinemia [117, 118]. Aerobic exercise training can reduce soluble VCAM-1 and decrease leukocyte adherence [119]. In addition, miR-126 also controls the sirtuin 1 (SIRT1) and superoxide dismutase-2 expression against ROS imbalance in hind limb ischemia-subjected ob/ob mice [120]. Exercises decrease ROS production and increase NO availability in hypertensive patients [121] and the diabetic patients [122]. Inhibiting miR-126 increases the inflammatory markers and ROS generation in EPCs cultured under hyperglycemic conditions by PI3K/Akt pathway [123], which is crucial for modulating EPC migration and proliferation in T2DM [49, 123].
As a nuclear non-histone DNA-binding protein, HMGB1 is suppressed by miR-126-5p. HMGB1 level is increased in the serum of hyperglycemic rats and the management of hyperglycemia with insulin might decrease serum HMGB1 level [124]. HMGB1 could up-regulate toll-like receptors (TLR) [125] and receptor for advanced glycation end-products (RAGE) to enhance proinflammatory activities [126]. A tight junction complex composed of Claudin, Occluding, and ZO-1 is down-regulated potentially by the HMGB1/RAGE/Erk signaling pathway in the differentiated epithelium [126]. Overexpressing miR-126 in ECs under hyperglycemic condition could decrease inflammatory cytokines including TNF-α, ROS, and NADPH oxidase activity by inhibiting HMGB1 [33]. Human umbilical cord mesenchymal stem cell-derived exosomes carried overexpressing miR-126 alleviate the hyperglycemia-induced inflammation by reducing HMGB1 in human retinal ECs [127]. Moreover, HMGB1 is negatively related to post-exercise heart rate recovery in post-infarction patients, indicating that HMGB1 was involved in autonomic dysfunction during exercise [128]. As shown in Fig. 3, exercise decreases inflammation and improves diabetic cardiovascular function, probably through the miR-126-5p/HMGB1 pathway.
Autophagy
Autophagy is a critical defense mechanism for myocardial cell protection. It plays an important role in maintaining homeostasis by restoring or eliminating damaged organelles and lipids. MiR-126 regulates the level of beclin-1 and improves cardiac function after acute myocardial infarction [129]. Beclin-1 is a specific mediator of autophagy that can be phosphorylated on Thr388 by AMPK [130], and its absent reduces excessive autophagy-induced cardiomyocyte death in the diabetic heart [131]. In addition, beclin-1 can be phosphorylated by unc51-like kinase1 (Ulk1) in response to amino acid deficiency and mTOR inhibition [132]. mTOR complex1 inhibits autophagy and regulates cell survival in brain injury and disease through the insulin/PI3K/Akt signaling pathway [133]. T2DM patients often have autophagy deficiency. Metformin increases autophagy flux in cardiomyocytes by activating SIRT1 or AMPK phosphorylation, contributing to cardio-protection [134]. On the contrary, antihyperglycemic medications through the insulin pathway decrease autophagy and exacerbate heart failure [134]. MiR-126-induced loss of IRS-1 suppresses glucose uptake, leading to energy deprivation, and its depletion can reduce autophagy by AMPK-dependent phosphorylation of Ulk1 [135].
Glycophagy is an alternative pathway for cytosolic glycogen storage and degradation. Starch Binding Domain 1 (STBD1) is linked to the Atg8 family member GABA Type A Receptor Associated Protein Like 1 (GABARAPL1) at the N-terminus and glycogen at the C-terminal CBM20 domain. This process subsequently stimulates glycogen phagocytosis and lysosome fusion, which leads to autophagosome maturation. Excess glycogen can then be removed from the lysosome by acid alpha-glucosidase (GAA) [136, 137]. Unlike the macrophagy, cardiomyocyte glycophagy occurs under the condition of insulin and exogenous high glucose necessarily accompanied by an increase in STBD1 expression [138]. Thus, as shown in Fig. 2, the reduction of miR-126 in diabetes myocardium is associated with autophagy and glycogen synthesis, which lead to glycogen pathology in the myocardium. So far, the regulatory mechanisms of exercises on glycogen accumulation and glycophagy are still inconclusive, and whether it is related to miR-126 needs further elucidation.
Anti-apoptosis
Hyperglycemia causes the apoptosis of ECs and pancreatic β cells, aggravating the development of diabetic vascular complications [139]. MiR-126-5p inhibits cell apoptosis via its direct target protein TRAF7 which is one of the TRAF proteins involved in cell death and survival [32]. TRAF7 is a crucial regulatory protein that regulates whether the NF-κB transcription factor is activated or repressed [140]. TRAF7 also suppresses ECs apoptosis by increasing unusual polyubiquitination of the cellular fas-associated death domain-like IL-1-converting enzyme inhibitory protein (c-FLIP) [141] and the caspase-3-dependent pathway [142]. MiR-126-3p improves cell survival and decreases the expression of Bax and caspase-3 in high-glucose-induced human retinal ECs via targeting IL-17A and activating the PI3K/Akt pathway [143]. Due to the prevention of vascular apoptosis, exercise improves cardiovascular function. Aerobic exercise training significantly lowered blood pressure and heart rate in spontaneously hypertensive rats by increasing Bcl-2 levels [79]. Treadmill exercise promotes p-Akt expression, which assisted in the reduction of retinal apoptosis and neuron apoptosis in diabetic mice [144]. These findings imply that miR-126 and its downstream targets may be involved in the prevention of high glucose-induced apoptosis.
Conclusions
Exercise is an important method for reducing cardiovascular risk and mortality rate in T2MD. MiR-126 can promote angiogenesis, decrease vascular inflammation, regulate autophagy and reduce endothelial apoptosis by targeting its downstream proteins. Endurance aerobic exercise with moderate-intensity or above can raise the level of circulating and myocardial miR-126 in diabetes, whereas RT need further investigation. Chronic aerobic exercise is preferred to acute ones for long-term advantages in the expressions of miR-126 and VEGF. MiR-126 is responsible for the beneficial effects of exercise and could be applied as an exercise indicator for cardiovascular prescriptions and as a preventive or therapeutic target for cardiovascular complications in T2DM.
Availability of data and materials
Not applicable.
Abbreviations
- T2DM:
-
Type 2 diabetes mellitus
- ECs:
-
Endothelial cells
- EPCs:
-
Endothelial progenitor cells
- SPRED1:
-
Sprouty-related EVH1 domain-containing protein 1
- PIK3R2:
-
Phosphoinositide-3-kinase regulatory subunit 2
- HMGB1:
-
High-mobility group box 1
- VCAM1:
-
Vascular cell adhesion molecule 1
- TRAF7:
-
Tumor necrosis factor receptor-associated factor 7
- CVD:
-
Cardiovascular disease
- ROS:
-
Reactive oxygen species
- m-miR-126:
-
Myocardial miR-126
- c-miR-126:
-
Circulating miR-126
- mu-miR-126:
-
Muscle-miR-126
- VSMCs:
-
Vascular smooth muscle cells
- IR:
-
Insulin resistance
- eNOS:
-
Endothelial NO synthase
- AGEs:
-
Advanced glycation end products
- GLUT4:
-
Glucose transporter 4
- IRS-1:
-
Insulin receptor substrate-1
- GSK3:
-
Glycogen synthase kinase-3
- KDR:
-
Kinase insert domain-conjugating receptor
- VEGF:
-
Vascular endothelial growth factor
- MVs:
-
Microvesicles
- EV:
-
Extracellular vehicle
- ERK:
-
Extracellular signal-regulated kinase
- SHR:
-
Spontaneously hypertensive rats
- MI:
-
Myocardial infarction
- STZ rats:
-
Rats by streptozotocin injection
- V̇O2max :
-
Maximal oxygen consumption
- HIIT:
-
High intensity interval training
- HVT:
-
High volume training
- MT:
-
Moderate training
- PPO:
-
Peak power output
- RT:
-
Resistance training
- CE:
-
Chronic exercise
- FG:
-
Fasting blood glucose
- Ang-1:
-
Angiopoietin-1
- Dlk1:
-
Delta-like 1 homolog
- NF-κB:
-
Nuclear factor kappa B
- TNF:
-
Tumor necrosis factor
- IL-1:
-
Interleukin-1
- IL-6:
-
Interleukin-6
- IKK:
-
IκB kinase
- SIRT1:
-
Sirtuin 1
- TLR:
-
Toll-like receptors
- RAGE:
-
Advanced glycation end-products
- AMPK:
-
AMP activated protein kinase
- Ulk1:
-
Unc51-like kinase 1
- mTOR:
-
Mammalian target of rapamycin
- STBD1:
-
Starch Binding Domain 1
- GABARAPL1:
-
GABA Type A Receptor Associated Protein Like 1
- GAA:
-
Acid alpha-glucosidase
- FoxO:
-
Fork head box O
- c-FLIP:
-
Cellular fas-associated death domain-like IL-1-converting enzyme inhibitory protein
References
Steven S, Dib M, Hausding M, Kashani F, Oelze M, Kroller-Schon S, Hanf A, Daub S, Roohani S, Gramlich Y, et al. CD40L controls obesity-associated vascular inflammation, oxidative stress, and endothelial dysfunction in high fat diet-treated and db/db mice. Cardiovasc Res. 2018;114(2):312–23.
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17(1):83.
Lind M, Svensson AM, Kosiborod M, Gudbjornsdottir S, Pivodic A, Wedel H, Dahlqvist S, Clements M, Rosengren A. Glycemic control and excess mortality in type 1 diabetes. N Engl J Med. 2014;371(21):1972–82.
Kirkman MS, Mahmud H, Korytkowski MT. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes mellitus. Endocrinol Metab Clin North Am. 2018;47(1):81–96.
Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M, Lafont S, Bergeonneau C, Kassai B, Erpeldinger S, Wright JM, Gueyffier F, Cornu C. Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ. 2011;343: d4169.
Kirwan JP, Sacks J, Nieuwoudt S. The essential role of exercise in the management of type 2 diabetes. Clevel Clin J Med. 2017;84(7 Suppl 1):S15–21.
Gregg EW, Gerzoff RB, Caspersen CJ, Williamson DF, Narayan KM. Relationship of walking to mortality among US adults with diabetes. Arch Intern Med. 2003;163(12):1440–7.
Wang SY, Zhu S, Wu J, Zhang M, Xu Y, Xu W, Cui J, Yu B, Cao W, Liu J. Exercise enhances cardiac function by improving mitochondrial dysfunction and maintaining energy homoeostasis in the development of diabetic cardiomyopathy. J Mol Med. 2020;98(2):245–61.
Nazari A, Chehelcheraghi F. Using Apelin and exercise to protect the cardiac cells: synergic effect in ischemia reperfusion injuries treatment in rats. Bratisl Lek Listy. 2020;121(1):14–21.
Garber AJ, Handelsman Y, Grunberger G, Einhorn D, Abrahamson MJ, Barzilay JI, Blonde L, Bush MA, DeFronzo RA, Garber JR, et al. Consensus statement by the american association of clinical endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm - 2020 Executive Summary. Endocr Pract. 2020;26(1):107–39.
O’Brien J, Hayder H, Zayed Y, Peng C. Overview of MicroRNA biogenesis, mechanisms of actions, and circulation. Front Endocrinol. 2018;9:402.
Kim M, Zhang X. The profiling and role of miRNAs in diabetes mellitus. J Diab Clin Res. 2019;1(1):5–23.
Wang S, Aurora AB, Johnson BA, Qi X, McAnally J, Hill JA, Richardson JA, Bassel-Duby R, Olson EN. The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev Cell. 2008;15(2):261–71.
Dastah S, Tofighi A, Bonab SB. The effect of aerobic exercise on the expression of mir-126 and related target genes in the endothelial tissue of the cardiac muscle of diabetic rats. Microvasc Res. 2021;138: 104212.
Ma C, Wang J, Liu H, Chen Y, Ma X, Chen S, Chen Y, Bihl JI, Yang YI. Moderate exercise enhances endothelial progenitor cell exosomes release and function. Med Sci Sports Exerc. 2018;50(10):2024–32.
Madonna R, Pieragostino D, Balistreri CR, Rossi C, Geng YJ, Del Boccio P, De Caterina R. Diabetic macroangiopathy: Pathogenetic insights and novel therapeutic approaches with focus on high glucose-mediated vascular damage. Vasc Pharmacol. 2018;78:56.
Madonna R, Balistreri CR, Geng YJ, De Caterina R. Diabetic microangiopathy: pathogenetic insights and novel therapeutic approaches. Vascul Pharmacol. 2017;90:1–7.
Hinkel R, Howe A, Renner S, Ng J, Lee S, Klett K, Kaczmarek V, Moretti A, Laugwitz KL, Skroblin P, et al. Diabetes mellitus-induced microvascular destabilization in the Myocardium. J Am Coll Cardiol. 2017;69(2):131–43.
Yuan T, Yang T, Chen H, Fu D, Hu Y, Wang J, Yuan Q, Yu H, Xu W, Xie X. New insights into oxidative stress and inflammation during diabetes mellitus-accelerated atherosclerosis. Redox Biol. 2019;20:247–60.
Erion DM, Shulman GI. Diacylglycerol-mediated insulin resistance. Nat Med. 2010;16(4):400–2.
Olivieri F, Spazzafumo L, Bonafe M, Recchioni R, Prattichizzo F, Marcheselli F, Micolucci L, Mensa E, Giuliani A, Santini G, et al. MiR-21-5p and miR-126a-3p levels in plasma and circulating angiogenic cells: relationship with type 2 diabetes complications. Oncotarget. 2015;6(34):35372–82.
Naderi R, Mohaddes G, Mohammadi M, Alihemmati A, Khamaneh A, Ghyasi R, Ghaznavi R. The effect of garlic and voluntary exercise on cardiac angiogenesis in diabetes: the role of MiR-126 and MiR-210. Arq Bras Cardiol. 2019;112(2):154–62.
Zampetaki A, Kiechl S, Drozdov I, Willeit P, Mayr U, Prokopi M, Mayr A, Weger S, Oberhollenzer F, Bonora E, et al. Plasma microRNA profiling reveals loss of endothelial miR-126 and other microRNAs in type 2 diabetes. Circ Res. 2010;107(6):810–7.
Pordzik J, Eyileten-Postula C, Jakubik D, Czajka P, Nowak A, De Rosa S, Gasecka A, Cieslicka-Kaplon A, Sulikowski P, Filipiak KJ, et al. MiR-126 is an independent predictor of long-term all-cause mortality in patients with type 2 diabetes mellitus. J Clin Med. 2021;10(11):2371.
De Rosa S, Eposito F, Carella C, Strangio A, Ammirati G, Sabatino J, Abbate FG, Iaconetti C, Liguori V, Pergola V, et al. Transcoronary concentration gradients of circulating microRNAs in heart failure. Eur J Heart Fail. 2018;20(6):1000–10.
Al-Kafaji G, Al-Mahroos G, Al-Muhtaresh HA, Skrypnyk C, Sabry MA, Ramadan AR. Decreased expression of circulating microRNA-126 in patients with type 2 diabetic nephropathy: A potential blood-based biomarker. Exp Ther Med. 2016;12(2):815–22.
Lin DC, Lin JB, Chen Z, Chen R, Wan CY, Lin SW, Ruan QS, Li HY, Wu SY. Independent and combined effects of environmental factors and miR-126, miR-143, and miR-145 on the risk of coronary heart disease. J Geriatr Cardiol. 2017;14(11):688–95.
Fish JE, Santoro MM, Morton SU, Yu S, Yeh RF, Wythe JD, Ivey KN, Bruneau BG, Stainier DY, Srivastava D. miR-126 regulates angiogenic signaling and vascular integrity. Dev Cell. 2008;15(2):272–84.
Xi T, Jin F, Zhu Y, Wang J, Tang L, Wang Y, Liebeskind DS, He Z. MicroRNA-126-3p attenuates blood-brain barrier disruption, cerebral edema and neuronal injury following intracerebral hemorrhage by regulating PIK3R2 and Akt. Biochem Biophys Res Commun. 2017;494(1–2):144–51.
Li P, Wei J, Li X, Cheng Y, Chen W, Cui Y, Simoncini T, Gu Z, Yang J, Fu X. 17beta-estradiol enhances vascular endothelial Ets-1/miR-126-3p expression: the possible mechanism for attenuation of atherosclerosis. J Clin Endocrinol Metab. 2017;102(2):594–603.
Ho RC, Hirshman MF, Li Y, Cai D, Farmer JR, Aschenbach WG, Witczak CA, Shoelson SE, Goodyear LJ. Regulation of IkappaB kinase and NF-kappaB in contracting adult rat skeletal muscle. Am J Physiol Cell Physiol. 2005;289(4):C794-801.
Wang Y, Wang F, Wu Y, Zuo L, Zhang S, Zhou Q, Wei W, Wang Y, Zhu H. MicroRNA-126 attenuates palmitate-induced apoptosis by targeting TRAF7 in HUVECs. Mol Cell Biochem. 2015;399(1–2):123–30.
Tang ST, Wang F, Shao M, Wang Y, Zhu HQ. MicroRNA-126 suppresses inflammation in endothelial cells under hyperglycemic condition by targeting HMGB1. Vascul Pharmacol. 2017;88:48–55.
Poissonnier L, Villain G, Soncin F, Mattot V. miR126-5p repression of ALCAM and SetD5 in endothelial cells regulates leucocyte adhesion and transmigration. Cardiovasc Res. 2014;102(3):436–47.
Schober A, Nazari-Jahantigh M, Wei Y, Bidzhekov K, Gremse F, Grommes J, Megens RT, Heyll K, Noels H, Hristov M, et al. MicroRNA-126-5p promotes endothelial proliferation and limits atherosclerosis by suppressing Dlk1. Nat Med. 2014;20(4):368–76.
Zhou J, Li YS, Nguyen P, Wang KC, Weiss A, Kuo YC, Chiu JJ, Shyy JY, Chien S. Regulation of vascular smooth muscle cell turnover by endothelial cell-secreted microRNA-126: role of shear stress. Circ Res. 2013;113(1):40–51.
Baroni MG, D’Andrea MP, Montali A, Pannitteri G, Barilla F, Campagna F, Mazzei E, Lovari S, Seccareccia F, Campa PP, et al. A common mutation of the insulin receptor substrate-1 gene is a risk factor for coronary artery disease. Arterioscler Thromb Vasc Biol. 1999;19(12):2975–80.
Cook SA, Varela-Carver A, Mongillo M, Kleinert C, Khan MT, Leccisotti L, Strickland N, Matsui T, Das S, Rosenzweig A, et al. Abnormal myocardial insulin signalling in type 2 diabetes and left-ventricular dysfunction. Eur Heart J. 2010;31(1):100–11.
Tao H, Wang MM, Zhang M, Zhang SP, Wang CH, Yuan WJ, Sun T, He LJ, Hu QK. MiR-126 Suppresses the Glucose-Stimulated Proliferation via IRS-2 in INS-1 beta Cells. PLoS ONE. 2016;11(2): e0149954.
Suresh Babu S, Thandavarayan RA, Joladarashi D, Jeyabal P, Krishnamurthy S, Bhimaraj A, Youker KA, Krishnamurthy P. MicroRNA-126 overexpression rescues diabetes-induced impairment in efferocytosis of apoptotic cardiomyocytes. Sci Rep. 2016;6:36207.
Wang L, Liu J, Lu K, Qiu Y, Li X, Yue F, Zhang X. Long non-coding RNA NEAT1 regulates endothelial functions in subclinical hypothyroidism through miR-126/TRAF7 pathway. Hum Cell. 2021;34(3):825–35.
Huang CC, Kuo HM, Wu PC, Cheng SH, Chang TT, Chang YC, Kung ML, Wu DC, Chuang JH, Tai MH. Soluble delta-like 1 homolog (DLK1) stimulates angiogenesis through Notch1/Akt/eNOS signaling in endothelial cells. Angiogenesis. 2018;21(2):299–312.
Lyck R, Lecuyer MA, Abadier M, Wyss CB, Matti C, Rosito M, Enzmann G, Zeis T, Michel L, Garcia Martin AB, et al. ALCAM (CD166) is involved in extravasation of monocytes rather than T cells across the blood-brain barrier. J Cerebral Blood Flow Metabolism. 2017;37(8):2894–909.
Iwaguro H, Yamaguchi J, Kalka C, Murasawa S, Masuda H, Hayashi S, Silver M, Li T, Isner JM, Asahara T. Endothelial progenitor cell vascular endothelial growth factor gene transfer for vascular regeneration. Circulation. 2002;105(6):732–8.
Schmidt-Lucke C, Rossig L, Fichtlscherer S, Vasa M, Britten M, Kamper U, Dimmeler S, Zeiher AM. Reduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repair. Circulation. 2005;111(22):2981–7.
Wu K, Yang Y, Zhong Y, Ammar HM, Zhang P, Guo R, Liu H, Cheng C, Koroscil TM, Chen Y, et al. The effects of microvesicles on endothelial progenitor cells are compromised in type 2 diabetic patients via downregulation of the miR-126/VEGFR2 pathway. Am J Physiol Endocrinol Metab. 2016;310(10):E828-837.
Jeong HS, Hong SJ, Cho SA, Kim JH, Cho JY, Lee SH, Joo HJ, Park JH, Yu CW, Lim DS. Comparison of ticagrelor versus prasugrel for inflammation, vascular function, and circulating endothelial progenitor cells in diabetic patients with non-st-segment elevation acute coronary syndrome requiring coronary stenting: a prospective, randomized. Crossover Trial JACC Cardiovasc Interventions. 2017;10(16):1646–58.
Awad O, Jiao C, Ma N, Dunnwald M, Schatteman GC. Obese diabetic mouse environment differentially affects primitive and monocytic endothelial cell progenitors. Stem cells. 2005;23(4):575–83.
Meng S, Cao JT, Zhang B, Zhou Q, Shen CX, Wang CQ. Downregulation of microRNA-126 in endothelial progenitor cells from diabetes patients, impairs their functional properties, via target gene Spred-1. J Mol Cell Cardiol. 2012;53(1):64–72.
Li H, Liu Q, Wang N, Xu Y, Kang L, Ren Y, Zhu G. Transplantation of endothelial progenitor cells overexpressing miR-126-3p improves heart function in ischemic cardiomyopathy. Circ J. 2018;82(9):2332–41.
Pei CZ, Liu B, Li YT, Fang L, Zhang Y, Li YG, Meng S. MicroRNA-126 protects against vascular injury by promoting homing and maintaining stemness of late outgrowth endothelial progenitor cells. Stem Cell Res Ther. 2020;11(1):28.
Meister G, Tuschl T. Mechanisms of gene silencing by double-stranded RNA. Nature. 2004;431(7006):343–9.
Wang W, Zheng Y, Wang M, Yan M, Jiang J, Li Z. Exosomes derived miR-126 attenuates oxidative stress and apoptosis from ischemia and reperfusion injury by targeting ERRFI1. Gene. 2019;690:75–80.
Zhang Y, Xu Y, Zhou K, Kao G, Xiao J. MicroRNA-126 and VEGF enhance the function of endothelial progenitor cells in acute myocardial infarction. Exp Ther Med. 2022;23(2):142.
Abd El-Kader SM, Al-Shreef FM, Al-Jiffri OH. Impact of aerobic exercise versus resisted exercise on endothelial activation markers and inflammatory cytokines among elderly. Afr Health Sci. 2019;19(4):2874–80.
Uhlemann M, Mobius-Winkler S, Fikenzer S, Adam J, Redlich M, Mohlenkamp S, Hilberg T, Schuler GC, Adams V. Circulating microRNA-126 increases after different forms of endurance exercise in healthy adults. Eur J Prev Cardiol. 2014;21(4):484–91.
Sapp RM, Evans WS, Eagan LE, Chesney CA, Zietowski EM, Prior SJ, Ranadive SM, Hagberg JM. The effects of moderate and high-intensity exercise on circulating markers of endothelial integrity and activation in young, healthy men. J Appl Physiol. 2019;127(5):1245–56.
Wahl P, Wehmeier UF, Jansen FJ, Kilian Y, Bloch W, Werner N, Mester J, Hilberg T. Acute effects of different exercise protocols on the circulating vascular microRNAs -16, -21, and -126 in trained subjects. Front Physiol. 2016;7:643.
Kilian Y, Wehmeier UF, Wahl P, Mester J, Hilberg T, Sperlich B. Acute response of circulating vascular regulating MicroRNAs during and after high-intensity and high-volume cycling in children. Front Physiol. 2016;7:92.
Baggish AL, Park J, Min PK, Isaacs S, Parker BA, Thompson PD, Troyanos C, D’Hemecourt P, Dyer S, Thiel M, et al. Rapid upregulation and clearance of distinct circulating microRNAs after prolonged aerobic exercise. J Appl Physiol. 2014;116(5):522–31.
Lutz AH, Blumenthal JB, Landers-Ramos RQ, Prior SJ. Exercise-induced endothelial progenitor cell mobilization is attenuated in impaired glucose tolerance and type 2 diabetes. J Appl Physiol. 2016;121(1):36–41.
Schmitz B, Schelleckes K, Nedele J, Thorwesten L, Klose A, Lenders M, Kruger M, Brand E, Brand SM. Dose-Response of High-Intensity Training (HIT) on Atheroprotective miRNA-126 Levels. Front Physiol. 2017;8:349.
Schmitz B, Niehues H, Lenders M, Thorwesten L, Klose A, Kruger M, Brand E, Brand SM. Effects of high-intensity interval training on microvascular glycocalyx and associated microRNAs. Am J Physiol Heart Circ Physiol. 2019;316(6):H1538–51.
Barber JL, Zellars KN, Barringhaus KG, Bouchard C, Spinale FG, Sarzynski MA. The effects of regular exercise on circulating cardiovascular-related MicroRNAs. Sci Rep. 2019;9(1):7527.
Bittencourt CRO, Izar MCO, Franca CN, Schwerz VL, Povoa R, Fonseca FAH. Effects of chronic exercise on endothelial progenitor cells and microparticles in professional runners. Arq Bras Cardiol. 2017;108(3):212–6.
Ross MD, Wekesa AL, Phelan JP, Harrison M. Resistance exercise increases endothelial progenitor cells and angiogenic factors. Med Sci Sports Exerc. 2014;46(1):16–23.
Ribeiro F, Ribeiro IP, Goncalves AC, Alves AJ, Melo E, Fernandes R, Costa R, Sarmento-Ribeiro AB, Duarte JA, Carreira IM, et al. Effects of resistance exercise on endothelial progenitor cell mobilization in women. Sci Rep. 2017;7(1):17880.
Knox A, Sculthorpe N, Grace F. Caucasian and south Asian men show equivalent improvements in surrogate biomarkers of cardiovascular and metabolic health following 6-weeks of supervised resistance training. Research. 2018;7:1334.
D’Souza RF, Bjornsen T, Zeng N, Aasen KMM, Raastad T, Cameron-Smith D, Mitchell CJ. MicroRNAs in muscle: characterizing the powerlifter phenotype. Front Physiol. 2017;8:383.
Bao F, Slusher AL, Whitehurst M, Huang CJ. Circulating microRNAs are upregulated following acute aerobic exercise in obese individuals. Physiol Behav. 2018;197:15–21.
Morais Junior GS, Souza VC, Machado-Silva W, Henriques AD, Melo Alves A, Barbosa Morais D, Nobrega OT, Brito CJ, Dos Santos Silva RJ. Acute strength training promotes responses in whole blood circulating levels of miR-146a among older adults with type 2 diabetes mellitus. Clin Interv Aging. 2017;12:1443–50.
Lew JK, Pearson JT, Saw E, Tsuchimochi H, Wei M, Ghosh N, Du CK, Zhan DY, Jin M, Umetani K, et al. Exercise Regulates MicroRNAs to preserve coronary and cardiac function in the diabetic heart. Circ Res. 2020;127(11):1384–400.
Silva N, Fernandes T, Soci UP, Monteiro AW, Phillips MI. Swimming training in rats increases cardiac MicroRNA-126 expression and angiogenesis. Med Sci Sports Exer. 2012;44(8):1453–62.
Ghorbanzadeh V, Mohammadi M, Dariushnejad H, Abhari A, Chodari L, Mohaddes G. Cardioprotective effect of crocin combined with voluntary exercise in rat: role of Mir-126 and Mir-210 in Heart Angiogenesis. Arq Bras Cardiol. 2017;109(1):54–62.
Sabzevari Rad R, Shirvani H, Mahmoodzadeh Hosseini H, Shamsoddini A, Samadi M. Micro RNA-126 promoting angiogenesis in diabetic heart by VEGF/Spred-1/Raf-1 pathway: effects of high-intensity interval training. J Diabetes Metab Disord. 2020;19(2):1089–96.
Dariushnejad H, Chodari L, Ghorbanzadeh V. The combination effect of voluntary exercise and crocin on angiogenic miRNAs in high-fat diet/low-dose STZ-induced type2 diabetes in Rats: miR-126 and miR-210. Pharma Sci. 2020;26(4):379–85.
Akbari J, Shirvani H, Shamsoddini A, Bazgir B, Samadi M. Investigation of expression of myocardial miR-126, miR-29a and miR-222 as a potential marker in STZ- induced diabetic rats following interval and continuous exercise training. J Diabetes Metab Disord. 2022;21(1):189–95.
Gomes JL, Fernandes T, Soci UP, Silveira AC, Barretti DL, Negrao CE, Oliveira EM. Obesity downregulates MicroRNA-126 inducing capillary rarefaction in skeletal muscle: effects of aerobic exercise training. Oxid Med Cell Longev. 2017;2017:2415246.
Fernandes T, Magalhaes FC, Roque FR, Phillips MI, Oliveira EM. Exercise training prevents the microvascular rarefaction in hypertension balancing angiogenic and apoptotic factors: role of microRNAs-16, -21, and -126. Hypertension. 2012;59(2):513–20.
Song W, Liang Q, Cai M, Tian Z. HIF-1alpha-induced up-regulation of microRNA-126 contributes to the effectiveness of exercise training on myocardial angiogenesis in myocardial infarction rats. J Cell Mol Med. 2020;24(22):12970–9.
Domanska-Senderowska D, Laguette MN, Jegier A, Cieszczyk P, September AV, Brzezianska-Lasota E. MicroRNA profile and adaptive response to exercise training: a review. Int J Sports Med. 2019;40(4):227–35.
Donghui T, Shuang B, Xulong L, Meng Y, Yujing G, Yujie H, Juan L, Dongsheng Y. Improvement of microvascular endothelial dysfunction induced by exercise and diet is associated with microRNA-126 in obese adolescents. Microvasc Res. 2019;123:86–91.
Harris TA, Yamakuchi M, Kondo M, Oettgen P, Lowenstein CJ. Ets-1 and Ets-2 regulate the expression of microRNA-126 in endothelial cells. Arterioscler Thromb Vasc Biol. 2010;30(10):1990–7.
Oikawa M, Abe M, Kurosawa H, Hida W, Shirato K, Sato Y. Hypoxia induces transcription factor ETS-1 via the activity of hypoxia-inducible factor-1. Biochem Biophys Res Commun. 2001;289(1):39–43.
Costa EC, Hay JL, Kehler DS, Boreskie KF, Arora RC, Umpierre D, Szwajcer A, Duhamel TA. Effects of high-intensity interval training versus moderate-intensity continuous training on blood pressure in adults with pre- to established hypertension: a systematic review and meta-analysis of randomized trials. Sports Med. 2018;48(9):2127–42.
Tyldum GA, Schjerve IE, Tjonna AE, Kirkeby-Garstad I, Stolen TO, Richardson RS, Wisloff U. Endothelial dysfunction induced by post-prandial lipemia: complete protection afforded by high-intensity aerobic interval exercise. J Am Coll Cardiol. 2009;53(2):200–6.
Riedel S, Radzanowski S, Bowen TS, Werner S, Erbs S, Schuler G, Adams V. Exercise training improves high-density lipoprotein-mediated transcription of proangiogenic microRNA in endothelial cells. Eur J Prev Cardiol. 2015;22(7):899–903.
Ho SS, Dhaliwal SS, Hills AP, Pal S. The effect of 12 weeks of aerobic, resistance or combination exercise training on cardiovascular risk factors in the overweight and obese in a randomized trial. BMC Public Health. 2012;12:704.
Braith RW, Stewart KJ. Resistance exercise training: its role in the prevention of cardiovascular disease. Circulation. 2006;113(22):2642–50.
Rodriguez-Miguelez P, Lima-Cabello E, Martinez-Florez S, Almar M, Cuevas MJ, Gonzalez-Gallego J. Hypoxia-inducible factor-1 modulates the expression of vascular endothelial growth factor and endothelial nitric oxide synthase induced by eccentric exercise. J Appl Physiol. 2015;118(8):1075–83.
Terada T, Wilson BJ, Myette-Cote E, Kuzik N, Bell GJ, McCargar LJ, Boule NG. Targeting specific interstitial glycemic parameters with high-intensity interval exercise and fasted-state exercise in type 2 diabetes. Metabolism. 2016;65(5):599–608.
Colberg SR, Hernandez MJ, Shahzad F. Blood glucose responses to type, intensity, duration, and timing of exercise. Diabetes Care. 2013;36(10): e177.
Yaribeygi H, Atkin SL, Simental-Mendia LE, Sahebkar A. Molecular mechanisms by which aerobic exercise induces insulin sensitivity. J Cell Physiol. 2019;234(8):12385–92.
Ribeiro AS, Tomeleri CM, Souza MF, Pina FL, Schoenfeld BJ, Nascimento MA, Venturini D, Barbosa DS, Cyrino ES. Effect of resistance training on C-reactive protein, blood glucose and lipid profile in older women with differing levels of RT experience. Age. 2015;37(6):109.
van Dijk JW, Manders RJ, Tummers K, Bonomi AG, Stehouwer CD, Hartgens F, van Loon LJ. Both resistance- and endurance-type exercise reduce the prevalence of hyperglycaemia in individuals with impaired glucose tolerance and in insulin-treated and non-insulin-treated type 2 diabetic patients. Diabetologia. 2012;55(5):1273–82.
Holten MK, Zacho M, Gaster M, Juel C, Wojtaszewski JF, Dela F. Strength training increases insulin-mediated glucose uptake, GLUT4 content, and insulin signaling in skeletal muscle in patients with type 2 diabetes. Diabetes. 2004;53(2):294–305.
Sharma A, Lacko LA, Argueta LB, Glendinning MD, Stuhlmann H. miR-126 regulates glycogen trophoblast proliferation and DNA methylation in the murine placenta. Dev Biol. 2019;449(1):21–34.
Wu Q, Qi B, Duan X, Ming X, Yan F, He Y, Bu X, Sun S, Zhu H. MicroRNA-126 enhances the biological function of endothelial progenitor cells under oxidative stress via PI3K/Akt/GSK3beta and ERK1/2 signaling pathways. Bosn J Basic Med Sci. 2021;21(1):71–80.
Zhang J, Du YY, Lin YF, Chen YT, Yang L, Wang HJ, Ma D. The cell growth suppressor, mir-126, targets IRS-1. Biochem Biophys Res Commun. 2008;377(1):136–40.
Huisamen B, Lochner A. Exercise modulates myocardial protein kinase B/Akt in Zucker obese rats. Heart. 2005;91(2):227–8.
Christ-Roberts CY, Pratipanawatr T, Pratipanawatr W, Berria R, Belfort R, Kashyap S, Mandarino LJ. Exercise training increases glycogen synthase activity and GLUT4 expression but not insulin signaling in overweight nondiabetic and type 2 diabetic subjects. Metabolism. 2004;53(9):1233–42.
Lajoie C, Calderone A, Trudeau F, Lavoie N, Massicotte G, Gagnon S, Beliveau L. Exercise training attenuated the PKB and GSK-3 dephosphorylation in the myocardium of ZDF rats. J Appl Physiol. 2004;96(5):1606–12.
Shearer J, Ross KD, Hughey CC, Johnsen VL, Hittel DS, Severson DL. Exercise training does not correct abnormal cardiac glycogen accumulation in the db/db mouse model of type 2 diabetes. Am J Physiol Endocrinol Metab. 2011;301(1):E31-39.
Ha J, Guan KL, Kim J. AMPK and autophagy in glucose/glycogen metabolism. Mol Aspects Med. 2015;46:46–62.
Wang Y, Nagase S, Koyama A. Stimulatory effect of IGF-I and VEGF on eNOS message, protein expression, eNOS phosphorylation and nitric oxide production in rat glomeruli, and the involvement of PI3-K signaling pathway. Nitric Oxide Biol Chem. 2004;10(1):25–35.
Sessa R, Seano G, di Blasio L, Gagliardi PA, Isella C, Medico E, Cotelli F, Bussolino F, Primo L. The miR-126 regulates angiopoietin-1 signaling and vessel maturation by targeting p85beta. Biochem Biophys Acta. 2012;1823(10):1925–35.
Mariappan N, Elks CM, Sriramula S, Guggilam A, Liu Z, Borkhsenious O, Francis J. NF-kappaB-induced oxidative stress contributes to mitochondrial and cardiac dysfunction in type II diabetes. Cardiovasc Res. 2010;85(3):473–83.
Qin L, Yao ZQ, Chang Q, Zhao YL, Liu NN, Zhu XS, Liu QQ, Wang LF, Yang AG, Gao CF, et al. Swimming attenuates inflammation, oxidative stress, and apoptosis in a rat model of dextran sulfate sodium-induced chronic colitis. Oncotarget. 2017;8(5):7391–404.
Rada I, Deldicque L, Francaux M, Zbinden-Foncea H. Toll like receptor expression induced by exercise in obesity and metabolic syndrome: A systematic review. Exerc Immunol Rev. 2018;24:60–71.
Pedersen BK. Anti-inflammatory effects of exercise: role in diabetes and cardiovascular disease. Eur J Clin Invest. 2017;47(8):600–11.
Scheffer DDL, Ghisoni K, Aguiar AS Jr, Latini A. Moderate running exercise prevents excessive immune system activation. Physiol Behav. 2019;204:248–55.
Fuller KNZ, Summers CM, Valentine RJ. Effect of a single bout of aerobic exercise on high-fat meal-induced inflammation. Metabolism. 2017;71:144–52.
Dimitrov S, Hulteng E, Hong S. Inflammation and exercise: Inhibition of monocytic intracellular TNF production by acute exercise via beta2-adrenergic activation. Brain Behav Immun. 2017;61:60–8.
Wang X, Peng H, Huang Y, Kong W, Cui Q, Du J, Jin H. Post-translational Modifications of IkappaBalpha: The State of the Art. Front Cell Develop Biol. 2020;8: 574706.
Feng X, Wang H, Ye S, Guan J, Tan W, Cheng S, Wei G, Wu W, Wu F, Zhou Y. Up-regulation of microRNA-126 may contribute to pathogenesis of ulcerative colitis via regulating NF-kappaB inhibitor IkappaBalpha. PLoS ONE. 2012;7(12): e52782.
Hartge MM, Unger T, Kintscher U. The endothelium and vascular inflammation in diabetes. Diab Vasc Dis Res. 2007;4(2):84–8.
Madonna R, Massaro M, De Caterina R. Insulin potentiates cytokine-induced VCAM-1 expression in human endothelial cells. Biochem Biophys Acta. 2008;1782(9):511–6.
Harris TA, Yamakuchi M, Ferlito M, Mendell JT, Lowenstein CJ. MicroRNA-126 regulates endothelial expression of vascular cell adhesion molecule 1. Proc Natl Acad Sci USA. 2008;105(5):1516–21.
Abd El-Kader SM, Al-Jiffri OH. Impact of weight reduction on insulin resistance, adhesive molecules and adipokines dysregulation among obese type 2 diabetic patients. Afr Health Sci. 2018;18(4):873–83.
Togliatto G, Trombetta A, Dentelli P, Gallo S, Rosso A, Cotogni P, Granata R, Falcioni R, Delale T, Ghigo E, et al. Unacylated ghrelin induces oxidative stress resistance in a glucose intolerance and peripheral artery disease mouse model by restoring endothelial cell miR-126 expression. Diabetes. 2015;64(4):1370–82.
Campos JC, Fernandes T, Bechara LR, da Paixao NA, Brum PC, de Oliveira EM, Ferreira JC. Increased clearance of reactive aldehydes and damaged proteins in hypertension-induced compensated cardiac hypertrophy: impact of exercise training. Oxid Med Cell Longev. 2015;2015: 464195.
Newsholme P, Homem De Bittencourt PI, C OH, De Vito G, Murphy C, Krause MS. Exercise and possible molecular mechanisms of protection from vascular disease and diabetes: the central role of ROS and nitric oxide. Clin Sci. 2009, 118(5):341–349.
Li Y, Zhou Q, Pei C, Liu B, Li M, Fang L, Sun Y, Li Y, Meng S. Hyperglycemia and advanced glycation end products regulate miR-126 expression in endothelial progenitor cells. J Vasc Res. 2016;53(1–2):94–104.
Hagiwara S, Iwasaka H, Hasegawa A, Koga H, Noguchi T. Effects of hyperglycemia and insulin therapy on high mobility group box 1 in endotoxin-induced acute lung injury in a rat model. Crit Care Med. 2008;36(8):2407–13.
Goligorsky MS. TLR4 and HMGB1: partners in crime? Kidney Int. 2011;80(5):450–2.
Huang W, Zhao H, Dong H, Wu Y, Yao L, Zou F, Cai S. High-mobility group box 1 impairs airway epithelial barrier function through the activation of the RAGE/ERK pathway. Int J Mol Med. 2016;37(5):1189–98.
Zhang W, Wang Y, Kong Y. Exosomes derived from mesenchymal stem cells modulate miR-126 to ameliorate hyperglycemia-induced retinal inflammation via targeting HMGB1. Invest Ophthalmol Vis Sci. 2019;60(1):294–303.
Giallauria F, Cirillo P, Lucci R, Pacileo M, D’Agostino M, Maietta P, Vitelli A, Chiariello M, Vigorito C. Autonomic dysfunction is associated with high mobility group box-1 levels in patients after acute myocardial infarction. Atherosclerosis. 2010;208(1):280–4.
Shi CC, Pan LY, Peng ZY, Li JG. MiR-126 regulated myocardial autophagy on myocardial infarction. Eur Rev Med Pharmacol Sci. 2020;24(12):6971–9.
Zhang D, Wang W, Sun X, Xu D, Wang C, Zhang Q, Wang H, Luo W, Chen Y, Chen H, et al. AMPK regulates autophagy by phosphorylating BECN1 at threonine 388. Autophagy. 2016;12(9):1447–59.
Munasinghe PE, Riu F, Dixit P, Edamatsu M, Saxena P, Hamer NS, Galvin IF, Bunton RW, Lequeux S, Jones G, et al. Type-2 diabetes increases autophagy in the human heart through promotion of Beclin-1 mediated pathway. Int J Cardiol. 2016;202:13–20.
Russell RC, Tian Y, Yuan H, Park HW, Chang YY, Kim J, Kim H, Neufeld TP, Dillin A, Guan KL. ULK1 induces autophagy by phosphorylating Beclin-1 and activating VPS34 lipid kinase. Nat Cell Biol. 2013;15(7):741–50.
Garza-Lombo C, Schroder A, Reyes-Reyes EM, Franco R. mTOR/AMPK signaling in the brain: Cell metabolism, proteostasis and survival. Current opinion in toxicology. 2018;8:102–10.
Packer M. Autophagy-dependent and -independent modulation of oxidative and organellar stress in the diabetic heart by glucose-lowering drugs. Cardiovasc Diabetol. 2020;19(1):62.
Tomasetti M, Monaco F, Manzella N, Rohlena J, Rohlenova K, Staffolani S, Gaetani S, Ciarapica V, Amati M, Bracci M, et al. MicroRNA-126 induces autophagy by altering cell metabolism in malignant mesothelioma. Oncotarget. 2016;7(24):36338–52.
Jiang S, Wells CD, Roach PJ. Starch-binding domain-containing protein 1 (Stbd1) and glycogen metabolism: Identification of the Atg8 family interacting motif (AIM) in Stbd1 required for interaction with GABARAPL1. Biochem Biophys Res Commun. 2011;413(3):420–5.
Kotoulas OB, Kalamidas SA, Kondomerkos DJ. Glycogen autophagy in glucose homeostasis. Pathol Res Pract. 2006;202(9):631–8.
Mellor KM, Varma U, Stapleton DI, Delbridge LM. Cardiomyocyte glycophagy is regulated by insulin and exposure to high extracellular glucose. Am J Physiol Heart Circ Physiol. 2014;306(8):H1240-1245.
Tal MG. Type 2 diabetes: Microvascular ischemia of pancreatic islets? Med Hypotheses. 2009;73(3):357–8.
Tang X, Zhang L, Wei W. Roles of TRAFs in NF-kappaB signaling pathways mediated by BAFF. Immunol Lett. 2018;196:113–8.
Scudiero I, Zotti T, Ferravante A, Vessichelli M, Reale C, Masone MC, Leonardi A, Vito P, Stilo R. Tumor necrosis factor (TNF) receptor-associated factor 7 is required for TNFalpha-induced Jun NH2-terminal kinase activation and promotes cell death by regulating polyubiquitination and lysosomal degradation of c-FLIP protein. J Biol Chem. 2012;287(8):6053–61.
Xu D, Zhao W, Wang C, Zhu H, He M, Zhu X, Liu W, Wang F, Fan J, Chen C, et al. Up-regulation of TNF Receptor-associated Factor 7 after spinal cord injury in rats may have implication for neuronal apoptosis. Neuropeptides. 2018;71:81–9.
Chen X, Yu X, Li X, Li L, Li F, Guo T, Guan C, Miao L, Cao G. MiR-126 targets IL-17A to enhance proliferation and inhibit apoptosis in high-glucose-induced human retinal endothelial cells. Biochemistry and cell biology = Biochimie et biologie cellulaire. 2020, 98(2):277–283.
Ji ES, Ko IG, Cho JW, Davis RW, Hwang GY, Jee YS, Lim BV. Treadmill exercise inhibits apoptotic neuronal cell death with suppressed vascular endothelial growth factor expression in the retinas of the diabetic rats. J Exer Rehab. 2013;9(3):348–53.
Acknowledgements
Not applicable.
Funding
This work is supported by the National Natural Science Foundation of China (Nos. 81700280; 81970261); Advantageous and Characteristic Disciplines (Groups) of Colleges and Universities in Hubei Province during the 14th Five Year Plan; Research and innovation team project of Wuhan Sports University (No. 21KT04).
Author information
Authors and Affiliations
Contributions
YXM, HL and YW wrote the manuscript; JJX and XG draw the figures, HXD and CLM collected references; YFC and YY developed the concepts and revise the review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, Y., Liu, H., Wang, Y. et al. Roles of physical exercise-induced MiR-126 in cardiovascular health of type 2 diabetes. Diabetol Metab Syndr 14, 169 (2022). https://doi.org/10.1186/s13098-022-00942-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00942-6