Abstract
Background
Irisin has been proposed to have a beneficial influence on the metabolic status of animals and humans. However, the relationship between circulating irisin levels and the risks of metabolic components in humans remains unclear. In the present meta-analysis, we aimed to evaluate the association between circulating irisin and metabolic parameters in nonobese, nondiabetic adults.
Methods
We searched PubMed, Embase, the Cochrane Library, Web of Science and ClinicalTrial.gov using the main search terms and identified original articles published prior to March 7, 2022. Studies that met our inclusion criteria and reported the association between irisin and metabolic parameters were included in our meta-analysis. We used the Newcastle Ottawa scale to assess the quality of the included studies.
Results
A total of 14 studies (711 subjects) in 11 articles were included for qualitative and quantitative synthesis. The pooled results showed that circulating irisin was positively and significantly correlated with fasting blood glucose (r = 0.159), HOMA-IR (r = 0.217) and waist-to-hip ratio (WHR) (r = 0.168). However, no significant association was detected between irisin levels and other metabolic parameters.
Conclusions
Thus, these findings indicated the possible link between irisin levels and part of the metabolic parameters in apparently metabolically normal individuals. However, the regulation of irisin in metabolism in humans remains to be fully elucidated, and well-designed prospective studies will be needed in the future.
Trial registration The review protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO): CRD42022315269.
Similar content being viewed by others
Background
Metabolic syndrome (MetS) is a complex pathophysiologic condition characterized by dysregulated glucose homeostasis, abdominal obesity, dyslipidaemia and increased arterial blood pressure [1, 2], and it increases the risk of cardiovascular diseases, stroke and certain types of tumours [3]. The syndrome results mainly from the imbalance of energy intake and consumption, but it is also determined by genetic or epigenetic makeup of individuals and a sedentary or active lifestyle [1]. It is estimated that over a billion people in the world are now suffering from metabolic syndrome, which has become one of the primary causes of morbidity and mortality in the modern world, resulting in financial burdens to society and families worldwide [1]. However, mild metabolic disorders may already take place before any clinical manifestation emerges and is detected by current metabolic biomarkers. Therefore, novel biomarkers are needed in apparently metabolically healthy populations to identify metabolic abnormalities in the early stage.
Irisin, a hormone first described in 2012 by Boström et al. [4], is a thermogenic myokine cleaved from fibronectin type III domain containing protein 5 (FNDC5), which is mainly released by muscle and adipose tissue and secreted upon physical activity [3] and cold exposure [5]. Irisin has been proposed to have a beneficial influence on the metabolic status of animals and humans, especially in inhibiting the accumulation of fat and obesity because it promotes the browning of white adipose tissue [3, 6]. Since the identification of irisin, a hypothesis has been proposed that a beneficial role of exercise in metabolic diseases may be related to irisin, suggesting that it has a potential role in the diagnosis and treatment of metabolic diseases, such as diabetes mellitus and obesity [7, 8]. However, before further exploring the application of exogenous irisin, the rational next step is to clarify the link between endogenous irisin and metabolic parameters as well as the underlying pathophysiological mechanism.
However, the relationship between circulating irisin levels and the risks of metabolic components in humans remains unclear. A cross-sectional study has evaluated the relation of irisin to MetS components in 151 participants and observed positive associations between irisin and various metabolic parameters [9]. Regarding the association between irisin and anthropometric parameters, most evidence shows a positive association between irisin levels and indices of adiposity, including body mass index (BMI), waist circumference, waist-to-hip ratio (WHR) and fat mass [9,10,11,12,13,14,15]. However, several studies have not detected any association [16] or reported a negative correlation of irisin with fat mass, BMI and WHR [17]. In patients with type 2 diabetes mellitus and prediabetes, most studies have observed lower circulating irisin levels than controls [17,18,19,20], suggesting a downregulated level of irisin under the conditions of impaired glucose tolerance [6]. In contrast, evidence from studies in nondiabetic populations has shown that irisin levels are positively correlated with fasting blood glucose [10, 19, 21], beta cell function [22] and insulin resistance [23]. Similarly, insulin sensitivity has been reported to be negatively associated with irisin [23, 24], except for one study reporting a positive association in a Caucasian population [17]. Regarding lipid metabolism, studies have suggested that the expression of FNDC5 or the administration of irisin promotes lipolysis and inhibits the synthesis of lipids [25,26,27]. However, data from human research are inconsistent. On the one hand, a positive correlation between irisin levels and an unfavourable lipid profile, such as triglycerides (TGs) [9, 28], total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and fasting fatty acids [29, 30], has been reported. Additionally, irisin has been reported to be negatively associated with high-density lipoprotein cholesterol (HDL-C) in patients at high cardiometabolic risk [9, 31]. On the other hand, irisin has been suggested to be inversely associated with total, LDL cholesterol and triglycerides in a Central European general population [32]. However, in several studies, no association of irisin with lipid indices has been reported in healthy and young individuals [33], normal-weight individuals with increased body fat [34] and male subjects with mild hypercholesterolemia [35]. Animal experiments have provided evidence that irisin administration lowers blood pressure [36, 37]. However, few studies have been conducted to investigate the association between irisin levels and blood pressure in humans. Positive correlations have been found between irisin levels and blood pressure in obstructive sleep apnoea patients [38]. Similarly, a study including 24 obese and 63 normal-weight children has found that irisin levels are positively correlated with systolic and diastolic blood pressure [39]. However, a significant relationship between irisin and 24-h blood pressure has not been reported in studies including young hypertensive adults [40].
The inconsistent findings observed across the studies indicate the complexity of the relationship between circulating irisin levels and metabolic components. However, the wide range of BMI and different degrees of glucose homeostasis of subjects across the studies may be sources of clinical heterogeneity. To reduce the influence of obesity or abnormal glucose tolerance on irisin levels, we performed a meta-analysis to evaluate the association between circulating irisin levels and metabolic parameters in nonobese, nondiabetic adults. Thus, the results will be more reasonable in the absence of these two major metabolic components. It should be noted that we did not exclude patients with other metabolic disorders, such as overweight, NAFLD, PCOS or dyslipidaemia.To the best of our knowledge, no systematic review or meta-analysis has been performed on this basis. Thus, the present study provided evidence supporting irisin as a potential biomarker of the risk of metabolic disorders in this population to some extent.
Material and methods
Study protocol
The present study was conducted according to the Meta-analysis of Observational Studies in Epidemiology (MOOSE) standards [41]. The review protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO): CRD42022315269.
Data sources and search strategy
A systematic literature search of electronic databases, including PubMed, Embase, the Cochrane Library, Web of Science and ClinicalTrial.gov, was conducted by two authors independently using the main search terms and database-specific terms related to “irisin”, “metabolic parameters” and “clinical trials” (see detailed search strategy in Additional file 1). Original articles published prior to March 7, 2022 were identified. The reference lists of relevant reviews and conference abstracts were also screened for potential studies.
Study selection
The titles and abstracts of articles were screened for potentially eligible studies. The full texts of all eligible articles were then obtained and reviewed by two authors independently to ensure that the articles met the inclusion criteria of the review. Any disagreements about the study selection were resolved by consensus. Studies meeting the following criteria were included: (a) enrolled nonobese, nondiabetic adult subjects; (b) reported the relation of circulating irisin to at least one metabolic parameter, including fasting blood glucose (FBG), homeostasis model assessment-insulin resistance (HOMA-IR), insulin levels, BMI, waist circumference (WC), WHR, TG, TC, LDL-C, HDL-C, systolic blood pressure (SBP) or diastolic blood pressure (DBP), at baseline using Spearman correlation analysis, Pearson correlation analysis or simple linear regression analysis; and (c) designed as a cross-sectional, cohort or case–control study. Studies involving healthy control groups were only included when a BMI less than 30 kg/m2 (according to the definition of WHO [42]) could be deduced from the baseline data in the article or was confirmed by the corresponding author, thus overweight participants(25 ≤ BMI < 30 kg/ m2) were not excluded from our study. Studies that enrolled patients with impaired glucose regulation or obesity without excluding them from the entire study population when calculating the correlation coefficients were excluded. However, we did not exclude patients with other metabolic disorders. Pregnant women were also excluded considering the complicated and heterogeneous changes during the gestational period.
Data extraction and quality assessment
Data extraction was conducted independently by two reviewers (L.Y. and X.Z.) using a predesigned standardized data extraction form, which included the first author, year of publication, study location, type of study, sample size, characteristics of participants (sex ratio, age range, BMI range and health status), blood sample, ELISA kits for irisin measurement, analysis methods and correlation or regression coefficients. The corresponding authors of the articles were contacted by email, if necessary, for unpublished information. The methodological quality of each study was assessed according to the Newcastle–Ottawa Scale (NOS) [43], which contains eight items classified into three aspects (selection, comparability and outcome or exposure) [43]. The range of NOS was 0–9 stars, and a study was defined as high-quality when it achieved 7 or more stars. Two researchers (L.Y. and X.Z.) independently assessed the quality of the studies. Any disagreements in any phase were settled through discussion.
Data analysis
For studies with interventions, only the baseline correlation coefficient was included in the meta-analysis. For studies with more than one eligible group, only the collective correlation coefficients (if provided) were used in our analysis. For studies using Spearman’s method to calculate the correlation coefficients, the correlation coefficients (rs) were converted into approximate Pearson correlation coefficients (r) prior to inclusion in the meta-analysis, considering the significant difference between the two methods [44]. For studies that used simple linear regression to calculate the correlation coefficients, the results were directly applied in the analysis. Fisher's z transformation of correlation coefficients, the variance of z and standard error were calculated using the following formulas before obtaining the summary effect size (r) [45]:
All metabolic parameters assessed were considered as continuous variables. The pooled effect estimates were calculated using a random-effect model. The inverse variance method was applied to estimate the weight of each study. Statistical heterogeneity was tested using the chi-squared test, and I2 with a value greater than 50% indicated substantial heterogeneity across studies. Additionally, sensitivity analyses were performed to assess the robustness of the results using the leave-one-out method. Furthermore, subgroup meta-analyses were conducted to explore the heterogeneity and to evaluate the impact of specific factors on the outcome estimates. Publication bias was assessed with funnel plot analysis and Egger's regression asymmetry test. All statistical analyses were performed using RevMan 5.3.5 (The Nordic Cochrane Centre, the Cochrane Collaboration, 2014) or Stata Software 16.0 (College Station, TX, 77845, USA).
Results
Search results
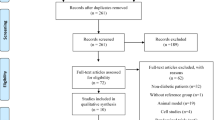
A total of 953 studies were identified through database searching. After the removal of duplicates, 794 unique records were screened by reading the titles and abstracts. The full texts of 264 articles were then retrieved for detailed assessment. Studies with ineligible study subjects or that did not report the outcome of interest were excluded. Studies were also excluded when they enrolled diabetic or obese subjects without excluding them from the entire population when calculating the correlation coefficients. Studies using multivariate linear regression to calculate the correlation between irisin and metabolic parameters were also excluded, considering the complexity of various confounders and models in different studies. The corresponding authors of articles in which data were inadequate for our meta-analysis were contacted by email. Overall, 14 studies in 11 articles were included for qualitative and quantitative synthesis. The detailed process of study selection is illustrated in Fig. 1.
Study characteristics
The characteristics of the included studies are summarized in Table 1. The selected studies were published between 2013 and 2022 with five cross-sectional studies and nine case–control studies. Regarding the location of the studies, four studies were conducted in Europe, five studies were conducted in Asia, four studies were conducted in Africa and one study was conducted in Australia. The sample sizes ranged from 26 to 122 with a median of 45. Of the 711 participants in the included articles, 410 (57.7%) were females. Two studies recruited only male subjects, and 6 studies recruited only female subjects. Most studies (n = 8) recruited healthy subjects or included healthy control groups, except for one study involving nonalcoholic fatty liver disease patients, three studies involving polycystic ovary syndrome (PCOS) patients, one study including mild hypercholesterolemia and one study including normal weight individuals with increased body fat (> 30%). Nine studies used serum blood samples of irisin, and five studies used plasma irisin. For the ELISA kits used to measure circulating irisin levels, three studies used Phoenix Pharmaceuticals, six studies used BioVendor and five studies used other kits. Some studies strictly controlled for potential confounders, such as physical activity [33, 46, 47] and daily energy or macronutrient intake of subjects [33, 46, 47] before examination, considering the impact of recent lifestyle on the measurement of circulating irisin concentrations. One study considered cold exposure and controlled room temperature during the examination period [46].
The association between irisin levels and at least one of the metabolic parameters was evaluated in 13 studies for glycaemic parameters and insulin resistance as well as in 11 studies for lipid metabolism parameters and anthropometric measurements. The statistical analyses to measure the correlation coefficients between irisin levels and metabolic parameters included Spearman correlation analysis in five studies, Pearson correlation analysis in six studies and simple linear regression in one study, and two studies did not state a specific method. Almost all studies reported unadjusted results, except for two studies, which provided adjusted data as well. The range of quality scores was from 6 to 8 with a median score of 8 for case–control studies and a median score of 7 for cross-sectional studies.
Quality assessment
Figure 2 illustrates the proportion of included articles that reported each of the NOS items. The majority of the included studies (n = 8) scored as of good quality (7–8 stars). The detailed quality assessment for each study is shown in Additional file 2.
Association between irisin and metabolic parameters
Glucose metabolism, insulin levels and insulin resistance
Of 14 studies calculating the correlation coefficient of circulating irisin with metabolic parameters, 13 studies reported the results of fasting blood glucose. Fisher's z transformation of correlation coefficients was calculated and imputed in the meta-analysis. The results (Fig. 3 and Table 2) showed that circulating irisin was positively and significantly correlated with fasting blood glucose (summary r = 0.159, 95% CI 0.060–0.254, p < 0.05). Moreover, sensitivity analysis suggested that the result was robust. The heterogeneity test demonstrated I2 = 32% (p > 0.05), indicating no significant heterogeneity among studies. The subgroup analyses by study design, blood sample, ELISA kits, male-to-female ratio, study location, metabolic status, study quality and whether overweight subjects were included in the study are shown in Additional file 3.
Insulin levels and HOMA-IR were evaluated in 11 and 10 studies, respectively. The random-effect meta-analysis did not show a significant association between irisin and insulin levels (summary r = 0.110, 95% CI −0.080 to 0.291, p > 0.05). However, subgroup analysis by metabolic status showed that irisin was significantly correlated with insulin levels in metabolic disorder subjects (summary r = 0.327, 95% CI 0.149–0.485, p < 0.05). In contrast, a significant positive association was observed between irisin and HOMA-IR (summary r = 0.217, 95% CI 0.01–0.414, p < 0.05). Similar to insulin levels, the result only remained significant in metabolic disorder subjects (summary r = 0.438, 95% CI 0.149–0.653, p < 0.05) when the subgroup analysis was conducted (shown in Additional file 4).
Anthropometric measurement
The association between irisin levels and anthropometric measurements is shown in Fig. 4 and Table 2. Eleven studies, 4 and 6 studies reported the results of BMI, WC and WHR, respectively. The random-effect meta-analysis did not show a significant association between irisin levels and BMI (summary r = 0.149, 95% CI −0.00 to 0.300, p = 0.05) with a medium-to-high level of heterogeneity across the included studies (I2 = 70%, p˂0.05). Subgroup analyses were also conducted to determine the correlation between irisin and BMI. The results showed that study design, ELISA kits, sex, study location and metabolic status were sources of heterogeneity as shown in Additional file 5. In addition, irisin levels were significantly and positively associated with BMI in the studies that included metabolically healthy individuals (summary r = 0.139; 95% CI 0.01–0.273), studies that included more female subjects (summary r = 0.282; 95% CI 0.060–0.470) and studies designed as case–control studies (summary r = 0.235; 95% CI 0.01–0.430) (shown in Additional file 5). In contrast, the pooled results showed that circulating irisin levels were significantly and positively associated with WHR (summary r = 0.168, 95% CI 0.020–0.310, p < 0.05). However, no significant correlation was detected between circulating irisin and WC (summary r = 0.020, 95% CI −0.129 to 0.178, p > 0.05). The heterogeneity was not significant in studies including the outcomes of WC and WHR.
Lipid profile
The association between circulating irisin levels and lipid profiles was evaluated in 11 studies. Of note, 11 studies reported the outcome of TC, HDL-C and TG, and 9 studies reported the outcome of LDL-C. Overall, no significant correlation was found between irisin levels and TC (summary r = 0.030, 95% CI −0.100 to 0.149, p > 0.05), HDL-C (summary r = 0.020, 95% CI −0.100 to 0.139, p > 0.05), LDL-C (summary r = 0.070, 95% CI: −0.070 to 0.188, p > 0.05) or TG (summary r = 0.070, 95% CI −0.080 to 0.207, p > 0.05). In addition, there was a moderate-to-high level of statistical heterogeneity across studies for each outcome with I2 ranging from 50 to 70% (P < 0.05) (data are shown in Fig. 5 and Table 2).
Publication bias
Funnel plots of included studies were presented in Additional file 6. (Due to the small number of studies included in several outcomes, the funnel plots were only performed in the outcomes of FBG, HOMA-IR, BMI, insulin, TC, HDL-C, and TG), and no significant publication bias was observed through visual evaluation of funnel plots. Egger’s test was also conducted, and the results were p = 0.1199 for FBG, p = 0.4201 for insulin, p = 0.9729 for HOMA-IR, p = 0.8866 for BMI, p = 0.4421 for TC, p = 0.3704 for HDL-C and p = 0.6461 for TG, demonstrating no evidence of publication bias in these metabolic parameters.
Discussion
Main findings
In the present study, we conducted a meta-analysis of 711 subjects in 14 studies to evaluate the association between irisin levels and metabolic parameters in nondiabetic, nonobese adults. We found that irisin levels were positively correlated with fasting blood glucose, HOMA-IR and WHR in this population. However, no significant association was detected between irisin levels and other metabolic parameters. To the best of our knowledge, this is the first meta-analysis to systematically evaluate the correlation between circulating irisin levels and metabolic parameters in a population without obesity or impaired glucose tolerance. Our findings provide a clue to understand the relationship between irisin and metabolic components in people with relatively normal metabolism.
Interpretation
Glycaemic indices
Previous studies have indicated potential beneficial effects of irisin on glucose homeostasis and insulin resistance. However, human studies published to date [10, 14, 17, 19] have reported inconsistent results on the association between circulating irisin levels and glucose levels, insulin levels and insulin resistance in diabetic subjects. In contrast, in nondiabetic subjects, most studies have indicated that blood glucose is positively associated with irisin levels [10, 19, 21]. In the present meta-analysis, a significant positive correlation was also observed between irisin levels and fasting blood glucose when pooled across studies, and the estimate was robust across sensitivity analyses. Although the demonstrated correlation was relatively modest, our finding was in line with results from the literature. In addition, subgroup analyses indicated that the association between irisin levels and fasting blood glucose was likely to be influenced by the male-to-female ratio of the subjects, the method of irisin measurement, the study location and the NOS score of the study. Of note, irisin remained significantly associated with FBG only in studies that included overweight participants, whereas the correlation was not significant in studies that enrolled only normal weight subjects (BMI < 25 kg/m2), indicating the nonnegligible role of adiposity in the impact on circulating irisin levels, which may result from increased secretion from adiposity or resistance of irisin [9].
Insulin levels and insulin resistance
Studies have reported that irisin overexpression in mice fed a high-fat diet results in improved insulin sensitivity and glucose tolerance [17]. In humans, a cross-sectional study including 254 individuals with normal glucose tolerance has been conducted and found that irisin is positively correlated with circulating insulin levels and the homeostasis model assessment (HOMA)-β, even after adjustment for anthropometric and metabolic confounders [22]. A recent meta-analysis has revealed a significantly positive association between circulating irisin levels and insulin resistance in subjects with normal glucose tolerance [23]. In the present study, the pooled results did not show a significant association between circulating irisin and insulin levels. However, subgroup analysis by metabolic status demonstrated a significant and positive correlation between circulating irisin and insulin levels in studies that included patients with metabolic disorders (including three studies that enrolled PCOS patients, 1 study that enrolled NAFLD patients, one study that included individuals with mild hypercholesterolemia and one study that included people with BF% > 30). However, the results of studies enrolling metabolically healthy participants remained insignificant. In contrast, HOMA-IR was found to be significantly correlated with irisin levels, but subgroup analysis revealed a positive and significant correlation only in the metabolic disorder subgroup. These two outcomes combined indicated that insulin resistance and insulin levels are positively correlated with circulating levels of irisin under the condition of metabolic disorders but that the correlation is not obvious in metabolic healthy individuals. These findings were consistent with several studies, suggesting elevated circulating irisin levels in PCOS, metabolic syndrome, prediabetes and obese individuals in comparison with healthy controls [9, 11, 48, 49]. The increased secretion of irisin levels observed in metabolically abnormal individuals can be explained by increased adipose or muscle tissue in populations with metabolic disorders. Another possible explanation for the higher circulating irisin in metabolically abnormal patients is “irisin resistance”, a compensatory increase in circulating hormone levels to overcome resistance, similar to insulin resistance or leptin resistance [9, 50].
Anthropometric measurement
Numerous animal experiments and human research studies have focused on the potential association between irisin levels and obesity. Most studies have revealed a positive correlation of circulating irisin levels with BMI, weight, waist circumference waist-to-hip ratio and fat mass [9,10,11,12,13,14,15]. Furthermore, weight loss due to bariatric surgery lowers circulating irisin levels, which are restored after regaining the lost weight [11, 15], indicating the apparent link between adiposity and irisin. In contrast, one study including both normal-weight and overweight males did not detect any association between irisin and BMI [16]. Another study involving morbidly obese individuals has reported a negative association between irisin and BMI [17]. The contradictory results may be due to differences in health status and anthropometric parameters, especially the different degrees of obesity of the populations in these studies. It is well recognized that in healthy and normal weight populations, irisin in blood is mainly secreted by muscle cells, however, in obese individuals, the amount of irisin produced by adipose tissue is higher due to the increased amount of fat mass [15, 51], and it is plausible that the different amount of fat mass is a source of clinical heterogeneity in regard to the production of circulating irisin. Our results did not reveal a significant correlation between irisin and BMI in nondiabetic, nonobese subjects. Interestingly, subgroup analysis by male-to-female ratio revealed that the BMI of studies that included more female than male subjects was significantly associated with irisin, while studies with a male-to-female ratio > 1 showed a negative but insignificant correlation, suggesting a gender dimorphism of irisin in its relation to BMI. The results were confirmed by further subgroup analysis based on studies that included only male subjects and only female subjects. The sex difference in irisin has been explored in multiple studies [47, 52]. Females are suggested to have a higher irisin level than males after adjusting for potential confounders [33]. Similarly, another study has reported higher levels of irisin in healthy girls than in boys [52], suggesting sex differences in circulating irisin. A previously published study conducted in male and female subjects has reported sex discrepancies in the correlation of irisin with metabolic indices [47], and the author explained that the inconsistent results between males and females may be attributed to the different body compositions, such as fat distribution [53, 54], skeletal muscle mass and hormonal differences [10].
The pooled results also demonstrated a significant positive association between irisin and WHR as expected with robust results after conducting sensitivity analysis and low heterogeneity across studies. In contrast, no significant correlation was observed between irisin and WC, which may be due to insufficient studies included in regard to this outcome.
Lipid profile
Many studies have investigated the association between circulating irisin levels and lipid profiles with inconsistent findings. Animal experiments have suggested that the expression of FNDC5 or the administration of irisin promotes lipolysis and inhibits the synthesis of lipids [25,26,27]. In human studies, positive correlations between irisin levels and an unfavourable lipid profile have been reported [9, 28,29,30]. In contrast, a study that investigated obese subjects with nonalcoholic fatty liver disease (NAFLD) has suggested that lower blood triglycerides and transaminases are associated with a higher level of irisin [55], suggesting a favourable role of irisin in lipogenesis. Similarly, Anastasios et al. [46] found a negative and significant correlation between plasma irisin and fasting triglycerides, even after adjusting for potential confounders. However, in other studies, no significant association between irisin levels and lipid parameters has been observed [33,34,35]. In the present analysis, the lipid profile was evaluated in terms of the association with circulating irisin levels. The pooled results indicated that TC, HDL-C and LDL-C were not significantly correlated with irisin levels in the nondiabetic, nonobese population. The results remained largely unchanged after sensitivity analysis and subgroup analyses by study design, NOS score, ELISA kits, male-to-female ratio, metabolic status, study location, the method of irisin measurement and sample size of the studies. Notably, we did not observe a significant association between irisin and TG; however, by conducting subgroup analyses by study location, the direction of the correlation did not change but became significant and positive in studies conducted in Asia, indicating the possible impact of ethnicity on the correlation between irisin and TG.
Limitation
The present study had several limitations. First, because we limited the population of our study to nonobese, nondiabetic subjects, the number of eligible studies with several results of interest was inadequate. Blood pressure, an important component of metabolic syndrome, was not included in the outcome due to the relatively small number of studies eligible for our meta-analysis. In addition, lifestyle, energy intake of participants and medication history were not considered for further subgroup analysis due to the limited number of studies included. Therefore, these factors that may affect the results need to be further clarified in future research. Second, although we excluded obese and diabetic populations from our meta-analysis, we did not exclude patients with other metabolic disorders, such as overweight, NAFLD, PCOS or dyslipidaemia. According to the literature, these disorders may also have some complex interactions with circulating irisin. However, we performed a subgroup analysis by metabolic status to analyse the clinical heterogeneity. Third, not all studies mentioned strict control of the diet and exercise of the participants. However, physical activity, especially the intensity and duration of the exercise or the type of training, can cause significant differences in irisin levels. Moreover, some results showed substantial heterogeneity across studies. Although we conducted a sensitivity analysis and subgroup analyses to explore the sources of heterogeneity, some remained unexplained, and meta-regression analysis was limited due to the insufficient number of studies included. Last, although several metabolic indices were found to be significantly associated with irisin levels, both the pooled results and individual studies showed a relatively modest correlation, suggesting that our results should be interpretated with caution.
Conclusions
Our findings showed positive associations between irisin levels and several metabolic parameters in a relatively metabolically normal population. If irisin represents the link between the favourable influence of physical activity and improvement in metabolic status as well as if a clear association between irisin and certain metabolic diseases is confirmed by future studies, irisin may be a biomarker and therapeutic candidate in the treatment of these diseases. However, the regulation of irisin in humans and the role of irisin in glucose metabolism remain to be fully elucidated, and well-designed prospective studies are required. Additionally, the gender dimorphism of irisin observed in the present study indicated a need to investigate the association between irisin and metabolic syndrome based on different genders in future studies.
Availability of data and materials
Data are available from the authors upon reasonable request.
References
Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20(2):12. https://doi.org/10.1007/s11906-018-0812-z.
Kassi E, Pervanidou P, Kaltsas G, Chrousos G. Metabolic syndrome: definitions and controversies. BMC Med. 2011;9:48. https://doi.org/10.1186/1741-7015-9-48.
Arhire LI, Mihalache L, Covasa M. Irisin: a hope in understanding and managing obesity and metabolic syndrome. Front Endocrinol (Lausanne). 2019;10:524. https://doi.org/10.3389/fendo.2019.00524.
Boström P, Wu J, Jedrychowski MP, et al. A PGC1-α-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012;481(7382):463–8. https://doi.org/10.1038/nature10777.
Lee P, Linderman JD, Smith S, et al. Irisin and FGF21 are cold-induced endocrine activators of brown fat function in humans. Cell Metab. 2014;19(2):302–9. https://doi.org/10.1016/j.cmet.2013.12.017.
Hofmann T, Elbelt U, Stengel A. Irisin as a muscle-derived hormone stimulating thermogenesis–a critical update. Peptides. 2014;54:89–100. https://doi.org/10.1016/j.peptides.2014.01.016.
Castillo-Quan JI. From white to brown fat through the PGC-1α-dependent myokine irisin: implications for diabetes and obesity. Dis Model Mech. 2012;5(3):293–5. https://doi.org/10.1242/dmm.009894.
Polyzos SA, Kountouras J, Shields K, Mantzoros CS. Irisin: a renaissance in metabolism? Metabolism. 2013;62(8):1037–44. https://doi.org/10.1016/j.metabol.2013.04.008.
Park KH, Zaichenko L, Brinkoetter M, et al. Circulating irisin in relation to insulin resistance and the metabolic syndrome [published correction appears in J Clin Endocrinol Metab. 2014 May;99(5):1910]. J Clin Endocrinol Metab. 2013;98(12):4899–907. https://doi.org/10.1210/jc.2013-2373.
Huh JY, Panagiotou G, Mougios V, et al. FNDC5 and irisin in humans: I. Predictors of circulating concentrations in serum and plasma and II. mRNA expression and circulating concentrations in response to weight loss and exercise. Metabolism. 2012;61(12):1725–38. https://doi.org/10.1016/j.metabol.2012.09.002.
Crujeiras AB, Pardo M, Arturo RR, et al. Longitudinal variation of circulating irisin after an energy restriction-induced weight loss and following weight regain in obese men and women. Am J Hum Biol. 2014;26(2):198–207. https://doi.org/10.1002/ajhb.22493.
Gutierrez-Repiso C, Garcia-Serrano S, Rodriguez-Pacheco F, et al. FNDC5 could be regulated by leptin in adipose tissue. Eur J Clin Invest. 2014;44(10):918–25. https://doi.org/10.1111/eci.12324.
Löffler D, Müller U, Scheuermann K, et al. Serum irisin levels are regulated by acute strenuous exercise. J Clin Endocrinol Metab. 2015;100(4):1289–99. https://doi.org/10.1210/jc.2014-2932.
Stengel A, Hofmann T, Goebel-Stengel M, Elbelt U, Kobelt P, Klapp BF. Circulating levels of irisin in patients with anorexia nervosa and different stages of obesity–correlation with body mass index. Peptides. 2013;39:125–30. https://doi.org/10.1016/j.peptides.2012.11.014.
Crujeiras AB, Zulet MA, Lopez-Legarrea P, et al. Association between circulating irisin levels and the promotion of insulin resistance during the weight maintenance period after a dietary weight-lowering program in obese patients. Metabolism. 2014;63(4):520–31. https://doi.org/10.1016/j.metabol.2013.12.007.
Pekkala S, Wiklund PK, Hulmi JJ, et al. Are skeletal muscle FNDC5 gene expression and irisin release regulated by exercise and related to health? J Physiol. 2013;591(21):5393–400. https://doi.org/10.1113/jphysiol.2013.263707.
Moreno-Navarrete JM, Ortega F, Serrano M, et al. Irisin is expressed and produced by human muscle and adipose tissue in association with obesity and insulin resistance. J Clin Endocrinol Metab. 2013;98(4):E769–78. https://doi.org/10.1210/jc.2012-2749.
Choi YK, Kim MK, Bae KH, et al. Serum irisin levels in new-onset type 2 diabetes. Diabetes Res Clin Pract. 2013;100(1):96–101. https://doi.org/10.1016/j.diabres.2013.01.007.
Liu JJ, Wong MD, Toy WC, et al. Lower circulating irisin is associated with type 2 diabetes mellitus. J Diabetes Complicat. 2013;27(4):365–9. https://doi.org/10.1016/j.jdiacomp.2013.03.002.
Duran ID, Gülçelik NE, Ünal M, et al. Irisin levels in the progression of diabetes in sedentary women. Clin Biochem. 2015;48(18):1268–72. https://doi.org/10.1016/j.clinbiochem.2015.07.098.
Huerta AE, Prieto-Hontoria PL, Fernández-Galilea M, et al. Circulating irisin and glucose metabolism in overweight/obese women: effects of α-lipoic acid and eicosapentaenoic acid. J Physiol Biochem. 2015;71(3):547–58. https://doi.org/10.1007/s13105-015-0400-5.
Yang M, Chen P, Jin H, et al. Circulating levels of irisin in middle-aged first-degree relatives of type 2 diabetes mellitus - correlation with pancreatic β-cell function. Diabetol Metab Syndr. 2014;6(1):133. https://doi.org/10.1186/1758-5996-6-133.
Qiu S, Cai X, Yin H, et al. Association between circulating irisin and insulin resistance in non-diabetic adults: a meta-analysis. Metabolism. 2016;65(6):825–34. https://doi.org/10.1016/j.metabol.2016.02.006.
Sesti G, Andreozzi F, Fiorentino TV, et al. High circulating irisin levels are associated with insulin resistance and vascular atherosclerosis in a cohort of nondiabetic adult subjects. Acta Diabetol. 2014;51(5):705–13. https://doi.org/10.1007/s00592-014-0576-0.
Gao S, Li F, Li H, Huang Y, Liu Y, Chen Y. Effects and molecular mechanism of GST-irisin on lipolysis and autocrine function in 3T3-L1 adipocytes. PLoS ONE. 2016;11(1):e0147480. https://doi.org/10.1371/journal.pone.0147480.
Xiong XQ, Chen D, Sun HJ, et al. FNDC5 overexpression and irisin ameliorate glucose/lipid metabolic derangements and enhance lipolysis in obesity. Biochim Biophys Acta. 2015;1852(9):1867–75. https://doi.org/10.1016/j.bbadis.2015.06.017.
Huh JY, Dincer F, Mesfum E, Mantzoros CS. Irisin stimulates muscle growth-related genes and regulates adipocyte differentiation and metabolism in humans. Int J Obes (Lond). 2014;38(12):1538–44. https://doi.org/10.1038/ijo.2014.42.
Moreno M, Moreno-Navarrete JM, Serrano M, et al. Circulating irisin levels are positively associated with metabolic risk factors in sedentary subjects. PLoS ONE. 2015;10(4):e0124100. https://doi.org/10.1371/journal.pone.0124100.
Tang S, Zhang R, Jiang F, et al. Circulating irisin levels are associated with lipid and uric acid metabolism in a Chinese population. Clin Exp Pharmacol Physiol. 2015;42(9):896–901. https://doi.org/10.1111/1440-1681.12439.
Jang HB, Kim HJ, Kang JH, Park SI, Park KH, Lee HJ. Association of circulating irisin levels with metabolic and metabolite profiles of Korean adolescents. Metabolism. 2017;73:100–8. https://doi.org/10.1016/j.metabol.2017.05.007.
Panagiotou G, Mu L, Na B, Mukamal KJ, Mantzoros CS. Circulating irisin, omentin-1, and lipoprotein subparticles in adults at higher cardiovascular risk. Metabolism. 2014;63(10):1265–71. https://doi.org/10.1016/j.metabol.2014.06.001.
Oelmann S, Nauck M, Völzke H, Bahls M, Friedrich N. Circulating irisin concentrations are associated with a favourable lipid profile in the general population. PLoS ONE. 2016;11(4):e0154319. https://doi.org/10.1371/journal.pone.0154319.
Anastasilakis AD, Polyzos SA, Saridakis ZG, et al. Circulating irisin in healthy, young individuals: day-night rhythm, effects of food intake and exercise, and associations with gender, physical activity, diet, and body composition. J Clin Endocrinol Metab. 2014;99(9):3247–55. https://doi.org/10.1210/jc.2014-1367.
Mehrabian S, Taheri E, Karkhaneh M, Qorbani M, Hosseini S. Association of circulating irisin levels with normal weight obesity, glycemic and lipid profile. J Diabetes Metab Disord. 2016;15:17. https://doi.org/10.1186/s40200-016-0239-5.
Gouni-Berthold I, Berthold HK, Huh JY, et al. Effects of lipid-lowering drugs on irisin in human subjects in vivo and in human skeletal muscle cells ex vivo. PLoS ONE. 2013;8(9):e72858. https://doi.org/10.1371/journal.pone.0072858.
Huo CJ, Yu XJ, Sun YJ, et al. Irisin lowers blood pressure by activating the Nrf2 signaling pathway in the hypothalamic paraventricular nucleus of spontaneously hypertensive rats. Toxicol Appl Pharmacol. 2020;394: 114953. https://doi.org/10.1016/j.taap.2020.114953.
Huang Y, Chen Q, Jiang Q, Zhao Z, Fang J, Chen L. Irisin lowers blood pressure in Zucker diabetic rats by regulating the functions of renal angiotensin II type 1 receptor via the inhibition of the NF-κB signaling pathway. Peptides. 2022;147: 170688. https://doi.org/10.1016/j.peptides.2021.170688.
Wang X, Zhang Z, Lan X, et al. Irisin is correlated with blood pressure in obstructive sleep apnea patients. Int J Hypertens. 2021;2021:4717349. https://doi.org/10.1155/2021/4717349.
De Meneck F, Victorino de Souza L, Oliveira V, do Franco MC. High irisin levels in overweight/obese children and its positive correlation with metabolic profile, blood pressure, and endothelial progenitor cells. Nutr Metab Cardiovasc Dis. 2018;28(7):756–64. https://doi.org/10.1016/j.numecd.2018.04.009.
Miazgowski T, Miazgowski B, Kaczmarkiewicz A, Kopeć J. Associations of circulating irisin with 24-h blood pressure, total and visceral fat, and metabolic parameters in young adult hypertensives. Arch Endocrinol Metab. 2021;65(2):137–43. https://doi.org/10.20945/2359-3997000000333.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12. https://doi.org/10.1001/jama.283.15.2008.
World Health Organization. Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight Accessed 9 June 2021
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Rupinski MT, Dunlap WP. Approximating pearson product-moment correlations from kendall’s tau and spearman’s rho. Educational Psychol Meas. 1996. https://doi.org/10.1177/0013164496056003004.
Higgins J. Introduction to meta-analysis. Hoboken: Wiley; 2009.
Tentolouris A, Eleftheriadou I, Tsilingiris D, et al. Plasma irisin levels in subjects with type 1 diabetes: comparison with healthy controls. Horm Metab Res. 2018;50(11):803–10. https://doi.org/10.1055/a-0748-6170.
Jameel F, Thota RN, Wood LG, Plunkett B, Garg ML. Sex-dependent association between circulating irisin levels and insulin resistance in healthy adults. J Nutr Intermediary Metab. 2015;2(3–4):86–92. https://doi.org/10.1016/j.jnim.2015.10.001.
Norheim F, Langleite TM, Hjorth M, et al. The effects of acute and chronic exercise on PGC-1α, irisin and browning of subcutaneous adipose tissue in humans. FEBS J. 2014;281(3):739–49. https://doi.org/10.1111/febs.12619.
Li M, Yang M, Zhou X, et al. Elevated circulating levels of irisin and the effect of metformin treatment in women with polycystic ovary syndrome [published correction appears in J Clin Endocrinol Metab. 2015 Aug;100(8):3219]. J Clin Endocrinol Metab. 2015;100(4):1485–93. https://doi.org/10.1210/jc.2014-2544.
Moon HS, Dalamaga M, Kim SY, et al. Leptin’s role in lipodystrophic and nonlipodystrophic insulin-resistant and diabetic individuals. Endocr Rev. 2013;34(3):377–412. https://doi.org/10.1210/er.2012-1053.
Crujeiras AB, Pardo M, Casanueva FF. Irisin: “fat” or artefact. Clin Endocrinol. 2014;82(4):467–74.
Al-Daghri NM, Alkharfy KM, Rahman S, et al. Irisin as a predictor of glucose metabolism in children: sexually dimorphic effects. Eur J Clin Invest. 2014;44(2):119–24. https://doi.org/10.1111/eci.12196.
Cypess AM, Lehman S, Williams G, et al. Identification and importance of brown adipose tissue in adult humans. N Engl J Med. 2009;360(15):1509–17. https://doi.org/10.1056/NEJMoa0810780.
Nookaew I, Svensson PA, Jacobson P, et al. Adipose tissue resting energy expenditure and expression of genes involved in mitochondrial function are higher in women than in men. J Clin Endocrinol Metab. 2013;98(2):E370–8. https://doi.org/10.1210/jc.2012-2764.
Zhang HJ, Zhang XF, Ma ZM, et al. Irisin is inversely associated with intrahepatic triglyceride contents in obese adults. J Hepatol. 2013;59(3):557–62. https://doi.org/10.1016/j.jhep.2013.04.030.
Armandi A, Rosso C, Nicolosi A, Caviglia GP, Abate ML, Olivero A, D’Amato D, Vernero M, Gaggini M, Saracco GM, Ribaldone DG, Leeming DJ, Gastaldelli A, Bugianesi E. Crosstalk between irisin levels liver fibrogenesis and liver damage in non-obese non-diabetic individuals with non-alcoholic fatty liver disease. J Clin Med. 2022;11(3):635. https://doi.org/10.3390/jcm11030635
Foda AA, Foda EA, Abel-Aal I. Serum irisin levels as a marker in some phenotypes of PCOS. Middle East Fertil Soc J. 2018;23(2):112–116. https://doi.org/10.1016/j.mefs.2017.09.005
Foda AA, Foda EA, El-Said ZH. Serum irisin levels in polycystic ovary syndrome after ovarian drilling. Diab Metab Syndr Clin Res Rev. 2019;13(2):1463–1468. https://doi.org/10.1016/j.dsx.2019.02.019
Mehrabian S, Taheri E, Karkhaneh M, Qorbani M, Hosseini S. Association of circulating irisin levels with normal weight obesity glycemic and lipid profile. J Diab Metab Disord. 2015;15(1):17. https://doi.org/10.1186/s40200-016-0239-5
Rashid FA, Abbas HJ, Naser NA, Addai Ali H. Effect of long-term moderate physical exercise on irisin between normal weight and obese men. Sci World J. 2020;2020:1–7. https://doi.org/10.1155/2020/1897027
Zhu H, Liu M, Zhang N, Pan H, Lin G, Li N, Wang L, Yang H, Yan K,Gong F. Serum and adipose tissue mRNA levels of ATF3 and FNDC5/irisin in colorectal cancer patients with or without obesity. Front Physiol. 2018;9. https://doi.org/10.3389/fphys.2018.01125
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
YL: conceptualization, methodology, data analysis, writing-original draft preparation. ZX: methodology, writing- reviewing and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search strategy and results.
Additional file 2.
Methodological Quality of case–control and cross-sectional studies included in the meta-analysis.
Additional file 3.
Summary of the subgroup analyses of the correlation between circulating irisin levels and fasting blood glucose.
Additional file 4.
Summary of the subgroup analyses of the correlation between circulating irisin levels and HOMA-IR.
Additional file 5.
Summary of the subgroup analyses of the correlation between circulating irisin levels and BMI.
Additional file 6.
Funnel plots of included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Y., Xu, Z. Association between irisin and metabolic parameters in nondiabetic, nonobese adults: a meta-analysis. Diabetol Metab Syndr 14, 152 (2022). https://doi.org/10.1186/s13098-022-00922-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00922-w