Abstract
Background
Increased serum carcinoembryonic antigen (CEA) levels are reported to be associated with various metabolic and inflammatory diseases. This study assessed whether high-normal serum CEA is related to diabetic peripheral neuropathy (DPN) in patients with type 2 diabetes (T2D).
Methods
All subjects received DPN assessment based on neuropathic symptoms, neuropathic signs, and nerve conduction studies to calculate composite Z scores of nerve latency, amplitude and conduction velocity (NCV). DPN was confirmed by both at least a presentation of neuropathic symptoms/signs and an abnormal nerve conduction index. Serum CEA levels and other clinical indices were also synchronously detected. Multivariable linear regression analyses were used to determine the independent effects of serum CEA levels on nerve conduction indices, multivariable logistic regression analyses were used to determine the independent impact of CEA levels on the risk of DPN, and receiver operating characteristic (ROC) curve analysis was used to assess the diagnostic capability of CEA levels to discriminate DPN.
Results
We ultimately recruited 402 eligible subjects with normal ranges of serum CEA for this study, and 25.4% (n = 102) were determined to have DPN. After adjusting for other clinical covariates, serum CEA levels were independently associated with the composite Z score for latency (β = 0.132, t = 2.330, p = 0.021), amplitude (β = − 0.164, t = − 2.838, p = 0.005) and NCV (β = − 0.210, t = − 3.662, p < 0.001). Moreover, the prevalence of DPN in the first, second, third and fourth quartiles of CEA level was 12.9%, 19.0%, 29.4% and 40.4%, respectively (p for trend < 0.001); the corresponding adjusted odds ratios and 95% CIs for DPN in CEA quartiles were 1, 1.47 (0.45–4.82), 1.72 (0.54–5.53) and 4.58 (1.39–15.06), respectively. Furthermore, the optimal cut-off value of high-normal serum CEA to discriminate DPN was ≥ 2.66 ng/mL, with a Youden index of 0.28, sensitivity of 66.67% and specificity of 61.00%.
Conclusions
Increased serum CEA levels within the normal range are closely linked to dysfunction of peripheral nerve conduction and the risk of DPN, and high-normal serum CEA levels are a potential risk factor for DPN in T2D.
Similar content being viewed by others
Background
Diabetic peripheral neuropathy (DPN), developing in the background of diabetes, is a main precipitating factor for falls, fractures, trauma, foot ulcerations, lower limb amputation and no specific death [1, 2]. Patients with DPN tend to have disability, a poor quality of life, reduced psychosocial well-being and a high burden of health care costs [3, 4]. Although the pathogenesis of DPN is not thoroughly understood, it involves interactions between multiple risk factors in the context of diabetes. Therefore, it is worthwhile to explore additional reliable risk factors associated with DPN pathogenesis, which may help formulate earlier approaches to ameliorate DPN.
Carcinoembryonic antigen (CEA), originally regarded as an oncofoetal antigen, is highly expressed in carcinomas [5]. In contrast, CEA is expressed at low levels in normal tissues of epithelial origin [6]. Moreover, increased levels of serum CEA within the normal or near-normal range are reported to be associated with various metabolic and inflammatory diseases. Increased serum CEA levels are not only cross-sectionally associated with obesity, metabolic syndrome, and leukoaraiosis of the brain [7,8,9] but can also longitudinally predict cardiovascular events and mortality in the general population [10]. Additionally, serum CEA levels are increased in patients with prediabetes and type 2 diabetes (T2D) and are associated with diabetic complications, such as diabetic nephropathy [11, 12]. Nevertheless, the relationship between serum CEA levels and DPN in T2D has not been well investigated. Therefore, we hypothesize that increased serum CEA levels may be a risk factor for DPN in T2D.
We designed the present study to explore whether increased serum CEA levels within the normal range are associated with an increased risk of DPN in T2D.
Methods
Subject recruitment
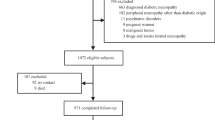
This study was part of a series we designed to explore potential risks for DPN. We recruited subjects with T2D who visited the Endocrinology Department of First People’s Hospital of Nantong City and Second People’s Hospital of Nantong City between November 2017 and December 2021. The inclusion criteria were as follows: (1) between 20 and 80 years of age; (2) meeting the diagnostic criteria for T2D (2015 Edition, American Diabetes Association) [13]; (3) serum CEA level < 10 ng/mL; and (4) voluntarily agreed to participate in the study. The exclusion criteria were as follows: (1) positive for anti-insulin antibodies; (2) thyroid hormonal abnormality; (3) history of cancer; (4) any possible space-occupying lesions detected by chest X-ray and abdominal ultrasonography; (5) excessive alcohol consumption (excessive alcohol intake, > 40 g daily for women and > 60 g daily for men); (6) severe cardio-cerebral vascular disease (e.g., myocardial infarction); (7) chronic kidney disease and estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2; (8) autoimmune disease; (9) acute or chronic infectious disease; (10) connective tissue disease; (11) use of drugs with neurotoxic side effects; (12) deficiency in folate or vitamin B12; (13) neurodegenerative disease; (14) inflammatory demyelinating neuropathy; and (15) spinal or foraminal stenosis. We ultimately recruited 402 eligible subjects with serum CEA levels in the normal range for this study. As the study was initiated and academically supported by First People’s Hospital of Nantong, the study protocol was reviewed and approved by the First People’s Hospital of Nantong. In addition, the processes of the study followed the Declaration of Helsinki, and all participants provided informed consent when recruited.
Clinical data collection
Collection of clinical data from all participants was carried out by trained clinical staff. Relevant clinical data for statistical analyses included age, sex, body mass index (BMI), systolic/diastolic blood pressure (SBP/DBP), diabetes duration, hypertension status, drinking behavior, statin use, and antidiabetic treatments. Hypertension was identified as reported in our previous study [14]. Drinking behaviour was divided into three categories: no alcohol consumption, alcohol consumption (mild-to-moderate alcohol intake) and excessive alcohol consumption (excessive alcohol intake, > 40 g daily for women and > 60 g daily for men). Antidiabetic treatments were divided into nine categories: drug naive, insulin, secretagogues, metformin, thiozolindiones (TZDs), α-glucosidase inhibitors (AGIs), dipeptidyl peptidase-4 inhibitors (DPP-4Is), sodium-glucose cotransporter-2 inhibitors (SGLT-2Is), and glucagon-like peptide-1 receptor agonists (GLP-1RAs).
Serum was isolated from blood specimens (stored in CAT Serum Clot Activator tubes, Greiner Bio-one) to detect CEA, alanine aminotransferase (ALT), total bilirubin (TBI), albumin, triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDLC), low-density lipoprotein cholesterol (LDLC), uric acid (UA) and C-peptide. Whole-blood specimens were drawn to detect glycosylated haemoglobin (HbA1c). Plasma was isolated to detect glucagon. Serum creatinine was detected to calculate the estimated glomerular filtration rate (eGFR) using the Modification of Diet in Renal Disease equation [15].
Serum CEA levels were measured by chemiluminescence microcarticle immunoassays (CEA Reagent Kit, Architect System, Abbott Ireland Diagnostics Division, Sligo, Ireland) using a fully automated immunoassay analyser (i200SR, Architect, Abbott Laboratories, IL, USA). The precision of the serum CEA assay was tested by determination of intra-assay variation (%CV) and total intralaboratory variation (%CV). Total intralaboratory variation is an overall assessment of intra-assay variation, interassay variation and interday variation. The intra-assay variation in serum CEA was < 2.5%, and the intralaboratory variation was < 2.9%.
Screening for DPN and nerve conduction analysis
Confirmation of DPN is dependent on both at least a presentation of neuropathic manifestations (neuropathic symptoms or signs) and an abnormal index of peripheral nerve conduction, which is based on the Toronto Consensus Guideline [16]. The screening process for DPN was also described in our previous studies [17, 18].
Neuropathic symptoms and signs were collected by detailed history taking and physical examinations. Neurological symptoms manifested as numbness, imbalance, paresthesia (e.g., cooling sensation) and paroxysmal/persistent pain, such as tingling, burning, electric shock, cutting, and stabbing pain. Neuropathic signs caused by the involvement of large fibre neuropathy were assessed based on reduced or absent ankle reflexes and deep sensation (e.g., vibration perception, pressure perception, balance perception and proprioception) and by involvement of small fibre neuropathy according to superficial sensation (e.g., thermal sensation, haptic sensations and pinprick sensation).
Nerve conduction studies were performed by an experienced neuropathic technician using an electromyogram (MEB-9200K, Nihon Kohden), including the median nerve (MN) and ulnar nerve (UN) of the bilateral upper limbs and the common peroneal nerve (CPN), posterior tibial nerve (PTN), sural nerve (SN) and superficial peroneal nerve (SPN) of the bilateral lower limbs. The nerve conduction parameters included the nerve action potential onset latency, amplitude and conduction velocity (NCV) of the MN, UN, CPN and PTN motor nerves and of the MN, UN, SN and SPN sensory nerves. Data for nerve latency, amplitude and NCV were then Z score transformed. Furthermore, a composite Z score of latency was generated by taking the average value of the latency Z score of all motor and sensory nerves of the upper and lower limbs, as also described in our previous study [18]. In the same way, composite Z scores of amplitude and NCV were generated.
Statistical analysis
The clinical variables were pooled and analysed with SPSS for Windows (Version 25.0, IBM Corp.), and statistical significance was defined as p < 0.05.
Clinical variables are shown for all subjects and four subgroups based on the serum CEA quartiles. Normally distributed data were described as the means and standard deviations, skew-distributed data were described as medians and interquartile ranges, and categorical data were described as frequencies and percentages. Serum CEA was skew-distributed and was natural-logarithm transformed (lnCEA). To analyse changes in trends of clinical data among the four subgroups, one-way analysis of variance (ANOVA) with linear polynomial contrasts (F value), the Jonckheere–Terpstra test (standard Z value) and the chi-squared test with linear-by-linear association (x2 value) were used, as appropriate.
Pearson’s correlation was employed to assess univariate correlation between serum CEA levels and nerve conduction indices. Moreover, given that HbA1c may exert an effect on these correlations, partial correlation was used to adjust the effect of HbA1c.
Multivariable linear regression analyses were used to determine the independent effects of serum CEA levels on nerve conduction indices, multivariable logistic regression analyses were used to determine odds ratios (ORs) and 95% confidence intervals (CIs) for the risk of DPN in the four subgroups based on CEA quartiles, and receiver operating characteristic (ROC) curve analysis was used to assess the diagnostic capability of CEA levels to discriminate DPN.
Results
Clinical features of recruited subjects
The clinical features of all eligible subjects are shown in Table 1. The range of serum CEA levels in all subjects was 0.33–9.72 ng/mL, and those of the first, second, third and fourth quartiles (Q1, Q2, Q3 and Q4) were 0.33–1.73 ng/mL, 1.74–2.54 ng/mL, 2.55–3.70 ng/mL and 3.72–9.72 ng/mL, respectively. Age, SBP and HbA1c increased with ascending serum CEA quartile, whereas the female distribution, albumin and fasting C-peptide decreased. Conversely, diabetes duration, DBP, hypertension history, statin use, ALT, lipid profiles, UA, eGFR and glucagon showed no differences among the four subgroups. Regarding antidiabetic treatments, insulin use tended to increase serum CEA within the normal range (p = 0.020), but SGLT-2I use tended to decrease it (p = 0.011). The parameters drug naive and use of secretagogues, metformin, TZDs, AGIs, DPP-4Is and GLP-1RAs were comparable among the four subgroups.
Correlations between serum CEA and nerve conduction indices
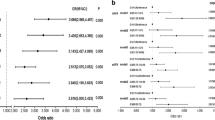
With increasing quartiles of serum CEA, the composite Z score of latency increased, whereas that of amplitude and NCV decreased markedly (Table 1). Univariate correlation analysis demonstrated serum CEA levels to be linked to the composite Z score of nerve latency, amplitude and NCV (r = 0.270, − 0.263 and − 0.328, respectively, p < 0.001). After controlling for the potential effect of HbA1c on these correlations by partial correlation analysis, serum CEA levels remained linked to the composite Z score of nerve latency, amplitude and NCV (r = 0.211, − 0.223 and − 0.260, respectively, p < 0.001). These correlations are graphically displayed in Figs. 1 and 2.
Moreover, we used multivariable linear regression analyses to determine the effects of serum CEA levels on nerve conduction indices (Table 2). After gradually adjusting for other coagulation function indices and clinical covariates (from model 0 to model 4), serum CEA remained independently associated with nerve conduction indices. According to fully adjusted model 4, serum CEA levels were independently and positively related to the composite Z score of latency (β = 0.132, t = 2.330, p = 0.021) and independently and negatively related to the composite Z score of amplitude (β = − 0.164, t = − 2.838, p = 0.005) and NCV (β = − 0.210, t = − 3.662, p < 0.001).
Risks for DPN of different serum CEA quartiles
After DPN assessment, 25.4% (n = 102) of the recruited subjects were determined to have DPN. The prevalence of DPN in CEA level Q1, Q2, Q3 and Q4 was 12.9%, 19.0%, 29.4% and 40.4%, respectively (p for trend < 0.001). Moreover, the ORs and 95% CIs for DPN in CEA level Q1, Q2, Q3 and Q4 were 1, 1.59 (0.74–3.42), 2.82 (1.37–5.80), and 4.59 (2.26–9.31), respectively (Table 3). After adjusting for other clinical covariates by multivariable logistic regression analyses, the corresponding ORs and 95% CIs for DPN in Q1, Q2, Q3 and Q4 were 1, 1.47 (0.45–4.82), 1.72 (0.54–5.53) and 4.58 (1.39–15.06), respectively (Table 3).
Potential capability of serum CEA to discriminate DPN
Figure 3 illustrates the ability of serum CEA to discriminate DPN after ROC curve analysis. The area under the ROC curve (AUC) of serum CEA was 0.666 (95% CI 0.617–0.712). Additionally, ROC analysis determined an optimal cut-off value of serum CEA to discriminate DPN of ≥ 2.66 ng/mL, with Youden index = 0.28, sensitivity = 66.67%, and specificity = 61.00%.
Comparison of serum CEA and HbA1c to discriminate DPN
Because HbA1c was identified as a traditional risk factor for DPN in our previous studies [14, 17], we used ROC analysis to compare the capability of serum CEA and HbA1c to discriminate DPN by the methods of DeLong et al. (Additional file 1: Fig. S1). The AUC of HbA1c in our present study was 0.693 (95% CI 0.646–0.738). After comparing with HbA1c, we found that the capability of serum CEA to discriminate DPN was comparable to that of HbA1c (AUC difference of 0.0277 [95% CI − 0.0516 to 0.107], Z = 0.684, p = 0.494).
Discussion
The pathogenesis of DPN is complex and not thoroughly understood [19]. Several risk factors have been proposed for DPN discrimination during the exploration of DPN pathogenesis [20]. We have also initiated series expecting to find new potential risk factors to assist in DPN discrimination. In the series, we routinely tested tumor markers to screen or exclude tumors. To our surprise, we found that increased serum CEA levels within the normal range are related to DPN in T2D. The present study then explored the relationship in depth. The main contributions of the present study are as follows: first, high-normal serum CEA levels were closely connected with the nerve action potential onset latency, amplitude and conduction velocity in patients with T2D; second, the risk of DPN was estimated to be fourfold (OR 4.58, 95% CI 1.39–15.06) higher in patients in the highest quartile of serum CEA than in those in the lowest quartile; third, serum CEA level ≥ 2.66 ng/mL was the optimal cut-off value to discriminate DPN (sensitivity = 66.67%, specificity = 61.00%); fourth, serum CEA and HbA1c, a well-established risk factor for DPN, were comparable in their ability to discriminate DPN.
Increased serum CEA levels have been demonstrated to be associated with a range of unfavourable clinical outcomes under nonmalignant conditions, as well as in malignant tumours, due to its overexpression in adenocarcinomas. In a healthy checkup population (n = 18,131), serum CEA levels correlated positively with age, white blood cell (WBC) count, haemoglobin, aspartate aminotransferase and HbA1c and negatively with BMI and sex (reference: male) [21]. Moreover, increased levels of serum CEA, even within the normal or near-normal range, may be involved in arterial stiffness [22], carotid atherosclerosis [23], abdominal visceral fat accumulation [7], metabolic syndrome [8], metabolic-associated fatty liver disease [24], chronic kidney disease [25], leukoaraiosis [9], and Parkinson’s disease [26] in the general population. In a follow-up study, increased serum CEA may also account for the progression of coronavirus disease 2019 [27], more frequent fracture incidence [28], severity of heart failure (HF), HF adverse prognosis [29], CVD events and all-cause mortality [10]. Furthermore, elevated serum CEA may be an important risk factor for prediabetes and T2D [11], and the levels of serum CEA are closely associated with poor glycaemic control [30] and oxygen desaturation index [31] in patients with T2D. Regarding diabetic complications, higher serum CEA levels may independently contribute to macroalbuminuria in patients with diabetes [12]. In our present study, we found that increased serum CEA is independently associated with increased nerve action potential onset latency and decreased nerve amplitude and NCV in T2D. Patients in the highest serum CEA level quartile showed a fourfold higher DPN risk than those in the lowest quartile. We also calculated that serum CEA ≥ 2.66 ng/mL is the optimal cut-off value to discriminate DPN, with a sensitivity of 66.67% and specificity of 61.00%. Our study adds evidence to support that high-normal serum CEA is a promising risk factor for DPN in patients with T2D.
DPN is a progressive multifactorial diabetic complication. Hyperglycaemia is one of the primary promoters for DPN in T2D, but other risk factors, such as dyslipidaemia, hyperinsulinaemia and inflammation, also contribute [19, 32]. Inflammation is closely connected to hyperglycaemia, insulin resistance and dyslipidaemia in central pathways for DPN [20]. Several cross-sectional and longitudinal studies have recognized the potential clinical relevance of systemic markers of chronic inflammation for DPN. A meta-analysis by Mu et al. [33] showed that a higher level of serum tumour necrosis factor-α (TNF-α) may be independently associated with a higher risk of DPN. Circulating blood leukocyte parameters, such as the neutrophil-to-lymphocyte ratio (NLR) and total WBC count, have been shown to be associated with impaired peripheral nerve functions and increased risk of DPN [34, 35]. Herder et al. [36] revealed in a 6.5-year follow-up study that elevated proinflammatory cytokines, including high-sensitivity C-reactive protein (hs-CRP), interleukin-6 (IL-6), TNF-α, and soluble intercellular adhesion molecule (sICAM-1), can predict the incidence of DPN; hs-CRP, IL-6 and sICAM-1 were also linked to painful DPN independent of metabolic covariates [37, 38]. The serum CEA is actually a pro-thrombotic and pro-inflammatory factor rather than a purely biochemical marker for carcinomas [9]. In our present study, high-normal serum CEA levels were closely associated with DPN independent of glycaemic exposure, dyslipidaemia and other clinical confounders.
Although the role of increased serum CEA in patients with DPN remains unclear, several possible mechanisms may be suggested for the relationship between this marker and DPN pathogenesis. Recent experimental, clinical, and epidemiological studies have pointed towards oxidative stress and inflammatory reactions as important physiopathological mechanisms of diabetic neuropathy [19, 20, 39]. Oxidative stress and inflammatory processes cause DNA damage, endoplasmic reticulum stress, mitochondrial overproduction of superoxide and subsequent apoptosis, and loss of neurotrophic signalling, all of which ultimately lead to nerve dysfunction and neuropathy [20, 40]. Increased serum CEA may serve as an inflammatory mediator and a trigger of oxidative stress in DPN pathogenesis pathways. First, serum CEA levels are closely linked to systemic inflammation markers, such as the total WBC count [41, 42], neutrophil-to-lymphocyte ratio and hs-CRP [26], which reportedly contribute to DPN. Second, some experimental studies have shown that CEA stimulates monocytes and macrophages to release pro-inflammatory cytokines such as IL-1, IL-6, and TNF-α [43, 44]. Third, increased serum CEA is closely associated with oxidative stress markers assessed by serum malondialdehyde (MDA) [45], indicating that increased serum CEA may promote oxidative stress. Additionally, previous studies have revealed that increased serum CEA may have an important role in CNS degeneration, such as leukoaraiosis and Parkinson’s disease [9, 26], which indirectly suggests a role for increased CEA in nerve tissue injury.
The present study should be considered in light of a few limitations. First, due to the cross-sectional design, our data are not sufficient to establish a causal role of increased serum CEA in the development of DPN. In this regard, a longitudinal study is currently being conducted to compensate for this deficiency. Second, the levels of serum CEA correlated with markers of systemic inflammation and oxidative stress, but we did not assess the effect of inflammation and oxidative stress markers on the relationship between serum CEA and DPN. Third, due to the small sample size of patients with painful DPN in our present study, we did not assess the association between CEA levels and the severity of neuropathic pain. Fourth, our results may be affected by the heterogeneity among T2D patients who received multiple antidiabetic agents. We sought to compensate for this limitation by adjusting for antidiabetic agents during the statistical analysis.
Conclusion
In summary, increased serum CEA levels within the normal range are closely linked to dysfunction of peripheral nerve conduction and the prevalence of DPN, and high-normal serum CEA levels are a potential risk factor for DPN in T2D.
Availability of data and materials
Data for this study are available from the principal investigators upon reasonable request.
Abbreviations
- CEA:
-
Carcinoembryonic antigen
- lnCEA:
-
Natural logarithm-transformed CEA
- Q1:
-
First quartile of CEA levels
- Q2:
-
Second quartile of CEA levels
- Q3:
-
Third quartile of CEA levels
- Q4:
-
Fourth quartile of CEA levels
- T2D:
-
Type 2 diabetes
- DPN:
-
Diabetic peripheral neuropathy
- NCV:
-
Nerve conduction velocity
- SBP/DBP:
-
Systolic/diastolic blood pressure
- BMI:
-
Body mass index
- TZDs:
-
Thiozolindiones
- AGIs:
-
α-Glucosidase inhibitors
- DPP-4Is:
-
Dipeptidyl peptidase-4 inhibitors
- SGLT-2Is:
-
Sodium-glucose cotransporter-2 inhibitors
- GLP-1RAs:
-
Glucagon-like peptide-1 receptor agonists
- ALT:
-
Alanine aminotransferase
- TBI:
-
Total bilirubin
- TG:
-
Triglycerides
- TC:
-
Total cholesterol
- HDLC:
-
High-density lipoprotein cholesterol
- LDLC:
-
Low-density lipoprotein cholesterol
- UA:
-
Uric acid
- eGFR:
-
Estimated glomerular filtration rate
- HbA1c:
-
Glycosylated hemoglobin A1c
- MN:
-
Median nerve
- UN:
-
Ulnar nerve
- CPN:
-
Common peroneal nerve
- PTN:
-
Posterior tibial nerve
- SN:
-
Sural nerve
- SPN:
-
Superficial peroneal nerve
References
Vas PRJ, Edmonds ME. Early recognition of diabetic peripheral neuropathy and the need for one-stop microvascular assessment. Lancet Diabetes Endocrinol. 2016;4(9):723–5.
Hicks CW, Selvin E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diabetes Rep. 2019;19(10):86.
Jaiswal M, Fufaa GD, Martin CL, Pop-Busui R, Nelson RG, Feldman EL. Burden of diabetic peripheral neuropathy in Pima Indians with type 2 diabetes. Diabetes Care. 2016;39(4):e63–4.
Ebata-Kogure N, Nozawa K, Murakami A, Toyoda T, Haga Y, Fujii K. Clinical and economic burdens experienced by patients with painful diabetic peripheral neuropathy: an observational study using a Japanese claims database. PLoS ONE. 2017;12(10): e0187250.
Loosen SH, Roderburg C, Kauertz KL, Koch A, Vucur M, Schneider AT, et al. CEA but not CA19-9 is an independent prognostic factor in patients undergoing resection of cholangiocarcinoma. Sci Rep. 2017;7(1):16975.
Hammarström S. The carcinoembryonic antigen (CEA) family: structures, suggested functions and expression in normal and malignant tissues. Semin Cancer Biol. 1999;9(2):67–81.
Lee JY, Lee HK, Lee DC, Lee JW. Serum carcinoembryonic antigen is associated with abdominal visceral fat accumulation in female Korean nonsmokers. PLoS ONE. 2012;7(8): e43518.
Lee JW, Park KD, Im JA, Hwang HJ, Kim SH. Serum carcinoembryonic antigen is associated with metabolic syndrome in female Korean non-smokers. Clin Chim Acta. 2011;412(7–8):527–30.
Seo MS, Shim JY, Lee YJ. Association between serum carcinoembryonic antigen (CEA) levels and leukoaraiosis in middle-aged and older adults: a cross-sectional study. Exp Gerontol. 2019;125: 110682.
Bracun V, Suthahar N, Shi C, de Wit S, Meijers WC, Klip IT, et al. Established tumour biomarkers predict cardiovascular events and mortality in the general population. Front Cardiovasc Med. 2021;8: 753885.
Cheng YC, Li YH, Hsu CY, Lee IT. Synergistic association of carcinoembryonic antigen and carbohydrate antigen 19-9 on the risk of abnormal glucose regulation. Diabetes Metab Syndr Obes. 2020;13:1933–42.
Chen J, Tao F, Zhang B, Chen Q, Qiu Y, Luo Q, et al. Elevated squamous cell carcinoma antigen, cytokeratin 19 fragment, and carcinoembryonic antigen levels in diabetic nephropathy. Int J Endocrinol. 2017;2017:5304391.
American Diabetes Association. (2) Classification and diagnosis of diabetes. Diabetes Care. 2015;38(Suppl):S8-16.
Hu YM, Zhao LH, Zhang XL, Cai HL, Huang HY, Xu F, et al. Association of glycaemic variability evaluated by continuous glucose monitoring with diabetic peripheral neuropathy in type 2 diabetic patients. Endocrine. 2018;60(2):292–300.
Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145(4):247–54.
Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33(10):2285–93.
Su JB, Zhao LH, Zhang XL, Cai HL, Huang HY, Xu F, et al. HbA1c variability and diabetic peripheral neuropathy in type 2 diabetic patients. Cardiovasc Diabetol. 2018;17(1):47.
Xu F, Zhao LH, Wang XH, Wang CH, Yu C, Zhang XL, et al. Plasma 1,5-anhydro-d-glucitol is associated with peripheral nerve function and diabetic peripheral neuropathy in patients with type 2 diabetes and mild-to-moderate hyperglycemia. Diabetol Metab Syndr. 2022;14(1):24.
Sloan G, Selvarajah D, Tesfaye S. Pathogenesis, diagnosis and clinical management of diabetic sensorimotor peripheral neuropathy. Nat Rev Endocrinol. 2021;17(7):400–20.
Bönhof GJ, Herder C, Strom A, Papanas N, Roden M, Ziegler D. Emerging biomarkers, tools, and treatments for diabetic polyneuropathy. Endocr Rev. 2019;40(1):153–92.
Kang HY, Choe EK, Park KJ, Lee Y. Factors requiring adjustment in the interpretation of serum carcinoembryonic antigen: a cross-sectional study of 18,131 healthy nonsmokers. Gastroenterol Res Pract. 2017;2017:9858931.
Bae U, Shim JY, Lee HR, Shin JY. Serum carcinoembryonic antigen level is associated with arterial stiffness in healthy Korean adult. Clin Chim Acta. 2013;415:286–9.
Ishizaka N, Ishizaka Y, Toda E, Koike K, Yamakado M, Nagai R. Are serum carcinoembryonic antigen levels associated with carotid atherosclerosis in Japanese men? Arterioscler Thromb Vasc Biol. 2008;28(1):160–5.
Lee JY, Lee DC, Lee JW. Serum carcinoembryonic antigen is associated with non-alcoholic fatty liver disease in healthy Korean non-smokers. Clin Chem Lab Med. 2013;51(7):1499–504.
Tong HL, Dong ZN, Wen XY, Gao J, Wang B, Tian YP. Impact of chronic kidney disease on serum tumor markers concentrations. Chin Med J (Engl). 2013;126(2):274–9.
Akıl E, Bulut A, Kaplan İ, Özdemir HH, Arslan D, Aluçlu MU. The increase of carcinoembryonic antigen (CEA), high-sensitivity C-reactive protein, and neutrophil/lymphocyte ratio in Parkinson’s disease. Neurol Sci. 2015;36(3):423–8.
Huang R, Meng T, Zha Q, Cheng K, Zhou X, Zheng J, et al. The predicting roles of carcinoembryonic antigen and its underlying mechanism in the progression of coronavirus disease 2019. Crit Care. 2021;25(1):234.
Kim BJ, Baek S, Lee SH, Ahn SH, Kim HM, Kim SH, et al. Higher serum carcinoembryonic antigen levels associate with more frequent development of incident fractures in Korean women: a longitudinal study using the national health insurance claim data. Bone. 2015;73:190–7.
Shi C, van der Wal HH, Silljé HHW, Dokter MM, van den Berg F, Huizinga L, et al. Tumour biomarkers: association with heart failure outcomes. J Intern Med. 2020;288(2):207–18.
Lu J, Wang H, Zhang X, Yu X. HbA1c is positively associated with serum carcinoembryonic antigen (CEA) in patients with diabetes: a cross-sectional study. Diabetes Ther. 2018;9(1):209–17.
Zhou J, Huang X, Jiang X. Effects of obstructive sleep apnea-hypopnea syndrome on serum carcinoembryonic antigen levels in patients with type 2 diabetes mellitus. Med Sci Monit. 2019;25:3558–65.
Selvarajah D, Kar D, Khunti K, Davies MJ, Scott AR, Walker J, et al. Diabetic peripheral neuropathy: advances in diagnosis and strategies for screening and early intervention. Lancet Diabetes Endocrinol. 2019;7(12):938–48.
Mu ZP, Wang YG, Li CQ, Lv WS, Wang B, Jing ZH, et al. Association between tumor necrosis factor-alpha and diabetic peripheral neuropathy in patients with type 2 diabetes: a meta-analysis. Mol Neurobiol. 2017;54(2):983–96.
Wang DD, Bakhotmah BA, Hu FB, Alzahrani HA. Prevalence and correlates of diabetic peripheral neuropathy in a Saudi Arabic population: a cross-sectional study. PLoS ONE. 2014;9(9): e106935.
Liu S, Zheng H, Zhu X, Mao F, Zhang S, Shi H, et al. Neutrophil-to-lymphocyte ratio is associated with diabetic peripheral neuropathy in type 2 diabetes patients. Diabetes Res Clin Pract. 2017;130:90–7.
Herder C, Kannenberg JM, Huth C, Carstensen-Kirberg M, Rathmann W, Koenig W, et al. Proinflammatory cytokines predict the incidence and progression of distal sensorimotor polyneuropathy: KORA F4/FF4 study. Diabetes Care. 2017;40(4):569–76.
Herder C, Bongaerts BW, Rathmann W, Heier M, Kowall B, Koenig W, et al. Differential association between biomarkers of subclinical inflammation and painful polyneuropathy: results from the KORA F4 study. Diabetes Care. 2015;38(1):91–6.
Shillo P, Sloan G, Greig M, Hunt L, Selvarajah D, Elliott J, et al. Painful and painless diabetic neuropathies: what is the difference? Curr Diabetes Rep. 2019;19(6):32.
El Boghdady NA, Badr GA. Evaluation of oxidative stress markers and vascular risk factors in patients with diabetic peripheral neuropathy. Cell Biochem Funct. 2012;30(4):328–34.
Callaghan BC, Cheng HT, Stables CL, Smith AL, Feldman EL. Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol. 2012;11(6):521–34.
Ge S, Xie J, Zheng L, Yang L, Zhu H, Cheng X, et al. Associations of serum anti-ganglioside antibodies and inflammatory markers in diabetic peripheral neuropathy. Diabetes Res Clin Pract. 2016;115:68–75.
Kwon YJ, Lee HS, Shim JY, Lee YJ. Serum carcinoembryonic antigen is positively associated with leukocyte count in Korean adults. J Clin Lab Anal. 2018;32(3): e22291.
Ganguly A, Yeltsin E, Robbins J. Identification of a carcinoembryonic antigen binding protein on monocytes. Biochem Biophys Res Commun. 2003;311(2):319–23.
Thomas P, Hayashi H, Zimmer R, Forse RA. Regulation of cytokine production in carcinoembryonic antigen stimulated Kupffer cells by beta-2 adrenergic receptors: implications for hepatic metastasis. Cancer Lett. 2004;209(2):251–7.
Hasan M, Mohieldein A. Association between serum carcinoembryonic antigen level and oxidative stress parameters among diabetic females. Int J Clin Exp Med. 2015;8(4):6489–94.
Acknowledgements
Not applicable.
Funding
The study was funded by Social Development Projects of Nantong (MS22015065, MS12019019 and HS2020005), Medical Research Project of Nantong Health Commission (MB2019010 and MB2020029) and Medical Research Project of Jiangsu Health Commission (QNRC2016408).
Author information
Authors and Affiliations
Contributions
JbS and XqW initiated and acquired the funding for the series. ChW, CY and JbS designed the study. DmZ coordinated and supervised the study. CY, LZ, FX, LhZ, XhW, LyN and XlZ recruited the patients and collected the data. CY and JbS analysed the data and interpreted the results. ChW drafted the manuscript. All authors modified the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was reviewed and approved by the Ethics Committee of Affiliated Hospital 2 of Nantong University, and its conduction was in accordance with the Declaration of Helsinki. In addition, all participants provided informed consent when they were enrolled in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
ROC curve comparing the capability of serum CEA levels with that of HbA1c to discriminate DPN.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Ch., Yu, C., Zhuang, L. et al. High-normal serum carcinoembryonic antigen levels and increased risk of diabetic peripheral neuropathy in type 2 diabetes. Diabetol Metab Syndr 14, 142 (2022). https://doi.org/10.1186/s13098-022-00909-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00909-7