Abstract
Background
The enzyme 11-beta hydroxysteroid dehydrogenase type 1 (HSD11B1) converts inactive cortisone to active cortisol in a process mediated by the enzyme hexose-6-phosphate dehydrogenase (H6PD). The generation of cortisol from this reaction may increase intra-abdominal cortisol levels and contribute to the physiopathogenesis of obesity and metabolic syndrome (MetS). The relationship of HSD11B1 rs45487298 and H6PD rs6688832 polymorphisms with obesity and MetS was studied. We also studied how HSD11B1 abdominal subcutaneous (SAT) and visceral adipose tissue (VAT) gene expression is related to body fat distribution.
Methods
Rates of obesity and MetS features were cross-sectionally analyzed according to these polymorphisms in 1006 Brazilian white patients with type 2 diabetes (T2DM). Additionally, HSD11B1 expression was analyzed in VAT and SAT in a different cohort of 28 participants with and without obesity who underwent elective abdominal operations.
Results
Although polymorphisms of the two genes were not individually associated with MetS features, a synergistic effect was observed between both. Carriers of at least three minor alleles exhibited lower BMI compared to those with two or fewer minor alleles adjusting for gender and age (27.4 ± 4.9 vs. 29.3 ± 5.3 kg/m2; P = 0.005; mean ± SD). Obesity frequency was also lower in the first group (24.4% vs. 41.6%, OR = 0.43, 95% CI 0.21–0.87; P = 0.019). In the second cohort of 28 subjects, HSD11B1 gene expression in VAT was inversely correlated with BMI (r = − 0.435, P = 0.034), waist circumference (r = − 0.584, P = 0.003) and waist-to-height ratio (r = − 0.526, P = 0.010).
Conclusions
These polymorphisms might interact in the protection against obesity in T2DM individuals. Obese individuals may have decreased intra-abdominal VAT HSD11B1 gene expression resulting in decreasing intra-abdominal cortisol levels as a compensatory mechanism against central and general adiposity.
Similar content being viewed by others
Background
Obesity is a major public health problem causing a significant reduction in quality of life and life expectancy [1,2,3]. Obesity is one of the main components of the metabolic syndrome (MetS), which is characterized also by the co-occurrence of other well defined cardiovascular risk factors, including type 2 diabetes mellitus, atherogenic dyslipidemia and hypertension [4]. Weight gain promotes body fat accumulation, resulting in the activation of the inflammatory pathways, abnormal fat metabolism and the development of insulin resistance [5, 6]. The mechanisms behind this process are not clear, but in view of the similarities between individuals with Cushing’s syndrome and those with metabolic syndrome (MetS), it has been proposed that, despite normal levels of circulating cortisol, these phenotypes might arise as a consequence of tissue-specific cortisol excess due to increased activity of the enzyme 11-beta hydroxysteroid dehydrogenase type 1 (HSD11B1) [7].
Although HSD11B1 is a bidirectional enzyme in vitro, under normal circumstances it works as a reductase in the liver and adipose tissue, catalyzing the conversion of hormonally inactive cortisone into its active form, cortisol [8]. The activity of this enzyme is dependent on the provision of NADPH by the co-localized enzyme hexose-6-phosphate dehydrogenase (H6PD). In the absence of H6PD, HSD11B1 acts as a dehydrogenase, inactivating cortisol [9].
Patients with type 2 diabetes (T2DM) frequently present with obesity and visceral adiposity. Both diseases are considered among the most important determinants of a significant decrease of quality of life, cardiovascular disease and death. Transgenic mice overexpressing HSD11B1 develop visceral obesity and exhibited insulin-resistant diabetes and dyslipidemia [10], while HSD11B1-knockout mice are protected from the adverse metabolic complications of obesity and high fat diet-induced hyperglycemia [11]. Moreover, HSD11B1 inhibitors improve insulin sensitivity in mice [12]. We recently systematically reviewed the relationship among HSD11B1 abdominal adipose gene expression with obesity, T2DM and MetS in humans and reported that abdominal adipose HSD11B1 expression increased with increasing body mass index and abnormalities of glucose metabolism in most studies, but not in all, and varied with the presence of MetS. Variants of HSD11B1 were associated with the MetS and T2DM only in specific populations [13].
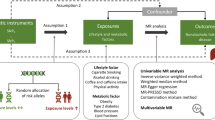
Because H6PD activity determines the directionality of HSD11B1 activity, we hypothesize that polymorphisms in the H6PD gene might influence the effects of HSD11B1 polymorphisms resulting in changes in gene expression related to adipose tissue metabolism, body fat distribution and the development of the MetS. Indeed, Draper et al. [14] reported that a combination of polymorphisms in the HSD11B1 (rs45487298:delA>insA) and H6PD (rs6688832:G>A) genes interacts to cause cortisone reductase deficiency. They proposed a digenic triallelic mode of inheritance in which at least three minor alleles from two loci are necessary for trait manifestation [14].
Therefore, in the present study we investigated the potential synergistic effect of HSD11B1 (rs45487298:delA>insA) and H6PD (rs6688832:G>A) polymorphisms on obesity and MetS-related characteristics in white T2DM individuals. We also investigated the relationship of HSD11B1 gene expression in abdominal subcutaneous (SAT) and visceral (VAT) adipose tissue with body fat distribution in individuals with and without MetS.
Methods
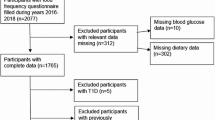
Participants
We performed a cross-sectional analysis of T2DM individuals who were participants of a multicenter study in Southern Brazil. This study started in 2002 with the aim of studying risk factors for T2DM and its complications. Ethnicity was mostly of European ancestry. A detailed description of this study can be found elsewhere [15]. T2DM was defined according to cut offs adopted by the American Diabetes Association (ADA).
The HSD11B1 (rs45487298:delA>insA) and H6PD (rs6688832:G>A) polymorphisms were analyzed in blood samples from 1006 white T2DM individuals and compared individually for the presence of MetS. Next, MetS rates were compared according to the presence of at least three minor alleles vs. two or fewer minor alleles of these polymorphic variants. HSD11B1 abdominal subcutaneous and visceral adipose tissue (SAT and VAT) gene expression was performed in other 28 participants with and without MetS and different degrees of glucose tolerance who underwent elective abdominal surgery. Paired samples of visceral and subcutaneous abdominal adipose tissue were collected during the procedure, cleaned with sodium chloride 0.9%, immediately frozen in liquid nitrogen and stored at − 80 °C.
The study protocol was approved by the ethics committees of the participating centers, and all individuals provided written informed consent. This study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki.
Clinical and anthropometric profiles and laboratory analyses
For both, the polymorphism and gene expression studies, a standard questionnaire was used to collect medical history, physical and laboratory evaluation to phenotype the study sample. For the gene expression study participants were additionally submitted to a 2-h 75-g oral glucose tolerance test with determination of plasma glucose every 30 min.
Participants were classified as having MetS using the new International Diabetes Federation criteria [16].
Serum samples were collected for laboratory testing after a 12-h fast. Glucose levels were determined using the glucose hexokinase method (Advia 1800 analyzer, Siemens Healthcare, Munich, Germany); glycated hemoglobin (A1c), by an ion-exchange HPLC procedure (Merck-Hitachi L-9100 analyzer, Darmstadt, Germany; reference range: 28–42 mmol/mol (4.7–6.0%); and total plasma cholesterol, HDL, and triglycerides, by enzymatic colorimetric methods (Advia 1800 analyzer, Siemens Healthcare, Munich, Germany). Low-density lipoprotein cholesterol (LDL) cholesterol was calculated using the Friedewald equation.
Genetic analyses
Polymorphism analyses
A total of 1006 individuals were recruited for this study. From this, 998 were genotyped for the HSD11B1 rs4548729883:delA>insA and 924 for the H6PD rs6688832:G>A. Genotyping success rate was 99.2% for HSD11B1 rs4548729883:delA>insA and 91.8% for H6PD rs6688832:G>A. The calculated allele frequency error rate based on PCR duplicates was 0%. The consensus rate was 91.1%. Amplification reactions were performed twice.
DNA was extracted from peripheral blood leukocytes and polymorphisms were determined using primers and probes contained in the Human Custom TaqMan Genotyping Assay 40× (Assays-By-Design Service, Life Technologies, Foster City, CA, USA) as following:
HSD11B1 rs4548729883:delA>insA: HSD11B1-5′-CTTACCTCCTCCTCTGAACTTTGC-3′ (forward primer), HSD11B1-5′-TCCTCCTGCAAGAGATGGCTATATT-3′ (reverse primer), HSD11B1-FAM-5′-CACCAAGAGCTTTT-3′, HSD11B1-VIC-5′-CACCAAAGAGCTTTT-3′.
H6PD rs6688832:G>A polymorphism: H6PD-5′-TCTGTCCGATTACTACGCCTACA-3′ (forward primer), H6PD-5′-GGCCATGGAAGATATGGGATAAGAG-3′ (reverse primer), H6PD-FAM-5′-CTGTGCGGGAGCG-3′, H6PD-VIC-5′-CCTGTGCAGGAGCG-3′.
Reactions were conducted in 96-well plates, in a total reaction volume of 5 µL, using 2 ng of genomic DNA, TaqMan Genotyping Master Mix 1× (Life Technologies, Foster City, CA, USA), and Custom TaqMan Genotyping Assay 1x. Plates were then placed in a real-time PCR thermal cycler (7500 Fast Real PCR System; Life Technologies, Foster City, CA, USA) and heated for 10 min at 95 °C, followed by 50 cycles of 95 °C for 15 s and 62 °C for 1 min. Fluorescence data files from each plate were analyzed using automated allele-calling software (SDS 2.1; Life Technologies, Foster City, CA, USA).
Gene expression study
RNA was extracted from adipose tissue using Trizol® reagent (Invitrogen; Life Technologies, Foster City, CA, USA). Concentration and quality of the product obtained was tested using the NanoDrop 2000 Spectrophotometer (Thermo Scientific Inc., Newark, USA). Only samples with suitable purity ratios (A260/A280 = 1.9–2.1) were used in subsequent analyses.
Real-Time reverse transcription PCR (RT-PCR) was performed in two separate steps: first, RNA was reverse transcribed into cDNA. Second, cDNA was amplified by quantitative RT-PCR (RT-qPCR). In this procedure, 1 μg of RNA was reverse transcribed to cDNA using the SuperScript® III First-Strand Synthesis System for RT-PCR (Invitrogen; Life Technologies, Foster City, CA, USA) following the manufacturer’s protocol for the oligo (dT)12–18 method. RT-qPCR experiments were performed in a 7500 Fast Real-Time PCR System Thermal Cycler with 7500 FAST Sequence Detection System Software (Life Technologies, Foster City, CA, USA) monitoring the increase in fluorescence of the SYBR® green dye [17]. Each sample was analyzed in triplicate and a negative control was added in each experiment.
Target and reference gene amplifications showed similar efficiencies in all experiments (E = 95% to 105%) allowing the use of this method. Primers for HSD11B1 (target gene) and β-actin (reference gene) were designed using the Primer Express 3.0 software (Life Technologies): HSD11B1: 5′-GCTGCCTTGCCCATGCT-3′ (forward primer), 5′-CAGCCAGAGAGGAGACGACAA-3′ (reverse primer); β-actin: 5′-GCGCGGCTACAGCTTCA-3′ (forward primer), 5′-CTTAATGTCACGCACGATTTCC-3′ (reverse primer).
RT-qPCR reactions were performed using 10 μL 2× Fast SYBR® Green Master Mix (Life Technologies, Foster City, CA, USA), 1 μL (1 ng/μL) of primers for HSD11B1 or β-actin, 1 μL (1 μg/μL) of cDNA, in a total volume of 20 μL. The reaction conditions were: initial cycle of 20 s at 95 °C, followed by 50 cycles at 95 °C for 3 s and 60 °C for 1 min. RT-qPCR specificity was determined using melting curve analyses and all primers generated amplicons that produced a single sharp peak during the analyses.
The measurement of HSD11B1 expression was performed by relative quantification using the comparative ΔΔCq method and expressed relative to the reference gene (β-actin) [18]. Validation tests were carried out by amplification of the target gene (HSD11B1) and the reference gene (β-actin), using serial dilutions of cDNA samples. The ΔΔCq method calculates changes in gene expression as relative fold changes (n-fold change) between the experimental sample and an external calibrator.
Statistical analyses
Results are expressed as means and standard deviations (SD), percentages, or median (interquartile range). Clinical and laboratory characteristics were compared using analysis of variance (ANOVA), the unpaired Student’s t test, Pearson’s correlation or χ2 as appropriate. Variables with skewed distribution were log-transformed. Bonferroni corrections were used to account for multiple comparisons. Departures from the Hardy–Weinberg equilibrium were verified using the Chi-square test (χ2). The relationship of HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A polymorphisms with different MetS-related components were tested by general linear model univariate analyses, adjusting for covariates.
Using the digenic triallelic mode of inheritance proposed by Draper et al. we analyzed the combined effect of at least three minor alleles of the HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A polymorphisms in modulating different MetS-related characteristics: systolic and diastolic BP, BMI, WC, HDL, and triglyceride levels [14]. Multiple logistic regression analysis was performed with the presence of obesity as the dependent variable and age, gender, and presence of at least three minor alleles of the two analyzed polymorphisms as independent variables.
It was calculated a sample size (WinPepi program, version 11.39, London, UK) of 15 subjects to compare the relationship between SAT and VAT HSD11B1 expression using a significance level of 5%, power of 90%, 1 to 1 proportion between insulin sensitive and resistant individuals based on the follow study [19].
All analyses were performed in the SPSS 18.0 (SPSS Inc., Chicago, USA). P < 0.05 was considered significant.
Results
Relationship between polymorphisms and MetS-related parameters
The 1006 T2DM included in the study were 58.4 ± 10.2 years old, 43.0% males, known T2DM duration of 11.6 ± 8.6 years, BMI 29.1 ± 5.2 kg/m2 (obesity = 40.3%), 63.6% had hypertension, and 76.3% had MetS. In the gene expression study 16.6% of subjects were lean, 25% were overweight and 58.4% were obese.
Of the 998 individuals genotyped for the HSD11B1 rs45487298:delA>insA polymorphism, 654 (65.5%) individuals were homozygous for the delA allele (delA/delA), 311 (31.2%) were heterozygous (delA/insA), and 33 (3.3%) were homozygous for the insA allele (insA/insA). Genotypes were in agreement with those predicted by Hardy–Weinberg equilibrium (P > 0.05). The insA allele frequency was 0.189. Table 1 summarizes the clinical and laboratory data of the individuals grouped according to the HSD11B1 rs45487298:delA>insA polymorphism. Systolic and diastolic BP, BMI, WC, total cholesterol, HDL, LDL, and triglyceride levels were not significantly different among the three genotypes. It bears mentioning that none of these variables exhibited significant differences when assuming dominant (insA/insA + insA/delA vs. delA/delA) or recessive (insA/insA vs. insA/delA + delA/delA) models of inheritance for the insA allele (data not shown).
Four-hundred and sixty-four (50.2%) individuals had the H6PD G/G genotype, 377 (40.8%) the A/G genotype, and 83 (9.0%) the A/A genotype of the rs6688832:G>A polymorphism. All genotypes were in Hardy–Weinberg equilibrium (P > 0.05), and the A allele frequency was 0.294. Table 2 illustrates the clinical and laboratory data of the individuals grouped according to the H6PD rs6688832:G>A polymorphism. This polymorphism had no statistically significant relationship with the MetS-related characteristics listed in Table 2. Furthermore, none of these variables exhibited significant differences when assuming dominant (A/A + G/A vs. G/G) or recessive (A/A vs. G/A + A/A) models of inheritance for the A allele (data not shown). Clinical and laboratory characteristics of T2DM individuals grouped according to the presence of at least three minor alleles of HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A polymorphisms are shown in Table 3. Taking into consideration a Bonferroni threshold of 0.0055 (P = 0.05 divided by 9 MetS-related features analyzed in Table 3), we observed that BMI was significantly lower in carriers of at least three minor alleles of the HSD11B1 and H6PD polymorphisms as compared to individuals with fewer than three minor alleles, adjusting for age and gender (P = 0.005). No significant gene–gene interaction was observed between the HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A polymorphisms in modulating other MetS-related features (Table 3). As expected, the frequency of obesity was lower among individuals carrying at least three minor alleles of HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A polymorphisms than in the group of individuals with fewer than three minor alleles (24.4% vs. 41.6%, respectively; P = 0.033). Logistic regression analysis, with adjustment for age and gender, confirmed that the presence of at least three minor alleles of both polymorphisms is an independent protection factor against obesity in patients with T2DM (OR = 0.43, 95% CI 0.21–0.87, P = 0.019).
None of the analyzed variables exhibited significant differences among individuals carrying at least two minor alleles of HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A polymorphisms and individuals with fewer than two minor alleles (data not shown). Furthermore, taking into account that only three individuals had four rs45487298:delA>insA and rs6688832:G>A minor alleles, it was not possible to evaluate if the protection to obesity could increase on those individuals carrying all minor alleles of the two genes.
Relationship between HSD11B1 gene expression in abdominal subcutaneous and visceral adipose tissue with anthropometric parameters
There were no difference in HSD11B1 abdominal SAT and VAT gene expressions between obese (BMI > 30 kg/m2) and non-obese individuals. Also there were no differences in HSD11B1 abdominal SAT and VAT gene expressions between patients with and without MetS (Table 4).
HSD11B1 SAT expression was not related with BMI, waist circumference, and waist-to-height ratio (Table 5). In contrast VAT expression was inversely related to all of these parameters (adjusting for age and gender). In order to better understand these relationships, we stratified the sample by body size and MetS presence. HSD11B1 VAT but not SAT expression was inversely related to BMI, WC and WHtR in participants with BMI ≥ 30 kg/m2. However, both VAT and SAT expression were not related to these parameters in those with BMI < 30 kg/m2. When stratifying the study sample by the presence of MetS, HSD11B1 VAT expression was inversely related to all these anthropometric parameters, being statistically significant only for WC and WHtR in the MetS+ group. Although there was a trend towards SAT expression to be related to BMI, WC and WHtR in those without the MetS, it did not reach statistical significance. For MetS participants, SAT expression was not related to these anthropometric parameters (Table 5).
Discussion
This study investigated the association of the HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A polymorphisms with MetS-related characteristics in white subjects with T2DM. When independently analyzed, neither of these two polymorphisms was associated with any feature of MetS. However, when analyzing the rs45487298:delA>insA and rs6688832:G>A polymorphisms in combination, we observed a significant gene–gene interaction modulating the risk of obesity in T2DM individuals carrying at least three minor alleles of the two polymorphisms.
There is compelling biochemical evidence of cooperativity between H6PD and HSD11B1 enzymes [9, 20]. Lavery et al. [21] showed that H6PD knockout mice have a profound switch in HSD11B1 activity from oxoreductase to dehydrogenase, increasing corticosterone clearance and resulting in a reduction in circulating corticosterone levels. This demonstrates a critical requirement of H6PD for HSD11B1 oxoreductase activity.
The effect of this interaction has been previously associated with risk of cortisone reductase deficiency [14]. As suggested by Draper et al. [14], this interaction might occur because both rs45487298:delA>insA and rs6688832:G>A polymorphisms seem to have functional effects. The rs45487298:delA>insA polymorphism is located in an enhancer region of intron 3 of the HSD11B1 gene. It has been associated with decreased HSD11B1 expression in vivo and after transfection of minigene constructs in cultured cells [14]. Draper et al. [14] also reported that in cell cultures the rs6688832:G>A polymorphism in the H6PD gene decreased the enzyme activity to less than 50% of normal, impairing the generation of reduced NADPH and, consequently, reducing HSD11B1 activity. Nevertheless, Lavery et al. have not found a reduction in H6PD enzyme activity by the rs6688832:G>A variant [22].
Previous studies have suggested an association between different HSD11B1 gene polymorphisms and MetS features [23,24,25,26,27]. The rs45487298:delA>insA polymorphism was associated with higher BMI, altered body composition and insulin resistance in obese US children [25]. Nair et al. [26] reported an association between the rs846910:G>A and rs12086634:A>G polymorphisms in the HSD11B1 gene and risk of T2DM in Pima Indians. Devang et al. also revealed that the HSD11B1 rs846910 AG contributed to an increased risk of T2D in South Indians. The authors also indicated that HSD11B1 rs12086634 TG contributed to an increased risk of both T2D and MetS [27]. Gandhi et al. detected a significant association between the HSD11B1 gene polymorphism (rs12086634) and occurrence of MetS compared to controls [28].
In contrast, other studies showed no association between HSD11B1 gene polymorphisms and body composition, glucose metabolism or MetS [13]. White et al. [29] did not find any association between HSD11B1 rs12086634:T>G and H6PD rs6688832:G>A polymorphisms (either separately or in combination) and BMI, waist-to-hip ratio, visceral adiposity, measures of insulin sensitivity or risk of polycystic ovary syndrome (PCOS) in a population-based sample from the Dallas Heart Study. Furthermore, Draper et al. [30] showed no association of the HSD11B1 rs12086634 variant (which is in complete linkage disequilibrium with the rs45487298:delA>insA variant) and H6PD rs6688832 variant with susceptibility to BMI and waist-to-hip ratio in a UK study with 213 women with PCOS and 549 controls.
Recently, Moon et al. reported that HSD11B1 rs12086634:A>G and rs1000283:C>T polymorphisms were associated with MetS in T2DM individuals, while the H6PD rs17368528:C>T polymorphism was a risk factor for MetS in non-diabetic South Koreans [31]. However, differently from what we found in our study, no significant association of these SNPs with type 2 diabetes and metabolic syndrome was found after considering the multiple comparisons in the total study population. Therefore, HSD11B1 and H6PD polymorphisms analyzed individually may not be associated with type 2 diabetes and MetS.
The inconsistent results reported by the studies cited herein may be at least partly explained by differences in study designs, sample sizes, ethnicity, and analyzed HSD11B1 polymorphisms. Moreover, a number of studies analyzed only the expression of polymorphisms of the HSD11B1 gene. Thus, such studies may not have observed associations of the interaction of HSD11B1 gene polymorphisms to certain H6PD polymorphisms with MetS-related characteristics. There might also be additional polymorphisms in these two genes that were not identified in previous studies, but could have major effects on HSD11B1 gene expression or enzyme activity.
Despite inconsistent results regarding associations between HSD11B1 gene polymorphisms and MetS-related characteristics, a compelling evidence base argues for HSD11B1 as a major etiological factor in obesity and related features [9, 32, 33]. In addition, modulation of HSD11B1 activity has also an effect on multiple target tissues which promote insulin resistance independently of obesity. For example, in lean glucose-intolerant individuals, adipose HSD11B1 activity is not increased and hepatic HSD11B1 activity is maintained [34] compared with the downregulation of hepatic HSD11B1 that occurs in obesity [35]. Inhibition of HSD11B1 with oral carbenoxolone enhances hepatic insulin sensitivity [36], and has a greater effect in non-obese glucose-intolerant participants than in healthy people [37]. Moreover, the expression of HSD11B1 in myoblast cultures stimulated with glucocorticoids was negatively correlated with insulin sensitivity [38]. Consequently, HSD11B1 is a promising target for pharmacological inhibition in individuals with T2DM and/or MetS [9].
In this context, overexpression of the HSD11B1 gene might determine an increase in cortisol generation and, secondarily, generate pro-obesity effects. Therefore, we hypothesize that the interaction between HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A polymorphisms may generate a significant decrease in HSD11B1 levels in adipocytes and other tissues; and consequently, this may decrease the risk of obesity in individuals with T2DM who carry at least three minor alleles of these polymorphisms. However, taking into account the controversial functional studies regarding the H6PD rs6688832:G>A effect on H6PD activity [14, 22], it seems possible that this polymorphism might be only a neutral polymorphic variant in linkage disequilibrium with an unknown causative mutation to be found elsewhere in the H6PD gene. In addition, in view that has been previously shown differences in regulation of glucocorticoid activity in individuals with and without impaired glucose tolerance [39,40,41], the present data should be interpreted with caution when translated to non-glucose-tolerant obese participants.
Data of HSD11B1 gene expression and its association with anthropometric parameters are conflicting due to the large difference between the studied populations. Studies performed in participants without MetS have shown that HSD11B1 abdominal adipose tissue expression is positively related with BMI and measurements of central adiposity such as waist circumference [42, 43] whereas HSD11B1 gene expression was not related or inversed related to anthropometric parameters in participants with MetS [38, 44].
While we found no relationships of HSD11B1 gene expression in abdominal SAT with measurements of adiposity distribution, namely BMI, WC and WHtR, the expression of this gene in abdominal VAT was inversely and significantly related to these parameters. When stratifying the sample either by the presence of obesity or MetS, in both groups we have found an inverse relationship between abdominal adipose tissue HSD11B1 gene expression and BMI, but this relationship remained significant only in those with obesity. Lutz et al. investigated the expression of nine different polymorphisms for the HSD11B1 gene in a total of 327 German patients [45]. The major C allele of rs2235543 and the major G allele of rs12565406 were significantly associated with increased VAT mass. It would be interesting to have analyzed these polymorphic variants in participants of our sample in which adipose tissue gene expression was studied. However, due to the low frequency of the minor allele of HSD11B1 in the polymorphism study sample (0.33% of homozygozity), it would be unlikely to have enough number of subjects identified as having this allelic combination in the 28 participants which were studied in our gene expression cohort. As a result, even with a common direction of the polymorphism and gene expression studies, we believed that would be interesting to have a future studied in which polymorphism and gene expression analysis will be performed in the same subjects of a larger sample size population, what we, unfortunately, were not able to do it.
The results of the present study suggest that HSD11B1 abdominal adipose tissue expression in participants with obesity and/or MetS decreases in order to compensate increased HSD11B1 activity. Although we did not tested this hypothesis, we believe this may explain in part why T2DM participants carrying at least three minor alleles of HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A exhibit lower BMI than those carrying fewer than three minor alleles.
Conclusions
We have shown that the HSD11B1 rs45487298:delA>insA and H6PD rs6688832:G>A polymorphisms might interact in protecting against obesity in T2DM individuals. Further research is required to provide functional analyses of the effects of these polymorphisms on the pathogenesis of obesity and MetS, and to confirm this result in other populations. Since HSD11B1 inhibition is now recognized as a promising pathway for pharmacological treatment of obesity, T2DM and MetS, our results might have an importance in future pharmacogenetics studies regarding the clinical testing of genetic variations that could give rise to different responses to HSD11B1 inhibitors.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANOVA:
-
analysis of variance
- A1c:
-
glycated hemoglobin
- HPLC:
-
high-performance liquid chromatography
- HSD11B1:
-
11-beta hydrosteroid dehydrogenase type 1
- H6PD:
-
glucose-6-phosphate dehydrogenase
- LDL:
-
low-density lipoprotein cholesterol cholesterol
- MetS:
-
metabolic syndrome
- NADPH:
-
nicotinamide adenine dinucleotide phosphate
- RT-qPCR:
-
quantitative RT-PCR
- SAT:
-
subcutaneous abdominal tissue
- SD:
-
standard deviations
- T2DM:
-
type 2 diabetes
- VAT:
-
visceral abdominal tissue
References
Vidra N, Trias-Llimos S, Janssen F. Impact of obesity on life expectancy among different European countries: secondary analysis of population-level data over the 1975–2012 period. BMJ Open. 2019;9:e028086.
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187–93.
DALYs GBD, Collaborators H. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–922.
Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006;119:812–9.
Antoniolli LP, Nedel BL, Pazinato TC, de Andrade Mesquita L, Gerchman F. Accuracy of insulin resistance indices for metabolic syndrome: a cross-sectional study in adults. Diabetol Metab Syndr. 2018;10:65.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6.
Stimson RH, Walker BR. Glucocorticoids and 11beta-hydroxysteroid dehydrogenase type 1 in obesity and the metabolic syndrome. Minerva Endocrinol. 2007;32:141–59.
Tomlinson JW, Walker EA, Bujalska IJ, Draper N, Lavery GG, Cooper MS, et al. 11beta-hydroxysteroid dehydrogenase type 1: a tissue-specific regulator of glucocorticoid response. Endocr Rev. 2004;25:831–66.
Morton NM. Obesity and corticosteroids: 11beta-hydroxysteroid type 1 as a cause and therapeutic target in metabolic disease. Mol Cell Endocrinol. 2010;316:154–64.
Masuzaki H, Paterson J, Shinyama H, Morton NM, Mullins JJ, Seckl JR, et al. A transgenic model of visceral obesity and the metabolic syndrome. Science. 2001;294:2166–70.
Kotelevtsev Y, Holmes MC, Burchell A, Houston PM, Schmoll D, Jamieson P, et al. 11beta-hydroxysteroid dehydrogenase type 1 knockout mice show attenuated glucocorticoid-inducible responses and resist hyperglycemia on obesity or stress. Proc Natl Acad Sci USA. 1997;94:14924–9.
Alberts P, Nilsson C, Selen G, Engblom LO, Edling NH, Norling S, et al. Selective inhibition of 11 beta-hydroxysteroid dehydrogenase type 1 improves hepatic insulin sensitivity in hyperglycemic mice strains. Endocrinology. 2003;144:4755–62.
do Nascimento FV, Piccoli V, Beer MA, von Frankenberg AD, Crispim D, Gerchman F. Association of HSD11B1 polymorphic variants and adipose tissue gene expression with metabolic syndrome, obesity and type 2 diabetes mellitus: a systematic review. Diabetol Metab Syndr. 2015;7:38.
Draper N, Walker EA, Bujalska IJ, Tomlinson JW, Chalder SM, Arlt W, et al. Mutations in the genes encoding 11beta-hydroxysteroid dehydrogenase type 1 and hexose-6-phosphate dehydrogenase interact to cause cortisone reductase deficiency. Nat Genet. 2003;34:434–9.
Canani L, Capp C, Ng D, Choo S, Maia A, Nabinger G, et al. The fatty acid-binding protein-2 A54T polymorphism is associated with renal disease in patients with type 2 diabetes. Diabetes. 2005;54:3326–30.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Higuchi R, Fockler C, Dollinger G, Watson R. Kinetic PCR analysis: real-time monitoring of DNA amplification reactions. Biotechnology. 1993;11:1026–30.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) method. Methods. 2001;25:402–8.
Yao-Borengasser A, Varma V, Bodles AM, Rasouli N, Phanavanh B, Lee MJ, et al. Retinol binding protein 4 expression in humans: relationship to insulin resistance, inflammation, and response to pioglitazone. J Clin Endocrinol Metab. 2007;92:2590–7.
Banhegyi G, Benedetti A, Fulceri R, Senesi S. Cooperativity between 11beta-hydroxysteroid dehydrogenase type 1 and hexose-6-phosphate dehydrogenase in the lumen of the endoplasmic reticulum. J Biol Chem. 2004;279:27017–21.
Lavery GG, Walker EA, Draper N, Jeyasuria P, Marcos J, Shackleton CH, et al. Hexose-6-phosphate dehydrogenase knock-out mice lack 11 beta-hydroxysteroid dehydrogenase type 1-mediated glucocorticoid generation. J Biol Chem. 2006;281:6546–51.
Lavery GG, Walker EA, Tiganescu A, Ride JP, Shackleton CH, Tomlinson JW, et al. Steroid biomarkers and genetic studies reveal inactivating mutations in hexose-6-phosphate dehydrogenase in patients with cortisone reductase deficiency. J Clin Endocrinol Metab. 2008;93:3827–32.
Franks PW, Knowler WC, Nair S, Koska J, Lee YH, Lindsay RS, et al. Interaction between an 11betaHSD1 gene variant and birth era modifies the risk of hypertension in Pima Indians. Hypertension. 2004;44:681–8.
Morales MA, Carvajal CA, Ortiz E, Mosso LM, Artigas RA, Owen GI, et al. Possible pathogenetic role of 11 beta-hydroxysteroid dehydrogenase type 1 (11betaHSD1) gene polymorphisms in arterial hypertension. Rev Med Chil. 2008;136:701–10.
Gelernter-Yaniv L, Feng N, Sebring NG, Hochberg Z, Yanovski JA. Associations between a polymorphism in the 11 beta hydroxysteroid dehydrogenase type I gene and body composition. Int J Obes Relat Metab Disord. 2003;27:983–6.
Nair S, Lee YH, Lindsay RS, Walker BR, Tataranni PA, Bogardus C, et al. 11beta-Hydroxysteroid dehydrogenase type 1: genetic polymorphisms are associated with Type 2 diabetes in Pima Indians independently of obesity and expression in adipocyte and muscle. Diabetologia. 2004;47:1088–95.
Devang N, Satyamoorthy K, Rai PS, Nandini M, Rao S, Phani NM, Adhikari P. Association of HSD11B1 gene polymorphisms with type 2 diabetes and metabolic syndrome in South Indian population. Diabetes Res Clin Pract. 2017;131:142–8.
Gandhi K, Adhikari P, Basu A, Achappa B. Association between a 11β-hydroxysteroid dehydrogenase type 1 gene polymorphism and metabolic syndrome in a South Indian population. Metab Syndr Relat Disord. 2013;11:397–402.
White PC. Genotypes at 11beta-hydroxysteroid dehydrogenase type 11B1 and hexose-6-phosphate dehydrogenase loci are not risk factors for apparent cortisone reductase deficiency in a large population-based sample. J Clin Endocrinol Metab. 2005;90:5880–3.
Draper N, Powell BL, Franks S, Conway GS, Stewart PM, McCarthy MI. Variants implicated in cortisone reductase deficiency do not contribute to susceptibility to common forms of polycystic ovary syndrome. Clin Endocrinol. 2006;65:64–70.
Moon SS, Lee YS, Kim JG, Kim SW, Jeong JY, Jeon EJ, et al. Relationship of 11beta-hydroxysteroid dehydrogenase type 1 and hexose-6-phosphate dehydrogenase gene polymorphisms with metabolic syndrome and type 2 diabetes. Endocr J. 2011;58:949–59.
Tomlinson JW, Stewart PM. Mechanisms of disease: selective inhibition of 11beta-hydroxysteroid dehydrogenase type 1 as a novel treatment for the metabolic syndrome. Nat Clin Pract Endocrinol Metab. 2005;1:92–9.
Staab CA, Maser E. 11beta-Hydroxysteroid dehydrogenase type 1 is an important regulator at the interface of obesity and inflammation. J Steroid Biochem Mol Biol. 2010;119:56–72.
Andrews RC, Herlihy O, Livingstone DE, Andrew R, Walker BR. Abnormal cortisol metabolism and tissue sensitivity to cortisol in patients with glucose intolerance. J Clin Endocrinol Metab. 2002;87:5587–93.
Stewart PM, Boulton A, Kumar S, Clark PM, Shackleton CH. Cortisol metabolism in human obesity: impaired cortisone⟶ cortisol conversion in subjects with central adiposity. J Clin Endocrinol Metab. 1999;84:1022–7.
Walker BR, Connacher AA, Lindsay RM, Webb DJ, Edwards CR. Carbenoxolone increases hepatic insulin sensitivity in man: a novel role for 11-oxosteroid reductase in enhancing glucocorticoid receptor activation. J Clin Endocrinol Metab. 1995;80:3155–9.
Andrews RC, Rooyackers O, Walker BR. Effects of the 11 beta-hydroxysteroid dehydrogenase inhibitor carbenoxolone on insulin sensitivity in men with type 2 diabetes. J Clin Endocrinol Metab. 2003;88:285–91.
Whorwood CB, Donovan SJ, Flanagan D, Phillips DI, Byrne CD. Increased glucocorticoid receptor expression in human skeletal muscle cells may contribute to the pathogenesis of the metabolic syndrome. Diabetes. 2002;51:1066–75.
Ruan LL, Xu J, Wang CL, Zou CC. Variants of 11β-hydroxysteroid dehydrogenase (HSD11B) gene type 1 and 2 in Chinese obese adolescents. J Endocrinol Investig. 2014;37:565–73.
Karlsson C, Jernas M, Olsson B, Lystig T, Gummesson A, Storlien L, et al. Differences in associations between HSD11B1 gene expression and metabolic parameters in subjects with and without impaired glucose homeostasis. Diabetes Res Clin Pract. 2010;88:252–8.
Jang C, Obeyesekere VR, Dilley RJ, Krozowski Z, Inder WJ, Alford FP. Altered activity of 11beta-hydroxysteroid dehydrogenase types 1 and 2 in skeletal muscle confers metabolic protection in subjects with type 2 diabetes. J Clin Endocrinol Metab. 2007;92:3314–20.
Paulsen SK, Pedersen SB, Fisker S, Richelsen B. 11Beta-HSD type 1 expression in human adipose tissue: impact of gender, obesity, and fat localization. Obesity. 2007;15:1954–60.
Michailidou Z, Jensen MD, Dumesic DA, Chapman KE, Seckl JR, Walker BR, et al. Omental 11beta-hydroxysteroid dehydrogenase 1 correlates with fat cell size independently of obesity. Obesity. 2007;15:1155–63.
Tomlinson JW, Sinha B, Bujalska I, Hewison M, Stewart PM. Expression of 11beta-hydroxysteroid dehydrogenase type 1 in adipose tissue is not increased in human obesity. J Clin Endocrinol Metab. 2002;87:5630–5.
Lutz SZ, Peter A, Machicao F, et al. Genetic variation in the 11β-hydroxysteroid-dehydrogenase 1 gene determines NAFLD and visceral obesity. J Clin Endocrinol Metab. 2016;101:4743–51.
Acknowledgements
We would like to thank Prof. Jorge L. Gross (in memoriam) for his contribution in the concept of this study.
Funding
This work was supported by the Brazilian National Research Council [CNPq 486802/2013-2] and FIPE-Hospital de Clinicas de Porto Alegre [09-407], Brazil.
Author information
Authors and Affiliations
Contributions
FVN, MFC and FG reviewed the literature and wrote the manuscript. FSO, BMS and CRPK, RRG, LHC, and DC coassisted in researching the data and reviewed the manuscript. FG and MFC discussed the results with all others, and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chedid, M.F., do Nascimento, F.V., de Oliveira, F.S. et al. Interaction of HSD11B1 and H6PD polymorphisms in subjects with type 2 diabetes are protective factors against obesity: a cross-sectional study. Diabetol Metab Syndr 11, 78 (2019). https://doi.org/10.1186/s13098-019-0474-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-019-0474-2