Abstract
Objectives
The purpose of this study is to provide expert consensus recommendations to establish a global ultrasound curriculum for undergraduate medical students.
Methods
64 multi-disciplinary ultrasound experts from 16 countries, 50 multi-disciplinary ultrasound consultants, and 21 medical students and residents contributed to these recommendations. A modified Delphi consensus method was used that included a systematic literature search, evaluation of the quality of literature by the GRADE system, and the RAND appropriateness method for panel judgment and consensus decisions. The process included four in-person international discussion sessions and two rounds of online voting.
Results
A total of 332 consensus conference statements in four curricular domains were considered: (1) curricular scope (4 statements), (2) curricular rationale (10 statements), (3) curricular characteristics (14 statements), and (4) curricular content (304 statements). Of these 332 statements, 145 were recommended, 126 were strongly recommended, and 61 were not recommended. Important aspects of an undergraduate ultrasound curriculum identified include curricular integration across the basic and clinical sciences and a competency and entrustable professional activity-based model. The curriculum should form the foundation of a life-long continuum of ultrasound education that prepares students for advanced training and patient care. In addition, the curriculum should complement and support the medical school curriculum as a whole with enhanced understanding of anatomy, physiology, pathophysiological processes and clinical practice without displacing other important undergraduate learning. The content of the curriculum should be appropriate for the medical student level of training, evidence and expert opinion based, and include ongoing collaborative research and development to ensure optimum educational value and patient care.
Conclusions
The international consensus conference has provided the first comprehensive document of recommendations for a basic ultrasound curriculum. The document reflects the opinion of a diverse and representative group of international expert ultrasound practitioners, educators, and learners. These recommendations can standardize undergraduate medical student ultrasound education while serving as a basis for additional research in medical education and the application of ultrasound in clinical practice.
Similar content being viewed by others
Introduction
The use of ultrasound in medical student (undergraduate) education first appeared in the literature in the 1990s. Early studies from Europe reported enhanced learning of cardiac physiology and human gross anatomy with ultrasound [1, 2]. Since that time, ultrasound as a teaching tool has steadily expanded for both the basic and clinical sciences.
Much of this expansion has been driven by the clinical use of ultrasound at the bedside referred to as point-of-care ultrasound or POCUS. In POCUS, the treating clinician performs ultrasound examinations and interprets the ultrasound images at the bedside to assist with immediate diagnostic and patient management decisions as well as to assist in guiding procedures such as vascular access. The number and diversity of ultrasound clinical applications have grown significantly over the past three decades and ultrasound is now used in almost every practice specialty and subspecialty from primary care to transplant surgery [3, 4].
Most recently, there has been an exponential increase in interest in ultrasound education in medical school as evidenced by the number of ultrasound education-related publications (Fig. 1). Contributing to this rapid rise in interest have been advances in ultrasound technology such as artificial intelligence-assisted image display and automated functions such as computation of the cardiac ejection fraction. These advances have resulted in easier to use hand-held and laptop-sized ultrasound devices with high-quality images. Newer devices are also much more affordable than the previous portable ultrasound machines that initiated the POCUS era. These changes in ease of use, quality of images, functionality, and cost have made teaching large numbers of medical students with ultrasound much more feasible.
Ultrasound education after medical school (postgraduate or residency), outside the traditional ultrasound-use specialties of radiology, cardiology and obstetrics and gynecology, began in the 1990s in the specialties of Emergency Medicine and Critical Care Medicine. Ultrasound leaders in these two specialties have created extensive point-of-care educational resources, have developed postgraduate training competencies and milestones, and have established ultrasound fellowships for advanced training of clinicians, educators, and researchers [5,6,7,8,9,10,11,12]. These contributions have been critical to developing practice standards for the appropriate and safe use of POCUS and the expansion of ultrasound to other specialties and subspecialties.
Because of the broad range of ultrasound applications, mounting evidence of the clinical value of point-of-care ultrasound, the availability of educational resources, and the advances in ultrasound technology, many specialties and subspecialties have been incorporating and/or expanding the role of ultrasound in their postgraduate training programs [13,14,15,16,17]. Postgraduate ultrasound education publications like those in undergraduate education are showing an exponential rise, as depicted in Fig. 2.
Thus, a continuum of ultrasound education is evolving, beginning in undergraduate medical education. Necessary and central to the success of such an educational continuum will be the establishment of foundational ultrasound knowledge, attitude, and skills for the definition of basic ultrasound competencies with attendant milestones and assessment. To this end, the Society of Ultrasound in Medical Education (SUSME) and the World Interactive Network Focused on Critical Ultrasound (WINFOCUS) conducted this international conference to provide consensus recommendations for developing a global ultrasound curriculum for undergraduate medical education. Such recommendations will serve as the basis for establishing ultrasound as a core clinical competency for all medical school graduates and prepare these graduates for future advanced clinical training.
Four domains of statements related to medical student ultrasound education were addressed: the scope of an international consensus ultrasound curriculum, the rationale for the curriculum, the characteristics of the curriculum, and curricular content. This last domain was of particular importance as the lack of standardized content for ultrasound education has been a significant obstacle to the broad adoption of ultrasound in medical student education [18,19,20]. Such standardization is necessary to facilitate faculty development as well as promote ultrasound educational and clinical research to further develop evidence that guides the use of ultrasound in medical education and clinical practice [21,22,23].
A modified Delphi consensus method was used that included a systematic search of the literature, the GRADE method of assessment of level of quality of evidence, and RAND appropriateness methodology for the degree of consensus and strength of recommendations. Even though the number of publications on ultrasound education is relatively large, those of high-quality evidence-based studies are still quite limited. Thus, it was anticipated that this international consensus conference would need to rely heavily on expert opinion in establishing the most appropriate ultrasound content for medical student education. A large diverse group of expert ultrasound practitioners, researchers, and educators was recruited to participate in the process to enhance the validity of the consensus and ensure the best recommendations were achieved.
Overall, the consensus process involved expert voting panelists and expert consultants, along with the education stakeholders of medical students and residents. This broad group of participants was designed to capture consensus recommendations applicable across educational settings with variable curricular structures, needs, and resources, as well as to address several limitations of previous papers on ultrasound curricular content for medical students. These prior publications were usually limited by medical specialty or discipline representation and the breadth of their institutional applicability and accreditation standards. Recommendations on methods of teaching ultrasound and student assessment were beyond the scope of this consensus conference.
Methods
Literature search
Initial PubMed literature searches were conducted in 2016 and 2017 using the following query: ((("medical students"[TIAB] OR "medical education"[TIAB]) OR "education, medical"[MeSH Terms]) OR "students, medical"[MeSH Terms]) AND ((("ultrasonics"[MeSH Terms] OR "ultrasonography"[MeSH Terms]) OR "ultrasound"[TIAB]) OR "ultrasonography"[TIAB] OR "ultrasonics"[TIAB]) AND (("1997/01/01"[PDat]: "3000/12/31"[PDat])).
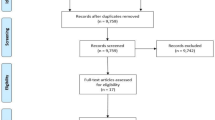
The search resulted in the identification of 1832 records. These records were then limited to English only and 20 years resulting in 1556 records. These records were then reviewed in duplicate by two steering committee members with inclusion and exclusion criteria to identify all records relative to medical student ultrasound education resulting in 275 records.
In addition to the primary PubMed searches, secondary parallel searches were performed in the following databases: Academic Search (68 records), CINAHL (58 records), Cochrane Library (3 records), ERIC (6 records), PsychINFO (11 records), and Web of Science (544 records).
The records from the secondary searches were compared to the initial PubMed record list and duplications were removed. These records were screened for relevancy and added to records recommended by the Domain leaders from literature searched through 2018. A total of 283 records were used for the consensus process as shown in Fig. 3. Search results were made available to all consensus conference participants on a central International Consensus Conference on Ultrasound in Medical Education website with other consensus resources such as published ultrasound standards and guidelines, community forums, updated searches, and links to other relevant sites. The website remained active throughout the entire consensus conference process.
Consensus conference steering committee, domains, and domain task teams
A consensus conference steering committee of eight members knowledgeable in ultrasound, education, and consensus processes was formed to guide the consensus process. Four of the members represented the Society of Ultrasound in Medical Education (SUSME) and four represented the World Interactive Network Focused on Critical Ultrasound (WINFOCUS). Six different specialties and subspecialties from four countries were represented on the steering committee. One member of the steering committee had advanced training in epidemiology with expertise in consensus methodology and oversaw the methodology of the process. The steering committee agreed on four general topics or domains of ultrasound in medical education to develop essential statements and consensus recommendations. These included Domain 1: Scope of the International Consensus Curriculum; Domain 2: Rationale for the Curriculum; Domain 3: Characteristics of the Curriculum; and Domain 4: Curricular Content.
Four domain task teams were formed with co-chairs to further evaluate the subject matter within their domain, identify additional literature, and develop relevant PICO consensus statements (population, intervention, comparison of intervention, outcomes) for Domains 1–3 and curricular content items for Domain 4. Discussion and editing of the domains among panelists and consultants took place at four international meetings on ultrasound (World Congress on Ultrasound in Medical Education in Lubbock, TX, September 2016, World Congress on Ultrasound in Medical Education in Montreal, Canada, October 2017, WINFOCUS World Congress on Ultrasound in Emergency and Critical Care in Dubai, United Arab Emirates, February 2019, and World Congress on Ultrasound in Medical Education in Irvine, CA, September 2019).
The individual curricular content items of Domain 4 were initially determined by a task team of eight expert ultrasound practitioners and educators with input from steering committee members. Content items were further discussed during the international ultrasound meetings. These content items were identified from the ultrasound literature and published ultrasound guidelines, but in general lacked evidence documenting their educational value per se. Thus, the content list was created to suggest content that could be of value to medical student education; the final recommendations on content were made by the expert voting panel consensus.
Voting panelists, consultants, and medical student/resident stakeholders
Nationally and internationally recognized clinicians, basic scientists, educators and researchers were invited to participate in the consensus process either as voting panelists or consultants based on their area of ultrasound expertise, clinical experience, educational experience, record of publications, and leadership positions in professional societies, hospital systems, and/or academia. All voting panelists and consultants completed a professional profile form and submitted a curriculum vitae and a declaration of interest/conflict of interest form for consideration.
Voting panelists
Voting panelists were selected to provide representation across clinical specialties and subspecialties, basic science expertise, geographic distribution, educational experience, and familiarity with the various medical education systems throughout the world. Broad yet balanced representation was sought to strengthen the validity of the consensus process for an integrated ultrasound curriculum that would span the basic and clinical sciences of medical student education and prepare medical students to pursue postgraduate medical education training in any specialty or subspecialty they should choose and within a variety of global medical educational systems.
As summarized in Table 1, the voting panelists represented a diverse group of educators and practitioners with a wide range of areas of expertise and experience, including over 20 medical and surgical specialties, adult and pediatric expertise, two foundational basic science disciplines, and non-physician ultrasound practitioners. Sixteen nations were represented (Table 2). When possible, voting panelists within the same specialty were chosen to cover a spectrum of ultrasound interests or primary foci in an attempt to balance areas of ultrasound expertise (i.e., radiology—general, vascular, musculoskeletal, dermatology).
The total number of panelist specialties, subspecialties, and area of special expertise exceeds the total individual panelists number of 64 since a number of panelists were formally trained, practiced, and taught in more than one area of ultrasound.
As a group, voting panelists accounted for many contributions to the ultrasound literature. Panelists had published an average of 32.7 peer-reviewed publications and 7.1 ultrasound book chapters. Thirty-one panelists had served as an ultrasound book editor. All panelists had been involved in national and international ultrasound societies and 86.6% had held leadership positions in these organizations.
Over 90% of panelists had greater than 5 years of experience in teaching medical students (93.7%), postgraduate residents (94.6%) and practicing physicians (96.4%). Many panelists had greater than 15 years of ultrasound teaching experience and had served as ultrasound education directors in their academic institutions and/or clinical ultrasound training program (83.3%). Eighty percent had greater than 5 years of experience teaching other healthcare providers such as nurses, nurse practitioners, physician assistants, and midwives. Eighty-eight percent of the panelists had been involved in ultrasound research for greater than 5 years.
Consultants
The credentials of the consultants were very similar to those of the voting panelists. The consultants were involved in discussions of the statements and recommendations. The consultants participated in a preliminary voting survey of Round 1 statements and recommendations. The results of the consultants’ survey were then made available to the voting panelists for consideration. Fifty consultants participated in the preliminary Round 1 voting. The decision to include participants as voting panelists or consultants was made on the time individuals had to commit to the process, the need for representative balance in specialty, subspecialty, and science discipline as well as level of expertise and geographical representation.
Medical students and residents
Medical students and residents as stakeholders in their education were given opportunities to provide input through online communities (Disqus) and complete a preliminary Round 1 survey. The results of this survey were made available to the voting panelists for consideration. Medical students and residents who participated were identified through various global medical student ultrasound interest groups and chief resident listings. No systematic attempt was made to seek a balanced representation of students and residents. Therefore, their input should be considered as that of a sample based on interest and convenience. Twenty-one students and residents participated in the preliminary voting and their responses were pooled together.
Voting and evaluations of recommendations
A modified Delphi method was used for two rounds of voting. The level of quality of evidence was determined by the GRADE method and the RAND appropriateness method was used for the degree of consensus and strength of recommendations [24, 25]. Voting was done anonymously. Levels of quality of evidence for literature supporting a statement were rated as: Level 1 (high), Level 2A (moderate), Level 2B (low), Level 3 (very low). A nine-point Likert scale of appropriateness for each PICO statement was used with 1–3 denoting inappropriate, 4–6 denoting somewhat appropriate, and 7–9 denoting appropriate. Using RAND Rules to determine whether a statement was recommended, strongly recommended, or not recommended included an assessment of the median level of appropriateness, the degree of consensus, and the percentage of disagreement of the voters.
During the consensus process, voting was accomplished using online customized forms. Voters were sent the voting link and allowed approximately 2 weeks to complete the surveys. Reminders were sent during the open voting period. Participants could complete the survey at one time or could return to complete the survey as convenient for them.
In April 2019, a voting survey of statements of all four domains was distributed to all consultants with explicit voting instructions. Fifty of 54 consultants completed the survey (93%). Summary graphic and numerical results of consultants’ responses were made available to the voting panelists via an active link for consideration during the voting period.
In June 2019, a voting survey of statements of all four domains was distributed to students and residents. A total of 21 responded. Summary graphic and numerical results of student /resident responses were made available to the voting panel via an active link for consideration during the voting period.
In August 2019, Round 1 of the voting survey of statements of all four domains was distributed to all 64 voting panelists and 64 completed the survey (100%). For Domains 1–3, the number of supporting references at each Grade of Evidence for each statement was listed with the statement. Available to all voting panelists at the time of voting was access via electronic links to results of the consultants’ survey responses and the students’/residents’ survey responses for each statement and each curricular content item. In addition, a comprehensive PDF of all domain statements with comments, rationales, and supporting citations with links to abstracts and/or original articles or documents was also available. Links were also available of descriptions and explanations of the RAND Rules and the GRADE process and scoring.
In September 2019, Round 2 of the voting survey was conducted with the voting panelists. Fifty-nine of 64 panelists completed the survey (92%). Twenty-five new curricular content elements were added based on Round 1 panelists’ comments and discussion and feedback at the consensus conference meeting held in Irvine, CA, during the World Congress on Ultrasound in Medical education between Round 1 and Round 2.
During this second round of voting, statistics for each statement, level of consensus (perfect, very good, good, some, and no consensus) as well as individual panelists’ Round 1 comments and relevant comments from the Irvine consensus conference meeting were made available for panelists to consider prior to voting.
Voting results
Table 3 lists all statements in Domains 1–3 with references that were considered as evidence for each statement, the median appropriateness score for Round 2, the degree of consensus, the level of evidence, and the strength of the recommendation. Table 4 lists all Domain 4 content items considered for an undergraduate medical student ultrasound curriculum.
Statements and discussion
There were a total of 332 consensus conference statements and curricular content items in Domains 1–4. Of these, 145 were recommended, 126 were strongly recommended, and 61 were not recommended. Relevant conference discussion, written survey comments of participants, and more recent references have been included in the discussion of the final consensus recommendations.
Domains 1–3
Of the 28 statements in Domains 1–3 covering the scope, the rationale, and the characteristics of an undergraduate ultrasound curriculum, 19 statements were recommended and 9 were strongly recommended. As anticipated, GRADE evaluation of the literature did not demonstrate a high level of evidence for the statements, confirming the need for an emphasis on expert opinion.
These 28 consensus statements can serve as a guide for medical school curriculum directors and their institutions in the planning, development, and expansion of ultrasound medical student education. Details including statements, rationales and relevant references of all 28 statements can be found in Additional file 1: Appendix S1. The nine statements that the expert panelists strongly recommended are highlighted here as well as one of the recommended statements of particular significance related to non-physician ultrasound education.
Domain 1: scope of consensus conference curriculum
D1.1: The ICC will produce consensus recommendations on “An integrated ultrasound curriculum” (“curriculum”) for undergraduate medical education (medical school).
The overall structure of the medical student curriculum should be that of an integrated curriculum across concurrent courses horizontally and across courses and clinical clerkships vertically for each year of medical school. Integration can be broadly defined operationally as deliberately unifying separate areas of knowledge [26]. Globally, medical education accrediting bodies have encouraged and even required that medical school curricula be integrated [27,28,29]. The Carnegie Foundation Report in 2010 Educating Physicians: A Call for Reform of Medical School and Residency calls for more integration throughout medical education [31]. Various levels of integrated ultrasound curricula have been successfully implemented in medical schools internationally varying in size, school mission, and integration format [33,34,35,36,37,38, 157, 173].
D1.2: The curriculum forms the foundation for ultrasound as a core clinical competency for all graduates regardless of specialty choice.
Over the past two decades, competency-based medical education (CBME) has become the standard for medical education. Competency can be defined as an observable, measurable, and assessable ability of a health professional. Competencies can be broken down into milestones that are observable steps used to assess and document a learner’s progress toward a given competency along a developmental continuum [39, 40].
General Physician Competencies have been clustered into domains of competence which are broad but distinguishable areas of competence that constitute a general descriptive framework for a profession [41]. From the work on competencies and domains have come Entrustable Professional Activities (EPAs). EPAs are units of professional practice, defined as tasks or responsibilities that trainees are entrusted to perform unsupervised once they have attained sufficient specific competence [42, 43].
Ultrasound is well suited for a competency-based model of medical education and EPAs. Ultrasound can directly serve as a competency component for a number of the core EPAs such as performing a quality physical examination (EPA 1), prioritizing a differential diagnosis following a clinical encounter (EPA 2), recommending and interpreting common diagnostic and screening tests (EPA 3), recognizing a patient requiring urgent or emergent care and initiating evaluation and management (EPA 10), and performing general procedures of a physician (EPA 12) [3, 44,45,46,47,48,49,50,51,52].
In addition to these direct roles that ultrasound can play in these EPAs, it can also play important indirect roles in several other core EPAs such as being more knowledgeable about ordering imaging studies (EPA 4), forming clinical questions (EPA 7), collaborating on an inter-professional team (EPA 9), understanding informed consent (EPA 11), and contributing to a culture of safety and improvement (EPA 13).
Patient safety is an important aspect of EPAs as it has been proclaimed as “the primary motivation for the work on EPAs” [42]. Because ultrasound does not use ionizing radiation like X-rays and computed tomography, it is a particularly safe imaging modality. In addition, the Agency for Healthcare Research and Quality (AHRQ) has identified the use of real-time ultrasound guidance during central line insertion as a top ten patient safety practice. The AHRQ also recommends that providers not delay in adopting this practice of using ultrasound guidance [53].
Domain 2: rationale for the curriculum
D2.8: The curriculum enhances the overall educational experience.
Early POCUS research on medical student exposure to ultrasound focused primarily on student satisfaction and found that students enjoy having ultrasound in the curriculum and feel it enhances their education [33, 70, 82, 84, 116,117,118,119]. However, some evidence suggests that students can feel overconfident in their POCUS skills or image interpretation at a time when they have limited understanding of the underlying core principles of patient management leading to the consideration that POCUS might best be considered as a supplemental skill [120]. POCUS has been described as motivating students to delve deeper into matters of interest while not appearing to adversely impact the time necessary to learn the content that already exist in overcrowded undergraduate curricula [35, 121]. Although there is some suggestion that ultrasound improves basic science knowledge and clinical skill, future educational research will need to focus more on objective outcomes that show that ultrasound enhances learning of content and prepares students for advanced training and clinical practice.
D2.9: Medical students can learn basic ultrasound.
There is ample evidence that students can learn basic ultrasound and ultrasound applications, including both image acquisition and image interpretation [35, 70,71,72, 75, 122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142]. Image integration into clinical practice still requires clinical knowledge that exposure to ultrasound anatomy and physiology alone does not confer. Once a standardized ultrasound curriculum is established, more individual and collaborative research efforts will be needed to further define the best methods of ultrasound instruction and assessment of student ultrasound knowledge and skill.
Domain 3: characteristics of the curriculum
D3.1: The ultrasound curriculum forms the foundation for ultrasound training along a continuum of medical education from undergraduate through graduate to continuing medical education.
Point-of-care ultrasound at the patient's bedside represents a new tool for the practicing physician. Originally introduced by those caring for emergency and critical care patients to rapidly evaluate and manage their patients, its use has spread throughout hospital services and outpatient care settings. As many as 20 US medical and surgical specialties now require competency and/or experience in ultrasound applications at the completion of their graduate medical education training [152].
Because POCUS is rapidly diffusing into medical practice, it is essential that there be a structured and well-organized program to facilitate ultrasound training in schools of medicine and a smooth transition to postgraduate training.
A recent scoping review of the literature on ultrasound in medical school education and a consensus of ultrasound education directors support the need for a standardized point-of-care ultrasound curriculum that would lead to the development of common standards for milestones and competency-based assessments [19, 155]. Hence, a standardized foundational curriculum delineated by experts in the field of ultrasonography, by those experienced in its use in diverse clinical settings and at the point of patient care, and by educators knowledgeable about the trajectory of physician development can provide guidance as this new skill is integrated into the profession throughout the world.
D3.8: The ultrasound curriculum enhances the learning of clinical sciences through the integration of ultrasound into clinical problem solving.
Along with the integration of the patient history, the physical exam, and laboratory data, point-of-care ultrasound can provide additional information readily available at the time of the patient encounter leading to a more rapid and accurate guide to diagnosis and treatment [3, 163]. Thus, the introduction of ultrasound into the medical school curriculum, likewise, may provide additional accuracy in the accumulation of patient information that fosters improved understanding of underlying pathophysiology. Such improved understanding can aid in the development of a student’s rational diagnostic or therapeutic plan. Ultrasound in undergraduate medical education has been shown to improve the accuracy of the student physical examination. For example, students with limited ultrasound training were more accurate than cardiologists in cardiac exams [44]; than faculty in estimating the size of the liver [45]; and in locating the femoral artery with than without ultrasound [99]. Integration of ultrasound has the potential to improve other aspects of the physical exam, including evidence of professionalism [154]. Use of ultrasound by students may enhance their ability to assess patients with critical presentations, such as hypotension [100]. Accurate patient assessment during physical examination allows the student to better integrate findings into their overall clinical problem solving.
The following recommendations are clustered for discussion as all three relate to the value and validity of the recommended curriculum in the context of organized medical ultrasound.
D3.12: The ultrasound curriculum is based on evidence and expert opinion.
D3.13: The ultrasound curriculum is consistent with recommendations and guidelines of well-established specialty organizations.
D3.14: The ultrasound curriculum is consistent with recommendations and guidelines of regulatory bodies with significant experience in ultrasound.
Point-of-care ultrasound represents a new clinical skill with much information now accumulating on its applicability to many areas of medicine. As such, a burgeoning literature along with expert opinion is becoming widely accessible to guide the development of an international curriculum. A number of professional societies have developed or are developing guidelines and/or curricula in the area of ultrasound [5, 106, 164,165,166,167,168,169,170,171,172]. The International Consensus Curriculum aligns with these societal guidelines to prepare early learners with the necessary foundation to use POCUS in their future chosen area of medicine, as supported by the guidelines of these national and international societies.
In addition to these strong recommendations from Domains 1–3, recommended statement D1.4 concerning the role of the consensus conference curriculum in non-physician education warrants some clarification based on considerable conference meeting discussion and survey comments.
D1.4: The curriculum can serve as a valuable resource for the development of ultrasound training programs for non-physician healthcare providers such as advanced nurse practitioners and physician assistants.
Considering the overlap in medical student educational content and skill with that of other healthcare professionals as set by their accrediting bodies such as nurse practitioners, nurses, physician assistants, and emergency medicine technicians, an integrated ultrasound curriculum for medical students should prove to be a valuable and appropriate resource for the education of these and other healthcare professionals [27, 59,60,61,62]. It has been demonstrated that non-physician providers can learn and competently use ultrasound in the clinical setting [63,64,65,66]. In addition, a common clinical skill like ultrasound offers excellent opportunities for inter-professional training.
There was agreement in conference discussions that a standardized ultrasound curriculum for medical students determined by this consensus conference could be a valuable resource for non-physician healthcare providers. However, it was emphasized that the curriculum should not be considered a recommended curriculum; it should only serve as a resource for curricular development. Other healthcare providers will need to determine the specifics of their ultrasound curricula based on their accreditation and clinical practice standards as determined by their own professional organizations.
Domain 4: curricular content
Domain 4 focused on the content of a medical student ultrasound curriculum. Of the 304 Domain 4 content items, 126 (41.4%) were recommended, 117 (38.5%) were strongly recommended, and 61 (20.1%) were not recommended. All recommended content would be considered appropriate for a medical student ultrasound curriculum, but should not be considered as required content. Content used within an individual medical student curriculum should be based on a number of factors including how well the specific content items fulfill the needs and objectives of the courses and clinical clerkships in the curriculum, the availability of adequate resources to implement the specific ultrasound components, and the faculty expertise available to teach the specific components of the ultrasound curriculum.
It should also be noted that for those medical educational systems that have medical school graduates immediately engaged in various levels of independent clinical practice, assessment of medical student ultrasound competency at graduation would need particular attention. Completion of the recommended ultrasound curricular content does not ensure independent clinical ultrasound competency. The decision of practice competency directly after medical school graduation will need to be made by the individual medical school and/or the appropriate accrediting body in accordance with established clinical practice standards.
Medical schools with successful ultrasound programs have generally started by introducing a small number of basic ultrasound components into the curriculum and have then expanded the number of ultrasound components over time [33, 37, 38, 157]. It is important to not overwhelm faculty and students with new material on ultrasound to assimilate into an already crowded curriculum. An incremental approach also allows time to gather student and faculty feedback evaluating the program as it develops so that informed curricular management decisions can be made.
Domain 4 part 1: basic foundations of point-of-care ultrasound
Part one of Domain 4 contained 92 content items related to the “Basic Foundations of Point-of-Care Ultrasound”. These items covered the physics of ultrasound, imaging modalities, ultrasound terminology, machine and probe characteristics, image acquisition, basic image interpretation, patient care issues, and correlation of clinical findings.
Of the 92 items, 26 (28.3%) were recommended, 64 (69.6%) were strongly recommended, and 2 (2.2%) were not recommended. The two items not recommended were related to the acquisition of images with power Doppler (D4.74) and spectral Doppler (D4.75) imaging modalities. Although it was recommended that students should understand the fundamental principles of power Doppler and spectral Doppler, it was felt that image acquisition with these two modalities was too advanced for medical student ultrasound education.
The 90 basic foundation items recommended or strongly recommended are consistent with the essentials and standards for education in medical sonography across multiple ultrasound societies and accrediting bodies [174,175,176,177,178,179]. These recommended basic items should help promote the standardization of medical student ultrasound education globally as well as provide a common language and framework to enhance communication among those interested in ultrasound education, practice, and research. This will be particularly helpful as collaborative efforts develop across the continuum of ultrasound education from undergraduate to postgraduate medical education. Further strengthening the continuum of ultrasound education with standardization of the basics will allow directors of postgraduate medical education to anticipate the ultrasound knowledge and skill levels of incoming medical school graduates and plan a smooth transition to postgraduate training.
Several topics and items within Domain 4 Part 1 deserve special comment. The first of these concerns “proper care for the patient” which focuses on patient interactions that include professional communication (D4.85), informed consent (D4.86), privacy (D4.87), comfort (D4.88), patient positioning D4.89), and documentation (D4.90). These strongly recommended patient interactions should be at the core of medical student education and taught, modeled, and assessed from the earliest stages of teaching ultrasound to students. With ultrasound education, the patient’s well-being should always be the primary focus of the patient encounter and not become secondary to the technology. One of the significant advantages of ultrasound education is a greater return to the patient’s bedside offering many opportunities to teach and model the art, the science, and the humanity of practicing medicine. Spending more time with the patient at the bedside is consistent with initiatives to foster more meaning and joy in work and deeper engagement with patients [180].
In addition to these recommendations, two other patient-centered recommendations related to patient safety need special emphasis. Specifically related to patient safety were strong recommendations for the principle of using ultrasound intensity as low as reasonably achievable, known as the ALARA principle, (D4.91) and the importance of appropriate cleaning and disinfection of probes (D4.27) prior to scanning. This recommendation of probe disinfection has taken on an even greater significance during the COVID pandemic with acute concern for transmission of infection during ultrasound procedures. Portable bedside ultrasound has played a significant role in the diagnosis and management of COVID patients across the globe [181]. In addition, the ability to more easily clean and disinfect these portable bedside devices rather than the larger cart-based machines and those in the radiology suite and limiting the need to transport patients throughout the medical facility for imaging will likely improve protection against transmission of infection to non-COVID patients, staff, and healthcare providers.
Also worthy of special note in Domain 4 Part 1 is the importance of correlating ultrasound images with clinical findings (D4.92). This statement received the highest mean appropriateness score (8.95) of all statements in the survey and reflects the high priority the voting panelists place on the educational value of ultrasound as an important tool to better understand medicine and improve clinical care.
An issue under “Basic Foundations” of ultrasound that generated significant discussion and comments was related to transducer or probe manipulation terminology (D4.28-D4.33). Even though all six manipulation items were recommended or strongly recommended, a number of panelists commented on a preference for specific transducer manipulation terms while scanning and expressed the need for more standardization of probe manipulation terms to enhance consistency of hands-on scanning instruction.
Probe manipulation terminology has been a controversial issue for years as multiple terms have been used for the same or similar manipulations of the probe such as “fan” or “tilt” the probe. These terms have been variably adopted by ultrasound users and educators and can be a source of confusion to new learners who are being taught by various instructors using different terms for the same probe maneuver. It can also be a source of confusion when students are viewing instructional videos that use different terminology from what they have learned. Comments from the panelists were mixed on this topic with some experts recommending that an effort be made for a universally accepted set of terms while others felt a group of acceptable terms could be recommended and individuals in various educational programs could decide which ones they wish to use coincident with local use. For the consensus conference, it was decided to use six probe motions that have been well-described in the literature [182]. Even though it is unlikely that a single set of probe manipulation terms will be universally adopted from this consensus process, these recommendations may encourage movement toward a more uniform set of terms.
Domain 4 part 2: views, structure/physiology, pathology
Domain 4, Part 2 items relate to specific ultrasound views, structures/physiology, and pathology with regional and organ subdivisions of heart and vessels, lungs and chest, abdomen, pelvis, head and neck, and musculoskeletal. Of the 196 items, 92 (46.9%) were recommended, 51 (26.0%) were strongly recommended, and 53 (27.1%) items were not recommended.
Ultrasound views
There was very good agreement on teaching students ultrasound views proposed by the Domain 4 task team and the expert voting panel. Of the 30 views, 10 (33.3%) were recommended, 17 (56.2%) were strongly recommended, and 3 (10.0%) were not recommended.
The recommended and strongly recommended views include widely recognized standard views of the various organ systems. The transvaginal view of the pelvis (D4.198) was not recommended as it was felt to be more appropriate for postgraduate medical education. In addition, cultural differences were also noted with respect to training students in the transvaginal view and it was felt that if the transvaginal view is taught, it should be done on simulators and not patients. The other two views not recommended were two specific ankle views (D4.248–249) that were not felt to be of significant value to warrant having students learn them in medical school.
Recommendations on what ultrasound views to teach students are critically important, especially early in the ultrasound learning process. Introductory views should be relatively easy to learn for those new to ultrasound. They should also allow students to visualize anatomical structures and physiological organ functioning important in understanding normal anatomy, normal physiology, and common pathophysiology to prepare them well for postgraduate training.
A limited number of more advanced views can be taught in medical school, but it would not be practical to teach students all ultrasound views in medical school due to the time required. Should a school wish to offer more advanced ultrasound scanning skills for students, several elective options can be considered. These include an independent ultrasound study month, departmental ultrasound offerings, participation in ultrasound research, and final year compressed or boot camp ultrasound experience to prepare students for specific residency ultrasound applications [21, 33, 68, 183,184,185]. Another option that allows interested students to gain more advanced ultrasound skills is through student ultrasound interest group activities which generally occur outside of the formal curricular schedule [186].
It should be noted that even with standard basic ultrasound views, some of these views are easier to learn than others, such as the parasternal long axis (PLAX) view of the heart as compared to the apical 4 chamber view of the heart. Once the PLAX view is learned and practiced, learning the apical 4 chamber view is generally much easier. Thus, it is best to start with relatively easy to learn views and progress to slightly more difficult views over time. This same approach is also true in considering the scanning difficulty level of models and patients used for ultrasound instruction. Starting with relatively easy-to-scan models and progressing to more difficult-to-scan models creates a better learning experience. This approach allows students to progressively improve their basic scanning skills and confidence. It also allows them to more efficiently capture quality images of the important structures and organs under study to enhance learning of the primary course content material.
Structures/physiology
There was good agreement between Doman 4 task team proposed structure and physiology content and the expert voting panel. Of the 94 structure/physiology items, 52 (55.3%) were recommended, 21 (22.3%) were strongly recommended, and 21 (22.3%) were not recommended.
Similar to the considerations for what ultrasound views to teach, the specific structures and physiology to teach with ultrasound should be based on their value in learning normal anatomy and physiology and preparing students to better understand pathophysiology important to the practice of medicine. They also need to be appropriate for the undergraduate level of medical education. More advanced content should be left for postgraduate medical education or offered in student electives for those wanting to learn more than what is offered in the required student curriculum.
The voting panel did not recommend the 21 content items for three primary reasons. From international conference discussion and panelists’ written comments, some of the required ultrasound images were considered too difficult for students to consistently visualize well enough for them to be used to teach the course content such as the adrenal glands (D4.174), the pancreas (D4.168), and the appendix (D4.184). Some structures and physiology were just not considered appropriate for a medical student basic curriculum such as the placenta (D4.205) and testes (D4.206). Finally, it was felt that topics with multiple appropriate examples in the same class of structures, such as peripheral blood vessels and musculoskeletal structures, should not be covered comprehensively, but instead one or two examples should be taught. For example, students could learn common musculoskeletal joint structures and biomechanical principles by learning to scan the knee without spending additional time scanning multiple other joints.
Pathology
The final section of Part 2 was concerned with what pathology to teach medical students with ultrasound. This section had a relatively low level of agreement between what the Domain 4 task team proposed for curricular content and what the expert panel felt was appropriate for medical student education. Of 70 pathology items only 30 (42.9%) were recommended, 11 (15.7%) were strongly recommended, and 29 (41.4%) were not recommended.
This low level of recommendation was not related to the value of ultrasound in teaching pathology, but rather to the specific ultrasound pathology content. Much of the pathology was felt to be more appropriate for postgraduate training as opposed to medical student education. There was also some concern expressed by panelists that students could become overconfident in their ability to identify or rule out pathology with ultrasound. This could have serious adverse consequences for patients such as pursuing additional unnecessary and costly testing with potential risk or not recognizing significant clinical findings, thus delaying diagnosis and treatment. An example of this type of pathology that was not recommended to be included was dissection of an abdominal aortic aneurysm (D4.135).
While not included as content for voting in this international consensus conference, the notion of overconfidence, knowing one's limitations in ultrasound and medical knowledge, as well as, understanding the inherent limitations of ultrasound in specific circumstances should be addressed in the curriculum as a whole. These aspects of ultrasound education could be clustered as learning the indications, limitations, benefits, and risks of ultrasound in common clinical scenarios [19].
Less consensus for recommending the pathologies to teach medical students may have been partly related to the diverse composition of the voting panelists. Different specialists and subspecialists would likely differ in the value they place on various pathologies to teach medical students and the ability of students to adequately capture and interpret those ultrasound images during medical student education.
Under pathology, it is instructive to note that the Sonographic Murphy Sign (D4.189) is a good example of ultrasound enhancing the physical examination (D2.5). Sonographic Murphy sign is a painful reaction of the patient when pressing directly over the gallbladder with the ultrasound probe which could be consistent with acute cholecystitis. Being able to look under the skin with ultrasound to provide visual information can enhance the accuracy of the physical examination as well as enhance learning of physical examination skills by providing real-time validation of the physical examination component. Ultrasound can be applied to learning many aspects of the physical examination such as confirming inspection of the neck for the location and size of the thyroid, palpating the liver and gallbladder for location, size, and tenderness, percussing the lungs for the resonance of normal lung or the dullness of a pleural effusion, and auscultating the heart for a murmur or a pericardial friction rub. [33, 135, 154].
Domain 4 part 3: procedures and protocols
Domain 4, Part 3 items relate to ultrasound procedures and protocols and it also had a relatively low level of agreement between the Domain 4 task team proposals and the expert voting panel. Of 16 items, 8 (50.0%) were recommended, 2 (12.5) were strongly recommended, and 6 (37.5%) were not recommended.
The skill of ultrasound-guided procedures was robustly discussed during face-to-face consensus conference meetings and a number of written comments appeared on the voting survey. It was strongly felt that students should be taught to visualize fluid-filled cavities with ultrasound (D4.298) and how to use ultrasound to guide a needle safely into a fluid-filled cavity (D4.299). A number of common guided procedures were recommended, including peripheral (D4.289) and central line cannulation (D4.290), paracentesis (D4.292), thoracentesis (D4.293), and arthrocentesis (D4.294). However, the less common and more risky guided procedures of pericardiocentesis (D4.291) and lumbar puncture (D4.295) were not recommended. However, it was also expressed that how to use ultrasound to guide a needle or catheter was the important skill and there was no need to learn multiple guided procedures. Learning a variety of guided procedures was best reserved for postgraduate medical training when the focus could be on procedures more relevant to the specialty pursued. It was also expressed that, in general, learning guided procedures is best done on phantom models and not on live subjects.
The final category of Part 3 was ultrasound protocols and included the more common clinical protocols. Two of these were recommended for medical student curricula. These included the E-FAST protocol (Extended Focused Assessment with Sonography in Trauma) (D4.300) for trauma and the RUSH protocol (Rapid Ultrasound for Shock and Hypotension) (D4. 301) for hypotension and shock. Other protocols were not recommended. There was general discussion and panelists commented that individual components of protocols could be taught, but there would not be significant value in teaching more than one or two protocols given the many and continually expanding list of protocols. Most protocols are best left for advanced training where specific protocols related to various specialties could be learned and clinically applied.
It should be noted that both the E-FAST and RUSH protocols have been used for teaching medical student content such as physiology clinical correlation and trauma assessment in emergency medicine and surgery [33, 34, 187]. Thus, these two protocols could serve as valuable teaching protocol examples should a school wish to introduce a few select protocols consistent with their curricular objectives.
Consultant and student/resident survey responses
There was overall good agreement with the survey results of the voting panelists and the consultants using mean appropriateness scores. Some minor differences of note were higher scores from the consultants than the voting panelists for the role of ultrasound in self-directed learning (D3.10)—8.44 versus 7.83 and life-long learning (D3.11)—8.42 versus 7.62. The highest score for both groups was for the importance of correlating ultrasound images with clinical findings (D4.92)—8.98 consultants, 8.95 voting panelists.
A high score for correlation with clinical findings was also recorded by the students/residents (8.88), but their highest score (8.94) went to multiple content items on the basics of scanning and concern for the patient. In general, students/residents gave higher scores for pathology items in the curricula content than the voting panelists. For example, appropriateness scores for abdominal aortic aneurysm dissection (D4.135) for panelists was 7.07 and 8.06 for the students/residents. The students also gave higher appropriateness scores for ultrasound procedures and ultrasound protocols. Because of the small, self-selected nature of the student/resident survey participants, definitive conclusions cannot be drawn about student/resident opinions, but it does suggest a difference of opinion in some areas of ultrasound education. These potential differences should be explored and students and residents should be included in curricular development.
Additional comments from consultants for the most part echoed those of the voting panelists including the need for balance of ultrasound content in an already crowded medical student curriculum and remaining within the appropriate level of knowledge, attitude, and skills for medical students, especially with respect to advanced scanning techniques, pathology, and protocols. Students did mention that the curricular content appeared to be comprehensive and would require strong medical school buy-in to be successful.
Consensus conference conclusions
A sense of urgency exists for the need to incorporate ultrasound into medical student education. The data for the value of ultrasound to improve the quality of patient care, patient safety, and access to care for all patients across the globe have been mounting for almost three decades. The technological advances and lower cost have made ultrasound highly accessible and the interest in ultrasound education in medical school is rising at an exponential rate. The adoption of ultrasound across postgraduate (residency) programs is rapidly increasing and the calls for help in developing the appropriate educational support are growing louder as echoed in a recent POCUS article in the New England Journal of Medicine [23].
It is imperative that the undergraduate medical education community proceed in a timely fashion with a plan to help ensure ultrasound training for medical students that is appropriate, supported with ongoing quality research efforts, and offers a smooth transition to postgraduate training. Establishing a standardized ultrasound curriculum based on the available evidence and global expert opinion is a critical step in that process. This conference was designed to address this need. All recommended and strongly recommended statements of curricular content are listed in Additional file 2: Appendix S2.
The international conference addressed several limitations of previously reported consensus recommendations for foundational ultrasound curricula for medical student education [155, 158, 188]. These earlier recommendations often were directed at specific clinical components rather than an integrated curriculum that spans basic and clinical sciences of undergraduate medical education. By necessity, these recommendations usually engaged a national or regional approach, as opposed to the global approach taken here. Previous consensus conferences often lacked expertise across clinical specialties, subspecialties, and basic science disciplines, a much-needed perspective for an integrated curriculum. Likewise, there has also been limited representation across global educational systems which not only vary in location but also culture, curricular models, available resources, educational accrediting standards, and institutional vision and mission [189]. In addition, some of the earlier publications used a less comprehensive consensus methodology than was used here, which includes quantifying the level of evidence of the relevant literature and making that available to the voting participants.
To overcome these various limitations, especially those related to the diversity of expert ultrasound practitioners and educators, a large, diverse group of 64 expert voting panelists representing over 20 specialists, subspecialists, and basic science educators from 16 countries were selected to participate. Over 90% of panelists voted in both rounds, ensuring recommendations from a diversity of panelists. Also, contributing expert input to the consensus process were 50 global consultants with similar ultrasound credentials as the voting panelists as well as 21 medical students and residents with a keen interest in ultrasound education. An extensive multi-source literature search and a rigorous modified Delphi methodology were utilized including the GRADE method to evaluate level of evidence and the RAND methodology for degree of appropriateness, consensus, and final recommendations.
In addition to the formal voting results for each statement, relevant concerns, comments, and advice from the consensus participants have been included in the discussion. These comments provide valuable insight from those who have extensive experience in ultrasound education and can further assist those new to medical student ultrasound education in implementing an ultrasound curriculum. Also included in the discussion are the results of more recent publications on ultrasound education. All voting panelists reviewed the journal manuscript for accuracy of content prior to submission. This consensus conference represents the most comprehensive medical school consensus process to date to standardize a global ultrasound curriculum.
There were several limitations of the consensus process that should be noted. Despite the broad representation of clinical specialties and subspecialties, not all areas of medicine were included (e.g., ophthalmology and physical medicine) that might have considerations for future ultrasound practice. Additional representation of basic biomedical science, pathology, and even genetics could provide an even broader perspective. Likewise, a broader global ultrasound education perspective should be considered in the future (i.e., Africa). While students and residents were included, more systematic inclusion of these stakeholders will likely be more feasible as ultrasound education spreads throughout institutions. This input will prove more helpful when teaching and assessment methods are critically addressed in future research and consensus processes.
It is hoped that the consensus curriculum will facilitate independent and collaborative research into what aspects of the proposed curriculum work well and what should be modified, added, or eliminated. The curriculum should be considered an ongoing global educational project. It will need to be updated as new ultrasound technology, ultrasound applications, and research-based educational and clinical results and advances become available. A standardized curriculum should enhance collaboration among directors of undergraduate and postgraduate medical education to strengthen the continuum of ultrasound education and help ensure the smooth transition from one stage of training to the next and advance patient care.
Currently medical student ultrasound education, including hands-on scanning instruction, is supported by the ultrasound specialties of radiology, cardiology, obstetrics and gynecology and major national and international ultrasound organizations with publications, meetings, student interest groups, and online education material on their websites [158, 175,176,177,178,179, 190,191,192,193]. Collaborative efforts with these established ultrasound groups will help modify and advance this curriculum, as well as strengthen the continuum of ultrasound education across the professional lives of healthcare providers.
Ultrasound presents an opportunity in our lifetimes to improve how we fundamentally teach and practice medicine to the benefit of students and patients across the globe. In the rich humanitarian tradition of medicine, may we seize this opportunity for teaching and using ultrasound to make this world a healthier and better place for all.
Availability of data and materials
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Teichgräber UK, Meyer JM, Poulsen Nautrup C, von Rautenfeld DB (1996) Ultrasound anatomy: a practical teaching system in human gross anatomy. Med Educ 30(4):296–298. https://doi.org/10.1111/j.1365-2923.1996.tb00832.x
Brunner M, Moeslinger T, Spieckermann PG (1995) Echocardiography for teaching cardiac physiology in practical student courses. Am J Physiol 268(6 Pt 3):S2–S9. https://doi.org/10.1152/advances.1995.268.6.S2
Moore CL, Copel JA (2011) Point-of-care ultrasonography. N Engl J Med 364(8):749–757. https://doi.org/10.1056/NEJMra0909487
Kiss G, Korda D, Szabó G et al (2019) Oncological screening of kidney transplant patients: the role of ultrasound examination. Transplant Proc 51(4):1231–1233. https://doi.org/10.1016/j.transproceed.2019.04.016
Ultrasound guidelines—emergency point of care and American College of Emergency Physicians Policy Statement. https://www.acep.org/globalassets/new-pdfs/policy-statements/ultrasound-guidelines---emergency-point-of-care-and-clinical-ultrasound-guidelines-in-medicine.pdf. Accessed 25 April 2022
Society of Clinical Ultrasound Fellowships. Society of Clinical Ultrasound Fellowships Web site. https://eusfellowships.com/. Accessed 25 April 2022
Lewiss RE, Adhikari S, Carmody K et al (2016) The society of clinical ultrasound fellowships: an innovation in the point of care ultrasound fellowship application process. Am J Emerg Med 34(7):1303–1305. https://doi.org/10.1016/j.ajem.2016.03.070
Neri L, Storti E, Lichtenstein D (2007) Toward an ultrasound curriculum for critical care medicine. Crit Care Med 35(5 Suppl):S290–S304. https://doi.org/10.1097/01.CCM.0000260680.16213.26
Expert Round Table on Ultrasound in ICU (2011) International expert statement on training standards for critical care ultrasonography. Intensive Care Med 37(7):1077–1083. https://doi.org/10.1007/s00134-011-2246-9
Frankel HL, Kirkpatrick AW, Elbarbary M et al (2015) Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients—part I: general ultrasonography. Crit Care Med 43(11):2479–2502. https://doi.org/10.1097/CCM.0000000000001216
Levitov A, Frankel HL, Blaivas M et al (2016) Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients—part II: cardiac ultrasonography. Crit Care Med 44(6):1206–1227. https://doi.org/10.1097/CCM.0000000000001847
Wong A, Galarza L, Forni L et al (2020) Recommendations for core critical care ultrasound competencies as a part of specialist training in multidisciplinary intensive care: a framework proposed by the European Society of Intensive Care Medicine (ESICM). Crit Care 24(1):393. https://doi.org/10.1186/s13054-020-03099-8
Bornemann P (2017) Assessment of a novel point-of-care ultrasound curriculum’s effect on competency measures in family medicine graduate medical education. J Ultrasound Med 36(6):1205–1211. https://doi.org/10.7863/ultra.16.05002
Hall JWW, Holman H, Barreto TW et al (2020) Point-of-care ultrasound in family medicine residencies 5-year update: a CERA study. Fam Med 52(7):505–511. https://doi.org/10.22454/FamMed.2020.223648
American College of Emergency Physicians Policy Statement. Ultrasound guidelines: emergency, point-of-care, and clinical ultrasound guidelines in medicine. Approved June 2016. American College of Emergency Physicians Web site. https://www.acep.org/globalassets/new-pdfs/policy-statements/ultrasound-guidelines---emergency-point-of-care-and-clinical-ultrasound-guidelines-in-medicine.pdf. Published 2022. Accessed 25 April 2022
Aafp.org. American Academy of Family Physicians Web site. https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf. Published 2022. Accessed 25 April 2022
Barron KR, Wagner MS, Hunt PS et al (2019) A primary care ultrasound fellowship: training for clinical practice and future educators. J Ultrasound Med 38(4):1061–1068. https://doi.org/10.1002/jum.14772
Bahner DP, Goldman E, Way D, Royall NA, Liu YT (2014) The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med 89(12):1681–1686. https://doi.org/10.1097/ACM.0000000000000414
Tarique U, Tang B, Singh M, Kulasegaram KM, Ailon J (2018) Ultrasound curricula in undergraduate medical education: a scoping review. J Ultrasound Med 37(1):69–82. https://doi.org/10.1002/jum.14333
Glass C, Sarwal A, Zavitz J et al (2021) Scoping review of implementing a longitudinal curriculum in undergraduate medical education: the wake forest experience. Ultrasound J 13(1):23. https://doi.org/10.1186/s13089-021-00206-w
Sena A, Alerhand S, Lamba S (2021) Milestone approach to designing a point-of-care ultrasound curriculum for transition-to-residency programs in the United States. Teach Learn Med 33(3):270–281. https://doi.org/10.1080/10401334.2020.1814296
Feilchenfeld Z, Kuper A, Whitehead C (2018) Stethoscope of the 21st century: dominant discourses of ultrasound in medical education. Med Educ 52(12):1271–1287. https://doi.org/10.1111/medu.13714
Díaz-Gómez JL, Mayo PH, Koenig SJ (2021) Point-of-care ultrasonography. N Engl J Med 385(17):1593–1602. https://doi.org/10.1056/NEJMra1916062
Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A (2011) GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 64(4):380–382. https://doi.org/10.1016/j.jclinepi.2010.09.011
Fitch K, Bernstein SJ, Aguilar MD et al (2001) The RAND/UCLA appropriateness method user’s manual. RAND Corporation, Arlington
Goldman E, Schroth WS (2012) Perspective: deconstructing integration: a framework for the rational application of integration as a guiding curricular strategy. Acad Med 87(6):729–734. https://doi.org/10.1097/ACM.0b013e318253cad4
Functions and structure of a medical school: standards for accreditation of medical education programs leading to the MD degree. Liaison Committee on Medical Education. https://lcme.org/publications/. Published 2020. Accessed 26 April 2022
Standards for assessment and accreditation of primary medical programs by the Australian Medical Council 2012. Australian Medical Council Limited. https://www.amc.org.au/wp-content/uploads/2019/10/Standards-for-Assessment-and-Accreditation-of-Primary-Medical-Programs-by-the-Australian-Medical-Council-2012.pdf. Published 2012. Accessed 26 April 2022
The future of medical education in Canada (FMEC): a collective vision for MD education. The Association of Faculties of Medicine of Canada (AFMC). https://www.afmc.ca/sites/default/files/pdf/2010-FMEC-MD_EN.pdf. Published 2010. Accessed 26 April 2022
Brauer DG, Ferguson KJ (2015) The integrated curriculum in medical education: AMEE guide no. 96. Med Teach 37(4):312–322. https://doi.org/10.3109/0142159X.2014.970998
Irby DM, Cooke M, O’Brien BC (2010) Calls for reform of medical education by the Carnegie Foundation for the Advancement of Teaching: 1910 and 2010. Acad Med 85(2):220–227. https://doi.org/10.1097/ACM.0b013e3181c88449
Van der Veken J, Valcke M, De Maeseneer J, Schuwirth L, Derese A (2009) Impact on knowledge acquisition of the transition from a conventional to an integrated contextual medical curriculum. Med Educ 43(7):704–713. https://doi.org/10.1111/j.1365-2923.2009.03397.x
Hoppmann RA, Rao VV, Bell F et al (2015) The evolution of an integrated ultrasound curriculum (iUSC) for medical students: 9-year experience. Crit Ultrasound J 7(1):18. https://doi.org/10.1186/s13089-015-0035-3
Palma JK (2015) Successful strategies for integrating bedside ultrasound into undergraduate medical education. Mil Med 180(4 Suppl):153–157. https://doi.org/10.7205/MILMED-D-14-00573
Rao S, van Holsbeeck L, Musial JL et al (2008) A pilot study of comprehensive ultrasound education at the Wayne State University School of Medicine: a pioneer year review. J Ultrasound Med 27(5):745–749. https://doi.org/10.7863/jum.2008.27.5.745
Russ BA, Evans D, Morrad D et al (2017) Integrating point-of-care ultrasonography into the osteopathic medical school curriculum. J Am Osteopath Assoc 117(7):451–456. https://doi.org/10.7556/jaoa.2017.091
Bahner DP, Adkins EJ, Hughes D, Barrie M, Boulger CT, Royall NA (2013) Integrated medical school ultrasound: development of an ultrasound vertical curriculum. Crit Ultrasound J 5(1):6. https://doi.org/10.1186/2036-7902-5-6
Wilson SP, Mefford JM, Lahham S et al (2017) Implementation of a 4-year point-of-care ultrasound curriculum in a Liaison Committee on Medical Education-Accredited US Medical School. J Ultrasound Med 36(2):321–325. https://doi.org/10.7863/ultra.16.03068 (published correction appears in J Ultrasound Med. 2017 Jun;36(6):1289)
Frank JR, Snell LS, Cate OT et al (2010) Competency-based medical education: theory to practice. Med Teach 32(8):638–645. https://doi.org/10.3109/0142159X.2010.501190
Holmboe ES, Edgar L, Hamstra S (2016) ACGME: the milestones guidebook
Englander R, Cameron T, Ballard AJ, Dodge J, Bull J, Aschenbrener CA (2013) Toward a common taxonomy of competency domains for the health professions and competencies for physicians. Acad Med 88(8):1088–1094. https://doi.org/10.1097/ACM.0b013e31829a3b2b
Core entrustable professional activities for entering residency: curriculum developers’ guide. Association of American Medical Colleges. https://www.aamc.org/media/20211/download. Published 2017. Accessed 26 April 2022
Ten Cate O, Chen HC, Hoff RG, Peters H, Bok H, van der Schaaf M (2015) Curriculum development for the workplace using Entrustable Professional Activities (EPAs): AMEE guide no. 99. Med Teach 37(11):983–1002. https://doi.org/10.3109/0142159X.2015.1060308
Kobal SL, Trento L, Baharami S et al (2005) Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol 96(7):1002–1006. https://doi.org/10.1016/j.amjcard.2005.05.060
Mouratev G, Howe D, Hoppmann R et al (2013) Teaching medical students ultrasound to measure liver size: comparison with experienced clinicians using physical examination alone. Teach Learn Med 25(1):84–88. https://doi.org/10.1080/10401334.2012.741535
Steinmetz P, Oleskevich S, Dyachenko A, McCusker J, Lewis J (2018) Accuracy of medical students in detecting pleural effusion using lung ultrasound as an adjunct to the physical examination. J Ultrasound Med 37(11):2545–2552. https://doi.org/10.1002/jum.14612
Mai T, Woo MY, Boles K, Jetty P (2018) Point-of-care ultrasound performed by a medical student compared to physical examination by vascular surgeons in the detection of abdominal aortic aneurysms. Ann Vasc Surg 52:15–21. https://doi.org/10.1016/j.avsg.2018.03.015
Perera P, Mailhot T, Riley D, Mandavia D (2010) The RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically lll. Emerg Med Clin North Am 28(1):29–vii. https://doi.org/10.1016/j.emc.2009.09.010
Lichtenstein DA, Mezière GA (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 134(1):117–125. https://doi.org/10.1378/chest.07-2800 (published correction appears in Chest. 2013 Aug;144(2):721)
Minton KK, Abuhamad A (2013) 2012 ultrasound first forum proceedings. J Ultrasound Med 32(4):555–566
Ultrasound Guidelines (2017) Emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med 69(5):e27–e54. https://doi.org/10.1016/j.annemergmed.2016.08.457
Bhagra A, Tierney DM, Sekiguchi H, Soni NJ (2016) Point-of-care ultrasonography for primary care physicians and general internists. Mayo Clin Proc 91(12):1811–1827. https://doi.org/10.1016/j.mayocp.2016.08.023
Shekelle PG, Wachter RM, Pronovost PJ et al (2013) Making health care safer II: an updated critical analysis of the evidence for patient safety practices. Evid Rep Technol Assess 211:1–945
The Emergency Medical Services Milestone Project July 2015. Accreditation Council for Graduate Medical Education (ACGME) and The American Board of Emergency Medicine. https://www.acgme.org/Portals/0/PDFs/Milestones/EmergencyMedicalServicesMilestones.pdf?ver=2015-11-06-120532-130. Published July 2012. Accessed 26 April 2022
Beal EW, Sigmond BR, Sage-Silski L, Lahey S, Nguyen V, Bahner DP (2017) Point-of-care ultrasound in general surgery residency training: a proposal for milestones in graduate medical education ultrasound. J Ultrasound Med 36(12):2577–2584. https://doi.org/10.1002/jum.14298
Accreditation of colleges of osteopathic medicine: COM accreditation standards and procedures. American Osteopathic Association. https://osteopathic.org/wp-content/uploads/2018/02/com-accreditation-standards-8-29-2016.pdf. Published August 2016. Accessed 26 April 2022
Diretrizes Curriculares Nacionais do Curso de Graduação em Medicina (National Curricular Guidelines of the Undergraduate Medical Course). http://www.fmb.unesp.br/Home/Graduacao/resolucao-dcn-2014.pdf. Published 2014. Accessed 2019
Standards and outcomes. General Medical Council. https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes. Accessed 26 April 2022
Accreditation Standards for Physician Assistant Education, Fourth edition. Accreditation review commission on education for the physician assistant. http://www.arc-pa.org/wp-content/uploads/2018/12/AccredManual-4th-edition.rev5_.18.pdf. Published October 2010. Accessed 26 April 2022
Standards and guidelines for the accreditation of educational programs in the emergency medical services professions. The Commission on Accreditation of Allied Health Education Programs (CAAHEP). https://emsa.ca.gov/wp-content/uploads/sites/71/2019/07/CAAHEP-Standards-and-Guidelines-for-the-Accreditation-of-Educational-Programs-in-the-Emergency-Medical-Services-Professions-2015.pdf. Published 2015. Accessed 26 April 2022
American Nurses Association (2015) Nursing: scope and standards of practice, 3rd edn. American Nurses Association, Silver Spring
The National Task Force on Quality Nurse Practitioner Education (2016) Criteria for evaluation of nurse practitioner programs 5th Edition
Atkinson P, Madan R, Kendall R, Fraser J, Lewis D (2014) Detection of soft tissue foreign bodies by nurse practitioner-performed ultrasound. Crit Ultrasound J 6(1):2. https://doi.org/10.1186/2036-7902-6-2
Mumoli N, Vitale J, Giorgi-Pierfranceschi M et al (2016) Accuracy of nurse-performed lung ultrasound in patients with acute dyspnea: a prospective observational study. Medicine 95(9):e2925. https://doi.org/10.1097/MD.0000000000002925
Balog TP, Rhodehouse BB, Turner EK et al (2017) Accuracy of ultrasound-guided intra-articular hip injections performed in the orthopedic clinic. Orthopedics 40(2):96–100. https://doi.org/10.3928/01477447-20161213-03
Duran-Gehring P, Bryant L, Reynolds JA, Aldridge P, Kalynych CJ, Guirgis FW (2016) Ultrasound-guided peripheral intravenous catheter training results in physician-level success for emergency department technicians. J Ultrasound Med 35(11):2343–2352. https://doi.org/10.7863/ultra.15.11059
Soucy ZP, Mills LD (2015) American academy of emergency medicine position statement: ultrasound should be integrated into undergraduate medical education curriculum. J Emerg Med 49(1):89–90. https://doi.org/10.1016/j.jemermed.2014.12.092
Bahner DP, Royall NA (2013) Advanced ultrasound training for fourth-year medical students: a novel training program at The Ohio State University College of Medicine. Acad Med 88(2):206–213. https://doi.org/10.1097/ACM.0b013e31827c562d
Steller J, Russell B, Lotfipour S et al (2014) USEFUL: ultrasound exam for underlying lesions incorporated into physical exam. West J Emerg Med 15(3):260–266. https://doi.org/10.5811/westjem.2013.8.19080
Eissa K, Alokla K, Assasa O, Itani A, Shawwa K, Kheir F (2015) Using simulation-based training to incorporate thoracic ultrasound into physical examination. J La State Med Soc 167(6):264–267
Arger PH, Schultz SM, Sehgal CM, Cary TW, Aronchick J (2005) Teaching medical students diagnostic sonography. J Ultrasound Med 24(10):1365–1369. https://doi.org/10.7863/jum.2005.24.10.1365
Fox JC, Cusick S, Scruggs W et al (2007) Educational assessment of medical student rotation in emergency ultrasound. West J Emerg Med 8(3):84–87
Udrea DS, Sumnicht A, Lo D et al (2017) Effects of student-performed point-of-care ultrasound on physician diagnosis and management of patients in the emergency department. J Emerg Med 53(1):102–109. https://doi.org/10.1016/j.jemermed.2017.01.021
Swamy M, Searle RF (2012) Anatomy teaching with portable ultrasound to medical students. BMC Med Educ 12:99. https://doi.org/10.1186/1472-6920-12-99
Tshibwabwa ET, Groves HM (2005) Integration of ultrasound in the education programme in anatomy. Med Educ 39(11):1148. https://doi.org/10.1111/j.1365-2929.2005.02288.x
Stringer MD, Duncan LJ, Samalia L (2012) Using real-time ultrasound to teach living anatomy: an alternative model for large classes. N Z Med J 125(1361):37–45
Griksaitis MJ, Sawdon MA, Finn GM (2012) Ultrasound and cadaveric prosections as methods for teaching cardiac anatomy: a comparative study. Anat Sci Educ 5(1):20–26. https://doi.org/10.1002/ase.259
Kondrashov P, Johnson JC, Boehm K, Rice D, Kondrashova T (2015) Impact of the clinical ultrasound elective course on retention of anatomical knowledge by second-year medical students in preparation for board exams. Clin Anat 28(2):156–163. https://doi.org/10.1002/ca.22494
Paganini M, Bondì M, Rubini A (2017) Evaluation of chest ultrasound integrated teaching of respiratory system physiology to medical students. Adv Physiol Educ 41(4):514–517. https://doi.org/10.1152/advan.00062.2017
Feilchenfeld Z, Dornan T, Whitehead C, Kuper A (2017) Ultrasound in undergraduate medical education: a systematic and critical review. Med Educ 51(4):366–378. https://doi.org/10.1111/medu.13211
Serrao G, Tassoni M, Magenta-Biasina AM et al (2017) Competency-based medical education studying live anatomy by ultrasound. Int J Med Educ 8:268–269. https://doi.org/10.5116/ijme.595f.b183
Wright SA, Bell AL (2008) Enhancement of undergraduate rheumatology teaching through the use of musculoskeletal ultrasound. Rheumatology 47(10):1564–1566. https://doi.org/10.1093/rheumatology/ken324
Alfageme F, Cerezo E, Fernandez IS, Aguilo R, Vilas-Sueiro A, Roustan G (2016) Introduction of basic dermatologic ultrasound in undergraduate medical education. Ultrasound Int Open 2(4):E136–E139. https://doi.org/10.1055/s-0042-120273
Tshibwabwa ET, Groves HM, Levine MA (2007) Teaching musculoskeletal ultrasound in the undergraduate medical curriculum. Med Educ 41(5):517–518. https://doi.org/10.1111/j.1365-2929.2007.02745.x
Kafer I, Rennie W, Noor A, Pellerito JS (2017) Hunger games: interactive ultrasound imaging for learning gastrointestinal physiology. J Ultrasound Med 36(2):361–365. https://doi.org/10.7863/ultra.16.01048
Panoulas VF, Daigeler AL, Malaweera AS et al (2013) Pocket-size hand-held cardiac ultrasound as an adjunct to clinical examination in the hands of medical students and junior doctors. Eur Heart J Cardiovasc Imaging 14(4):323–330. https://doi.org/10.1093/ehjci/jes140
Komasawa N, Mihara R, Hattori K, Minami T (2016) Evaluation of artery and vein differentiation methods using ultrasound imaging among medical students. Br J Anaesth 117(6):832–833. https://doi.org/10.1093/bja/aew371
Shmueli H, Burstein Y, Sagy I et al (2013) Briefly trained medical students can effectively identify rheumatic mitral valve injury using a hand-carried ultrasound. Echocardiography 30(6):621–626. https://doi.org/10.1111/echo.12122
Decara JM, Kirkpatrick JN, Spencer KT et al (2005) Use of hand-carried ultrasound devices to augment the accuracy of medical student bedside cardiac diagnoses. J Am Soc Echocardiogr 18(3):257–263. https://doi.org/10.1016/j.echo.2004.11.015
Hoppmann R, Hunt P, Louis H et al (2011) Medical student identification of knee effusion by ultrasound. ISRN Rheumatol 2011:874596. https://doi.org/10.5402/2011/874596
Andersen GN, Viset A, Mjølstad OC, Salvesen Ø, Dalen H, Haugen BO (2014) Feasibility and accuracy of point-of-care pocket-size ultrasonography performed by medical students. BMC Med Educ 14(1):156. https://doi.org/10.1186/1472-6920-14-156
Stokke TM, Ruddox V, Sarvari SI, Otterstad JE, Aune E, Edvardsen T (2014) Brief group training of medical students in focused cardiac ultrasound may improve diagnostic accuracy of physical examination. J Am Soc Echocardiogr 27(11):1238–1246. https://doi.org/10.1016/j.echo.2014.08.001
Ruiz-Curiel A, Díaz-Barreda MD, González-Rodríguez M et al (2016) Musculoskeletal ultrasound: an effective tool to help medical students improve joint inflammation detection? Med Ultrason 18(3):294. https://doi.org/10.11152/mu.2013.2066.183.ruz
Walrod BJ, Schroeder A, Conroy MJ et al (2018) Does ultrasound-enhanced instruction of musculoskeletal anatomy improve physical examination skills of first-year medical students? J Ultrasound Med 37(1):225–232. https://doi.org/10.1002/jum.14322
Butter J, Grant TH, Egan M et al (2007) Does ultrasound training boost year 1 medical student competence and confidence when learning abdominal examination? Med Educ 41(9):843–848. https://doi.org/10.1111/j.1365-2923.2007.02848.x
de Vries KD, Brown R, Mazzie J, Jung M-K, Yao SC, Terzella MJ (2018) Effect of ultrasonography on student learning of shoulder anatomy and landmarks. J Am Osteopath Assoc 118(1):34. https://doi.org/10.7556/jaoa.2018.006
Woods R, Wisniewski SJ, Lueders DR, Pittelkow TP, Larson DR, Finnoff JT (2017) Can ultrasound be used to improve the palpation skills of physicians in training? A prospective study. PM&R. https://doi.org/10.1016/j.pmrj.2017.11.016
Parikh T, Czuzak M, Bui N et al (2018) Novel use of ultrasound to teach reproductive system physical examination skills and pelvic anatomy. J Ultrasound Med 37(3):709–715. https://doi.org/10.1002/jum.14408
Ahn JS, French AJ, Thiessen MEW et al (2015) Using ultrasound to enhance medical students’ femoral vascular physical examination skills. J Ultrasound Med 34(10):1771–1776. https://doi.org/10.7863/ultra.15.14.11014
Amini R, Stolz L, Hernandez N et al (2016) Sonography and hypotension: a change to critical problem solving in undergraduate medical education. Adv Med Educ Pract 7:7. https://doi.org/10.2147/AMEP.S97491
Parks AR, Verheul G, LeBlanc-Duchin D, Atkinson P (2015) Effect of a point-of-care ultrasound protocol on the diagnostic performance of medical learners during simulated cardiorespiratory scenarios. CJEM 17(03):263–269. https://doi.org/10.1017/cem.2014.41
Fox JC, Lahham S, Maldonado G et al (2017) Hypertrophic cardiomyopathy in youth athletes: successful screening with point-of-care ultrasound by medical students. J Ultrasound Med 36(6):1109–1115. https://doi.org/10.7863/ultra.16.06044
Bahner DP, Jasne A, Boore S, Mueller A, Cortez E (2012) The ultrasound challenge: a novel approach to medical student ultrasound education. J Ultrasound Med 31(12):2013–2016. https://doi.org/10.7863/jum.2012.31.12.2013
Barsky M, Kushner L, Ansbro M et al (2015) A feasibility study to determine if minimally trained medical students can identify markers of chronic parasitic infection using bedside ultrasound in rural Tanzania. World J Emerg Med 6(4):293. https://doi.org/10.5847/wjem.j.1920-8642.2015.04.008
Lee JB, Tse C, Keown T et al (2017) Evaluation of a point of care ultrasound curriculum for Indonesian physicians taught by first-year medical students. World J Emerg Med 8(4):281. https://doi.org/10.5847/wjem.j.1920-8642.2017.04.006
Heinzow HS, Friederichs H, Lenz P et al (2013) Teaching ultrasound in a curricular course according to certified EFSUMB standards during undergraduate medical education: a prospective study. BMC Med Educ 13(1):84. https://doi.org/10.1186/1472-6920-13-84.26
Prats MI, Royall NA, Panchal AR, Way DP, Bahner DP (2016) Outcomes of an advanced ultrasound elective. J Ultrasound Med 35(5):975–982. https://doi.org/10.7863/ultra.15.06060
Kondrashova T, Lockwood MD (2015) Innovative approach to teaching osteopathic manipulative medicine: the integration of ultrasonography. J Am Osteopath Assoc 115(4):212. https://doi.org/10.7556/jaoa.2015.043
Tokumine J, Matsushima H, Lefor AK, Igarashi H, Ono K (2015) Ultrasound-guided subclavian venipuncture is more rapidly learned than the anatomic landmark technique in simulation training. J Vasc Access 16(2):144–147. https://doi.org/10.5301/jva.5000318
Blackstock U, Munson J, Szyld D (2015) Bedside ultrasound curriculum for medical students: report of a blended learning curriculum implementation and validation. J Clin Ultrasound 43(3):139–144. https://doi.org/10.1002/jcu.22224
Naeger DM, Conrad M, Nguyen J, Kohi MP, Webb EM (2013) Students teaching students. Acad Radiol 20(9):1177–1182. https://doi.org/10.1016/j.acra.2013.04.004
Ahn JS, French AJ, Thiessen MEW, Kendall JL (2014) Training peer instructors for a combined ultrasound/physical exam curriculum. Teach Learn Med 26(3):292–295. https://doi.org/10.1080/10401334.2014.910464
Shapiro RS, Ko PK, Jacobson S (2002) A pilot project to study the use of ultrasonography for teaching physical examination to medical students. Comput Biol Med 32(6):403–409. https://doi.org/10.1016/s0010-4825(02)00033-1
Dickerson J, Paul K, Vila P, Whiticar R (2017) The role for peer-assisted ultrasound teaching in medical school. Clin Teach 14(3):170–174. https://doi.org/10.1111/tct.12541
Denny SP, Minteer WB, Fenning RTH et al (2018) Ultrasound curriculum taught by first-year medical students: a four-year experience in Tanzania. World J Emerg Med 9(1):33. https://doi.org/10.5847/wjem.j.1920-8642.2018.01.005
Hammoudi N, Arangalage D, Boubrit L et al (2013) Ultrasound-based teaching of cardiac anatomy and physiology to undergraduate medical students. Arch Cardiovasc Dis 106(10):487–491. https://doi.org/10.1016/j.acvd.2013.06.002
Webb EM, Cotton JB, Kane K, Straus CM, Topp KS, Naeger DM (2014) Teaching point of care ultrasound skills in medical school. Acad Radiol 21(7):893–901. https://doi.org/10.1016/j.acra.2014.03.001.28
Bell FE, Wilson LB, Hoppmann RA (2015) Using ultrasound to teach medical students cardiac physiology. Adv Physiol Educ 39(4):392–396. https://doi.org/10.1152/advan.00123.2015
Favot M, Courage C, Mantouffel J, Amponsah D (2015) Ultrasound training in the emergency medicine clerkship. West J Emerg Med 16(6):938–942. https://doi.org/10.5811/westjem.2015.9.27290
Sweetman GM, Crawford G, Hird K, Fear MW (2013) The benefits and limitations of using ultrasonography to supplement anatomical understanding. Anat Sci Educ 6(3):141–148. https://doi.org/10.1002/ase.1327
Fox JC, Schlang JR, Maldonado G, Lotfipour S, Clayman RV (2014) Proactive medicine: the “UCI 30”, an ultrasound-based clinical initiative from the University of California, Irvine. Acad Med 89(7):984–989. https://doi.org/10.1097/ACM.0000000000000292
Brascher A-K, Blunk JA, Bauer K, Feldmann R, Benrath J (2014) Comprehensive curriculum for phantom-based training of ultrasound-guided intercostal nerve and stellate ganglion blocks. Pain Med 15(10):1647–1656. https://doi.org/10.1111/pme.12365
Hoppmann RA, Rao VV, Poston MB et al (2011) An integrated ultrasound curriculum (iUSC) for medical students: 4-year experience. Crit Ultrasound J 3(1):1–12. https://doi.org/10.1007/s13089-011-0052-9
Wong I, Jayatilleke T, Kendall R, Atkinson P (2011) Feasibility of a focused ultrasound training programme for medical undergraduate students. Clin Teach 8(1):3–7. https://doi.org/10.1111/j.1743-498X.2010.00416.x
Cawthorn TR, Nickel C, O’Reilly M et al (2014) Development and evaluation of methodologies for teaching focused cardiac ultrasound skills to medical students. J Am Soc Echocardiogr 27(3):302–309. https://doi.org/10.1016/j.echo.2013.12.006
Hope MD, de la Pena E, Yang PC, Liang DH, McConnell MV, Rosenthal DN (2003) A visual approach for the accurate determination of echocardiographic left ventricular ejection fraction by medical students. J Am Soc Echocardiogr 16(8):824–831. https://doi.org/10.1067/S0894-7317(03)00400-0
Galusko V, Khanji MY, Bodger O, Weston C, Chambers J, Ionescu A (2017) Handheld ultrasound scanners in medical education: a systematic review. J Cardiovasc Ultrasound 25(3):75. https://doi.org/10.4250/jcu.2017.25.3.75
Dinh VA, Dukes WS, Prigge J, Avila M (2015) Ultrasound integration in undergraduate medical education: comparison of ultrasound proficiency between trained and untrained medical students. J Ultrasound Med 34(10):1819–1824. https://doi.org/10.7863/ultra.14.12045
Mandavia DP, Aragona J, Chan L, Chan D, Henderson SO (2000) Ultrasound training for emergency physicians—a prospective study. Acad Emerg Med 7(9):1008–1014. https://doi.org/10.1111/j.1553-2712.2000.tb02092.x
Gogalniceanu P, Sheena Y, Kashef E, Purkayastha S, Darzi A, Paraskeva P (2010) Is basic emergency ultrasound training feasible as part of standard undergraduate medical education? J Surg Educ 67(3):152–156. https://doi.org/10.1016/j.jsurg.2010.02.008
Yoo MC, Villegas L, Jones DB (2004) Basic ultrasound curriculum for medical students: validation of content and phantom. J Laparoendosc Adv Surg Tech A 14(6):374–379. https://doi.org/10.1089/lap.2004.14.374
Nguyen HB, Losey T, Rasmussen J et al (2006) Interrater reliability of cardiac output measurements by transcutaneous Doppler ultrasound: implications for noninvasive hemodynamic monitoring in the ED. Am J Emerg Med 24(7):828–835. https://doi.org/10.1016/j.ajem.2006.05.012
Hoppmann R, Cook T, Hunt P et al (2006) Ultrasound in medical education: a vertical curriculum at the University of South Carolina School of Medicine. J S C Med Assoc 102(10):330–334
Angtuaco TL, Hopkins RH, DuBose TJ, Bursac Z, Angtuaco MJ, Ferris EJ (2007) Sonographic physical diagnosis 101: teaching senior medical students basic ultrasound scanning skills using a compact ultrasound system. Ultrasound Q 23(2):157–160. https://doi.org/10.1097/01.ruq.0000263847.00185.28
Afonso N, Amponsah D, Yang J et al (2010) Adding new tools to the black bag—introduction of ultrasound into the physical diagnosis course. J Gen Intern Med 25(11):1248–1252. https://doi.org/10.1007/s11606-010-1451-5
Cheng W-C, Lin X-Z, Chen C-Y (2013) Using modern teaching strategies to teach upper abdominal sonography to medical students. J Chin Med Assoc 76(7):395–400. https://doi.org/10.1016/j.jcma.2013.03.011
Oveland NP, Lossius HM, Aagaard R, Connolly J, Sloth E, Knudsen L (2013) Animal laboratory training improves lung ultrasound proficiency and speed. J Emerg Med 45(3):e71–e78. https://doi.org/10.1016/j.jemermed.2013.03.029
Krause C, Krause R, Krause R, Gomez N, Jafry Z, Dinh VA (2017) Effectiveness of a 1-hour extended focused assessment with sonography in trauma session in the medical student surgery clerkship. J Surg Educ 74(6):968–974. https://doi.org/10.1016/j.jsurg.2017.03.007
Kobal SL, Lior Y, Ben-Sasson A, Liel-Cohen N, Galante O, Fuchs L (2017) The feasibility and efficacy of implementing a focused cardiac ultrasound course into a medical school curriculum. BMC Med Educ 17(1):94. https://doi.org/10.1186/s12909-017-0928-x
Syperda VA, Trivedi PN, Melo LC et al (2008) Ultrasonography in preclinical education: a pilot study. J Am Osteopath Assoc 108(10):601–605
Fernández-Frackelton M, Peterson M, Lewis RJ, Pérez JE, Coates WC (2007) A bedside ultrasound curriculum for medical students: prospective evaluation of skill acquisition. Teach Learn Med 19(1):14–19. https://doi.org/10.1080/10401330709336618
Ang J, Doyle B, Allen P, Cheek C (2017) Teaching bedside ultrasound to medical students. Clin Teach. https://doi.org/10.1111/tct.12692
Kim S-C, Hauser S, Staniek A, Weber S (2014) Learning curve of medical students in ultrasound-guided simulated nerve block. J Anesth 28(1):76–80. https://doi.org/10.1007/s00540-013-1680-y
Griswold-Theodorson S, Hannan H, Handly N et al (2009) Improving patient safety with ultrasonography guidance during internal jugular central venous catheter placement by novice practitioners. Simul Healthc 4(4):212–216. https://doi.org/10.1097/SIH.0b013e3181b1b837
Moak JH, Rajkumar JS, Woods WA (2013) The wire is really easy to see (WIRES): sonographic visualization of the guidewire by novices. CJEM 15(1):18–23. https://doi.org/10.2310/8000.2012.120800
Breslin R, Collins K, Cupitt J (2018) The use of ultrasound as an adjunct to peripheral venous cannulation by junior doctors in clinical practice. Med Teach. https://doi.org/10.1080/0142159X.2018.1428737
Heiberg J, Hansen L, Wemmelund K et al (2015) Point-of-care clinical ultrasound for medical students. Ultrasound Int Open 01(02):E58–E66. https://doi.org/10.1055/s0035-1565173
Barrington MJ, Viero LP, Kluger R, Clarke AL, Ivanusic JJ, Wong DM (2016) Determining the learning curve for acquiring core sonographic skills for 33 ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med 41(6):667–670. https://doi.org/10.1097/AAP.0000000000000487
Vitto MJ, Myers M, Vitto CM, Evans DP (2016) Perceived difficulty and success rate of standard versus ultrasound-guided peripheral intravenous cannulation in a novice study group. J Ultrasound Med 35(5):895–898. https://doi.org/10.7863/ultra.15.06057
Hoyer R, Means R, Robertson J et al (2016) Ultrasound-guided procedures in medical education: a fresh look at cadavers. Intern Emerg Med 11(3):431–436. https://doi.org/10.1007/s11739-015-1292-7
Amini R, Stolz LA, Breshears E et al (2016) Assessment of ultrasound-guided procedures in preclinical years. Intern Emerg Med 12(7):1–7. https://doi.org/10.1007/s11739-016-1525-4
The Accreditation Council for Graduate Medical Education (ACGME) Web site. https://www.acgme.org/. Accessed 26 April 2022
Dinh VA, Fu JY, Lu S, Chiem A, Fox JC, Blaivas M (2016) Integration of ultrasound in medical education at United States medical schools: a national survey of directors’ experiences. J Ultrasound Med 35(2):413–419. https://doi.org/10.7863/ultra.15.05073
Dinh VA, Frederick J, Bartos R, Shankel TM, Werner L (2015) Effects of ultrasound implementation on physical examination learning and teaching during the first year of medical education. J Ultrasound Med 34(1):43–50. https://doi.org/10.7863/ultra.34.1.43
Dinh VA, Lakoff D, Hess J et al (2016) Medical student core clinical ultrasound milestones: a consensus among directors in the United States. J Ultrasound Med 35(2):421–434. https://doi.org/10.7863/ultra.15.07080
Steinmetz P, Dobrescu O, Oleskevich S, Lewis J (2016) Bedside ultrasound education in Canadian medical schools: a national survey. Can Med Educ J 7(1):e78–e86
Wakefield RJ, Weerasinghe A, Tung P et al (2018) The development of a pragmatic, clinically driven ultrasound curriculum in a UK medical school. Med Teach 40(6):600–606. https://doi.org/10.1080/0142159X.2018.1439579
Baltarowich OH, Di Salvo DN, Scoutt LM et al (2014) National ultrasound curriculum for medical students. Ultrasound Q 30(1):13–19. https://doi.org/10.1097/RUQ.0000000000000066
Lomis K, Amiel JM, Ryan MS et al (2017) Implementing an entrustable professional activities framework in undergraduate medical education: early lessons from the AAMC core entrustable professional activities for entering residency pilot. Acad Med 92(6):765–770. https://doi.org/10.1097/ACM.0000000000001543
Chen HC, McNamara M, Teherani A, Cate OT, O’Sullivan P (2016) Developing entrustable professional activities for entry into clerkship. Acad Med 91(2):247–255. https://doi.org/10.1097/ACM.0000000000000988
Patel SG, Benninger B, Mirjalili SA (2017) Integrating ultrasound into modern medical curricula. Clin Anat 30(4):452–460. https://doi.org/10.1002/ca.22864
So S, Patel RM, Orebaugh SL (2017) Ultrasound imaging in medical student education: impact on learning anatomy and physical diagnosis. Anat Sci Educ 10(2):176–189. https://doi.org/10.1002/ase.1630
Alpert JS, Mladenovic J, Hellmann DB (2009) Should a hand-carried ultrasound machine become standard equipment for every internist? Am J Med 122(1):1–3. https://doi.org/10.1016/j.amjmed.2008.05.013
AIUM practice parameter for the performance of point-of-care ultrasound examinations (2019) J Ultrasound Med 38(4):833–849. https://doi.org/10.1002/jum.14972
American Society of Echocardiography Web site. https://www.asecho.org/. Accessed 26 April 2022
Society of Critical Care Medicine Web site. https://www.sccm.org/Home. Accessed 26 April 2022
Via G, Hussain A, Wells M et al (2014) International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr 27(7):683.e1-683.e33. https://doi.org/10.1016/j.echo.2014.05.001
Volpicelli G, Elbarbary M, Blaivas M et al (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38(4):577–591. https://doi.org/10.1007/s00134-012-2513-4
Dancel R, Schnobrich D, Puri N et al (2018) Recommendations on the use of ultrasound guidance for adult thoracentesis: a position statement of the society of hospital medicine. J Hosp Med 13(2):126–135. https://doi.org/10.12788/jhm.2940
American Academy of Family Physicians (AAFP). Recommended curriculum guidelines for family medicine residents: point-of-care ultrasound. https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf. Published December 2016. Accessed 26 April 2022
POCUS Certificate of Completion. Society of Hospital Medicine Web site. https://www.hospitalmedicine.org/clinical-topics/ultrasound/pocus-certificate-of-completion/. Accessed 26 April 2022
Point-of-care ultrasound for internal medicine. American College of Physicians Web site. https://www.acponline.org/meetings-courses/focused-topics/point-of-care-ultrasound-pocus-for-internal-medicine. Accessed 26 April 2022
Celebi N, Griewatz J, Malek NP et al (2019) Development and implementation of a comprehensive ultrasound curriculum for undergraduate medical students. BMC Med Educ 19(1):170. https://doi.org/10.1186/s12909-019-1611-1
Standards and guidelines for the accreditation of educational programs in diagnostic medical sonography. Commission on Accreditation of Allied Health Education Programs. https://www.caahep.org/CAAHEP/media/CAAHEP-Documents/CAAHEPStandards-DMS-approved9182020.pdf. Published 2020. Accessed 26 April 2022
Ultrasound in medical education. World interactive network focused on critical ultrasound Web site. https://www.winfocus.org/unltrasaound-on-medical-education/. Accessed 26 April 2022
Medical education portal. American Institute of Ultrasound in Medicine Web site. http://meded.aium.org. Accessed 26 April 2022
Scanning videos. Society of ultrasound in medical education web site. https://www.susme.org/. Accessed 26 April 2022
World federation for ultrasound in medicine and biology web site. https://wfumb.info/. Accessed 26 April 2022
American Society of Echocardiography Web site. https://www.asecho.org. Accessed 26 April 2022
Back to bedside. The Accreditation Council for Graduate Medical Education (ACGME) Web site. https://www.acgme.org/residents-and-fellows/back-to-bedside/. Accessed 26 April 2022
Hussain A, Via G, Melniker L et al (2020) Multi-organ point-of-care ultrasound for COVID-19 (PoCUS4COVID): international expert consensus. Crit Care 24(1):702. https://doi.org/10.1186/s13054-020-03369-5
Bahner DP, Blickendorf JM, Bockbrader M et al (2016) Language of transducer manipulation: codifying terms for effective teaching. J Ultrasound Med 35(1):183–188. https://doi.org/10.7863/ultra.15.02036
Garofalo E, Bruni A, Pelaia C et al (2019) Comparisons of two diaphragm ultrasound-teaching programs: a multicenter randomized controlled educational study. Ultrasound J 11(1):21. https://doi.org/10.1186/s13089-019-0137-4
Bauman B, Kernahan P, Weinhaus A, Walker MJ, Irwin E, Sundin A, Yerxa D, Vakayil V, Harmon JV (2021) An interprofessional senior medical student preparation course: improvement in knowledge and self-confidence before entering surgical training. Adv Med Educ Pract 7(12):441–451. https://doi.org/10.2147/AMEP.S287430
Lamba S, Wilson B, Natal B, Nagurka R, Anana M, Sule H (2016) A suggested emergency medicine boot camp curriculum for medical students based on the mapping of core entrustable professional activities to emergency medicine level 1 milestones. Adv Med Educ Pract 1(7):115–124. https://doi.org/10.2147/AMEP.S97106
Fu JY, Krause C, Krause R, Mccoy J, Schindler A, Udrea DS, Villarreal LA, Jafry Z, Dinh VA (2016) Integration of point-of-care ultrasound training into undergraduate medical curricula—a perspective from medical students. J Med Educ Curric Dev 3:JMECD.S38240. https://doi.org/10.4137/JMECD.S38240
Wolf R, Geuthel N, Gnatzy F, Rotzoll D (2019) Undergraduate ultrasound education at German-speaking medical faculties: a survey. GMS J Med Educ 36(4):Doc34. https://doi.org/10.3205/zma001242
Ma IWY, Steinmetz P, Weerdenburg K et al (2020) The Canadian medical student ultrasound curriculum: a statement from the Canadian ultrasound consensus for undergraduate medical education group. J Ultrasound Med 39(7):1279–1287. https://doi.org/10.1002/jum.15218
Rajendram R, Alrasheed AO, Boqaeid AA, Alkharashi FK, Qasim SS, Hussain A (2022) Training medical students in physical examination and point-of-care ultrasound: an assessment of the needs and barriers to acquiring skills in point-of-care ultrasound. J Family Community Med 29(1):62–70. https://doi.org/10.4103/jfcm.jfcm_369_21
Johri AM, Durbin J, Newbigging J et al (2018) Cardiac point-of-care ultrasound: state-of-the-art in medical school education. J Am Soc Echocardiogr 31(7):749–760. https://doi.org/10.1016/j.echo.2018.01.014
Dietrich CF, Hoffmann B, Abramowicz J et al (2019) Medical student ultrasound education: a WFUMB position paper, part I. Ultrasound Med Biol 45(2):271–281. https://doi.org/10.1016/j.ultrasmedbio.2018.09.017
Hoffmann B, Blaivas M, Abramowicz J, Bachmann M, Badea R et al (2020) Medical student ultrasound education, a WFUMB position paper, part II. A consensus statement of ultrasound societies. Med Ultrason 22(2):220–229. https://doi.org/10.11152/mu-2599
Cantisani V, Dietrich CF, Badea R et al (2016) EFSUMB statement on medical student education in ultrasound [long version]. Ultrasound Int Open 2(1):E2–E7. https://doi.org/10.1055/s-0035-1569413
Acknowledgements
The following individual ultrasound experts participated as consultants adding significant value to the consensus process and validity of the recommendations. Their expert contributions are greatly appreciated. They are listed alphabetically with their primary affiliation.
Reem S. Abu-Rustum, University of Florida College of Medicine; Srikar Adhikari, University of Arizona; Abdulmohsen Alsaawi, College of Medicine, King Saud Bin Abdulaziz University for Health Sciences; Keith Boniface, The George Washington University; Janice Boughton, CHAS health; James F. Catroppo, University of South Carolina School of Medicine Columbia; Adj A/P Hong Chuen, Khoo Teck Puat Hospital; Chiara Cogliati, University of Milan; José L. Díaz-Gómez, Baylor College of Medicine; Pradeep Dcosta, Sahyadri Hospital; Rebecca J. Etheridge, Medical College of Georgia at Augusta University; Ryan C. Gibbons, Lewis Katz School of Medicine at Temple University; Laleh Gharahbaghian, Stanford School of Medicine; Alberto Goffi, University of Toronto and St. Michael’s Hospital; Ramesh Gopalakrishan, Oceania University of Medicine; Serge Goulet, University of Sherbrooke; Geoffrey D. Guttmann, Texas Tech University Health Science Center El Paso; Young-Rock Ha, Seongnam Citizens Medical Center; Christine A Kauffman, University of Central Florida College of Medicine; Joseph Minardi, West Virginia University School of Medicine; Marcello Montomoli, Azienda USL Toscana Sud-Est; Jason T Nomura, Christiana Care Health System; Francisco Norman, Orlando Health; Alberto Oviedo-Garcia, Sevilla University; Philippe Pès, CHU de NANTES; Mary Beth Poston, University of South Carolina School of Medicine Columbia; Narayana G Prasad, Brigham and Women Hospital; Felipe de Jesús Montelongo, Universidad Autónoma del Estado de México; Chavez-Peña Quetzalcoatl, University of Guadalajara; Aarti Sarwal, Atrium Wake Forest School of Medicine; Eman Sobh, Al-Azhar University, Ana Claudia Tonelli, UNISINOS University, School of medicine; Patrick Tung, University of Leeds, School of Medicine; Julie Christie G. Visperas, University of Santo Tomas; Dr Shaik Farid Abdull Wahab, Universiti Sains Malaysia; Connie Willis, Baptist Health Sciences University.
Special acknowledgement
Mahmoud Elbarbary, MD [MBBH], PhD, MSc, EDIC – Professor of Critical Care Medicine at King Saud Bin Abdulaziz College of Medicine and Consultant Pediatric Intensivist in the Department of Cardiac Sciences at King Abdulaziz Cardiac Center in Riyadh, Saudi Arabia; Assistant Professor at McMaster University in Hamilton, Ontario, Canada; and Clinical Associate Professor at University of South Carolina in Columbia. Through his work at McMaster University and the DECIDE Research Group at Stockholm University, Dr Elbarbary played a critical role in developing the methodologies and the planning of the World Interactive Network Focused on Critical Ultrasound (WINFOCUS) International Consensus Conference Series and was an international leader for point-of-care ultrasound for many years until his untimely death in 2017.
Funding
There was no funding support for this research.
Author information
Authors and Affiliations
Contributions
All authors actively participated in the consensus process over an extended period of four years significantly contributing to the success and validity of the consensus process and writing of the manuscript. Participation included multiple profile surveys, participating in face-to-face international conference meetings, online voting, providing written and oral input critical to the final consensus recommendations and manuscript discussion. All authors reviewed the manuscript at least twice providing input and final approval of the submitted manuscript. Primary writing of the manuscript was performed by RH, JM, and LM. Strategic planning and oversite of the entire process was provided by the Steering Committee which included RB, MB, MM, AA, RH, JM, and LM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Office of Research Compliance of the University of South Carolina Institutional Review Board reviewed and approved this study.
Consent for publication
Not applicable.
Competing interests
The only authors declaring competing interests are listed below with their corresponding disclosure. All other authors declare that they have no competing interests. Richard Hoppmann, Patent Royalties on University of South Carolina license with EchoNous. Jeanette Mladenovic, Medical Advisory Board for EchoNous. Michael Blaivas, Consulting for Anavasi Diagnostics, Mendaera, and Intuitap. Bret P. Nelson, Medical Advisory Boards of DIA Imaging Analysis Ltd and EchoNous. Keith Reeves Barron Jr, Medical Advisory Board for EchoNous. Renee K Dversdal, Serves as Chief Medical Officer for Vave Health. David Tierney, Medical Advisory Board for EchoNous. James W. Tsung, Consultant for GE Healthcare and DIA Imaging Analysis Ltd. Paula Nocera, Associate on Cardiopriori Learning Platform. Rachel Liu, Consultant for Philips Healthcare and Caption Health and Medical Advisory Board for POCUSPro. Maxime Valois, Founding Partner in Sonoscope/EGLS Courses. Jean-Francois Lanctot, Founding Partner in Sonoscope/EGLS Courses. Resa E Lewiss, Medical Advisory Board for EchoNous. Kevin Bergman, Partner in Global Ultrasound Institute. Ximena Wortsman, Speaker Bureau of AbbVie.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix S1.
International Consensus Conference Statements, Rationale, and References for Domains 1-3.
Additional file 2: Appendix S2.
Recommended medical student ultrasound curricular content.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hoppmann, R.A., Mladenovic, J., Melniker, L. et al. International consensus conference recommendations on ultrasound education for undergraduate medical students. Ultrasound J 14, 31 (2022). https://doi.org/10.1186/s13089-022-00279-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13089-022-00279-1