Abstract
Background
Rheumatoid arthritis (RA) patients sometimes exhibit different levels of improvement in health assessment questionnaire-disability index (HAQ-DI) and subjective pain visual analogue score (VAS) even after achieving low disease activities (LDA). This study aimed to identify factors associated with improvement in HAQ-DI and pain VAS among those who achieved LDA.
Methods
Data of the FIRST registry, a multi-institutional cohort of RA patients treated with biological and targeted-synthetic DMARDs (b/tsDMARDs) were analyzed. Patients who were enrolled from August 2013 to February 2023 and who achieved clinical LDA [clinical disease activity index (CDAI) ≤ 10.0] at 6 months after starting treatment were included. Multiple logistic regression analyses were conducted to identify the factors that associated with achieving HAQ-DI normalization (< 0.5), HAQ-DI improvement (by > 0.22), or pain VAS reduction (≤ 40 mm).
Results
Among 1424 patients who achieved LDA at 6 months, 732 patients achieved HAQ-DI normalization and 454 achieved pain VAS reduction. The seropositivity and the use of JAK inhibitor compared with TNF inhibitor were associated with both HAQ-DI < 0.5 and pain VAS reduction at 6 months. On the other hand, older age, past failure in ≥ 2 classes of b/tsDMARDs, higher HAQ-DI at baseline, and use of glucocorticoid were associated with the lower likelihood of HAQ-DI normalization and pain VAS reduction. Longer disease duration, being female, and higher disease activity at baseline was negatively associated HAQ-DI normalization alone. Comorbidities were not associated with the outcomes.
Conclusions
These results suggest some preferable treatment may exist for improvement of HAQ-DI and pain VAS reduction in the early stage of the treatment, which is a clue to prevention of a criteria of difficult-to-treat RA.
Similar content being viewed by others
Introduction
Recent advances in the treatment of rheumatoid arthritis (RA) have dramatically improved the clinical and functional outcomes of the patients. A majority of RA patients now can achieve low disease activity (LDA) measured by parameters such as clinical disease activity index (CDAI), simplified disease activity index (SDAI), and disease activity score (DAS).
Nevertheless, some patients exhibit persistent symptoms even after achieving LDA, which is a part of the category of difficult-to-treat RA (D2T RA) by the European League Against Rheumatism (EULAR) [1] described as “well-controlled disease according to the above (universal) standards, but still having RA symptoms that are causing a reduction in quality of life”. A previous study reported that 35% of patients who achieved a moderate to good EULAR response did not consider their health to have improved a year after the treatment [2]. Another study showed that about one-fifth of patients with well-controlled disease activity do not feel well, determined subjectively [3], which can be a barrier to achieving the goal of treat-to-target.
Even though RA patients achieve LDA, persistent functional disability measured by high health assessment questionnaire-disability index (HAQ-DI) scores is often observed. In a previous cohort study, 10.9% of RA patients with persistently LDA had poor HAQ-DI scores [4]. Socioeconomic status, lifestyle, and social support [5] are also associated with higher HAQ-DI scores. However, these results might be partly due to less intensive treatment, which is often employed for patients with comorbidities and age-related physical dysfunction [6]. To exclude the contributions of differences in treatment intensity to disease activity measures, it is important to focus only on patients who are receiving sufficiently intensive treatment.
Here we analyzed the factors that are associated with the improvement of HAQ-DI and subjective pain of patients who achieved LDA by treatment with biological and targeted-synthetic (b/ts) disease-modifying antirheumatic drugs (DMARDs). The results of this study will inform the prevention of residual symptoms of RA patients and methods to optimize treat-to-target approaches.
Methods
Data source
The FIRST Registry is a multi-institutional cohort of RA patients treated with b/tsDMARDs, established by the University of Occupational and Environmental Health, Japan, and its multiple affiliated hospitals. Details of the cohort are available in other articles [7,8,9,10]. In this registry, all registered RA patients were enrolled in a long-term observational study at the time of receiving a new prescription or switching prescriptions of b/tsDMARDs. If a patient was treated with several b/tsDMARDs, each episode was treated as an independent episode.
By February 2023, 4842 patients were enrolled in the registry. In this study, b/tsDMARDs with the following four different mechanisms of action (classes) were included:
-
Tumor necrosis factor inhibitors (TNFis): infliximab and its biosimilars, etanercept and its biosimilars, adalimumab and its biosimilars, golimumab, certolizumab pegol, and ozoralizumab.
-
Interleukin-6 receptor inhibitors (IL-6Ris): tocilizumab, sarilumab, clazakizumab, and sirukumab.
-
Cytotoxic T-lymphocyte–associated antigen-4 immunoglobulin (CTLA4-Ig): abatacept.
-
Janus kinase inhibitors (JAKis): tofacitinib, baricitinib, peficitinib, and upadacitinib.
Rituximab was not included in this study because this drug was not yet approved by the Japanese government as a treatment option for RA. Clazakizumab and sirukumab were not included as new (current) prescription because they were still under testing.
At the start of b/tsDMARD treatment, baseline data were collected for all patients including demographics, disease duration, titers of rheumatoid factor (RF) and anti-cyclic citrullinated protein (anti-CCP) antibody, present and past treatments, serum creatinine levels, coexistence of interstitial lung disease (ILD), and past history of fractures and cancer. Measures of disease activity (CDAI, SDAI, DAS), functional status (HAQ-DI), duration of morning stiffness (MS), pain visual analogue scale (VAS), patients’ global health (GH), and evaluators’ global assessment (EGA), were also collected. Follow-up data on disease activity were collected at 6 months and one year after the start of therapy.
Eligibility criteria
As the outcomes of treatment may differ when the treatment options are limited, this study included only patients who were enrolled in the FIRST Registry after JAKis were first approved in Japan, i.e., after August 2013. For the analysis of HAQ-DI improvement, patients with LDA (CDAI ≤ 10.0) at 6 months after starting treatment were included for further analyses.
Exclusion criteria
Patients whose HAQ-DI data were not available at 6 months after starting treatment were excluded. To remove patients who received b/tsDMARDs as treatment for other autoimmune diseases (e.g., interstitial lung disease or vasculitis), patients treated with a > 15 mg/day prednisolone equivalent dose of glucocorticoids (GC) were excluded from the analysis. Patients who stopped treatment within 6 months were excluded for further analysis, but information about the reasons for the treatment cessation were collected.
Definition of clinical and functional parameters
The following definitions were employed as indicators of clinical and functional improvement.
-
Clinical LDA: CDAI ≤ 10.0 at 6 months.
-
HAQ-DI normalization: HAQ-DI < 0.5 at 6 months, which is defined in a previous study [11].
-
HAQ-DI improvement: improvement in HAQ-DI by > 0.22 units within 6 months, which is used in practice and in many other studies as a minimal clinically-important difference [4, 12,13,14].
-
Pain VAS reduction: reduction in the pain VAS by ≥ 40 mm, which is considered to be a clinically relevant change [15], within 6 months.
-
The changes in each clinical parameter within 6 months were calculated as follows:
Δvalue = (value at week 0) – (value at 6 months)
-
Glucose intolerance: hemoglobin (Hb) A1c > 6.5% or fasting blood glucose of > 200 mg/dL at week 0.
-
Overweight and obesity: body mass index (BMI) > 25 and > 30, respectively.
-
Chronic kidney disease (CKD): Estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73 m2. eGFR was calculated using the following formula:
Statistical analysis
Simple comparison of patient background
The baseline data of the patients who achieved functional and pain improvement (HAQ-DI normalization, HAQ-DI improvement, and Pain VAS reduction) and the patients who did not were compared. The Student’s t-test was used for numerical variables and the chi-square test for categorical variables.
Multiple regression analysis
Factors associated with HAQ-DI normalization, HAQ-DI improvement, and pain VAS reduction at 6 months and one year after starting treatment were analyzed using multiple logistic regression. Sensitivity analyses were conducted including only the patients whose disease duration was < 5 years. Another sensitivity analyses was performed including only the patients who achieved CDAI remission (< 2.8).
As there are many factors that may confound each other, the degree of multicollinearity was detected by determining the variance inflation factor (VIF). A value of less than 5 indicated that the correlation was not severe enough to require modification.
To determine which clinical symptoms had the greatest impact on the improvement of HAQ-DI, the associations between the HAQ-DI improvement and the change in each clinical value i.g. pain VAS, tender joint count (TJC), swollen joint count (SJC), GH, duration of MS, titer of erythrocyte sedimentation rate (ESR), and EGA were analyzed by simple comparisons and multiple logistic regression.
These statistical analyses were carried out using Stata/SE 16.0 (StataCorp LLC, College Station, TX, USA). P-values of < 0.05 were considered to be statistically significant.
Results
By February 2023, 4843 patients were enrolled in the FIRST Registry, of which 147 patients were treated with a > 15 mg/day prednisolone equivalent dose of GC. Another 1861 patients were enrolled before August 2013 when a JAK inhibitor was launched here and thus were excluded from this study. Within 6 months, 387 patients stopped treatment and the CDAI values at 6 months were missing for 620 patients. Among the remaining 1827 patients, 1474 achieved LDA (CDAI ≤ 10.0) at 6 months. The treatment outcomes of those who achieved LDA and those who did not are shown in Table 1. In total, 42.7% of patients (49.7% of patients with CDAI ≤ 10.0 and 13.1% of patients with CDAI > 10.0) achieved LDA. After excluding the patients whose HAQ-DI scores were not available (N = 22), 732 patients who achieved HAQ-DI < 0.5 and 692 patients who did not were included for further analyses (Fig. 1A). Patterns of treatment switching are shown in Fig. 1B.
To show the heterogeneity of patients by treatment types, the backgrounds and treatment outcomes and a breakdown of the reasons for treatment cessation by class of b/tsDMARDs were shown in Additional file 1 and Additional file 2, respectively. Although there was a significant heterogeneity in the background, the proportion of patients who achieved CDAI ≤ 10.0 did not significantly differ between drug types. Proportion of adverse events were small and did not seem to differ between drug types.
Background of the patients
The background of the included patients is shown in Table 2. All factors except the mean BMI, the titers of RF and anti-CCP antibody, and the proportion of glucose intolerance showed significant differences between the HAQ-DI normalization and non-normalization groups.
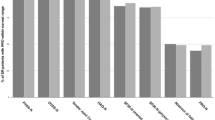
Pre-treatment factors associated with HAQ-DI normalization (< 0.5) at 6 months
Multiple logistic regression analysis was conducted to identify the factors associated with HAQ-DI normalization (< 0.5) at 6 months (Fig. 2, left column and Additional file 3). Age, sex, disease duration, coexisting diseases, refractory status to past DMARDs, RA-related status at week 0, the class of b/tsDMARD, and the concomitant use of methotrexate (MTX) and GC were employed as explanatory factors in this analysis. The seropositivity of RF or anti-CCP antibody [odds ratio (OR) 2.10, 95% confidence interval (CI) 1.42–3.12] and the use of JAKi compared with the use of TNFi (OR 2.52, 95%CI 1.52–4.18) were associated with the normalization. On the other hand, older age, longer disease duration, being female (OR 0.45, 95% CI 0.30–0.67), past failure in ≥ 2 classes of b/tsDMARDs (OR 0.46, 95% CI 0.32–0.68), the use of GC (OR 0.92, 95% CI 0.86–0.99), higher HAQ-DI at week 0 (OR 0.17, 95% CI 0.13–0.22), MDA and HDA at week 0 compared with LDA (OR 0.36, 95% CI 0.19–0.70 and OR 0.36, 95% CI 0.17–0.75, respectively) were associated with a lower likelihood of HAQ-DI normalization. The same analysis was conducted with outcome of HAQ-DI normalization at 1 year (Additional file 4). Similar tendency was observed, though the association was no more significant in the use of JAKi and GC.
Sensitivity analyses were applied to the patients with a disease duration of < 5 years (Additional file 5) and the who achieved CDAI remission (< 2.8) at 6 months (Additional files 6). Older age, longer disease duration, being female and past failure in ≥ 2 classes of b/tsDMARDs remained to be associated with lower likelihood of HAQ-DI improvement. However, the association was no more significant in the use of GC.
As the differences in HAQ-DI between patients with seropositivity or seronegativity of the RF and anti-CCP may reflect differences in the background of the patients, the backgrounds and outcome values were compared between seropositive and seronegative patients (Additional file 7). Seropositive patients were of older age, with longer disease durations, lower BMI values, higher eGFR values, and lower doses of GC compared with seronegative patients. On average, the seropositive patients showed higher HAQ-DI and DAS28-ESR scores at 6 months. However, the proportion of pain VAS reduction was also higher among the seropositive patients.
Factors associated with HAQ-DI improvement
HAQ-DI normalization at 6 months may have been due to low HAQ-DI scores at the start of the treatment, the factors associated with a significant improvement in HAQ-DI (by ≥ 0.22 units) were also analyzed (Fig. 2, middle column and Additional file 8). In total, 839 patients (59%) showed improvement of HAQ-DI scores. Multiple logistic regression analysis showed that seropositivity of RF and anti-CCP antibody (OR 1.86, 95% CI 1.27–2.72), higher HAQ-DI at baseline (OR 3.93, 95% CI 3.01–5.15), and the use of JAKi compared with the use of TNFi (OR 2.26, 95% CI 1.38 − 3.71) were associated with HAQ-DI improvement. On the other hand, an age of ≥ 80 years compared with an age of < 40 years (OR 0.26, 95% CI 0.11–0.59), a longer disease duration, a past history of fracture (OR 0.51, 95% CI 0.33–0.78), and the use of GC (OR 0.91, 95% CI 0.85–0.97) were associated with a lower likelihood of HAQ-DI improvement.
The proportion of patients with HAQ-DI improvement, among those who achieved LDA, might be affected by the proportion of LDA achievement with each drug class or each age group. However, the proportions of patients with LDA versus MDA-HDA at 6 months were not significantly different between the treatment classes (Additional file 1) and age groups (Additional file 9).
Factors associated with pain VAS reduction
Among the 1424 patients who achieved LDA, 454 (31.8%) achieved pain VAS reduction (≥ 40 mm) at 6 months. Multiple logistic regression analysis was conducted to identify the factors associated with pain VAS reduction (Fig. 2, right column and Additional file 10). Seropositivity of RF or anti-CCP antibody (OR 2.00, 95% CI 1.25 − 3.22), the use of JAKi compared with the use of TNFi (OR 1.80, 95% CI 1.00–3.24), and higher pain VAS scores at baseline (OR 1.10, 95% CI 1.09–1.12 for a 1 mm increase in pain VAS) were associated with pain VAS reduction. On the other hand, an age of ≥ 80 years compared with an age of < 40 years (OR 0.32, 95% CI 0.12–0.89), a past history of fracture (OR 0.44, 95% CI 0.26–0.75), the failure of ≥ 2 classes of b/tsDMARD (OR 0.45, 95% CI 0.29–0.72), the use of GC (OR 0.92, 95% CI 0.85–0.99), and a higher HAQ-DI score at baseline (OR 0.72, 95%CI 0.55–0.95) were associated with a lower likelihood of pain VAS reduction. The same analysis was conducted with outcome of pain VAS reduction at 1 year (Additional file 11). In this phase, only higher pain VAS at baseline and the failure of ≥ 2 classes of b/tsDMARD were associated with a lower likelihood of the reduction.
For sensitivity analyses, the same regression models used for Additional file 10 were applied to the patients with a disease duration of < 5 years (Additional file 12) and the who achieved CDAI remission (< 2.8) (Additional file 13). The similar tendency was observed, though the association with the use of GC was no more observed.
Post-treatment factors associated with HAQ-DI improvement
As HAQ-DI improvement status is affected by a variety of clinical symptoms, we analyzed the association between the changes in clinical variables (pain VAS, TJC, SJC, GH, MS, ESR, EGA) and HAQ-DI improvement (Table 3). All clinical variables improved more among the HAQ-DI improvement group compared with the non-improvement group. When logistic regression was conducted, improvements in the pain VAS, GH, and ESR were significantly associated with HAQ-DI improvement.
To detect collinearity of the explanatory factors, the VIF was calculated (Additional file 14). No factor showed a VIF > 5 and thus all factors were included in the analysis.
Discussion
This study analyzed the factors associated with improvement of HAQ-DI and reduction of subjective pain among RA patients who achieved LDA within 6 months and one year of treatment. The results showed that the pretreatment background and treatment options were both associated with the improvement. According to EULAR, the situation in which a patient has “well-controlled disease according to the above (universal) standards, but still having RA symptoms that are causing a reduction in quality of life” is categorized as one of the criteria of D2T RA [1]. As this is the flipside of the outcome of our study (improvement in symptoms after achieving LDA), our results may provide insights regarding the prediction of D2T RA to some extent.
A previous study targeting early RA patients showed that patients in the “low inflammation - high HAQ” group were on average older, were more often female, had more comorbidities and had more severe pain, fatigue, anxiety and depressive symptoms at baseline compared with patients in the “low inflammation - low HAQ” group [16]. Similarly, previous studies of RA patients have shown an association between comorbidities and poor functional outcomes [17] and difficulty in disease control [18]. These poor outcomes were partly attributed to the limited treatment options among patients with comorbidities [19]. However, our study showed that existing comorbidities such as overweight, CKD, and ILD, and a past history of cancer were not associated with HAQ-DI normalization. This is consistent with previous studies showing that comorbidities may not affect the refractoriness of treatment [20] or the improvement in physical function when controlling for other factors [21]. This discrepancy can be explained by the current development of b/tsDMARDs with better safety profiles, which made it possible for patients with comorbidities to receive more intensive treatment than in the past. Indeed, previous study suggested that significant increase in mortality rate among RA patients might be eliminated when they are treated with bDMARD [22]. Given these results, introduction of b/tsDMARDs in the early phase of RA would be recommended especially for patients with complications such as ILD and CKD.
On the other hand, higher age correlated with poor improvements in HAQ-DI and pain VAS scores (Fig. 2). As the proportion of LDA achievement was not different between age groups (Additional file 9), this result may reflect an increase in the baseline of pain VAS with age.
Considering each clinical factor, HAQ-DI improvement is strongly associated with the reduction of pain VAS rather than the number of tender joints or swollen joints (Table 3). Therefore, physicians may need to consider treatment intensification for patients with high pain levels, even after the number of affected joints has decreased. Interestingly, patients who experienced the failure of ≥ 2 classes of b/tsDMARD were less likely to achieve HAQ-DI normalization and pain VAS reduction. However, our previous study showed that the failure of ≥ 2 b/tsDMARDs does not predict poor CDAI improvement in response to b/tsDMARDs [23]. Therefore, the major cause of the D2T status of these patients might be due to residual pain rather than inflammatory status.
Our results also showed a negative correlation between HAQ-DI improvement / pain VAS reduction and the use of GC. Since a past history of fractures is also associated with these outcomes, this might be caused by steroid-induced osteoporosis and fractures. Although further prospective research is required, the early introduction of rapid-acting b/tsDMARDs rather than GC may be a preferable option for patients with a high risk of osteoporosis [24]. Another hypothesis is that inflammatory symptom such as swollen joints is masked among patients using GC who did not actually achieved LDA. This is supported by the result that the difference was no more observed when only those who achieved remission were included (Additional file 6, 13). In addition, promoted catabolism and suppression of hypothalamus-pituitary-adrenal axis caused by long-term GC treatment may increase risks of fatigue and malaise and thus affect physical activities. Further research including change in hormonal status may be needed to understand the mechanisms of residual pain among patients who achieve LDA.
In our study, JAKi were associated with HAQ-DI normalization and pain VAS reduction compared with TNFi at 6 months after starting treatment. The effectiveness of JAKi on patient-oriented outcomes among RA patients are well-established [25], including the effectiveness on pain among RA patients with low levels of inflammation [26]. This might be due to the direct effect of JAKi on signals on pain sensitivity [27], or the rapid-acting nature of these agents, within 24 h [24], one week [28], and two weeks [10], which may also contribute to the improvements in HAQ-DI in the early stages of treatment. This assumption is supported by the observation that the difference between drug classes was not significant one year after starting treatment (Additional file 4, 11). As the proportions of patients who achieved LDA were not significantly different (Additional file 1), this difference is less likely to be caused by the difference in response rates to the treatment at 6 months. Even so, this difference might be due to the differences in pre-treatment conditions that were not included in this study, and therefore, we should be careful in the interpretation of this result.
Interestingly, there was positive relationship between seropositivity of RF / anti-CCP antibodies and the improvement in clinical symptoms. Previous research associate seropositivity of ACPA and higher disease activity [29]. RF positivity with positive anti-CCP antibodies was also associated with higher systemic inflammation in early RA [30]. As the effect is observed when we included only those who achieved LDA or remission (Additional file 6 and 13), the difference was less likely to be persistent inflammation of the patients. Another possibility is difference in background between seropositive and seronegative patients (Additional file 7). Especially, disease duration is longer among seropositive patients. However, the difference remained significant even among those with shorter disease duration (< 5 years, Additional file 5, 12). Another possibility is that seropositive patients might have been diagnosed as b/tsDMARDs earlier compared with seronegative patients. In addition, promotion of osteoclastogenesis and nociception by autoantibodies [31] might be cancelled by earlier intensive treatment with b/tsDMARDs [22] that improves HAQ-DI and Pain VAS.
Limitations
Our study has several limitations, primarily due to its retrospective nature. First, this registry included several episodes of treatments of the same patients with different agents. Second, other comorbidities that may confound the outcomes, such as hepatic disorders and neurological disorders, were not included. Information about the severity of ILD was not collected, suggesting that our data about pre-existing comorbidities may not have been sufficient to determine a possible association. Third, some treatment options such as rituximab were not included in our study because it is not approved as a treatment for RA in Japan. In addition, psychological factors such as SF-36 scores were not included in this analysis, and the impact of these factors on functional outcomes is not clear. For example, a negative correlation between pain VAS reduction and longer disease duration may partly be caused by an increase in the proportion of patients with depressive status or fibromyalgia with time. Further research is required, including the use of drugs such as antidepressants and pregabalin for neuropathic pain. Nevertheless, our study is important in that it provides a clue to risk factors and beneficial factors affecting D2T RA.
Conclusions
Our study revealed several factors that are associated with a category of D2T RA, “well-controlled disease according to the above (universal) standards, but still having RA symptoms that are causing a reduction in quality of life”. Longer disease duration and a past history of fracture were associated with less improvement in HAQ-DI and pain VAS, suggesting the importance of T2T even among patients who achieve LDA in the early phases of treatment. As the failure of ≥ 2 classes of b/tsDMARD was associated with poor pain VAS reduction, further research might be required for the prevention of D2T RA. Our study also suggested that GC use is not preferable with regard to HAQ-DI and pain improvement. Therefore, the use of rapid-acting b/tsDMARDs instead of GC might be a preferable treatment option for patients with high disease activity, especially when the patients have osteoporosis.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- b/tsDMARD:
-
Biological and targeted synthetic disease modifying anti-rheumatic drug
- csDMARD:
-
Conventional synthetic disease modifying anti-rheumatic drug
- CCP:
-
Cyclic citrullinated peptide
- CDAI:
-
Clinical disease activity index
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CTLA4-Ig:
-
Cytotoxic T-lymphocyte-associated antigen 4 immunoglobulin
- D2T RA:
-
Difficult-to-treat rheumatoid arthritis
- DAS:
-
Disease activity score
- EGA:
-
Evaluator’s global assessment
- ESR:
-
Erythrocyte sedimentation rate
- GC:
-
Glucocorticoid
- GFR:
-
Glomerular filtration rate
- GH:
-
Patient’s global health
- HAQ-DI:
-
Health assessment questionnaire disability index
- HDA:
-
High disease activity
- IL6i:
-
Interleukin-6 receptor inhibitor
- ILD:
-
Interstitial lung disease
- JAKi:
-
Janus kinase inhibitor
- LDA:
-
Low disease activity
- MDA:
-
Middle disease activity
- MS:
-
Morning stiffness
- MTX:
-
Methotrexate
- OR:
-
Odds ratio
- RA:
-
Rheumatoid arthritis
- RF:
-
Rheumatoid factor
- SDAI:
-
Simplified disease activity index
- SJC:
-
Swollen joints count
- TJC:
-
Tender joints count
- TNFi:
-
Tumor necrosis factor inhibitor
- VAS:
-
Visualized analogue scale
References
Nagy G, Roodenrijs NMT, Welsing PM, Kedves M, Hamar A, van der Goes MC, et al. EULAR definition of difficult-to-treat rheumatoid arthritis. Ann Rheum Dis. 2021;80(1):31–5.
Steunebrink LMM, Oude Voshaar MAH, Taal E, Vonkeman HE, Zijlstra TR, van de Laar M. Determinants of Perceived Health Nonimprovement in early rheumatoid arthritis patients with favorable treatment outcomes. Arthritis Care Res. 2018;70(4):510–5.
Van der Elst K, Verschueren P, De Cock D, De Groef A, Stouten V, Pazmino S et al. One in five patients with rapidly and persistently controlled early rheumatoid arthritis report poor well-being after 1 year of treatment. RMD open. 2020;6(1).
Conaghan PG, Hensor EM, Keenan AM, Morgan AW, Emery P. Persistently moderate DAS-28 is not benign: loss of function occurs in early RA despite step-up DMARD therapy. Rheumatology (Oxford). 2010;49(10):1894–9.
Gwinnutt JM, Norton S, Hyrich KL, Lunt M, Combe B, Rincheval N, et al. Influence of Social Support, Financial Status, and Lifestyle on the Disparity between Inflammation and disability in rheumatoid arthritis. Arthritis Care Res. 2023;75(5):1026–35.
Tidblad L, Westerlind H, Delcoigne B, Askling J, Saevarsdottir S. Comorbidities and treatment patterns in early rheumatoid arthritis: a nationwide Swedish study. RMD open. 2022;8(2):e002700.
Ochi S, Saito K, Mizoguchi F, Kato S, Tanaka Y. Insensitivity versus poor response to tumour necrosis factor inhibitors in rheumatoid arthritis: a retrospective cohort study. Arthritis Res Ther. 2020;22(1):41.
Kawabe A, Nakano K, Kubo S, Asakawa T, Tanaka Y. Differential long-term retention of biological disease-modifying antirheumatic drugs in patients with rheumatoid arthritis by age group from the FIRST registry. Arthritis Res Ther. 2020;22(1):136.
Sonomoto K, Tanaka H, Nguyen TM, Yoshinari H, Nakano K, Nakayamada S, et al. Prophylaxis against pneumocystis pneumonia in rheumatoid arthritis patients treated with b/tsDMARDs: insights from 3787 cases in the FIRST registry. Rheumatology (Oxford). 2022;61(5):1831–40.
Ochi S, Sonomoto K, Nakayamada S, Tanaka Y. Preferable outcome of Janus kinase inhibitors for a group of difficult-to-treat rheumatoid arthritis patients: from the FIRST Registry. Arthritis Res Ther. 2022;24(1):61.
Takeuchi T, Fleischmann R, Iikuni N, Shi H, Soma K, Paulissen J, et al. Differences and similarities in clinical and functional responses among patients receiving tofacitinib monotherapy, tofacitinib plus methotrexate, and adalimumab plus methotrexate: a post hoc analysis of data from ORAL strategy. Arthritis Res Therapy. 2021;23(1):220.
Strand V, Scott DL, Emery P, Kalden JR, Smolen JS, Cannon GW, et al. Physical function and health related quality of life: analysis of 2-year data from randomized, controlled studies of leflunomide, sulfasalazine, or methotrexate in patients with active rheumatoid arthritis. J Rheumatol. 2005;32(4):590–601.
Zhang W, Bansback N, Guh D, Li X, Nosyk B, Marra CA, et al. Short-term influence of adalimumab on work productivity outcomes in patients with rheumatoid arthritis. J Rheumatol. 2008;35(9):1729–36.
Rigby W, Ferraccioli G, Greenwald M, Zazueta-Montiel B, Fleischmann R, Wassenberg S, et al. Effect of rituximab on physical function and quality of life in patients with rheumatoid arthritis previously untreated with methotrexate. Arthritis Care Res. 2011;63(5):711–20.
Grilo RM, Treves R, Preux PM, Vergne-Salle P, Bertin P. Clinically relevant VAS pain score change in patients with acute rheumatic conditions. Joint bone Spine. 2007;74(4):358–61.
Gwinnutt JM, Norton S, Hyrich KL, Lunt M, Combe B, Rincheval N, et al. Exploring the disparity between inflammation and disability in the 10-year outcomes of people with rheumatoid arthritis. Rheumatology (Oxford). 2022;61(12):4687–701.
Stouten V, Westhovens R, De Cock D, Van der Elst K, Pazmino S, Bertrand D, et al. Having a co-morbidity predicts worse outcome in early rheumatoid arthritis despite intensive treatment: a post hoc evaluation of the pragmatic randomized controlled CareRA trial. Rheumatology (Oxford). 2021;60(8):3699–708.
Batko B, Urbański K, Świerkot J, Wiland P, Raciborski F, Jędrzejewski M, et al. Comorbidity burden and clinical characteristics of patients with difficult-to-control rheumatoid arthritis. Clin Rheumatol. 2019;38(9):2473–81.
Roodenrijs NMT, van der Goes MC, Welsing PMJ, Tekstra J, Lafeber F, Jacobs JWG, et al. Difficult-to-treat rheumatoid arthritis: contributing factors and burden of disease. Rheumatology (Oxford). 2021;60(8):3778–88.
Norton S, Koduri G, Nikiphorou E, Dixey J, Williams P, Young A. A study of baseline prevalence and cumulative incidence of comorbidity and extra-articular manifestations in RA and their impact on outcome. Rheumatology (Oxford). 2013;52(1):99–110.
Busby AD, Wason J, Pratt AG, Young A, Isaacs JD, Nikiphorou E. Predictors of poor function in RA based on two prospective UK inception cohorts. Do Comorbidities Matter? Rheumatol (Oxford England). 2022;61(4):1563–9.
Alemao E, Bao Y, Weinblatt ME, Shadick N. Association of Seropositivity and Mortality in Rheumatoid Arthritis and the impact of treatment with Disease-modifying antirheumatic drugs: results from a real-world study. Arthritis Care Res. 2020;72(2):176–83.
Ochi S, Mizoguchi F, Nakano K, Tanaka Y. Difficult-to-treat rheumatoid arthritis with respect to responsiveness to biologic/targeted synthetic DMARDs: a retrospective cohort study from the FIRST registry. Clin Exp Rheumatol. 2022;40(1):86–96.
Wallenstein GV, Kanik KS, Wilkinson B, Cohen S, Cutolo M, Fleischmann RM, et al. Effects of the oral Janus kinase inhibitor tofacitinib on patient-reported outcomes in patients with active rheumatoid arthritis: results of two phase 2 randomised controlled trials. Clin Exp Rheumatol. 2016;34(3):430–42.
Tóth L, Juhász MF, Szabó L, Abada A, Kiss F, Hegyi P et al. Janus kinase inhibitors improve Disease Activity and patient-reported outcomes in rheumatoid arthritis: a systematic review and Meta-analysis of 24,135 patients. Int J Mol Sci. 2022;23(3).
De Stefano L, Bozzalla Cassione E, Bottazzi F, Marazzi E, Maggiore F, Morandi V, et al. Janus kinase inhibitors effectively improve pain across different disease activity states in rheumatoid arthritis. Intern Emerg Med. 2023;18(6):1733–40.
Busch-Dienstfertig M, González-Rodríguez S. IL-4, JAK-STAT signaling, and pain. Jak-stat. 2013;2(4):e27638.
Coombs JH, Bloom BJ, Breedveld FC, Fletcher MP, Gruben D, Kremer JM, et al. Improved pain, physical functioning and health status in patients with rheumatoid arthritis treated with CP-690,550, an orally active Janus kinase (JAK) inhibitor: results from a randomised, double-blind, placebo-controlled trial. Ann Rheum Dis. 2010;69(2):413–6.
Aletaha D, Alasti F, Smolen JS. Rheumatoid factor, not antibodies against citrullinated proteins, is associated with baseline disease activity in rheumatoid arthritis clinical trials. Arthritis Res Ther. 2015;17(1):229.
Pertsinidou E, Saevarsdottir S, Manivel VA, Klareskog L, Alfredsson L, Mathsson-Alm L, et al. In early rheumatoid arthritis, anticitrullinated peptide antibodies associate with low number of affected joints and rheumatoid factor associates with systemic inflammation. Ann Rheum Dis. 2024;83(3):277–87.
Bugatti S, Manzo A, Montecucco C, Caporali R. The clinical value of autoantibodies in Rheumatoid Arthritis. Front Med (Lausanne). 2018;5:339.
Acknowledgements
We thank Dr. Kazuyoshi Saito at Tobata General Hospital, Dr. Kentaro Hanami and Dr. Shunsuke Fukuyo at Wakamatsu Hospital of the University of Occupational and Environmental Health, Dr. Keisuke Nakatsuka at Fukuoka Yutaka Hospital, and all the staff members at Kitakyushu General Hospital and Shimonoseki Saiseikai Hospital for their engagement in the data collection of the FIRST Registry. The authors send special thanks to Ms. Hiroko Yoshida, Ms. Youko Saitou, and Ms. Ayumi Maruyama for the excellent data management in the FIRST Registry.
Funding
This work was supported by JSPS KAKENHI Grant Number 23K11156.
Author information
Authors and Affiliations
Contributions
S.O. conceptualized the research design under the advice of K.S., S.N., and Y.T. S.O. and K.S. analyzed the patient data of the FIRST registry. All authors contributed to the interpretation of the data. S.O. was a major contributor in writing the manuscript. K.S., S.N., and Y.T. scrutinized the draft and made a significant revision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was carried out in compliance with the Helsinki Declaration and was approved by the ethics review board of the University of Occupational and Environmental Health, Japan (approval number 04–23).
Consent for publication
Informed consent was obtained from all patients of the FIRST Registry.
Competing interests
YT has received speaking fees and/or honoraria from Eli Lilly, AstraZeneca, Abbvie, Gilead, Chugai, Behringer-Ingelheim, GlaxoSmithKline, Eisai, Taisho, Bristol-Myers, Pfizer, Taiho, received research grants from Mitsubishi-Tanabe, Eisai, Chugai, Taisho.SO has received speaking fees from Asahi-kasei, Astellas, Eisai, Janssen, Mitsubishi-Tanabe, and Taisho Pharmaceutical Holdings.S N has received consulting fees, speaking fees, lecture fees, and/or honoraria from AstraZeneca, GlaxoSmithKline, Pfizer, Bristol-Myers, Astellas, Asahi-kasei, AbbVie, Chugai, Sanofi, Eisai, Gilead Sciences, Mitsubishi-Tanabe, Janssen, Eli Lilly, and Ayumi.KS declares that there are no competing interests. SO has received speaking fees from Asahi-kasei, Astellas, Eisai, Janssen, Mitsubishi-Tanabe, and Taisho Pharmaceutical Holdings. S N has received consulting fees, speaking fees, lecture fees, and/or honoraria from AstraZeneca, GlaxoSmithKline, Pfizer, Bristol-Myers, Astellas, Asahi-kasei, AbbVie, Chugai, Sanofi, Eisai, Gilead Sciences, Mitsubishi-Tanabe, Janssen, Eli Lilly, and Ayumi. KS declares that there are no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ochi, S., Sonomoto, K., Nakayamada, S. et al. Predictors of functional improvement and pain reduction in rheumatoid arthritis patients who achieved low disease activity with disease-modifying antirheumatic drugs: a retrospective study of the FIRST Registry. Arthritis Res Ther 26, 140 (2024). https://doi.org/10.1186/s13075-024-03369-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-024-03369-8