Abstract
Background
Few studies have systematically examined whether knowledge translation (KT) strategies can be successfully implemented within the long-term care (LTC) setting. In this study, we examined the effectiveness of a multifaceted, interdisciplinary KT intervention for improving the prescribing of vitamin D, calcium and osteoporosis medications over 12-months.
Methods
We conducted a pilot, cluster randomized controlled trial in 40 LTC homes (21 control; 19 intervention) in Ontario, Canada. LTC homes were eligible if they had more than one prescribing physician and received services from a large pharmacy provider. Participants were interdisciplinary care teams (physicians, nurses, consultant pharmacists, and other staff) who met quarterly. Intervention homes participated in three educational meetings over 12 months, including a standardized presentation led by expert opinion leaders, action planning for quality improvement, and audit and feedback review. Control homes did not receive any additional intervention. Resident-level prescribing and clinical outcomes were collected from the pharmacy database; data collectors and analysts were blinded. In addition to feasibility measures, study outcomes were the proportion of residents taking vitamin D (≥800 IU/daily; primary), calcium ≥500 mg/day and osteoporosis medications (high-risk residents) over 12 months. Data were analyzed using the generalized estimating equations technique accounting for clustering within the LTC homes.
Results
At baseline, 5,478 residents, mean age 84.4 (standard deviation (SD) 10.9), 71% female, resided in 40 LTC homes, mean size = 137 beds (SD 76.7). In the intention-to-treat analysis (21 control; 19 intervention clusters), the intervention resulted in a significantly greater increase in prescribing from baseline to 12 months between intervention versus control arms for vitamin D (odds ratio (OR) 1.82, 95% confidence interval (CI): 1.12, 2.96) and calcium (OR 1.33, 95% CI: 1.01, 1.74), but not for osteoporosis medications (OR 1.17, 95% CI: 0.91, 1.51). In secondary analyses, excluding seven nonparticipating intervention homes, ORs were 3.06 (95% CI: 2.18, 4.29), 1.57 (95% CI: 1.12, 2.21), 1.20 (95% CI: 0.90, 1.60) for vitamin D, calcium and osteoporosis medications, respectively.
Conclusions
Our KT intervention significantly improved the prescribing of vitamin D and calcium and is a model that could potentially be applied to other areas requiring quality improvement.
Trial Registration
ClinicalTrials.gov: NCT01398527. Registered: 19 July 2011.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Effective knowledge translation (KT) interventions are essential to encourage the uptake of evidence-based practices. Ideally, the selection of interventions is guided by evidence of effectiveness and efficiency [1]; however, good evidence is not always available or may not be generalizable from one setting to another. Compared with community or acute care settings, there has been little KT enquiry in long-term care (LTC) homes [2].
LTC homes provide 24-hour nursing care and supervision to residents who often have multiple comorbidities, polypharmacy, and shortened life expectancies. Physicians are often located offsite and engage in collaborative decision making with the care team [3]. Given these characteristics, KT strategies need to be targeted at the interdisciplinary team and be tailored to this unique practice environment [4]. Furthermore, rigorous evaluation is required to ascertain whether KT strategies proven to be effective in other care settings are also effective in LTC.
The Vitamin D and Osteoporosis Study (ViDOS) was a pilot, cluster randomized controlled trial that examined both feasibility and prescribing changes as primary outcomes. Pilot trials are designed to assess a number of feasibility objectives prior to conducting a larger trial [5]. Particularly in situations where there is little previous data to inform the process, pilot trials are considered essential prerequisites that will enhance success of a future, wide-scale trial (ibid). Given the considerable resources required to implement such a trial, in addition to examining feasibility outcomes, we appropriately powered the study to assess the statistical significance of our primary prescribing outcome.
The knowledge being translated in the ViDOS intervention was evidence-based osteoporosis and fracture prevention strategies, particularly wide-scale, appropriate vitamin D prescribing. An estimated 60 to 80% of LTC residents have osteoporosis [6], and in Canada, it is estimated that the fracture rate for LTC residents is approximately 2 to 4 times that of similarly aged community-dwelling residents [7]. Meta-analyses demonstrate that vitamin D reduces falls [8], and calcium and vitamin D reduce fractures in LTC residents [9]. Despite strong evidence and acceptance by physicians [10], these strategies are under-utilized in LTC [11,12]. Barriers to implementing appropriate fracture prevention include knowledge gaps [13,14], lack of access to bone densitometry, difficulty in applying risk assessment tools within LTC [14], and a lack of organizational processes and policies that support bone health [15]. Our overall aim was to examine a knowledge translation model for delivering evidence-based practices within LTC homes that utilized a standard method of delivery and also addressed the unique learning needs of each home. Targeting interdisciplinary care teams (including medicine, nursing, rehabilitation, and nutrition), our multifaceted model utilized common professional interventions (for example, educational meetings, audit and feedback) and included elements of quality improvement. Reflecting the critical need to target whole system change when implementing evidence into practice [16], particularly in LTC [17], our intervention emphasized home-level process and policy changes.
The focus of the current article is on prescribing changes; feasibility and fidelity results of the ViDOS trial are published elsewhere [18]. Our primary prescribing objective was to determine if the intervention increased the proportion of all residents prescribed vitamin D ≥800 IU over 12 months. Secondary objectives were to examine the influence of the intervention on 1) calcium prescribing and 2) osteoporosis medication prescribing for high-risk residents.
Methods
Trial design and setting
The protocol for this trial (NCT01398527) has been published [19]. The Vitamin D and Osteoporosis Study (ViDOS) was a pilot, cluster randomized control trial (RCT) conducted in 40 LTC homes across the province of Ontario, Canada. In Ontario, there are approximately 630 licensed LTC homes that provide residents with onsite nursing care, 24-hour supervision, or personal support [20].
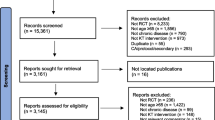
The trial had two arms: 19 LTC homes were assigned to the intervention group and 21 LTC homes were assigned to a control group (Figure 1). Cluster randomization was chosen due to the natural care clusters (the same professionals caring for residents) in LTC homes. In addition, we wished to minimize the potential for contamination between trial arms given that professionals in the same home may alter their practice for all residents. Furthermore, the ViDOS intervention targeted both individual prescribing physicians and home-level changes.
A data and safety monitoring board with expertise in geriatric medicine and clinical trials met twice to review trial processes. Informed consent was obtained from a representative at each LTC home and from individual professionals. The study was approved by the McMaster University/Hamilton Health Sciences Research Ethics Board (Reference #:09–215).
Recruitment of clusters
Our sampling frame was LTC homes who received medication and consulting services from Medical Pharmacies Group Limited, a large provider delivering services to approximately one-third of Ontario LTC homes. Homes were eligible if they had more than one prescribing physician and received services from Medical Pharmacies. There were no resident-level exclusion criteria. Our recruitment strategy included homes located in communities of all sizes and geographical regions across Ontario. Recruitment began in 2009 and was ongoing until the target sample size was reached. The final home completed the intervention in 2012.
Participants
The target audience within each LTC home was the core group of interdisciplinary care leaders (that is, the professional advisory committee). Depending on the size of the LTC home, this group included the medical director, director/assistant director of care, administrator, consultant pharmacist, food services director, other prescribing physicians, nurse practitioners, registered nurses, dieticians, and physiotherapists. Participation in the ViDOS intervention sessions is fully described elsewhere [18].
Randomization and blinding
LTC homes were allocated to control or intervention arms (1:1 allocation ratio) using stratified, block randomization. Stratified allocation was based on home size (<250 versus ≥250 beds) and profit/nonprofit status. An offsite investigator assigned homes to treatment groups based on a computer-generated allocation sequence. The database manager and analysts were blinded to allocation status; LTC homes, experts, and coordinators were not blinded.
Intervention
The design and implementation of our 12-month, multifaceted intervention (Figure 2) was founded on the Canadian Institutes of Health Research Knowledge-to-Action cycle [21], described in the study protocol [19].
Educational meetings
Informal “champions” (typically Directors of Care) worked with the research team to book educational meetings and encourage participation. Educational meetings had a combination of didactic presentation and interactive activities. Three, small-group, educational meetings, were held at each intervention home during approximately months 1, 6 and 12. Meetings were one-hour in length, typically had 5 to 10 participants, and were facilitated by one of six expert opinion leadersa [22], who were specialist physicians with expertise in osteoporosis or geriatrics. Experts engaged with study participants either in-person (meeting one only) or remotely; the study coordinator was on-site at the first two meetings to distribute/collect study materials and to facilitate the process (for example, connecting with the expert if remotely conducted). At each meeting, the expert delivered a standardized presentation reviewing best practices for osteoporosis management and fracture prevention (including case studies) with an emphasis on the importance of vitamin D for preventing falls and fractures. A question and answer session followed the presentation.
Action planning for quality improvement
After the presentation, interdisciplinary teams engaged in action planning based on the “plan-do-study-act” cycle [19,23]. Interdisciplinary care teams brainstormed regarding barriers and facilitators to implementing evidence-based strategies, particularly changes that could be made at an organizational level. An action plan worksheet was completed/updated at each educational meeting, which outlined specific tasks and steps for implementing process/policy changes. Ideas generated by teams were shared among LTC homes.
Audit and feedback reports
During the session, experts reviewed home-level audit and feedback reports with the interdisciplinary team. Reports included 1) vitamin D, calcium, and osteoporosis medication prescribing (based on previous month), which was benchmarked against other study homes; and 2) a summary of the falls and fractures occurring in the home in the previous 3 months. Confidential audit and feedback reports were also provided to each physician, containing a prescribing summary for their roster of patients.
Educational materials
Educational materials distributed included Ontario Osteoporosis Strategy [24] fracture prevention toolkits (ibid), process checklists, and paper-based treatment alerts to assist consultant pharmacists with flagging high-risk individuals [19].
Changes to intervention
The expert attended the initial educational meeting in-person at the first seven homes; it was not feasible to continue with this format, and the remainders were conducted remotely. We planned to use webinar technology to conduct the educational meetings; however, many homes did not have an accessible internet connection, and experts facilitated meetings via teleconference instead.
Control arm
Control homes received no intervention except fracture prevention toolkits provided to all LTC homes in the province by the Ontario Osteoporosis Strategy [24]; Osteoporosis Long-term care [www.osteoporosislongtermcare.ca].
Outcomes
Resident-level, de-identified prescribing/clinical data were obtained from the Medical Pharmacies central database. Data captured were point prevalence estimates; that is, medication/supplementation orders for all residents residing in the home on the day of the data download. Data were downloaded separately for each LTC home at approximately baseline, 6 and 12 months, just prior to the scheduled ViDOS educational sessionb. To ensure that the timing of data downloads was balanced between study arms throughout the study, data downloads for control homes were chronologically matched with an intervention home (the nearest one in the randomization sequence).
The primary outcome was the change in the proportion of all residents prescribed vitamin D ≥800 IU/day (including vitamin D2 or D3) over 12 months. Secondary prescribing outcomes were the change in 1) the proportion of all residents prescribed calcium ≥500 mg/day and 2) high-risk residents prescribed an osteoporosis medication (oral bisphosphonate, zoledronic acid, denosumab, or teriparatide). Algorithms to calculate supplement dosage included all daily/weekly/monthly preparations and medications and vitamin/mineral supplements that contain vitamin D and calcium. High-risk residents were those with a documented hip fracture, vertebral fracture, or osteoporosis diagnosis on the electronic Medication Administration Record (eMAR). The eMAR captured any medication indications or diagnoses that were present at admission, and further updates may have occurred when diagnoses were included on physician orders or quarterly medication reviews.
Falls and fractures
The study was not powered to make comparisons between study arms regarding incident falls and fractures. These data were collected to inform the feasibility of data collection for future trials in this setting. Falls and fracture data were collected for 3 months, in three nonconsecutive periods, coinciding with the educational meetings for the intervention homes. Home-specific feedback on the number of falls and fractures occurring was included in the audit and feedback reports (intervention homes only). Researchers provided the homes with a standardized data collection sheet and homes completed the information using various sources including electronic/paper-based charts, internal monitoring systems, Resident Assessment Instrument - Minimum Data Set 2.0 (RAI-MDS 2.0), and critical incident reports.
Sample size calculation
Given effect sizes observed in other KT interventions (for example, mixed interactive and didactic educational meetings [25]), we were interested in detecting a 15% difference in prescribing of vitamin D ≥800 IU/daily between the groups (anticipating a 20% increase in the intervention group, and a 5% increase in the control group due to ongoing provincial initiatives [24]). Based on prior work, we anticipated an average of 120 residents per LTC home and a baseline vitamin D (≥800 IU/day) prescribing rate of 30% [11]. Assuming an intracluster correlation of 0.10 and a Type I error of 5%, we determined that a sample size of 18 LTC homes (n = 2,160 residents) per arm was required to achieve 82% power. Factoring in a 10% dropout rate, the recruitment target was 40 LTC homes.
Statistical analysis
Differences in baseline characteristics between arms were examined using the chi-square procedure and independent samples T-test. Our primary analysis was intention-to-treat (ITT). To account for clustering within a LTC home, we analyzed resident-level data using the generalized estimating equations (GEE) technique, assuming an exchangeable correlation structure which specifies that all observations within the same cluster are equally correlated [26]. We examined the effect of the intervention on the change from baseline to 12 months in the proportion of residents prescribed vitamin D ≥800 IU/day and calcium ≥500 mg/day (that is, treatment group-by-time interaction). The same method was used to examine osteoporosis medication prescribing, including only high-risk residents. Odds ratios (ORs), corresponding 95% confidence intervals (CIs) are reported.
Sensitivity analyses
The above analyses were also conducted in the per protocol cohort, which excluded non-active intervention homes. We also examined the effect of adjusting GEE models for age, sex, and high-risk status.
Cluster-level analyses
For each outcome, we calculated the absolute prescribing change in each LTC home from baseline to 12-months. We report mean home-level prescribing changes within treatment arms and calculated the difference between arms, with 95% CIs adjusted for clustering using the method described by Donner and Klar [27].
All statistical analyses were performed using the SAS/STAT 9.2 software package (SAS Institute Inc., Cary, NC, USA) and SPSS v20. The criterion for statistical significance was set at ɑ = 0.05.
Results
The CONSORT flow diagram is displayed in Figure 1. The baseline cohort consisted of 5,478 residents residing in 40 LTC homes (19 intervention, 21 control). In total, 12 of the 19 intervention homes actively participated in the intervention. Of the seven nonactive intervention homes, six withdrew participation before beginning the study and one withdrew after the first educational meeting. The primary reasons for not participating were logistical or scheduling difficulties [18].
Facility characteristics
The majority of LTC homes in the study were for-profit and affiliated with a multifacility chain (Table 1). The mean facility size was larger in control (157 beds, standard deviation (SD) 80.2) versus intervention homes (115 beds, SD 67.9); however, both study arms had a similar proportion of small (<100 beds) and large (>250 beds) homes.
Resident characteristics
Residents in both arms were similar in baseline demographic characteristics. In the control arm, there was a higher prevalence of hip fractures; osteoporosis diagnoses; and baseline use of vitamin D ≥800 IU/day, calcium ≥500 mg/day, and osteoporosis medications (Table 2). Due to the correlated nature of clustered data and typically smaller number of units being randomized, achieving balance in baseline characteristics is less likely in cluster trials compared with individual RCT’s [28].
Prescribing changes
The median lengths of follow-up between baseline and final data download for all intervention, active intervention, and control homes, respectively, were 12.4 (min 7.4, max 15.0)c, 12.2 (min 11.4, max 15.0), and 12.1 (min 10.5, max 13.4) months.
The main findings are presented in Table 3. In the ITT cohort, GEE analyses indicated there was significantly greater prescribing change from baseline to 12 months in the intervention versus control groups for both vitamin D and calcium, with ORs 1.82 (95% CI: 1.12, 2.96) and 1.33 (95% CI: 1.01, 1,74), respectively.
The intervention had no significant effect on the change in osteoporosis medication prescribing in high-risk residents (OR 1.17, 95% CI: 0.91, 1.51).
The intracluster correlation coefficients for vitamin D, calcium, and osteoporosis medication prescribing were 0.194, 0.112, and 0.052, respectively.
Sensitivity analyses
In the per protocol cohort (including only actively participating homes), ORs were 3.06 (95% CI: 2.18, 4.29), 1.57 (95% CI: 1.12, 2.21), and 1.20 (95% CI: 0.90, 1.60) for vitamin D, calcium and osteoporosis medications, respectively.
Adjustment for confounding (age, sex, and high-risk status) had little impact on effect estimates (Table 3).
Absolute prescribing change
Over the course of the trial, the mean home-level prescribing change for vitamin D ≥800 IU/day was 22.2% (95% CI: 17.6, 26.7) in the intervention arm versus 7.5% (95% CI: 5.7, 9.3) in the control arm (between group difference = 14.7%, 95% CI: 13.1, 16.2). Mean home-level prescribing change for calcium ≥500 mg/day was 8.8% (95% CI: 6.6, 11.0) in the intervention arm versus 1.8% (95% CI: 0.30, 3.24) in the control arm (between group difference = 7.0%, 95% CI: 6.2, 7.9). In the per protocol cohort, the difference in mean home-level prescribing change between treatment arms was 27.0% (95% CI: 25.5, 28.5) for vitamin D and 13.1% (95% CI: 12.0, 14.2) for calcium.
There was no significant difference in the home-level prescribing change between arms for osteoporosis medications (between group difference, ITT = 3.4%, 95% CI: 2.6, 4.2; per protocol = 2.9%, 95% CI: 1.7, 4.1).
Falls and fractures
Complete falls and fracture data were received from 18 control (baseline residents, n = 2,727) and 11 intervention (baseline residents, n = 1290) homes. During 9 months of data collection (three nonconsecutive periods), 18 control homes (baseline residents, n = 2,727) reported 1,712 fallers (43.6% single fall, 19.3% two falls, and 37.1% =3 falls) and 11 intervention homes (baseline residents, n = 1290) reported 853 fallers (44.4% single fall, 19.0% with two falls, and 36.6% with three falls). In the control and intervention groups, respectively, 79/5,128 (1.5%) and 41/2,491 (1.6%) of all reported falls resulted in a fracture, including 40/79 (50.6%) and 17/41 (41.5%) hip fractures.
Discussion
Our results suggest that the ViDOS interdisciplinary, multifaceted intervention resulted in significantly greater uptake of appropriate vitamin D and calcium prescribing, with an absolute improvement in prescribing over 12 months of approximately 15% for vitamin D and 7% for calcium in the ITT cohort. Although not the focus of this report, we were also interested in the feasibility of conducting this type of KT intervention in the LTC setting. Despite challenges associated with recruitment and retention, there was good participation by interdisciplinary team members, including physicians, pharmacists and Directors of Care, and the intervention was well received [18].
Given that it is a tolerable, low-cost intervention that is recommended for all older adults [29], vitamin D may be particularly amenable to targeted change. In the community, a multifaceted intervention targeting improved osteoporosis management demonstrated a 13% absolute improvement in vitamin D [30]. In LTC, one KT intervention involving consultation and training by specialist osteoporosis nurses demonstrated a relative increase of 64% in calcium and vitamin D prescribing [31], but another study with a similar multifaceted intervention to ours did not demonstrate significant effects [32]. In the latter study, participation in the intervention was low, only high-risk residents were included in the analysis, and the authors also suggest a possible ceiling effect due to high baseline prescribing rates.
We did not see a significant effect for osteoporosis medication prescribing, which we hypothesize is attributable to several factors. Management with osteoporosis medications was reviewed in the didactic component of the educational meetings (the standardized presentation by the expert opinion leader), and this format has been demonstrated as less effective [33]. In the interactive component, action planning for change, several process and policy changes were discussed that may have been more amenable to vitamin D and calcium (for example, standard orders, dietary review and changes). It has been well documented that family physicians face a number of barriers for prescribing osteoporosis medications in LTC [10,14], including difficulty in applying general osteoporosis guidelines to LTC residents, particularly with regard to risk assessment. Currently, general osteoporosis clinical practice guidelines [29], are being adapted for the frail elderly residing in LTC. Furthermore, providing information and recommendations at the point of care that incorporate fracture risk may be necessary components for enhancing uptake in osteoporosis medications and is an area for future research.
One of the strengths of our multifaceted KT intervention was the inclusion of content and strategies that encouraged organizational change specific to the LTC setting, in addition to targeting professional behavior change. This is an important consideration, given that several structural and environmental barriers for implementing evidence-based practices within LTC homes have been identified including a high proportion of unregulated staff, absence of a learning culture, high turnover in management, heavy regulatory and documentation demands, routinized care rituals, and lack of familiarity with clinical practice guidelines [34-36]. Although not all barriers are easily modifiable, the ongoing monitoring of organizational-level barriers (formally, three times over 12 months) was an important design feature.
Another important design component was tailoring our intervention to interdisciplinary care teams. Compared with other practice settings, physicians who practice in LTC are typically more removed from daily patient care and more reliant on collaborative decision making. We engaged the entire interdisciplinary care team, including physicians, by scheduling educational meetings in conjunction with quarterly professional advisory meetings, enabling several off-site professionals to be present simultaneously.
Although not the focus of this paper, we had good fidelity with our intervention including active participation in educational meetings. Other similar KT studies in LTC, which included both physicians and LTC staff may have had nonsignificant [15,37] or less than optimal results [38], due to poor adherence with educational components. In addition to scheduling educational meetings with regularly scheduled meetings, feedback from ViDOS participants indicated that the direct involvement of an expert was highly valued [39].
This pilot study provides evidence that KT interventions can be successfully applied within the LTC setting, particularly when structured to fit the unique practice environment and organizational structure. Previously, these KT strategies have mainly been evaluated in non-LTC practice settings, and studies demonstrate small to moderate effectiveness [40]. Cochrane systematic reviews indicate median absolute improvements in care in the range of 4 to 12% for educational meetings (including interactive and didactic [25]), educational outreach [41], local opinion leaders [42], audit and feedback [43], and computerized reminders [44]. Some organizational interventions (for example, multidisciplinary collaboration and knowledge management change) also appear to improve some care outcomes [45], and interprofessional education has shown some positive results, but is an area requiring further study [46]. We observed similar or larger effect sizes compared with the medians reported in the systematic reviews noted above.
The ViDOS study had several methodological strengths, including the recruitment of homes that were geographically diverse and located in communities of varied population sizes. Both the study design and analysis took into the account clustered nature of the data, which minimizes the possibility of overestimating the treatment effect and spuriously significant findings [47].
Nonetheless, our study is not without limitations. While our study was generalizable in terms of geography and community size, we had an over-representation of chain affiliated and for-profit LTC homes compared with provincial averages [48]. Not-for-profit LTC homes have been associated with higher quality of care [49], although multifacility chains may have greater resources to facilitate implementation of clinical practice guidelines [34]. We experienced some challenges with recruitment and retention, which has also been noted in other KT trials in LTC [31,50]. This was a pragmatic RCT; some contamination between study arms likely occurred, which could have diluted our treatment effect. Six consultant pharmacists and four Medical Directors practiced in both control and intervention homes, and control homes may have been impacted by study activities via diffusion of messages (for example, homes in the same corporate chain). Future trials should consider adding region as a stratification factor to minimize contamination. Both arms were subject to outside influences including an ongoing province-wide initiative, the Ontario Osteoporosis Strategy for LTC, [www.osteoporosislongtermcare.ca) [24]].
We collected incident falls and fracture data for feasibility data, and the ability to obtain standardized data from LTC homes was a noted methodological limitation due to different fall reporting systems. Our fracture rate was slightly lower than the rate observed in a Canadian study using a standardized fall risk surveillance tool [51]. However, the purpose of this pilot study was to examine the feasibility and effectiveness of a KT model, and not to demonstrate the effectiveness of vitamin D for reducing falls and fractures. The choice of Vitamin D as our primary outcome was based on previous studies that demonstrated falls and fracture reduction [8,9] and our scoping review [52], which indicated that in LTC vitamin D supplementation was the intervention with the strongest evidence for reduction of hip fractures.
Given that our intervention was multifaceted, it is difficult to determine the most influential components. In general, multifaceted interventions may be more effective than single interventions [53], although Grimshaw et al. [40], have shown that adding more strategies may not improve effect sizes. We did not include measures of organizational context (for example, work culture, and type of leadership), which have been identified as an important factor influencing the uptake of research evidence [54]. Future trials should consider the interplay with contextual factors.
Conclusions
Although RCT’s evaluating KT interventions are increasing in the LTC setting [31,32,37,55], further implementation research evaluating professional and organizational KT strategies is still greatly needed. In this study, we demonstrated that an interdisciplinary, multifaceted intervention could be feasibly implemented in LTC [18] and that it improved uptake of vitamin D and calcium prescribing. Although our topic focused specifically on osteoporosis and fracture prevention, the ViDOS model could potentially be applied to a wider range of topics relevant to LTC residents.
Endnotes
aIn the framework by Locock et al. [18], an expert opinion leader was considered distinct from peer opinion leaders who are role models in daily practice and was a ‘credible authority (often an academic or consultant) able to explain the evidence and respond convincingly to challenges and debate’.
bOur rationale for linking data downloads with ViDOS session dates was to generate up-to-date audit and feedback reports. Six-month data were used to generate interim audit and feedback reports only, not for outcome evaluation.
cIn homes that were nonactive participants, there were additional challenges in obtaining the data. For two nonactive intervention homes, the elapsed time between baseline and a follow-up data download was less than 8 months. In the remaining homes, the time between baseline and follow-up ranged from 11 to 15 months. The variability in prescribing download dates was due to the timing of the data downloads with educational sessions.
Abbreviations
- ViDOS:
-
vitamin D and osteoporosis study
- LTC:
-
long-term care
- KT:
-
knowledge translation
- RCT:
-
randomized controlled trial
- OR:
-
odds ratio
- SD:
-
standard deviation
- eMAR:
-
electronic Medication Administration Record
- CI:
-
confidence interval
- GEE:
-
generalized estimating equations
- ITT:
-
intention-to-treat
References
Wensing M, Bosch M, Grol R. Developing and selecting interventions for translating knowledge to action. CMAJ. 2010;182:E85–8. doi:10.1503/cmaj.081233.
Bostrom AM, Slaughter SE, Chojecki D, Estabrooks CA. What do we know about knowledge translation in the care of older adults? A scoping review. J Am Med Dir Assoc. 2012;13:210–9. doi:10.1016/j.jamda.2010.12.004.
Kaasalainen S, Brazil K, Akhtar-Danesh N, Coker E, Ploeg J, Donald F, et al. The evaluation of an interdisciplinary pain protocol in long term care. J Am Med Dir Assoc. 2012;13:664–e1-8.
Berlowitz DR, Young GJ, Hickey EC, Joseph J, Anderson JJ, Ash AS, et al. Clinical practice guidelines in the nursing home. Am J Med Qual. 2001;16:189–95.
Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10:1. doi:10.1186/1471-2288-10-1.
Morley J. Osteoporosis and fragility fractures. J Am Med Dir Assoc. 2011;12:389–92.
Crilly RG, Tanner DA, Kloseck M, Chesworth BM. Hip fractures in long-term care: is the excess explained by the age and gender distribution of the residents? J Aging Res. 2010. doi: 10.4061/2010/291258.
Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2012;12:CD005465.
Avenell A, Gillespie WJ, Gillespie LD, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosis. Cochrane Database Syst Rev. 2009;2:CD000227.
Sawka AM, Ismaila N, Raina P, Thabane L, Straus S, Adachi JD, et al. Hip fracture prevention strategies in long-term care: a survey of Canadian physicians’ opinions. Can Fam Physician. 2010;56:e392–7.
Giangregorio LM, Jantzi M, Papaioannou A, Morin S, Cheung AM. Osteoporosis management among residents living in long-term care. Osteoporos Int. 2009;20:1471–8.
Ioannidis G, Kennedy CC, Dykeman J, Dudziak S, Papaioannou A. Association between vitamin D3 supplementation and serum 25-hydroxyvitamin D levels in older individuals residing in long-term care in Ontario, Canada. J Am Geriatr Soc. 2012;60:985–7.
Lau AN, Ioannidis G, Potts Y, Giangregorio LM, Van der Horst ML, Adachi JD, et al. What are the beliefs, attitudes and practices of front-line staff in long-term care (LTC) facilities related to osteoporosis awareness, management and fracture prevention? BMC Geriatr. 2010;10:73.
Wall M, Lohfeld L, Giangregorio L, Ioannidis G, Kennedy CC, Moser A, et al. Fracture risk assessment in long-term care: a survey of long-term care physicians. BMC Geriatr. 2013;13:109.
Colon-Emeric CS, Casebeer L, Saag K, Allison J, Levine D, Suh TT, et al. Barriers to providing osteoporosis care in skilled nursing facilities: perceptions of medical directors and directors of nursing. J Am Med Dir Assoc. 2004;5:361–6.
Grimshaw J, Eccles M, Tetroe J. Implementing clinical guidelines: current evidence and future implications. J Contin Educ Health Prof. 2004;24 Suppl 1:S31–7.
Kitson AL, Rycroft-Malone J, Harvey G, McCormack B, Seers K, Titchen A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implemen Sci. 2008;3:1.
Kennedy CC, Thabane L, Ioannidis G, Adachi JD, Papaioannou A. Implementing a knowledge translation intervention in long-term care: feasibility results from the Vitamin D and Osteoporosis Study (ViDOS). J Am Med Dir Assoc. 2014;15:943–5.
Kennedy CC, Ioannidis G, Giangregorio LM, Adachi JD, Thabane L, Morin SN, et al. An interdisciplinary knowledge translation intervention in long-term care: study protocol for the vitamin D and osteoporosis study (ViDOS) pilot cluster randomized controlled trial. Implemen Sci. 2012;7:48.
Ontario Ministry Health & Long-term Care. Reports on long-term care homes. 2010. http://www.health.gov.on.ca/en/public/programs/ltc/26_reporting.aspx. Accessed 30 December 30 2013.
Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26(1):13–24. doi:10.1002/chp.47.
Locock L, Dopson S, Chambers D, Gabbay J. Understanding the role of opinion leaders in improving clinical effectiveness. Soc Sci Med. 2001;53(6):745–57.
Agency for Healthcare Research and Quality. QualityTool: Plan-do-study-act (PDSA) cycle 2008. http://www.innovations.ahrq.gov/content.aspx?id=2398&tab=3. Accessed 30 Dec 2013.
Jaglal SB, Hawker G, Cameron C, Canavan J, Beaton D, Bogoch E, et al. The Ontario Osteoporosis Strategy: implementation of a population-based osteoporosis action plan in Canada. Osteoporos Int. 2010;21:903–8.
Forsetlund L, Bjorndal A, Rashidian A, Jamtvedt G, O’Brien MA, Wolf F, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2009;2:CD003030.
Hardin JW, Hilbe JM. Generalized estimating equations. 1st ed. New York: Chapman & Hall/CRC; 2003.
Donner A, Klar N. Confidence interval construction for effect measures arising from cluster randomization trials. J Clin Epidemiol. 1993;46:123–31.
Ivers NM, Halperin IJ, Barnsley J, Grimshaw JM, Shah BR, Tu K, et al. Allocation techniques for balance at baseline in cluster randomized trials: a methodological review. Trials. 2012;13:120.
Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, et al. 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182:1864–73.
Ciaschini PM, Straus SE, Dolovich LR, Goeree RA, Leung KM, Woods CR, et al. Community based intervention to optimize osteoporosis management: randomized controlled trial. BMC Geriatr. 2010;10:60.
Cox H, Puffer S, Morton V, Cooper C, Hodson J, Masud T, et al. Educating nursing home staff on fracture prevention: a cluster randomised trial. Age Ageing. 2008;37:167–72.
Colon-Emeric CS, Lyles KW, House P, Levine DA, Schenck AP, Allison J, et al. Randomized trial to improve fracture prevention in nursing home residents. Am J Med. 2007;120:886–92.
Davis D, O’Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282:867–74.
Berta W, Teare GF, Gilbart E, Ginsburg LS, Lemieux-Charles L, Davis D, et al. Spanning the know-do gap: understanding knowledge application and capacity in long-term care homes. Soc Sci Med. 2010;70:1326–34.
Resnick B, Quinn C, Baxter S. Testing the feasibility of implementation of clinical practice guidelines in long-term care facilities. J Am Med Dir Assoc. 2004;5:1–8.
Levine DA, Saag KG, Casebeer LL, Colon-Emeric C, Lyles KW, Shewchuk RM. Using a modified nominal group technique to elicit director of nursing input for an osteoporosis intervention. J Am Med Dir Assoc. 2006;7:420–5.
Beer C, Horner B, Flicker L, Scherer S, Lautenschlager NT, Bretland N, et al. A cluster-randomised trial of staff education to improve the quality of life of people with dementia living in residential care: the DIRECT study. PLoS One. 2011;6:e28155.
Tjia J, Mazor KM, Field T, Doherty P, Spenard A, Gurwitz JH. Predicting nursing home adherence to a clinical trial intervention: lessons for the conduct of cluster randomized trials. J Am Geriatr Soc. 2011;59:2332–6.
Kennedy CC, Lohfeld L, Adachi JD, Morin SM, Marr S, Crilly RG et al. Is a multifaceted knowledge translation intervention feasible and acceptable in long-term care? A qualitative study with ViDOS participants. Can Ger J. 2013;16
Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implemen Sci. 2012;7:50.
O’Brien MA, Rogers S, Jamtvedt G, Oxman AD, Odgaard-Jensen J, Kristoffersen DT, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007;4:CD000409.
Flodgren G, Parmelli E, Doumit G, Gattellari M, O’Brien MA, Grimshaw J, et al. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2011;8:CD000125.
Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259.
Shojania KG, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev. 2009;3:CD001096.
Wensing M, Wollersheim H, Grol R. Organizational interventions to implement improvements in patient care: a structured review of reviews. Implemen Sci. 2006;1:2.
Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes (update). Cochrane Database Syst Rev. 2013;3:CD002213.
Campbell MK, Grimshaw JM. BMJ. 1998;317:1171–2.
Berta W, Laporte A, Valdmanis V. Observations on institutional long-term care in Ontario: 1996–2002. Can J Aging. 2005;24:70–84.
Comondore VR, Devereaux PJ, Zhou Q, Stone SB, Busse JW, Ravindran NC, et al. Quality of care in for-profit and not-for-profit nursing homes: systematic review and meta-analysis. BMJ. 2009;339:b2732.
Ersek M, Polissar N, Pen AD, Jablonski A, Herr K, Neradilek MB. Addressing methodological challenges in implementing the nursing home pain management algorithm randomized controlled trial. Clin Trials. 2012;9:634–44.
Gallagher EM, Scott VJ. Final report: Canada health agency, population health fund stepping in: Long-term care collaborative falls prevention project. 2005. http://www.coag.uvic.ca/resources/publications/reports/Stepping_In-_Falls_Long_Term_Care.pdf. Accessed 19 Jan 2014.
Sawka AM, Ismaila N, Cranney A, Thabane L, Kastner M, Gafni A, et al. A scoping review of strategies for the prevention of hip fracture in elderly nursing home residents. PLoS One. 2010;53:e9515.
Wensing M, van der Weijden T, Grol R. Implementing guidelines and innovations in general practice: which interventions are effective? Br J Gen Pract. 1998;48:991–7.
Cummings GG, Estabrooks CA, Midodzi WK, Wallin L, Hayduk L. Influence of organizational characteristics and context on research utilization. Nurs Res. 2007;56(4 Suppl):S24–39.
Anderson RA, Corazzini K, Porter K, Daily K, McDaniel Jr RR, Colon-Emeric C. CONNECT for quality: protocol of a cluster randomized controlled trial to improve fall prevention in nursing homes. Implemen Sci. 2012;7:11.
Acknowledgements
We thank all of the LTC professionals who dedicated their time to participate in this study. In addition, we thank Jenna Johnson, Susanne King, Jacob Eappen, and Carly Skidmore for their invaluable assistance with coordinating the ViDOS study; Teresa Pitre for her assistance with recruitment; and the Data and Safety Monitoring Board: Dr. Stephanie Kaiser (Chair), Dr, Barbara Liu, and Dr. Barbara Power for their expertise.
This work was supported by an operating grant from the Canadian Institutes of Health Research (Funding Reference Number: MOP-114982). In addition, the ViDOS researchers wish to thank other key partners who supported this initiative: Ministry of Health and Long-Term Care - Ontario Osteoporosis Strategy, Ontario College of Family Physicians, Osteoporosis Canada, Medical Pharmacies Group Limited, Hamilton Health Sciences/GERAS Centre -St. Peter’s Hospital, McMaster University, and the Seniors Health Research Transfer Network (SHRTN).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Dr. Courtney Kennedy declares that she has no competing interests.
Dr. George Ioannidis declares that he has no competing interests.
Dr. Lehana Thabane declares that she has no competing interests.
Dr. Jonathan Adachi consults for and has received lecture fees from Amgen, Eli Lilly, Merck, Novartis, Warner Chilcott.
Dr. Sharon Marr has received funds from CHHO-Artic and Hamilton Health Sciences and is a board member for the Royal College Physicians and Surgeons Internal Medicine Exam Board.
Dr. Lora Giangregorio has received a research grant for Merck Canada Inc., Amgen; for a community speaking engagement on exercise.
Dr. Suzanne Morin is a board member for Eli Lilly, Merck, Amgen and Novartis and is part of the speaker forum for Eli Lilly and Amgen.
Dr. Richard Crilly declares that he has no competing interests.
Dr. Robert Josse received research grants and/or speaker honoraria and/or is part of the medical advisory board for Lilly, Amgen, Merck, Novartis, Warner Chilcott.
Laura Pickard declares that she has no competing interests.
Mary-Lou van der Horst declares that she has no competing interests.
Glenda Campbell declares that she has no competing interests.
Jackie Stroud declares that she has no competing interests.
Dr. Lisa Dolovich declares that she has no competing interests.
Dr. Anna Sawka received research grants from Canadian Institutes of Health Research, Cancer Care Ontario, University Health Network, University of Toronto, Canadian Society of Endocrinology and Metabolism and currently holds a Chair in Health Services Research from Cancer Care Ontario, funded by the Ontario Ministry of Health and Long-term Care.
Ravi Jain declares that he has no competing interests.
Dr. Lynn Nash declares that she has no competing interests.
Dr. Alexandra Papaioannou has received grants and research support from Amgen, Eli Lilly, Merck Canada Inc., Novartis, Warner Chilcott and consults for Amgen, Eli Lilly, Merck Canada Inc., Novartis, Warner Chilcott.
Authors’ contributions
AP conceived the study, provided leadership on all aspects of trial implementation, acquired funding, and was the lead facilitator of intervention sessions. CCK was responsible for study design, overseeing study implementation, providing methodological support to coordinators, designing/overseeing study databases, statistical analyses, and drafting the manuscript. GI advised on study design, participated in overseeing study implementation, and performed advanced statistical analyses. LT was the senior advisor on study design, implementation, and statistical analysis. LG advised on study design and participated in overseeing study implementation. JDA, SM, SNM, RGC, RGJ advised on osteoporosis content and were facilitators of the intervention sessions. LL was the qualitative methodology advisor. LEP provided leadership in study implementation and coordination. MLV participated in designing the intervention materials and implementing intervention sessions. GC and JS were responsible for the acquisition of all pharmacy data. LD and AMS were study methodology advisors. LN was the family medicine advisor. RJ acted as the Osteoporosis Canada liaison, providing additional leadership and support for this initiative. All authors participated in critical revision of the manuscript for important intellectual content and read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kennedy, C.C., Ioannidis, G., Thabane, L. et al. Successful knowledge translation intervention in long-term care: final results from the vitamin D and osteoporosis study (ViDOS) pilot cluster randomized controlled trial. Trials 16, 214 (2015). https://doi.org/10.1186/s13063-015-0720-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-015-0720-3