Abstract
Background
Molecular breast imaging (MBI) is a functional test used for supplemental screening of women with mammographically dense breasts. Additionally, MBI depicts variable levels of background parenchymal uptake (BPU) within nonmalignant, dense fibroglandular tissue. We investigated whether BPU is a risk factor for breast cancer.
Methods
We conducted a retrospective case-control study of 3027 eligible women who had undergone MBI between February 2004 and February 2014. Sixty-two incident breast cancer cases were identified. A total of 179 controls were matched on age, menopausal status, and MBI year. Two radiologists blinded to case status independently assessed BPU as one of four categories: photopenic, minimal to mild, moderate, or marked. Conditional logistic regression analysis was performed to estimate the associations (OR) of BPU categories (moderate or marked vs. minimal to mild or photopenic) and breast cancer risk, adjusted for other risk factors.
Results
The median age was 60.2 years (range 38–86 years) for cases vs. 60.2 years (range 38–88 years) for controls (p = 0.88). Women with moderate or marked BPU had a 3.4-fold (95 % CI 1.6–7.3) and 4.8-fold (95 % CI 2.1–10.8) increased risk of breast cancer, respectively, compared with women with photopenic or minimal to mild BPU, for two radiologists. The results were similar after adjustment for BI-RADS density (OR 3.3 [95 % CI 1.6–7.2] and OR 4.6 [95 % CI 2.1–10.5]) or postmenopausal hormone use (OR 3.6 [95 % CI 1.7–7.7] and OR 5.0 [95 % CI 2.2–11.4]). The association of BPU with breast cancer remained in analyses limited to postmenopausal women only (OR 3.8 [95 % CI 1.5–9.3] and OR 4.1 [95 % CI 1.6–10.2]) and invasive breast cancer cases only (OR 3.6 [95 % CI 1.5–8.8] and OR 4.4 [95 % CI 1.7–11.1]). Variable BPU was observed among women with similar mammographic density; the distribution of BPU categories differed across density categories (p < 0.0001).
Conclusions
This study provides the first evidence for BPU as a risk factor for breast cancer. Among women with dense breasts, who comprise >40 % of the screening population, BPU may serve as a functional imaging biomarker to identify the subset at greatest risk.
Similar content being viewed by others
Background
Mammographic density is known to be an important factor in reducing the sensitivity of mammography [1, 2]. Therefore, supplemental screening options capable of detecting mammographically occult cancers are now increasingly being offered to women with dense breasts [3–5]. Density is also strongly associated with breast cancer risk, even after accounting for its masking of cancers [1, 6]. However, density alone lacks sufficient discriminatory accuracy to be clinically useful in individual risk assessment [6, 7]. Risk models developed within the Breast Cancer Surveillance Consortium (BCSC) have incorporated American College of Radiology (ACR) Breast Imaging-Reporting and Data System (BI-RADS) breast density categories [8], a genetic risk score, and history of benign breast disease; yet, c-statistics, or AUC, remain <0.67 [9, 10]. Given the high prevalence of dense breasts (43 % of screening-eligible U.S. women have heterogeneously or extremely dense breasts according to BI-RADS criteria [11]), coupled with increasing adoption of breast density notification laws (in 26 states to date [12]), further tools are needed to identify women most likely to benefit from supplemental screening or primary prevention.
Molecular breast imaging (MBI) is a functional imaging technique that uses a specialized gamma camera to detect preferential uptake of Tc-99m sestamibi in metabolically active breast tissue. When used as a supplement to screening mammography in women with dense breasts, MBI showed an incremental cancer detection rate of 8.8 per 1000 women screened [5]. MBI can also show variable levels of radiotracer uptake within areas of nonmalignant fibroglandular tissue, a finding termed background parenchymal uptake (BPU) [13]. BPU is associated with hormonal influences, including menopausal status, postmenopausal hormone use, and phase of menstrual cycle [14, 15]. Also, BPU varies among women with similar mammographic density [14].
We hypothesized that the functional differences reflected in MBI background provide additional information for determining breast cancer risk in women with dense breasts. Here, our objective was to investigate whether BPU on MBI is a risk factor for breast cancer.
Methods
Study population
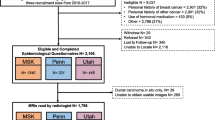
We performed a retrospective case-control study that was compliant with the U.S. Health Insurance Portability and Accountability Act and approved by the Mayo Clinic Institutional Review Board, which issued a waiver of informed consent. Our institutional MBI database was reviewed to identify all patients (n = 3202) who had had at least one MBI examination performed at the Mayo Clinic in Rochester, MN, USA, between 1 February 2005 and 28 February 2014. The Mayo Clinic patients provides a general authorization for use of medical record information for research purposes. We included only women who provided this authorization (n = 3085 [96 %] of 3202). For women who had had multiple MBI examinations performed, data from the earliest (index) MBI were used for analysis. Follow-up for breast cancer through December 2014 was conducted through review of medical records and linkage to the Mayo Clinic Tumor Registry.
Women with breast implants at the time of index MBI were excluded, as photopenia due to the presence of implants makes assessment of BPU difficult. Women with a history of breast cancer before the index MBI examination or a diagnosis within 180 days following the index MBI were also excluded to minimize prevalent cases, as done in prior studies [16]. After these exclusions, 3027 eligible participants remained from among whom to identify cases and controls. Average follow-up time of participants was 4.6 years.
Incident cases were defined as participants with a histopathologic diagnosis of ductal carcinoma in situ (DCIS) or invasive carcinoma in either breast at least 180 days after the index MBI. Sixty-two incident breast cancer cases were identified. The median time between index MBI examination and cancer diagnosis was 3.1 years (IQR 1.5–4.2 years). Fifty-eight (94 %) of sixty-two cases were diagnosed more than 1 year after the index MBI.
Up to three control subjects per case (n = 179) were selected from among the 2965 women who were not diagnosed with breast cancer over the study period, with matching to cases on age (within 5 years), menopausal status (exact), and year of MBI (within 1 year). Matched controls were required to be followed for at least as long as matched cases and to have had negative findings on all subsequent breast imaging performed at our institution over the corresponding follow-up time. Median follow-up time for controls was 6.1 years (IQR 3.7–7.8 years).
Of the 241 women studied, MBI was performed as a supplemental screen to mammography in 228 (95 %, comprising 57 cases and 171 controls). In the remaining 13 women (5 %), MBI was performed for further evaluation of the following: breast mass initially detected on mammography or ultrasound (three cases, five controls), recent histopathologic diagnosis of atypia or lobular carcinoma in situ (one case, two controls), bloody nipple discharge (one case), and breast pain (one control).
Covariate information, including body mass index (BMI), menopausal status, postmenopausal hormone use, breast biopsy history, and family history of breast cancer was obtained primarily in a prospective manner through questionnaires and medical record review performed at the time of the MBI examination. We examined only those factors previously shown to be associated with BPU [14]. Missing information was retrospectively abstracted by research nurses.
Molecular breast imaging procedure
MBI examinations were performed using one of two dedicated dual-head gamma camera systems equipped with cadmium zinc telluride detectors (LumaGEM, Gamma Medica, Salem, NH, USA; or Discovery NM750b, GE Healthcare, Haifa, Israel). Patients received an intravenous injection of Tc-99m sestamibi in an arm vein. Before June 2009, MBI examinations were performed with administered doses of 740 MBq of Tc-99 m sestamibi. Changes to the MBI detectors’ collimation, system energy window settings, and radiopharmaceutical injection techniques over the course of the study period resulted in an approximately threefold gain in the number of counts that could be collected during an MBI examination, such that we were able to lower the administered dose to patients proportionally while preserving count density and image quality [17, 18]. In June 2009 and later, the administered dose was between 240 and 300 MBq of Tc-99m sestamibi. Matching of cases and controls by year of MBI served to control for any changes in MBI examinations before and after the protocol change.
Imaging commenced approximately 5 minutes after injection. Bilateral views in craniocaudal and mediolateral oblique-analogous projections were acquired for 10 minutes per view, with the breast under light compression to limit patient motion. All study participants had bilateral MBI examinations.
Background parenchymal uptake assessment
MBI examinations were retrospectively reviewed by two breast imaging radiologists with 6 and 10 years of experience, respectively, in MBI interpretation. Readers interpreted BPU independently while blinded to the participants’ case status. BPU was qualitatively assessed per breast according to a validated lexicon for gamma imaging of the breast as one of four categories: photopenic, minimal to mild, moderate, or marked (Fig. 1) [19]. These categories describe the relative intensity of radiotracer uptake observed in areas of normal parenchyma compared with that in areas of subcutaneous fat, as follows: photopenic BPU, parenchymal intensity less than fat intensity; minimal to mild BPU, parenchymal intensity equal to or slightly greater than fat intensity; moderate BPU, parenchymal intensity greater than mild but less than twice as intense as fat; and marked, parenchymal intensity greater than twice fat intensity.
Examples of background parenchymal uptake categories. Molecular breast imaging (MBI) examinations and corresponding full-field digital mammograms from four different women are shown. All images were acquired in the mediolateral oblique projection. MBI with photopenic background parenchymal uptake (BPU) (a) and corresponding mammogram (b). MBI with minimal to mild BPU (c) and corresponding mammogram (d). MBI with moderate BPU (e) and corresponding mammogram (f). MBI with marked BPU (g) and corresponding mammogram (h)
Mammographic density assessment
Mammographic density was assessed on mammograms obtained closest to the time of MBI. Mammograms were available for 232 (96 %) of 241 subjects. Most mammograms were obtained within 21 days of MBI (223 [96 %] of 232). Six were obtained within 6 months, and the remaining three were obtained within 14 months of MBI. During the course of routine clinical practice, mammographic density was subjectively assessed according to ACR BI-RADS density categories (fourth edition) by breast imaging radiologists [8]. Density was also quantitatively assessed as percentage density by a trained operator using semiautomated software (Cumulus; University of Toronto, Toronto, ON, Canada [20]) as previously described [14, 21]. Percentage density was measured on right and left craniocaudal mammograms from either digitized film or “for presentation” digital mammograms in Digital Imaging and Communications in Medicine format.
Statistical analysis
Case and control characteristics are presented as mean, SD, and range for continuous variables and frequency and percentage for categorical variables. Conditional logistic regression analysis was performed to test for differences between cases and controls and to estimate the associations of BPU categories and risk of breast cancer with adjustments for covariates. Exploratory analyses were also repeated within premenopausal and postmenopausal subgroups and in a subgroup limited to invasive breast cancer cases. Further, we performed analyses on data from before and after June 2009 to examine whether changes in MBI protocol influenced the results. To measure the discriminatory ability of the models, the AUC for BPU discrimination was calculated within case-control sets to match the design.
Analysis was performed by first considering BPU as a four-category variable, using the category “minimal to mild” as a reference group because this was the largest group and provided a more stable relative risk estimate. Tests for trend were examined by including BPU as an ordinal variable in the conditional logistic regression model. Analysis was also performed considering BPU as a dichotomous variable by combining categories of “photopenic” with “minimal to mild” and “moderate” with “marked.”
The maximum BPU was used in participants whose BPU assessment differed between breasts, similarly to how clinical assessment of BI-RADS density is done [8]. To assess whether the associations were different for BPU assessed on contralateral vs. ipsilateral breasts, analyses were also done stratified by side as defined by cancer location. For this analysis, the side of the matched case was used to define the side for controls.
Interreader agreement in BPU assessment was summarized by the weighted κ statistic. κ values were interpreted as ≤0.20 or less, poor; 0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, good; and 0.81–1.00, very good agreement [22].
The χ2 test was used as appropriate to test for differences in distribution of BPU categories across BI-RADS density categories. For all comparisons, p < 0.05 was considered statistically significant. Analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC, USA).
Results
Study group characteristics
Characteristics of breast cancer cases and matched controls are shown in Table 1. As expected, cases and controls were similar on matched variables of age and menopausal status. Nearly all subjects (174 [97 %] of 179) were age-matched exactly; the remaining five subjects were age-matched within 1–3 years. Breast cancer cases had higher percentages of family history, history of atypia or lobular carcinoma in situ, mean BMI, Gail model 5-year risk, and BCSC model 5-year risk, but none of these reached statistical significance.
Of the 62 incident breast cancer cases, 45 (73 %) were invasive and 17 (27 %) were DCIS. Images from an example breast cancer case are given in Fig. 2. Details of cases are given in Additional file 1: Table S1.
Example of incident breast cancer case. Right and left mediolateral oblique views are shown. In this 41-year-old premenopausal woman, screening full-field digital mammography (a) was negative with Breast Imaging-Reporting and Data System density category of extremely dense. Supplemental screening molecular breast imaging (MBI) (b) performed at the time of the screening mammogram showed marked background parenchymal uptake. The next 2 years of screening mammography were negative. At 2.6 years after the initial MBI, the patient presented for diagnostic workup of nipple retraction. (c) MBI performed at the time showed a lesion in the left breast (arrow) that was diagnosed as a 9-mm, grade I invasive ductal carcinoma
BPU agreement
When BPU was considered as a four-category ordinal variable, interreader agreement was good (κ = 0.77, 95 % CI 0.70–0.84) with 85 % (205 of 241) agreement. When BPU was considered as a dichotomous variable, interreader agreement was good to very good (κ = 0.82, 95 % CI 0.74–0.92) with 94 % (227 of 241) agreement. BPU differed between breasts in 10 (4 %) of 241 participants (5 cases, 5 controls) for reader 1 and in 24 (10 %) of 241 participants (10 cases, 14 controls) for reader 2.
Breast cancer cases vs. controls
BPU level using either categorization was associated with breast cancer risk. When BPU was considered as a four-category variable, the BMI-adjusted OR increased with increasing BPU (Table 2). For reader 1, the OR increased from 0.8 for photopenic BPU to 3.0 for marked BPU (p-trend = 0.007). For reader 2, the OR increased from 0.5 for photopenic BPU to 6.2 for marked BPU (p-trend < 0.001).
When we considered BPU as a dichotomous variable, we found that women with moderate or marked BPU had a greater risk of incident breast cancer than women with photopenic or minimal to mild BPU. For the two readers, the BMI-adjusted ORs for moderate or marked BPU vs. photopenic or minimal to mild BPU was 3.4 (95 % CI 1.6–7.3) and 4.8 (95 % CI 2.1–10.8) (Table 3). When the dataset was limited to invasive breast cancer cases and respective matched controls, the results were similar: BMI-adjusted ORs were 3.6 (95 % CI 1.5–8.8) and 4.4 (95 % CI 1.7–11.1) for the two readers.
Neither BI-RADS density nor percentage density was statistically significantly associated with breast cancer in this study (BI-RADS ordinal OR 1.2, 95 % CI 0.7–2.0; percentage density OR [per 1 SD in square root of percentage density] 1.2, 95 % CI 0.8–1.8) (Table 1). As a result, adjustment for BI-RADS density (Table 3) and percentage density did not change BPU and breast cancer association (OR 3.3 [95 % CI 1.6–7.2] and OR 4.6 [95 % CI 2.1–10.5] for the two readers). BPU was associated with BI-RADS density in that the distribution of BPU categories differed across density categories overall (p < 0.0001), and among cases for one reader (reader 1, p = 0.04; reader 2, p = 0.10), and among controls for both readers (p < 0.001), as shown Fig. 3.
Mosaic plots show distribution of background parenchymal uptake (BPU) categories on molecular breast imaging (MBI) as a function of Breast Imaging-Reporting and Data System (BI-RADS) breast density categories for cases (a) and controls (b) interpreted by reader 1 and cases (c) and controls (d) interpreted by reader 2. BI-RADS 1 = almost entirely fat; BI-RADS 2 = scattered fibroglandular densities; BI-RADS 3 = heterogeneously dense; BI-RADS 4 = extremely dense
Additional adjustment for family history or Gail model 5-year risk within the model that included BMI and BI-RADS density adjustments had minimal impact on OR estimates. When additional adjustment for family history was made, the ORs for moderate or marked BPU vs. photopenic or minimal to mild BPU were 3.3 (95 % CI 1.5–7.2) and 4.7 (95 % CI 2.1–10.6), whereas additional adjustment for Gail model risk resulted in ORs of 3.5 (95 % CI 1.6–7.8) and 4.9 (95 % CI 2.1–11.5) for readers 1 and 2, respectively.
Moderate or marked BPU was more frequently observed among premenopausal women (26 [51 %] of 51 to 28 [55 %] of 51 for the two readers, respectively) than among postmenopausal women (25 [13 %] of 190 for both readers, p < 0.001). As shown in Table 3, the association of BPU with breast cancer remained in the postmenopausal subgroup for both readers. In the premenopausal subgroup, the association remained for reader 2 but did not reach statistical significance for reader 1. Among postmenopausal women, the results were unaffected with adjustment for use of hormone replacement therapy at the time of MBI. Finally, there was an elevated risk for the subset of cases and matched controls who had MBI with the reduced-dose protocol in June 2009 or later compared with those before June 2009 (OR 4.22 [95 % CI 1.55–11.52] and OR 8.08 [95 % CI 2.41–27.07] for the two readers), but there was no evidence for interaction (p = 0.28–0.45). The results were similar when we considered BPU assessment from the contralateral vs. ipsilateral breast for cancer cases and their respective matched controls (Additional files 2: Table S2).
The ability to discriminate between cases and controls, as assessed by the AUC, was 0.56 (95 % CI 0.48–0.63) for a model including BMI and BI-RADS mammographic density (age and menopausal status were matching variables). The addition of BPU to this model including BMI and density resulted in AUCs of 0.64–0.67 (Table 3).
Discussion
We present the first evidence for BPU on MBI as a risk factor for breast cancer. The ORs of developing breast cancer for women with moderate or marked BPU, compared with those with photopenic or minimal to mild BPU, were 3.4 and 4.8 for two readers, respectively. This association was unaffected by adjustment for mammographic density measures. The association was also unaffected by use of postmenopausal therapy and remained in analysis limited to postmenopausal women only in order to eliminate potential cyclic effects on BPU seen in premenopausal women. The association between BPU and breast cancer also remained in analysis limited to invasive breast cancer cases only. Last, the association was similar in analyses performed using BPU assessed on the ipsilateral breast vs. contralateral breast, suggesting that BPU is a general marker of breast cancer risk rather than being specific to the side of the eventual cancer.
The magnitude of the associations of breast cancer risk with BPU found in this study are comparable to the association of breast cancer with biopsy findings of atypical hyperplasia (relative risk 4.2) [23], noting the possible relevance for BPU information to be used in risk stratification. As shown in this study and previous work, BPU can vary substantially among women with similar mammographic density [14], suggesting that BPU provides risk information beyond associations with density.
While mammographic density is established as an important breast cancer risk factor, a growing body of work supports the existence of additional anatomical and functional features of breast fibroglandular tissue that differ in discriminatory capacity for predicting breast cancer risk. For instance, extraction of breast density’s textural features has shown potential to improve risk discrimination over BI-RADS density categories and quantitative density assessment [24–26]. In contrast to these mammographic measures that depict fibroglandular tissue’s anatomical appearance, BPU on MBI provides a functional measure of Tc-99m sestamibi uptake, which is believed to be related to the presence of abundant mitochondria [27], cellular proliferation, and likely blood flow and angiogenesis as well [28].
Breast magnetic resonance (MR) imaging also depicts functional behavior of breast lesions and benign fibroglandular tissue through gadolinium-based contrast enhancement, known as benign parenchymal enhancement (BPE). Similar to our findings with BPU on MBI, BPE on MR imaging is influenced by hormonal and reproductive risk factors [29, 30] and has been associated with breast cancer diagnosis in two studies with case-control designs, reporting ORs of 3.3–10.1, though these studies were not restricted to incident breast cancer cases [31, 32]. Similarly to Tc-99m sestamibi, accumulation of gadolinium chelate agents in breast tumors is related to angiogenesis and vascular permeability [33]. One study has shown Tc-99m sestamibi uptake and gadolinium enhancement in background parenchyma to be correlated [34]. Several studies have shown a lack of correlation between BPE and mammographic density [35–37].
Within the Mayo Clinic practice, MBI is currently offered to the population of women with mammographically dense breasts (BI-RADS density c or d) who seek supplemental screening but do not meet criteria for breast MR (>20 % lifetime risk by familial risk models) [38]. Also, MBI is used for women in whom MR is recommended but cannot be performed due to contraindications, including inability or unwillingness to pay for an MR examination.
Supplemental MBI screening in dense breasts has been shown to offer a relatively high incremental cancer detection rate (8.8 cancers per 1000 women screened), a low false-positive rate (18 % for mammography with supplemental MBI), and lower cost per cancer detected compared with mammography alone [5, 39]. These factors, coupled with ability to now perform MBI at radiation doses acceptable for routine screening [40], support continued consideration of MBI as a suitable screening option for women with dense breasts. In addition to the role of MBI in supplemental screening, findings from this study also support further investigation into whether MBI may be useful as a risk prediction tool, especially if incorporated with other clinical risk predictors.
A strength of our study was the inclusion of only incident breast cancer cases, diagnosed at least 180 days after index MBI. This study design allowed us to establish BPU as a risk factor for future development of breast cancer, thus supporting the potential utility of BPU in risk prediction. While a case-control study including prevalent cases [31, 32] could identify factors associated with a current breast cancer diagnosis, it would not necessarily identify factors to be used in predicting subsequent risk. Further, by excluding cases at the time of index MBI as well as patients with breast cancer history who may have had noticeable treatment effects, we avoided introducing potential bias into the interpretation of BPU.
Our study had several limitations. First, BPU was assessed as a subjective measure, which led to some differences between the two readers. However, this subjective measure represents how MBI is currently read in practice, and the two readers agreed on BPU assessment in 94 % of subjects.
A second potential limitation of our study was that we did not have follow-up on approximately 6 % (183 of 3085) of patients in our MBI database from which the breast cancer cases were selected. Therefore, it is possible that we could have missed some breast cancers diagnosed outside our institution. However, we matched on known follow-up time, so our controls represented our cases and we do not anticipate a systematic bias.
Finally, the study data lacked specific information on day of menstrual cycle at which MBI was performed among premenopausal women. In a prior cross-sectional analysis including 417 premenopausal or perimenopausal women, no association between BPU category and follicular vs. luteal phase was found (p = 0.65) [14]. However, in a subsequent study of 42 premenopausal women with regular menstrual cycles, serial MBIs were timed to be performed at peak follicular and luteal phases. Within-woman analyses showed high BPU (moderate or marked) to be observed more frequently at luteal phase than follicular phase [15]. It is currently unclear whether menstrual cycle effects on BPU have associations with breast cancer risk. However, our finding of a strong association between breast cancer and BPU in the postmenopausal subgroup, even after adjustment for hormone therapy, suggests that the association of BPU with breast cancer is not simply an artifact of premenopausal cyclic variation in BPU.
Our study included primarily women with mammographically dense breasts (80 % were either heterogeneously or extremely dense). The low number of women with nondense breasts likely accounts for the lack of a statistically significant association between mammographic density measures and breast cancer observed in this population. However, since this population is the target subgroup that would receive MBI, it is appropriate for our investigation.
Conclusions
BPU, which describes the functional uptake observed within fibroglandular tissue on MBI, is strongly associated with breast cancer risk, and this association remained after adjustments for mammographic density or postmenopausal hormone use. For women with dense breasts, who comprise over 40 % of the screening-eligible population, BPU may serve as an additional risk factor to help identify the subgroup most likely to benefit from tailored screening or primary prevention options.
Abbreviations
- ACR:
-
American College of Radiology
- BCSC:
-
Breast Cancer Surveillance Consortium
- BI-RADS:
-
Breast Imaging-Reporting and Data System
- BMI:
-
body mass index
- BPE:
-
background parenchymal enhancement
- BPU:
-
background parenchymal uptake
- DCIS:
-
ductal carcinoma in situ
- HRT:
-
hormone replacement therapy
- IQR:
-
interquartile range
- LCIS:
-
lobular carcinoma in situ
- MBI:
-
molecular breast imaging
- MR:
-
magnetic resonance
- NA:
-
not applicable
References
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356(3):227–36.
Mandelson MT, Oestreicher N, Porter PL, White D, Finder CA, Taplin SH, et al. Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst. 2000;92(13):1081–7.
Berg WA, Zhang Z, Lehrer D, Jong RA, Pisano ED, Barr RG, et al. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012;307(13):1394–404.
Brem RF, Lenihan MJ, Lieberman J, Torrente J. Screening breast ultrasound: past, present and future. AJR Am J Roentgenol. 2015;204(2):234–40.
Rhodes DJ, Hruska CB, Conners AL, Tortorelli CL, Maxwell RW, Jones KN, et al. Journal club: molecular breast imaging at reduced radiation dose for supplemental screening in mammographically dense breasts. AJR Am J Roentgenol. 2015;204(2):241–51.
Vachon CM, Van Gils CH, Sellers TA, Ghosh K, Pruthi S, Brandt KR, et al. Mammographic density, breast cancer risk and risk prediction. Breast Cancer Res. 2007;9(6):217.
Vachon C, Ghosh K, Brandt K. Mammographic density: potential as a risk factor and surrogate marker in the clinical setting. Curr Breast Cancer Rep. 2013;5(3):183–93.
D’Orsi CI, Bassett LW, Berg WA. ACR BI-RADS Breast Imaging Reporting and Data System: mammography. 4th ed. Reston, VA: American College of Radiology; 2003.
Tice JA, Miglioretti DL, Li CS, Vachon CM, Gard CC, Kerlikowske K. Breast density and benign breast disease: risk assessment to identify women at high risk of breast cancer. J Clin Oncol. 2015;33(28):3137–43.
Kerlikowske K, Zhu W, Tosteson AN, Sprague BL, Tice JA, Lehman CD, et al. Identifying women with dense breasts at high risk for interval cancer: a cohort study. Ann Intern Med. 2015;162(10):673–81.
Sprague BL, Gangnon RE, Burt V, Trentham-Dietz A, Hampton JM, Wellman RD, et al. Prevalence of mammographically dense breasts in the United States. J Natl Cancer Inst. 2014;106(10):dju255. doi: 10.1093/jnci/dju255.
Are You Dense Advocacy. http://areyoudenseadvocacy.org/. Accessed 20 Apr 2016.
Conners AL, Maxwell RW, Tortorelli CL, Hruska CB, Rhodes DJ, Boughey JC, et al. Gamma camera breast imaging lexicon. AJR Am J Roentgenol. 2012;199(6):W767–74.
Hruska CB, Rhodes DJ, Conners AL, Jones KN, Carter RE, Lingineni RK, et al. Background parenchymal uptake during molecular breast imaging and associated clinical factors. AJR Am J Roentgenol. 2015;204(3):W363–70.
Hruska CB, Conners AL, Vachon CM, O’Connor MK, Shuster LT, Bartley AC, et al. Effect of menstrual cycle phase on background parenchymal uptake at molecular breast imaging. Acad Radiol. 2015;22(9):1147–56.
Bertrand KA, Tamimi RM, Scott CG, Jensen MR, Pankratz VS, Visscher D, et al. Mammographic density and risk of breast cancer by age and tumor characteristics. Breast Cancer Res. 2013;15(6):R104.
Hruska CB, Weinmann AL, Tello Skjerseth CM, Wagenaar EM, Conners AL, Tortorelli CL, et al. Proof of concept for low-dose molecular breast imaging with a dual-head CZT gamma camera. Part II. Evaluation in patients. Med Phys. 2012;39(6):3476–83.
Swanson TN, Troung DT, Paulsen A, Hruska CB, O’Connor MK. Adsorption of 99mTc-sestamibi onto plastic syringes: evaluation of factors affecting the degree of adsorption and their impact on clinical studies. J Nucl Med Technol. 2013;41(4):247–52.
Conners AL, Hruska CB, Tortorelli CL, Maxwell RW, Rhodes DJ, Boughey JC, et al. Lexicon for standardized interpretation of gamma camera molecular breast imaging: observer agreement and diagnostic accuracy. Eur J Nucl Med Mol Imaging. 2012;39(6):971–82.
Byng JW, Boyd NF, Fishell E, Jong RA, Yaffe MJ. Automated analysis of mammographic densities. Phys Med Biol. 1996;41(5):909–23.
Vachon CM, Pankratz VS, Scott CG, Maloney SD, Ghosh K, Brandt KR, et al. Longitudinal trends in mammographic percent density and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2007;16(5):921–8.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Hartmann LC, Sellers TA, Frost MH, Lingle WL, Degnim AC, Ghosh K, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005;353(3):229–37.
Manduca A, Carston MJ, Heine JJ, Scott CG, Pankratz VS, Brandt KR, et al. Texture features from mammographic images and risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2009;18(3):837–45.
Nielsen M, Vachon CM, Scott CG, Chernoff K, Karemore G, Karssemeijer N, et al. Mammographic texture resemblance generalizes as an independent risk factor for breast cancer. Breast Cancer Res. 2014;16(2):R37.
Gierach GL, Li H, Loud J, Greene MH, Chow CK, Lan L, et al. Relationships between computer-extracted mammographic texture pattern features and BRCA1/2 mutation status: a cross-sectional study. Breast Cancer Res. 2014;16(4):424.
Arbab AS, Koizumi K, Toyama K, Araki T. Uptake of technetium-99 m-tetrofosmin, technetium-99 m-MIBI and thallium-201 in tumor cell lines. J Nucl Med. 1996;37(9):1551–6.
Del Vecchio S, Salvatore M. 99mTc-MIBI in the evaluation of breast cancer biology. Eur J Nucl Med Mol Imaging. 2004;31Suppl 1:S88–96.
Kuhl CK, Bieling HB, Gieseke J, Kreft BP, Sommer T, Lutterbey G, et al. Healthy premenopausal breast parenchyma in dynamic contrast-enhanced MR imaging of the breast: normal contrast medium enhancement and cyclical-phase dependency. Radiology. 1997;203(1):137–44.
Delille JP, Slanetz PJ, Yeh ED, Kopans DB, Halpern EF, Garrido L. Hormone replacement therapy in postmenopausal women: breast tissue perfusion determined with MR imaging—initial observations. Radiology. 2005;235:36.
King V, Brooks JD, Bernstein JL, Reiner AS, Pike MC, Morris EA. Background parenchymal enhancement at breast MR imaging and breast cancer risk. Radiology. 2011;260(1):50–60.
Dontchos BN, Rahbar H, Partridge SC, Korde LA, Lam DL, Scheel JR, et al. Are qualitative assessments of background parenchymal enhancement, amount of fibroglandular tissue on MR images, and mammographic density associated with breast cancer risk? Radiology. 2015;276(2):371–80.
Knopp MV, Weiss E, Sinn HP, Mattern J, Junkermann H, Radeleff J, et al. Pathophysiologic basis of contrast enhancement in breast tumors. J Magn Reson Imaging. 1999;10(3):260–6.
Kim MY, Choi N, Ko SM, Chung HW. Background uptake of breast-specific gamma imaging: correlation with mammographic breast density and background enhancement of breast MRI. Clin Imaging. 2014;38(3):255–8.
Ko ES, Lee BH, Choi HY, Kim RB, Noh WC. Background enhancement in breast MR: correlation with breast density in mammography and background echotexture in ultrasound. Eur J Radiol. 2011;80(3):719–23.
Cubuk R, Tasali N, Narin B, Keskiner F, Celik L, Guney S. Correlation between breast density in mammography and background enhancement in MR mammography. Radiol Med. 2010;115(3):434–41.
Hansen NL, Kuhl CK, Barabasch A, Strobel K, Schrading S. Does MRI breast “density” (degree of background enhancement) correlate with mammographic breast density? J Magn Reson Imaging. 2014;40(2):483–9.
Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
Hruska CB, Conners AL, Jones KN, O’Connor MK, Moriarty JP, Boughey JC, et al. Diagnostic workup and costs of a single supplemental molecular breast imaging screen of mammographically dense breasts. AJR Am J Roentgenol. 2015;204(6):1345–53.
Hruska CB, O’Connor MK. Curies, and grays, and sieverts, oh my: a guide for discussing radiation dose and risk of molecular breast imaging. J Am Coll Radiol. 2015;12(10):1103–5.
Acknowledgements
This work was supported by grants from the National Cancer Institute (R21 CA197752), the National Center for Advancing Translational Sciences (UL1 TR000135), and the Mayo Clinic Cancer Center, Fraternal Order of Eagles Cancer Research Fund. The authors thank Matt Jensen for statistical programming support, Fang Fang Wu for performing quantitative density measurements, and research nurses Wendy Gay, Denise Herman, Mary Dugdale, and Susan Moen for abstracting covariate data. The authors also acknowledge Dr. Stephen W. Phillips for initially questioning the importance of background parenchymal uptake on molecular breast imaging.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
CBH and MKO receive royalties for licensed technologies per agreement between Mayo Clinic and Gamma Medica, a manufacturer of molecular breast imaging systems. The other authors declare that they have no competing interests.
Authors’ contributions
CBH, CGS, and CMV conceived and designed the study. DJR and MKO provided image and questionnaire data from molecular breast imaging research trials. CGS and REC performed statistical analysis and interpretation of the data. ALC, DHW, KNH, and KRB performed reading of molecular breast imaging examinations and mammography for the study. All authors contributed to the drafting and revising of the manuscript, and all read and approved the final manuscript.
Additional files
Additional file 1: Table S1.
Characteristics of 62 incident breast cancer cases. (DOC 51 kb)
Additional file 2: Table S2.
Association of background parenchymal uptake (BPU) with breast cancer for ipsilateral vs. contralateral side. (DOC 43 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hruska, C.B., Scott, C.G., Conners, A.L. et al. Background parenchymal uptake on molecular breast imaging as a breast cancer risk factor: a case-control study. Breast Cancer Res 18, 42 (2016). https://doi.org/10.1186/s13058-016-0704-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-016-0704-6