Abstract
Background
Airway compromise is a leading cause of death in unconscious trauma patients. Although endotracheal intubation is regarded as the gold standard treatment, most prehospital providers are not trained to perform ETI in such patients. Therefore, various lateral positions are advocated for unconscious patients, but their use remains controversial in trauma patients. We conducted a systematic review to investigate whether the supine position is associated with loss of airway patency compared to the lateral position.
Methods
The review protocol was published in the PROSPERO database (Reg. no. CRD42012001190). We performed literature searches in PubMed, Medline, EMBASE, Cochrane Library, CINAHL and British Nursing Index and included studies related to airway patency, reduced level of consciousness and patient position. We conducted meta-analyses, where appropriate. We graded the quality of evidence with the GRADE methodology. The search was updated in June 2014.
Results
We identified 1,306 publications, 39 of which were included for further analysis. Sixteen of these publications were included in meta-analysis. We did not identify any studies reporting direct outcome measures (mortality or morbidity) related to airway compromise caused by the patient position (lateral vs. supine position) in trauma patients or in any other patient group. In studies reporting only indirect outcome measures, we found moderate evidence of reduced airway patency in the supine vs. the lateral position, which was measured by the apnea/hypopnea index (AHI). For other indirect outcomes, we only found low or very low quality evidence.
Conclusions
Although concerns other than airway patency may influence how a trauma patient is positioned, our systematic review provides evidence supporting the long held recommendation that unconscious trauma patients should be placed in a lateral position.
Similar content being viewed by others
Background
According to the World Health Organization, airway compromise is a leading cause of death during the first hours after trauma [1]. Thus, early endotracheal intubation (ETI) has been recommended for unconscious trauma patients [2-4]. However, on a global scale, most prehospital providers are not trained to perform ETI. Furthermore, prehospital ETI has been questioned because of the potential complications [5-8].
For decades, placing an unconscious, non-intubated patient in the lateral position (“recovery position”, Figure 1) has been recommended to maintain an open airway, which is also true for trauma [9-12] (Figure 2). However, due to the fear of worsening a potential cervical spine injury, clinical guidelines and authoritative training manuals dictate that such patients should be transported in the supine position while strapped to a spine board, with a cervical collar in place [13]. Attempting to balance these two considerations, various authors have proposed the use of adapted lateral positions [14-17] (Figures 3 and 4). The lateral trauma position (LTP) has, to some extent, been implemented in clinical practice [17]. However, the positioning of unconscious trauma patients is still a controversial issue worldwide, with both medical and medico-legal implications.
We conducted a systematic review to answer the following question: In the unconscious trauma patient, is the supine position associated with a loss of airway patency compared to the lateral position?
Methods
The protocol for this review was published in the PROSPERO database for systematic reviews [18]. We used the PICO (Population, Intervention, Comparison and Outcome measures) format to develop our research question and search strategies [19]. Furthermore, we used the PRISMA checklist (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [20] as a guide to ascertain the quality of the review process and manuscript. Written informed consent was obtained from the models for publication of the accompanying images.
Inclusion criteria
Types of participants
Our main question focused on unconscious trauma patients; however, due to the expected paucity of studies specifically dealing with unconscious trauma patients, we decided to include all patients with a reduced level of consciousness (LOC), regardless of the cause and patient location.
Types of interventions and comparisons
We defined the lateral position as the intervention, which was compared with the supine position. There are many forms of lateral position that are used in the medical literature. However, we did not restrict the intervention to any specific lateral position or to how the patient was placed in that position.
Because the study question was specifically linked to the supine position, we also included studies addressing the effect of a reduced LOC on airway patency in the supine position alone.
Outcome measures
We aimed to use patient mortality (short and long term) and morbidity (e.g., aspiration, aspiration pneumonia or the Glasgow outcome scale) as the measured outcomes in our analysis. However, due to the lack of studies reporting these variables, we included the following indirect airway patency outcome measures: hypoxia, hypercapnia, hypoventilation, stridor score, apnea/hypopnea index (AHI), respiratory disturbance index (RDI), upper airway resistance (Rua) and work of breathing (WOB). If a study reported multiple relevant outcome measures, we included all of them.
Study types
We included all study designs that used a control or comparison group, including crossover studies where patients/volunteers acted as their own controls.
Search methods used to identify the studies
We searched the following databases: PubMed, Medline, EMBASE, Cochrane Library, CINAHL and British Nursing Index. We modified the terms when searching different databases, as necessary. We also performed forward and backward citation searches and manual searches of “gray” literature, such as relevant textbooks. No limits on the publication date or language were applied. The searches were updated in June 2014. Combinations of the following words and their variations were sought:
-
unconscious, Glasgow Coma Scale, coma, craniocerebral trauma, brain injury, sleep apnea
-
patient positioning, supine position, spine-/backboard, vacuum mattress
-
airway obstruction, anoxia, hypoxia, hypoventilation, hypercapnia, mortality, morbidity, Glasgow Outcome Scale
The full search strategies for all the databases searched are described in Additional file 1.
Data collection and analysis
The principal investigator (PKH) assessed all studies that were identified in the searches. The remaining authors each assessed one portion of the studies, thus two investigators independently assessed each reference. All disagreements were resolved through discussion or by consulting with a third author.
Data extraction and management
We designed a data extraction form, with which two review authors independently extracted the data from the eligible studies. Discrepancies were resolved through discussion. We extracted the following data: the first author, publication year, population, intervention and comparison details, measured outcome, measurement time and measurement method. For studies relevant to the meta-analysis, the first author entered the outcome data into the Review Manager software program [21], and another author checked the data for accuracy.
Assessing the risk of bias in the included studies
Two review authors independently assessed the risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions [22] or the checklists from the Norwegian Knowledge Centre for the Health Services [23]. We resolved any disagreement by discussion or by including a third assessor.
The risk of bias was assessed according to the sequence generation, allocation concealment, selection of groups and group comparability, blinding of the participants, provider and assessor, and incomplete outcome data, including possible attrition bias and selective reporting bias.
Measuring the treatment effect
Dichotomous data
We planned to present the results as a summary risk ratio (RR) with 95% confidence intervals (CI) [19]. However, no such data were identified.
Continuous data
We reported the mean difference (with standard deviations) when the outcomes were measured in the same manner between the trials.
Analysis
Where appropriate, we combined the results from the different studies included in a meta-analysis. We performed the statistical analysis using RevMan [21] software. Expecting differences between trials, we used random-effects meta-analysis as the default method to combine the data. We used the generic inverse-variance method available in RevMan to perform the analysis. In cases in which it was inappropriate to combine the results, we descriptively present the results in tables.
Missing data
For the included studies, we noted the level of attrition, if any. Most of the included studies were crossover studies that used the patients as their own controls; in most of these studies, there was no attrition. In the remaining studies attrition was negligible, and we performed no further analyses. For the continuous measures, we used actual measurements (no imputations).
Assessment of the heterogeneity
We examined the meta-analysis forest plot for heterogeneity among studies, and considered the size and direction of the effect, using I2 statistics to quantify the level of heterogeneity. We recommend exercising caution in interpreting the results when unexplained heterogeneity is substantial or considerable (i.e., I2 between 30 and 60% or between 50 and 100%, respectively).
Assessing the studies that were not applicable to the meta-analysis
Most of the outcomes in these studies were insufficiently reported, so that they cannot be included in analysis. We present these studies according to the measured outcomes, which are described in the tables. Differences are noted as favoring one of the positions, designated by “+” for favoring the intervention (the lateral position) or “-“ for favoring the control (the supine position), and by “?” when the direction is unclear or not significant in favor of one of the positions.
Grading the quality of evidence
We used the GRADE methodology to grade the quality of evidence for each of the critically important outcomes with sufficient results presented [24]. For each outcome, the quality of the evidence was assessed using the eight GRADE criteria: five criteria for downgrading (study limitations, heterogeneity, indirectness of the evidence, imprecision, and reporting bias) and three criteria for upgrading (large effect, dose–response gradient, and plausible confounding). The outcomes that were insufficiently reported are associated with large uncertainty and should be interpreted with caution.
Results
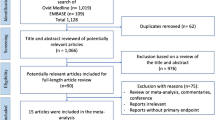
We did not identify any specific studies involving unconscious trauma patients and airway patency using patient mortality or morbidity as the measured outcomes. In addition, we did not find any trauma patient studies reporting indirect outcomes. Broadening the inclusion criteria to all patients with reduced consciousness, we still did not identify any studies reporting direct outcome measures (i.e., mortality or morbidity). However, when including studies that reported indirect outcome measures, we identified 1,316 unique publications, of which 43 were included for further analysis (Figure 5). Some of the included studies were randomized control trials (RCTs) that were designed to evaluate other interventions, but they included baseline data that were useful for our comparisons. We included these baseline data comparisons as observational data in our review.
We were able to combine the results from 20 publications (34 comparisons) in a meta-analysis (Figure 6). None of the included studies reported dichotomous outcome measures. The excluded articles and the reasons for their exclusion are summarized in Additional file 2.
We included 20 studies with a total of 34 comparisons in the meta-analysis. Some of the studies reported data from more than one group: REM-sleep1, 6; non-REM sleep3, 5; positional obstructive sleep apnea (OSA)2, 4, 18; non-positional OSA7, 8; with tonsillo-andenomegaly9; with adenoid hypertrophy17; no obstruction15; at 40-44 weeks post-conseptional age16; at 45-49 weeks post-conseptional age14; at 50-54 weeks post-conseptional age10; at 55-59 weeks post-conseptional age12; left lateral vs. supine position11; right lateral vs. supine position13; preoperative night18, first19 and third20 postoperative night.
Studies investigating only the supine position
We identified five studies [25-29] comparing the airway patency of awake patients in the supine position to the airway patency of the same patients during a reduced LOC. The causes of the reduced LOC were general anesthesia, drug-induced sedation or sleep. Using different types of indirect outcome measures, all studies indicated that reduced LOC in the supine position was associated with worsened airway patency (Table 1).
Studies of the lateral vs. supine positions
The included studies reported a multitude of outcome measures, including oxygen desaturation, stridor score, upper airway resistance (Rua), closing pressure (Pcrit and Pclose), minute ventilation (MV) volume, RDI, and AHI. Most of these studies could not be included in the meta-analysis, but the results are summarized in terms of the direction of the effect (Tables 2, 3, 4, and 5).
Oxygen desaturation was reported in six studies (a total of 472 cases) [30,31,33-36] in various manners (e.g., the mean peripheral oxygen saturation [Sp02], mean lowest Sp02, and time between the desaturation episodes). In four of the comparisons (representing 217 persons), there was an indication of better oxygenation in the lateral position vs. the supine position. For the remaining comparisons, the differences were clinically insignificant (Table 2).
The stridor score, a four-step scale ranging from total obstruction to normal air passage (judged by stethoscopy) was reported in two studies [36,37]. The participants included 48 children under general anesthesia in the lateral and supine positions. Airway obstruction was reduced in the lateral vs. the supine positions. The addition of jaw thrust and/or chin lift further reduced the obstruction (Table 3).
Upper airway resistance was reported in one study [38], in which there was a small difference between the two positions in favor of the lateral position (Table 3).
The upper airway closing pressure was reported in two studies (n = 24) [39,40] as a measure of collapsibility. Both studies observed a lower collapsibility in the lateral position than in the supine position (Table 3).
The inspiratory minute volume (MV) was reported in one study [38], and there was a small difference in favor of the lateral position (Table 3).
The volume of the upper airway was reported in one study [41], wherein there was a greater volume in the lateral position (Table 3).
The RDI (the number of episodes of apnea, hypopnea and respiratory-effort related arousals per hour) was reported in three studies [42-44]. Two of these studies included adults: one study included adults with cervical spine injuries, and the other included adults with stroke. The third study included children with possible obstructive sleep apnea. In these three studies, the investigators reported a statistically significant reduction in the RDI in the lateral position vs. the supine position (Table 4).
The AHI (the number of episodes of apnea or hypopnea per hour) was reported in 27 studies. In seven of these studies [34,45-50], the AHI was incompletely reported, and, therefore, could not be included in the meta-analysis. However, four of the six studies showed a reduction of the AHI in the lateral position, indicating improved airway patency (Table 5).
Seventeen studies [31,35,51-65] of adults with sleep apnea, stroke, or undergoing surgery, with 26 comparisons, were suitable for meta-analysis (Figure 6). In all three groups, the lateral position significantly reduced the AHI compared to the supine position. In infants and small children [66-68], there was no significant difference between the two positions (Figure 6).
Grading the evidence
Table 6 show the Summary of findings table for the comparison between the lateral and the supine position for patients with reduced consciousness. Full details are shown in the GRADE evidence profile (Additional file 3). The quality of the evidence was moderate for one of the four outcome comparisons. For the remainder, we rated the quality of evidence as low or very low.
Discussion
In our systematic review of airway patency in unconscious trauma patients, we focused on the effect of placing the patient in the supine position vs. the lateral position. We did not identify any studies reporting mortality, morbidity or other, more indirect, outcome measures in trauma patients. One reason for the lack of such studies could be the associated logistical and ethical issues [69,70]. Another likely cause is that placing unconscious patients in the lateral position is considered to be an obvious solution and regarded as a truth (“textbook knowledge”) that does not require investigation. Thus, this practice may be regarded as a dogma, a strong belief based on experience more than scientific evidence. However, many EMS systems worldwide dictate the use of rigorous supine immobilization regimes in unconscious trauma patients [13,71,72]. We view this practice as an unsolved contradiction.
Due to the lack of specific studies in trauma patients, we decided to broaden the inclusion criteria to patients who had reduced level of consciousness from all causes. Five studies compared the supine airway patency in the awake vs. unconscious states [25-28]. One of these studies is the 1959 milestone publication by Peter Safar et al. [25]. In this study, the investigators anesthetized 80 elective surgery patients in the supine position and scored the airways as either open or partially or totally obstructed. In the neutral head position, 36% of the patients had total obstruction, while 54% had partial obstruction. These findings may have been considered to be proof that does not require further investigation. The findings in Safar’s study provide strong evidence that the supine position may endanger the airway in all unconscious patients. We see no reason to suspect that this conclusion is not true in unconscious trauma patients; on the contrary, trauma may further endanger the airway with factors such as bleeding from facial injuries and gastrointestinal regurgitation.
In patients with reduced consciousness, we found evidence that the lateral position is better for securing an open airway than the supine position in a variety of settings. Our findings support the long-held recommendation to use a lateral position for all unconscious patients, including trauma. However, there are several caveats to the interpretation of our findings.
There are several limitations to the material available for this systematic review and meta-analysis. The first and foremost is the lack of direct endpoints and the absence of RCTs. The quality of evidence is lowered by indirectness in population. However, the effect size of the lateral position for improved airway patency (reduced AHI) in adults led to upgrading the quality of the evidence. During sleep, the difference between the two positions is likely to be greater with deeper levels of unconsciousness. We found considerable unexplained heterogeneity regarding the size of effect on AHI between the studies for adults; however, we did not downgrade for this variation.
Another limitation is that we did not address other concerns that were linked to the lateral positioning of trauma patients. One such concern is whether turning a patient with a cervical spine injury from the supine to the lateral position worsens the injury. We are in the process of addressing this question in a separate systematic review [18].
Conclusions
In this systematic review, we did not identify any studies that investigated the supine position and loss of airway patency in trauma patients. However, we found that the supine position was associated with worse airway patency in patients with reduced levels of consciousness in a variety of settings. We also observed that the lateral position was associated with improved airway patency compared to the supine position. Although concerns other than airway patency may influence how the trauma patient is positioned, our systematic review provides evidence supporting the long-held recommendation to place the unconscious trauma patient in a lateral position.
Consent
Written informed consent was obtained from the models for publication of the accompanying images.
References
Sasser S, Varghese M, Kellermann A, Lormand JD. 2.2.1 The need. In: Sasser S, Varghese M, Kellermann A, Lormand JD, editors. Prehospital trauma care systems. Geneva: World Health Organization; 2005. p. 7–8.
Smith CE, Walls RM, Lockey D, Kuhnigk H. Advanced Airway Management and Use of Anesthetic Drugs. In: Søreide E, Grande CM, editors. Prehospital Trauma Care. New York: Marcel Dekker, Inc; 2001. p. 203–53.
PHTLS Committee of NAEMT. Airway and Ventilation. In: McSwain NE, editor. PHTLS - Basic and Advanced Prehospital Trauma Life Support. 7th ed. St. Louis: Mosby JEMS, Elsevier; 2011. p. 133–77.
American College of Surgeons Committee on Trauma. Airway and Ventilatory Management. In: Rotondo MF, editor. Advanced Trauma Life Support for Doctors - Student Course Manual. 9th ed. Chicago: American College of Surgeons; 2012. p. 30–49.
Stiell IG, Nesbitt LP, Pickett W, Munkley D, Spaite DW, Banek J, et al. The OPALS Major Trauma Study: impact of advanced life-support on survival and morbidity. CMAJ. 2008;178:1141–52.
Davis DP, Peay J, Sise MJ, Vilke GM, Kennedy F, Eastman AB, et al. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J Trauma. 2005;58:933–9.
Lossius HM, Roislien J, Lockey DJ. Patient safety in pre-hospital emergency tracheal intubation: a comprehensive meta-analysis of the intubation success rates of EMS providers. Crit Care. 2012;16:R24.
Jayaraman S, Sethi D. Advanced trauma life support training for ambulance crews. Cochrane Database of Systematic Reviews 2010;(1):CD003109. doi: 10.1002/14651858.CD003109.
NATO. Emergency War Surgery Handbook. Paris: Supreme Headquarters, Allied Powers Europe; 1957.
Dam W, Edmund HH, Ibsen HP, Poulsen H, Rømer O. On complications during transport of patients with threatend airways in Denmark [Om komplikationer af respirationstruede patienter i Danmark]. In: Wulf HB, editor. Road Traffic Injuries in Scandinavia [Trafikskador i Skandinavien]. Lund: Nordisk Kirurgisk Förening/Berlingska Boktryckeriet; 1957. p. 205–10.
Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L. European Resuscitation Council guidelines for resuscitation 2005. Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2005;67(1):S7–23.
Deakin CD, Nolan JP, Soar J, Sunde K, Koster RW, Smith GB, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult advanced life support. Resuscitation. 2010;81:1305–52.
Theodore N, Hadley MN, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, et al. Prehospital cervical spinal immobilization after trauma. Neurosurgery. 2013;72 Suppl 2:22–34.
Haines J. Positioning an unconscious patient with suspected neck injury. JEMS: Journal of Emergency Medical Services. 1996;21:85.
Blake WE, Stillman BC, Eizenberg N, Briggs C, McMeeken JM. The position of the spine in the recovery position–an experimental comparison between the lateral recovery position and the modified HAINES position. Resuscitation. 2002;53:289–97.
Berlac P, Hyldmo PK, Kongstad P, Kurola J, Nakstad AR, Sandberg M. Pre-hospital airway management: guidelines from a task force from the Scandinavian Society for Anaesthesiology and Intensive Care Medicine. Acta Anaesthesiol Scand. 2008;52:897–907.
Fattah S, Ekas GR, Hyldmo PK, Wisborg T. The lateral trauma position: What do we know about it and how do we use it? A cross-sectional survey of all Norwegian emergency medical services. Scand J Trauma Resusc Emerg Med. 2011;19:45.
Hyldmo PK, Vist G, Søreide E, Rognås L, Magnusson V, Feyling AC. Is the lateral position a safe and useful method for basic airway management in trauma?. PROSPERO 2012:CRD42012001190 Available from http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42012001190.
O’Connor D, Green S, Higgins JPT. Defining the review question and developing criteria for including studies. In: Cochrane Handbook for Systematic Reviews of Interventions Edited by Higgins JPT, Green S. Chichester: John Wiley & Sons Ltd; 2008. p. 83–94.
Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
The Nordic Cochrane Centre: Review manager (RevMan), ver. 5.2. http://tech.cochrane.org/revman.
Higgins JPT, Altman DG. Assessing risk of bias in included studies. In: Cochrane Handbook for Systematic Reviews of Interventions Edited by Higgins JPT, Green S. Chichester: John Wiley & Sons Ltd; 2008. p. 187–241.
The Norwegian Knowledge Centre for the Health Services (Nasjonalt kunnskapssenter for helsetjenesten: Sjekklister for vurdering av forskningsartikler. 2012: http://www.kunnskapssenteret.no/verktoy/sjekklister-for-vurdering-av-forskningsartikler. Last accessed 28 Febr 2015.
Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–6.
Safar P, Escarraga LA, Chang F. Upper airway obstruction in the unconscious patient. J Appl Physiol. 1959;14:760–4.
Kopelman PG, Apps MC, Cope T, Ingram DA, Empey DW, Evans SJ. Nocturnal hypoxia and sleep apnoea in asymptomatic obese men. Int J Obes. 1986;10:211–7.
Ikeda H, Ayuse T, Oi K. The effects of head and body positioning on upper airway collapsibility in normal subjects who received midazolam sedation. J Clin Anesth. 2006;18:185–93.
Lee MY, Lin CC, Shen SY, Chiu CH, Liaw SF. Work of breathing in eucapnic and hypercapnic sleep apnea syndrome. Respiration. 2009;77:146–53.
Tagaito Y, Isono S, Tanaka A, Ishikawa T, Nishino T. Sitting posture decreases collapsibility of the passive pharynx in anesthetized paralyzed patients with obstructive sleep apnea 18. Anesthesiology. 2010;113:812–8.
Rosenberg-Adamsen S, Stausholm K, Edvardsen L, Zwarts M, Kehlet H, Rosenberg J. Body position and late postoperative nocturnal hypoxaemia. Anaesthesia. 1997;52:589–92.
Cao EH, Shi Y, Zhang W, Tong MR, Song Y, Zhao BB, et al. Influence of sleep position on respiratory function of patients with sleep apnea/hypopnea syndrome. Chin J Clin Rehabil. 2005;9:215–7.
Shao C, Li WJ, Li SQ, Wu XD, Zhou J, Lu SY, et al. Monitoring results and correlation analysis of polysomnography in 110 cases of elderly patients with obstructive sleep apnea-hypopnea syndrome. Respirology 2011:236.
Oksenberg A, Khamaysi I, Silverberg DS, Tarasiuk A. Association of body position with severity of apneic events in patients with severe nonpositional obstructive sleep apnea. Chest. 2000;118:1018–24.
Sasai T, Inoue Y, Matsuo A, Matsuura M, Matsushima E. Changes in respiratory disorder parameters during the night in patients with obstructive sleep apnoea. Respirology. 2011;16:116–23.
Browaldh N, Nerfeldt P, Lysdahl M, Bring J, Friberg D. SKUP3 randomised controlled trial: polysomnographic results after uvulopalatopharyngoplasty in selected patients with obstructive sleep apnoea. Thorax. 2013;68:846–53.
Arai YC, Fukunaga K, Hirota S, Fujimoto S. The effects of chin lift and jaw thrust while in the lateral position on stridor score in anesthetized children with adenotonsillar hypertrophy. Anesth Analg. 2004;99:1638–41.
Arai YC, Fukunaga K, Ueda W, Hamada M, Ikenaga H, Fukushima K. The endoscopically measured effects of airway maneuvers and the lateral position on airway patency in anesthetized children with adenotonsillar hypertrophy. Anesth Analg. 2005;100:949–52.
Jordan AS, Eckert DJ, Catcheside PG, McEvoy RD. Ventilatory response to brief arousal from non-rapid eye movement sleep is greater in men than in women. Am J Respir Crit Care Med. 2003;168:1512–9.
Penzel T, Moller M, Becker HF, Knaack L, Peter JH. Effect of sleep position and sleep stage on the collapsibility of the upper airways in patients with sleep apnea. Sleep. 2001;24:90–5.
Isono S, Tanaka A, Nishino T. Lateral position decreases collapsibility of the passive pharynx in patients with obstructive sleep apnea. Anesthesiology. 2002;97:780–5.
Litman RS, Wake N, Chan LM, McDonough JM, Sin S, Mahboubi S, et al. Effect of lateral positioning on upper airway size and morphology in sedated children. Anesthesiology. 2005;103:484–8.
McEvoy RD, Mykytyn I, Sajkov D, Flavell H, Marshall R, Antic R, et al. Sleep apnoea in patients with quadriplegia. Thorax. 1995;50:613–9.
Turkington PM, Bamford J, Wanklyn P, Elliott MW. Prevalence and predictors of upper airway obstruction in the first 24 hours after acute stroke. Stroke. 2002;33:2037–42.
Pereira KD, Roebuck JC, Howell L. The effect of body position on sleep apnea in children younger than 3 years. Arch Otolaryngol Head Neck Surg. 2005;131:1014–6.
Do Prado LBF, Li XB, Thompson R, Marcus CL. Body position and obstructive sleep apnea in children. Sleep. 2002;25:66–71.
Li YR, Han DM, Ye JY, Zhang YH, Yin GP, Wang XY, et al. Sites of obstruction in obstructive sleep apnea patients and their influencing factors: an overnight study. Chinese Journal of Otorhinolaryngology Head and Neck Surgery. 2006;41:437–42.
Zhang X, Li Y, Zhou F, Guo C, Huang Z. Association of body position with sleep architecture and respiratory disturbances in children with obstructive sleep apnea 83. Acta Otolaryngol (Stockh). 2007;127:1321–6.
Kim TW, Yoo B, Choi J, Lim HK, Lee SP, Hong SC: The role of sleep position in obstructive sleep apnea syndrome in Korean people. Sleep Biol Rhythms 2011, Conference: Worldsleep 2011:276.
Svatikova A, Chervin RD, Wing JJ, Sanchez BN, Migda EM, Brown DL. Positional therapy in ischemic stroke patients with obstructive sleep apnea. Sleep Med. 2011;12:262–6.
Nisbet LC, Phillips NN, Hoban TF, O’Brien LM. Effect of body position and sleep state on obstructive sleep apnea severity in children with Down syndrome. J Clin Sleep Med. 2014;10:81–8.
Cartwright R, Ristanovic R, Diaz F, Caldarelli D, Alder G. A comparative study of treatments for positional sleep apnea. Sleep. 1991;14:546–52.
Jokic R, Klimaszewski A, Crossley M, Sridhar G, Fitzpatrick MF. Positional treatment vs continuous positive airway pressure in patients with positional obstructive sleep apnea syndrome. Chest. 1999;115:771–81.
Younes M. Contributions of upper airway mechanics and control mechanisms to severity of obstructive apnea. Am J Respir Crit Care Med. 2003;168:645–58.
Cartwright RD. Effect of sleep position on sleep apnea severity. Sleep. 1984;7:110–4.
Szollosi I, Roebuck T, Thompson B, Naughton MT. Lateral sleeping position reduces severity of central sleep apnea/Cheyne-Stokes respiration. Sleep. 2006;29:1045–51.
Weihu C, Jingying Y, Demin H, Boxuan W. Relationship of body position, upper airway morphology, and severity of obstructive sleep apnea/hypopnea syndrome among chinese patients. Acta Otolaryngol (Stockh). 2011;131:173–80.
George CF, Millar TW, Kryger MH. Sleep apnea and body position during sleep. Sleep. 1988;11:90–9.
Bahammam AS, Tate R, Manfreda J, Kryger MH. Upper airway resistance syndrome: effect of nasal dilation, sleep stage, and sleep position. Sleep. 1999;22:592–8.
Chung JW, Enciso R, Levendowski DJ, Westbrook PR, Clark GT. Patients with positional versus nonpositional obstructive sleep apnea: a retrospective study of risk factors associated with apnea-hypopnea severity. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:605–10.
Wierzbicka A, Rola R, Wichniak A, Richter P, Ryglewicz D, Jernajczyk W. The incidence of sleep apnea in patients with stroke or transient ischemic attack. J Physiol Pharmacol. 2006;57:90.
Dziewas R, Hopmann B, Humpert M, Ritter M, Dittrich R, Schabitz WR, et al. Positional sleep apnea in patients with ischemic stroke. Neurol Res. 2008;30:645–8.
Permut I, Diaz-Abad M, Chatila W, Crocetti J, Gaughan JP, D’Alonzo GE, et al. Comparison of positional therapy to CPAP in patients with positional obstructive sleep apnea. J Clin Sleep Med. 2010;6:238–43.
Sunwoo WS, Hong SL, Kim SW, Park SJ, Han DH, Kim JW, et al. Association between Positional Dependency and Obstruction Site in Obstructive Sleep Apnea Syndrome. Clin Exp Otorhinolaryngol. 2012;5:218–21.
Chung F, Liao P, Elsaid H, Shapiro CM, Kang W. Factors Associated with Postoperative Exacerbation of Sleep-disordered Breathing. Anesthesiology. 2014;120:299–311.
Ozeke O, Erturk O, Gungor M, Hizel SB, Aydin D, Celenk MK, et al. Influence of the right- versus left-sided sleeping position on the apnea-hypopnea index in patients with sleep apnea. Sleep & breathing = Schlaf & Atmung. 2012;16:617–20.
Orr WC, Stahl ML, Duke J, McCaffree MA, Toubas P, Mattice C, et al. Effect of sleep state and position on the incidence of obstructive and central apnea in infants. Pediatrics. 1985;75:832–5.
Cuhadaroglu C, Keles N, Erdamar B, Aydemir N, Yucel E, Oguz F, et al. Body position and obstructive sleep apnea syndrome. Pediatr Pulmonol. 2003;36:335–8.
Pereira KD, Rathi NK, Fatakia A, Haque SA, Castriotta RJ. Body position and obstructive sleep apnea in 8-12-month-old infants. Int J Pediatr Otorhinolaryngol. 2008;72:897–900.
Singer EA, Mullner M. Implications of the EU directive on clinical trials for emergency medicine. BMJ. 2002;324:1169–70.
Robinson K, Andrews PJ. ‘(More) trials and tribulations’: the effect of the EU directive on clinical trials in intensive care and emergency medicine, five years after its implementation. J Med Ethics. 2010;36:322–5.
PHTLS Committee of NAEMT. Spinal Trauma. In: McSwain NE, editor. PHTLS - Basic and Advanced Prehospital Trauma Life Support. 7th ed. St. Louis: Mosby JEMS, Elsevier; 2011.
Anonymous. Neck and Back Trauma. In: Fisher JD, Brown SN, Cooke M, Walker A, Moore F, Chrispin P, editors. UK Ambulance Services Clinical Practice Guidelines 2013. Bridgewater: Class Professional Publishing; 2013.
Acknowledgements
We thank Senior Librarian Hege Sletsjøe at the Norwegian Directorate of Health for designing the search strategy and performing the searches, as well as Librarian Gyri Hval Straumann at the Norwegian Knowledge Center for the Health Services for updating the searches.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
PKH developed the concept of the LTP in Norway but has received no economic benefits from this concept. The other authors declare that they have no competing interests.
Authors’ contributions
PKH developed the research question. All authors participated in preparing the protocol, inclusion process, data extraction and analysis, and manuscript. GEV was the research group’s systematic review method expert.
Additional files
Additional file 1:
Search strategy.
Additional file 2:
Excluded full text articles.
Additional file 3:
GRADE evidence profile.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hyldmo, P.K., Vist, G.E., Feyling, A.C. et al. Is the supine position associated with loss of airway patency in unconscious trauma patients? A systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med 23, 50 (2015). https://doi.org/10.1186/s13049-015-0116-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-015-0116-0