Abstract
Background
Prone position is an option for rescue therapy for acute respiratory distress syndrome. However, there are limited relevant data among trauma and surgical patients, who may be at increased risk for complications following position changes. This study aimed to identify the benefits and risks of proning in this patient subgroup.
Methods
Follow the PRISMA 2020, MEDLINE and EMBASE database searches were conducted. Additional search of relevant primary literature and review articles was also performed. A random effects model was used to estimate the PF ratio, mortality rate, mechanical ventilator days, and intensive care unit length of stay using Review Manager 5.4.1 software.
Results
Of 1,128 studies, 15 articles were included in this meta-analysis. The prone position significantly improved the PF ratio compared with the supine position (mean difference, 79.26; 95% CI, 53.38 to 105.13). The prone position group had a statistically significant mortality benefit (risk ratio [RR], 0.48; 95% CI, 0.35 to 0.67). Although there was no significant difference in the intensive care unit length of stay, the prone position significantly decreased mechanical ventilator days (-2.59; 95% CI, -4.21 to -0.97). On systematic review, minor complications were frequent, especially facial edema. There were no differences in local wound complications.
Conclusions
The prone position has comparable complications to the supine position. With its benefits of increased oxygenation and decreased mortality, the prone position can be considered for trauma and surgical patients. A prospective multicenter study is warranted.
Similar content being viewed by others
Background
Regarding the Berlin definition 2012, acute respiratory distress syndrome (ARDS) is an acute respiratory failure with bilateral opacities which is not fully explained by cardiac failure or fluid overload. It has been classified into 3 severities based on the ratio of arterial oxygen partial pressure to fractional inspired oxygen (PF ratio) with PEEP or CPAP at least 5 cmH2O [1]. In the LUNG SAFE study [2], the largest observational ARDS study, the geographic variation in ARDS incidence ranged from 0.27 to 0.57 cases per intensive care unit (ICU) bed per 4 weeks, comprising 10% of ICU admissions. The primary diagnosis among most ARDS patients in this study was medical or surgical (65%), with trauma patients comprising 46% of over one hundred surgical patients included.
Prone positioning is theoretically helpful in ARDS by increasing homogeneous ventilation distribution, modifying chest wall and lung compliance/elastance, reducing ventilator-induced lung injury (VILI) and facilitating secretion mobilization and clearance [3]. PROSEVA trial, a large multi-center randomized control study, demonstrated that early application of prolonged prone-positioning significantly decreased mortality among severe ARDS patients [4]. However, it must be noted that studies on the benefits of prone positioning in ARDS have been performed primarily among medical patients (79–89%), with surgical patients making up only 4–9% and trauma patients comprising only 2–7% of all patients examined [4, 5]. Because trauma and surgical patients may be at increased risk from position changes as compared to medical patients, it is possible that the balance of risks and benefits for prone positioning in ARDS are different in this specific subset of patients.
Because of the limited evidence of the use of prone positioning among ARDS patients specifically among trauma or surgical patients, we endeavoured to determine the effect of prone positioning towards ARDS outcomes (P/F ratio - the ratio of arterial oxygen partial pressure to fractional inspired oxygen, mortality, ICU length of stay and mechanical ventilator day) among trauma and surgical patients.
Methods
Eligibility criteria
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) [6]. We applied the following inclusion criteria: trials studying the prone position and acute respiratory distress syndrome and trauma-surgical patient. All experimental and cohort studies, whether retrospective or prospective, were included. Exclusion criteria were as follows: case report, case series and ongoing trials. The outcome measures were P/F ratio, mortality, ICU length of stay and mechanical ventilator days.
Information sources and search strategy
Electronic systematic searches were conducted for articles published before November 30, 2022, using MEDLINE and EMBASE. The medical subject headings used in our searches were “trauma,” “surgical,” “acute respiratory failure,” and “prone position.” There was no language restriction.
Study selection and data collection
Two investigators (V.P. and N.O.) independently selected prospective studies using the predetermined eligibility criteria by title and abstract screening. The references of the included studies were also manually reviewed for additional relevant studies. Disagreements relating to any aspect of the data extraction process were resolved through discussion with the third investigator (W.O.), with the final decision made by consensus. The full-text articles of the selected studies were reviewed for the final study selection. The data were extracted and analyzed from the included studies.
Characteristics of included studies
The studies included in this meta-analysis were cohort or experimental studies (prospective or retrospective) of trauma or surgical patients diagnosed with ARDS.
Quality assessment
Regarding Cochrane recommendation, two investigators (V.P. and N.O.) assessed the quality of each study using the Cochrane risk-of bias tool for randomized trials (RoB 2) and the Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) for non-randomised studies [7, 8].
Statistical analysis
All statistical analyses were performed using Review Manager 5.4.1 software from the Cochrane Collaboration (London, United Kingdom). We extracted the proportions and 95% confidence intervals (CIs) from each study and pooled them using the random effect model. Cochran’s Q test was performed and quantified using the I2 statistic to determine the statistical heterogeneity among the included studies. An I2 value of 0–25% represents insignificant heterogeneity, greater than 25% but less than or equal to 50% represents low heterogeneity, greater than 50% but less than or equal to 75% represents moderate heterogeneity, and greater than 75% represents high heterogeneity. P-value less than 0.05 were considered statistically significant. The presence of a publication bias was visualized by a funnel plot. This study was registered at as http://www.inplasy.com as #INPLASY202330102.
Results
Search results
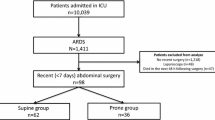
We identified 1,128 unique citations (Fig. 1) and reviewed the full text of 90 studies to ascertain eligibility. Fifteen studies (628 patients) were included in this systematic review. There were 2 randomized control trials [9, 10], 5 retrospective cohort studies [11,12,13,14,15], 2 prospective experimental studies [16, 17], and 6 retrospective experimental studies [18,19,20,21,22,23].
The study characteristics are listed in Table 1. The included studies consisted of postoperative abdominal surgery patients (3 studies) [11, 14, 21], postoperative cardiothoracic surgery patients (5 studies) [10, 13, 19, 20, 22], trauma patients (4 studies) [9, 15, 16, 18], and mixed postoperative and trauma patients (2 studies) [12, 17], and burn patients (1 study) [23]. The prone duration ranged from 4 to 18 h per session. The studies conducted duration of prone position less than 12 h were 6 studies [9, 10, 12, 13, 16, 17], while the studies conducted duration of prone per session with 12 h or greater were 9 studies [11, 14, 15, 18,19,20,21,22,23].
Effects of intervention
Primary outcome
A pooled analysis was performed on the 16 studies using a random effects model. The prone position showed a significantly improved PF ratio compared with the supine position. The mean difference was 79.26 (95% CI, 53.38 to 105.13; I2, 94%) (Fig. 2). This significant improvement was also demonstrated in both subgroups based on the quality and type of studies. The cohort study subgroup that examined patients in a prone position compared to those who were not prone showed a significantly improved PF ratio (41.70; 95% CI, 13.53 to 69.87; I2, 61%). Similarly, there was a significant increase in the PF ratio following proning in the experimental subgroup that compared the patients’ positions in supine and prone (88.41; 95% CI, 63.95 to 112.86; I2, 83%).
Secondary outcomes
Six studies reported in-hospital mortality. There was a significant difference in the mortality rates of the prone and supine positions (RR, 0.48; 95% CI, 0.35 to 0.67; I2, 2%; Fig. 3).
The prone position demonstrated no significant difference in ICU length of stay compared with the supine position (-2.23; 95% CI, -5.33 to 0.87; I2, 34%; Fig. 4). However, the prone position significantly decreased the mechanical ventilator days (-2.59; 95% CI, -4.21 to -0.97; I, 0%; Fig. 5).
Publication bias
The funnel plot of the PF ratio outcome of the prone and supine position groups was relatively symmetric and showed no publication bias (Fig. 6).
Other effects of prone position
Prone position and hemodynamic change
There were limited data on hemodynamic change. We identified 3 studies designed to examine hemodynamic measurements [17, 18, 21]. In general, pulmonary venous catheter with thermodilution technique was utilized for this purpose. Overall, intrapulmonary shunt (Qs/Qt) showed significant reduction in prone position compared to supine position in all studies (p < 0.05).
In Hernández‑López et al., the reduction of Qs/Qt demonstrated significantly 48 h after prone positioning until the end of measurement at 72 h. Concomitantly to Fridrich et al., Qs/Qt reductions were observed immediately after prone positioning which showed significant change compared to supine position 20 h after the turn. However, this result demonstrated persistently in the first three cycles, while there was no longer improvement after 72 h.
Johannigman et al. demonstrated significant increase of mean pulmonary artery pressure (mPAP) and pulmonary capillary wedge pressure (PCWP) on days 1 through 4 during prone positioning (p < 0.05), while Fridrich et al. reported slow decrease of mPAP and pulmonary vascular resistance (PVR) in the first four days of recording without consistent relation to the turning maneuvers. In addition, cardiac index showed no significant difference between two positions [17, 18].
Three of studies reported cardiac complications (brady-tachy arrhythmias and hemodynamic instability) during prone position [9, 18, 19]. In Voggenreiter 2005 et al., 8 of 19 (42%) patients who underwent prone position reported brady-tachy arrhythmia events, while 2 of 127 (1.54%) in Maillet et al. study reported atrial fibrillation required cardioversion. In Fridrich et al., 6 of 20 (30%) patients were terminated prone positioning due to hemodynamic instability.
Prone position and complications
Most studies reported on minor complications, including facial and neck swelling as well as pressure sores [9,10,11, 15,16,17, 19, 21, 23]. Three studies reported that all patients undergoing prone positioning developed facial or neck edema [10, 16, 17]. However, this complication was a transient event and was reported to be self-limited.
Surgical wound complications after prone positioning ranged from 3–42% [14, 19, 22]. In cardiac surgery, superficial sternal wound infection ranged from 3–13% [19, 22]. In abdominal surgery patients, Gaudry et al., reported 42% of patients with prone position had surgical wound complications: 8.3% with scar dehiscence, 14% with wound necrosis and leakage, and 3% with abdominal compartment syndrome. However, these rates were not significant different between prone and supine position.
In terms of safety, from 16 studies, 1 of 20 (5%) naso-gastric tube displacement [17], 8 of 20 (40%) peripheral intravenous catheter loss [17], 1 of 20 (5%) central venous catheter loss [18] and 1 event of endotracheal tube loss during prone positioning [18].
Discussion
This is the first meta-analysis focusing on the effect of prone position in surgical and trauma patients. Our study demonstrated the significant improvement in P/F ratio after proning. This benefit was shown in both overall and subgroup analysis. Prone position in surgical and trauma patients also significantly decreased mortality and mechanical ventilator days. There was no effect on cardiac index regarding two studies. Despite a low rate of serious complications from prone positioning in our systematic review, minor complications, particularly facial edema, were frequently reported among all studies.
Ventilator-induced lung injury (VILI) associated with barotrauma, volutrauma, atelectrauma, and biotrauma demonstrated largely influenced to mortality on ARDS [24, 25]. Lung-protective mechanical ventilation (MV) strategies have demonstrated improved survival in patients with ARDS over the past decades [26]. However, adjusting mechanical ventilation alone may not successfully improve outcomes, including oxygenation, MV day, ICU length of stay and mortality. Consequently, there are alternative methods proposed to help improve outcomes, including prone positioning [27].
One of the current therapeutic strategies for ARDS is prone positioning (PP), which has been studied in numerous major randomized controlled trials (RCT) to obtain the aforementioned benefits [3,4,5, 28,29,30]. There are, nevertheless, certain restrictions that were deemed to be proning contraindications. It was unclear if we could execute proning in patients with unstable fractures or unstable hemodynamics due to the shift in position. Therefore, the PROSEVA study’s exclusion criteria have often been implemented as a general contraindication, particularly for patients who have just undergone surgery [4]. However, there are a few relative contraindications to prone positioning that should be chosen on an individual basis. These include hemodynamic instability, trauma-related injuries (such as open abdominal wounds, increased intracranial pressure, unstable long bone or pelvic fracture), and late-term pregnancy. The only absolute contraindication to prone positioning is an unstable spinal fracture [31].
In our study, there was significant oxygenation improvement (increased P/F ratio) in patients who underwent PP compared to supine positioning (SP), (mean difference 79.26; 95% CI, 53.38-105.13; 10 studies; n = 624 patients). This outcome is consistent with the prior meta-analysis that comprised ten randomized control trials comparing supine and prone positioning in ARDS patients undergoing mechanical ventilation. They showed that, within the first three days following randomization, the PF ratio increased by 25–36%, indicating that oxygenation improvements were higher in the prone group than in the supine group [32].
Mortality benefit remained controversial among the studies. According to Sud et al., PP during mechanical ventilation decreased mortality among ARDS patients. The number needed to treat to save one life was 11(95% CI 6–50) [32]. One systematic review and meta-analysis included eight RCTs and evaluated the effect of prone positioning on 28-day mortality. It demonstrated a non-significant reduction in mortality in favour of PP; however, a subgroup analysis of patients with ≥ 12 h of PP found a significantly lower mortality in this group [31]. This mortality reduction was most marked among patients with moderate to severe ARDS. In our study, mortality was significantly improved in PP, (RR 0.48, 95% CI, 0.35–0.67; 6 studies, n = 362), although our included studies were heterogeneous in terms of the duration of PP, varying between < 12 h (6 studies) and ≥ 12 h (9 studies).
The PROSEVA study showed a significant reduction in 28 and 90 days on MV (14 ± 9 days and 33 ± 34 days, respectively) [5]. As in PROSEVA trial, our results indicated a significant reduction in MV days days in PP (mean difference − 2.59, 95% CI, -4.21-0.97; 3 studies; n = 165). While ICU LOS in PROSEVA study showed a trend in favour of PP (P = 0.05) ICU LOS, similar to our study demonstrated no significant difference between two groups (mean difference − 2.23, 95% CI, -5.33-0.87; 4 studies, n = 212).
In terms of hemodynamic aspect, Jozwiak et al. demonstrated that the microcirculatory effect of prone position result from three basic mechanisms: an increase in intraabdominal pressure, improvement in arterial oxygenation, and lung recruitment. These three effects can lead to significant increase in cardiac preload, decrease right ventricular afterload, and increase in left ventricular preload. However, cardiac output will increase only in preload reserve patients. While our study did not show increased cardiac output, this result might be explained by the lack of preload assessment data. However, other hemodynamic parameters, especially the decrease of pulmonary vascular resistance and the improvement of intrapulmonary shunt were similarly demonstrated.
Complications from prone positioning must also be noted, particularly since trauma and surgical patients may be at increased risk for morbidity from position changes due to the presence of fractures, surgical incisions, or increased support lines and devices. Adverse events such as facial swelling, loss of venous access, device displacement and pressure sore can occur during transition to and from prone position and during prone positioning itself; however, they can be attenuated with program training. It has been suggested that endotracheal tube obstruction and vasopressor requirement increased with prone position, while the incidence of barotrauma and ventilator-associated pneumonia and unexplained central catheter or endotracheal tube removal were not significant different between groups [33].
In this study, we reported surgical complications that ranged from 3 to 42%, particularly involving abdominal and sternal wound dehiscences related to prone position; however, it was not significantly different compared to supine position. In addition, there were some studies reported the incidence of intraabdominal hypertension or abdominal compartment syndrome in our study. Though prone position can increase intraabdominal pressure, the effect is small. There was no previous reported significant increased intraabdominal pressure resulting in abdominal compartment after prone position [34,35,36]. The possible explanation are the improper location of the cushion with abdominal compression, and the undetected preexisting intraabdominal hypertension.
Although this is the first meta-analysis of a large number of surgical and trauma patients with ARDS and prone positioning, we must acknowledge the limitations of this study. These include clinical and methodologic heterogeneity among included studies. We attempted to correct for some of these differences via subgroup analyses, but the possibility of bias from the data heterogeneity must be considered. Moreover, our study was unable to assess ARDS severity, especially the individual PF ratio. It is restricted to summarizing the impact of PP with respect to their level of severity. Thus, a large multicenter prospective study is warranted.
In summary, prone position can significantly improve the P/F ratio and has a mortality benefit among surgical and trauma patients who developed acute respiratory distress syndrome. It can cause minor complications, such as facial edema. There was no significant difference in local wound complications compared to those with supine position. Prone position may be an effective rescue therapy for surgical and trauma patients.
Data Availability
All data analysed during this study are included in this published article.
References
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–33.
Bellani G, Laffey JG, Pham T, Fan E. The LUNG SAFE study: a presentation of the prevalence of ARDS according to the Berlin definition! Crit Care. 2016;20(1):268.
Gattinoni L, Busana M, Giosa L, Macrì MM, Quintel M. Prone positioning in acute respiratory distress syndrome. Semin Respir Crit Care Med. 2019;40(1):94–100.
Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–68.
Guerin C, Gaillard S, Lemasson S, Ayzac L, Girard R, Beuret P, et al. Effects of systematic prone positioning in hypoxemic acute respiratory failure: a randomized controlled trial. JAMA. 2004;292(19):2379–87.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Voggenreiter G, Aufmkolk M, Stiletto RJ, Baacke MG, Waydhas C, Ose C, et al. Prone positioning improves oxygenation in post-traumatic lung injury–a prospective randomized trial. J Trauma. 2005;59(2):333–41. discussion 41 – 3.
Watanabe I, Fujihara H, Sato K, Honda T, Ohashi S, Endoh H, et al. Beneficial effect of a prone position for patients with hypoxemia after transthoracic esophagectomy. Crit Care Med. 2002;30(8):1799–802.
Akatsuka M, Tatsumi H, Yama N, Masuda Y. Therapeutic evaluation of computed tomography findings for efficacy of prone ventilation in acute respiratory distress syndrome patients with abdominal surgery. J Crit Care Med. 2020;6(1):32–40.
Davis JW, Lemaster DM, Moore EC, Eghbalieh B, Bilello JF, Townsend RN, et al. Prone ventilation in trauma or surgical patients with acute lung injury and adult respiratory distress syndrome: is it beneficial? J Trauma. 2007;62(5):1201–6.
Eremenko AA, Egorov VM, Levikov DI. Results of the treatment of cardiac surgery patients with postoperative acute respiratory distress syndrome by prone-position pulmonary ventilation. Anesteziol Reanimatol. 2000(5):42–5.
Gaudry S, Tuffet S, Lukaszewicz AC, Laplace C, Zucman N, Pocard M, et al. Prone positioning in acute respiratory distress syndrome after abdominal surgery: a multicenter retrospective study : SAPRONADONF (study of Ards and PRONe position after abDOmiNal Surgery in France). Ann Intensive Care. 2017;7(1):21.
Erhard J, Ruchholtz CWS, et al. Einfluû Der Kinetischen Therapie auf den Behandlungsverlauf Bei Patienten Mit Posttraumatischem Lungenversagen. Der Unfallchirurg. 1998;101:928–34.
Voggenreiter G, Neudeck F, Aufmkolk M, Fassbinder J, Hirche H, Obertacke U, et al. Intermittent prone positioning in the treatment of severe and moderate posttraumatic lung injury. Crit Care Med. 1999;27(11):2375–82.
Johannigman JA, Davis K Jr., Miller SL, Campbell RS, Luchette FA, Frame SB, et al. Prone positioning for acute respiratory distress syndrome in the surgical intensive care unit: who, when, and how long? Surgery. 2000;128(4):708–16.
Fridrich P, Krafft P, Hochleuthner H, Mauritz W. The effects of long-term prone positioning in patients with trauma-induced adult respiratory distress syndrome. Anesth Analg. 1996;83(6):1206–11.
Maillet JM, Thierry S, Brodaty D. Prone positioning and acute respiratory distress syndrome after cardiac surgery: a feasibility study. J Cardiothorac Vasc Anesth. 2008;22(3):414–7.
Saha S, Jebran AF, Leistner M, Kutschka I, Niehaus H. Turning things around: the role of prone positioning in the management of acute respiratory failure after cardiac surgery. J Cardiothorac Vasc Anesth. 2020;34(6):1434–8.
Hernández-López GD, Gorordo-Delsol L, Antonio, Hernández-Romero M, et al. Ventilación en posición prono en pacientes postoperados de cirugía abdominal complicados con síndrome de dificultad respiratoria aguda: análisis de una cohorte. Med Crit. 2019;33(5):245–50.
von Wardenburg C, Wenzl M, Dell’Aquila AM, Junger A, Fischlein T, Santarpino G. Prone positioning in cardiac surgery: for many, but not for everyone. Semin Thorac Cardiovasc Surg. 2016;28(2):281–7.
Hale DF, Cannon JW, Batchinsky AI, Cancio LC, Aden JK, White CE, et al. Prone positioning improves oxygenation in adult burn patients with severe acute respiratory distress syndrome. J Trauma Acute Care Surg. 2012;72(6):1634–9.
Tremblay LN, Slutsky AS. Ventilator-induced injury: from barotrauma to biotrauma. Proc Assoc Am Physicians. 1998;110(6):482–8.
Tremblay LN, Slutsky AS. Ventilator-induced lung injury: from the bench to the bedside. Intensive Care Med. 2006;32(1):24–33.
Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–8.
Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):69.
Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Labarta V, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001;345(8):568–73.
Mancebo J, Fernández R, Blanch L, Rialp G, Gordo F, Ferrer M, et al. A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;173(11):1233–9.
Taccone P, Pesenti A, Latini R, Polli F, Vagginelli F, Mietto C, et al. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2009;302(18):1977–84.
Guérin C, Albert RK, Beitler J, Gattinoni L, Jaber S, Marini JJ, et al. Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med. 2020;46(12):2385–96.
Sud S, Friedrich JO, Adhikari NK, Taccone P, Mancebo J, Polli F, et al. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. CMAJ. 2014;186(10):E381–90.
Munshi L, Del Sorbo L, Adhikari NKJ, Hodgson CL, Wunsch H, Meade MO, et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14(Supplement4):280–s8.
Jozwiak M, Teboul JL, Anguel N, Persichini R, Silva S, Chemla D, et al. Beneficial hemodynamic effects of prone positioning in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2013;188:1428–33.
Michelet P, Roch A, Gainnier M, Sainty JM, Auffray JP, Papazian L. Influence of support on intra-abdominal pressure, hepatic kinetics of indocyanine green and extravascular lung water during prone positioning in patients with ARDS: a randomized crossover study. Crit Care. 2005;9:R251–7.
Blanch L, Mancebo J, Perez M, Martinez M, Mas A, Betbese AJ, et al. Short-term effects of prone position in critically ill patients with acute respiratory distress syndrome. Intensive Care Med. 1997;23:1033–9.
Acknowledgements
None.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
Literature search (VP, NO, WO), study design (VP, NO, WO), data collection (VP, NO), data analysis (VP, NO, WO, MS). All authors contributed on data interpretation, writing, and critical revision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Presentation
This study was presented as an ePoster at the Critical Care Canada Forum 2022 Conference in Toronto, ON on November 22–25, 2022.
Implication statement
It is safe to apply prone position as a rescue therapy in trauma or surgical patients who are diagnosed with acute respiratory distress syndrome. Prone position can improve oxygenation without significant major complications.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Phoophiboon, V., Owattanapanich, N., Owattanapanich, W. et al. Effects of prone positioning on ARDS outcomes of trauma and surgical patients: a systematic review and meta-analysis. BMC Pulm Med 23, 504 (2023). https://doi.org/10.1186/s12890-023-02805-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02805-w