Abstract
Background
Cells are an essential part of the triple principles of tissue engineering and a crucial component of the engineered ovary as they can induce angiogenesis, synthesize extracellular matrix and influence follicle development. Here, we hypothesize that by changing the medium supplementation, we can obtain different cell populations isolated from the human ovary to use in the engineered ovary. To this end, we have in vitro cultured cells isolated from the menopausal ovarian cortex using different additives: KnockOut serum replacement (KO), fetal bovine serum (FBS), human serum albumin (HSA), and platelet lysate (PL).
Results
Our results showed that most cells soon after isolation (pre-culture, control) and cells in KO and FBS groups were CD31- CD34- (D0: vs. CD31-CD34+, CD31 + CD34+, and CD31 + CD34- p < 0.0001; KO: vs. CD31-CD34+, CD31 + CD34+, and CD31 + CD34- p < 0.0001; FBS: vs. CD31-CD34+ and CD31 + CD34+ p < 0.001, and vs. CD31 + CD34- p < 0.01). Moreover, a deeper analysis of the CD31-CD34- population demonstrated a significant augmentation (more than 86%) of the CD73+ and CD90+ cells (possibly fibroblasts, mesenchymal stem cells, or pericytes) in KO- and FBS-based media compared to the control (around 16%; p < 0.001). Still, in the CD31-CD34- population, we found a higher proportion (60%) of CD90+ and PDPN+ cells (fibroblast-like cells) compared to the control (around 7%; vs PL and KO p < 0.01 and vs FBS p < 0.001). Additionally, around 70% of cells in KO- and FBS-based media were positive for CD105 and CD146, which may indicate an increase in the number of pericytes in these media compared to a low percentage (4%) in the control group (vs KO and FBS p < 0.001). On the other hand, we remarked a significant decrease of CD31- CD34+ cells after in vitro culture using all different medium additives (HSA vs D0 p < 0.001, PL, KO, and FBS vs D0 P < 0.01). We also observed a significant increase in epithelial cells (CD326+) when the medium was supplemented with KO (vs D0 p < 0.05). Interestingly, HSA and PL showed more lymphatic endothelial cells compared to other groups (CD31 + CD34+: HSA and PL vs KO and FBS p < 0.05; CD31 + CD34 + CD90 + PDPN+: HSA and PL vs D0 p < 0.01).
Conclusion
Our results demonstrate that medium additives can influence the cell populations, which serve as building blocks for the engineered tissue. Therefore, according to the final application, different media can be used in vitro to favor different cell types, which will be incorporated into a functional matrix.
Similar content being viewed by others
Background
The ovaries are female reproductive organs that contain four layers, including the germinal epithelium layer, the collagenous connective tissue, the cortex holding preantral follicles, and the medulla comprising loose connective tissue, blood vessels, and antral follicles. Follicles are the main components of the ovary containing oocytes and granulosa cells [1]. Females are born with a limited number of oocytes (around 1–2 million), which are placed in primordial follicles [2]. Menopause begins when the woman’s follicular reserve is depleted, and she is no longer able to conceive naturally [3]. On the other hand, studies reported that both pre- and post-menopausal ovaries contain pluripotent/multipotent stem cells that may differentiate into multiple cell lineages [4,5,6]. Stimpfel et al. [4] investigated the adipogenic, osteogenic, neural, and pancreatic differentiation ability of stem cells derived from pre- and post-menopausal ovaries and demonstrated the high plasticity of the stem cells isolated from these ovaries. Somatic stem cells are a subgroup of normal tissues with self-renewal ability and the potential to create lineage-committed daughter cells, which are important for tissue regeneration and repair [7]. On the other hand, the culture of stem cells in different media (for instance, supplemented media with fetal calf serum, human serum, or platelet lysate) could affect their proliferation rate, function, and phenotype [8].
Fan et al. [9] and Wagner et al. [10] provided a map of isolated cells from reproductive-age ovaries and identified six groups of cells, including endothelial, immune, granulosa, smooth muscle, theca, and stroma cells. In tissue engineering, cells play a critical role in the constructed tissue. For instance, endothelial cells could accelerate vascularization, stem cells could improve regeneration, or theca cells are necessary for follicle development [1, 11,12,13]. Therefore, it is essential to identify various cell types in a tissue and their fate after culturing in different media to optimize the design of an engineered tissue. In this study, we characterize isolated cells from menopausal ovarian cortex before and after in vitro culture using four different supplements: fetal bovine serum (FBS), human serum albumin (HSA), platelet lysate (PL), and KnockOut serum replacement (KO).
Methods
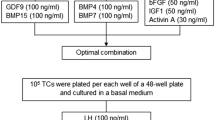
Ovarian stromal cell isolation
The ovarian tissue biopsies were collected from post-menopausal women (51–68 years old) and transferred to the laboratory in Dulbecco’s phosphate-buffered saline (DPBS; 14,190,144; Gibco). The ovarian cortical fragments were frozen using our standard method after the medullar section was removed [14]. After thawing of the ovarian samples, stromal cells were isolated following our published protocols [12, 15,16,17]. Briefly, a tissue chopper (Mickel Laboratory, the UK) set to 0.5 mm was utilized for the mechanical mincing of tissues, and then the enzymatic digestion of chopped tissues was performed by Liberase DH (05401054001; Sigma-Aldrich, Germany) and DNAse I (10,104,159,001; Sigma-Aldrich) at 37 °C for 75 minutes. Then, DPBS supplemented with 10% heat-inactivated fetal bovine serum (FBS; 16,140–071; Gibco, Belgium) was added to the digested tissue suspension to inactivate enzymatic reactions. The suspension was then centrifuged (500 g, 10 min) after filtering through 80 (NY8002500; Millipore, Belgium) and 30 μm (NY3002500; Millipore) nylon net filters. After cell counting, the cells were divided into 5 groups: cells for freezing (D0) and in vitro culture using FBS, HSA (Cliniques Universitaires Saint Luc, Belgium), PL (SER-HPL-GROPRO, Zenbio, USA), and KO (10,828,028; Gibco, Belgium).
Cell culture
Each cell culture medium consisted of Dulbecco’s modified Eagle’s medium F-12 nutrient mixture (DMEM/F12; 21,041–025; Gibco), 1% antibiotic and antimycotic (Anti-Anti; A5955; Gibco), and 10% FBS, HSA, PL, or KO. The cells were in vitro cultured at 37 °C in a humidified incubator with 5% CO2 and the medium was replaced every other day. After 16 days, the cells were detached using Accutase (A6964; Sigma-Aldrich) to perform multiparametric flow cytometry analysis. Furthermore, the light microscopy analysis on cell morphology and proliferation on days 5, 7, 9, and 15 was performed.
Flow cytometry
Human ovarian isolated and cultured cells were processed for flow cytometry according to the Feisst et al. [18] procedure to determine the cell populations. Before staining, the frozen-thawed cells were washed and incubated in FBS culture medium at 37 °C, 5% CO2 for 1 h. After washing with DPBS, frozen-thawed and cultured cells were stained with the following antibodies (Table 1): CD326 (324,233; BioLegend, the Netherlands), CD34 (343,615; BioLegend), CD31 (303,131; BioLegend), CD90 (328,113; BioLegend), CD73 (344,007; BioLegend), podoplanin (PDPN, 337005; BioLegend), CD146 (361,021; BioLegend), and CD105 (323,205; BioLegend) and dark-incubated at room temperature for 10 min.
At least 10,000 events were analyzed by BD FACSCanto™ II Clinical Flow Cytometry System (BD Biosciences, Belgium). FlowJo software (BD Biosciences, USA) was used for data analysis.
Statistical analysis
One-way ANOVA was used to examine the data and statistical significance was determined by P values less than 0.05. The quantitative data were presented as mean ± SD and a single sample standard deviation is represented by the error bars in graphs.
Results and discussion
Flow cytometry
In order to investigate the identity of ovarian stromal cells after isolation (D0) and culture in different media supplemented by HSA, FBS, PL, and KO, the cells were stained with 8 cell markers. These supplements are different from each other and their composition can therefore trigger different cell behaviors. FBS is an undefined serum, and its composition varies from lot to lot and depends on the diet and environment of a pregnant female. Indeed, Zheng et al. [19] investigated the growth of adult retinal pigment epithelial cells in three different FBS batches and reported that the growth rate of cells was significantly higher in one of the batches compared to others. While it is not possible to establish the exact composition of FBS, some of its contents have already been described in the literature, such as different types of hormones (follicle-stimulating hormone, glucagon, insulin, and thyroid hormones), growth factors and cytokines (basic fibroblast growth factor, endothelial cell growth factor, epidermal growth factor, and fibroblast growth factor) and other proteins (albumin, fibronectin, laminin, and transferrin) [20]. To reduce uncontrolled cell differentiation and avoid endotoxin and large variability observed in the FBS, this supplement has been replaced by other additives, such as serum-free medium, animal-free components, such as PL, and more defined serum replacement such as KO [21,22,23].
Studies have shown that undesired differentiation of cells cultured in a medium supplemented with KO is lower than FBS [24, 25]. KO is composed of well-defined growth factors, amino acids, vitamins, antioxidants, trace elements, and proteins, including transferrin (iron-saturated), insulin, and lipid-rich albumin (AlbuMAX) [26]. Nevertheless, it is important to bear in mind that the exact composition of KO is not provided by its supplier. Moreover, KO is not the completely free of animal components because of the presence of AlbuMAX [27] and embryo extracts [28]. Albumin is an important protein with antioxidant function as well as a role in binding and carrying biological important factors for cells. Moreover, surfaces coated with albumin cause non-adhesive surfaces, preventing cell attachment [29, 30]. Although HSA has been employed in cell culture, such as human endothelial cells, in which HSA acted as an apoptotic inhibitor [31], studies from human islet and embryo culture in FBS or FBS + HSA indicated superior results than HSA alone regarding oxygen consumption rate per DNA content or blastocyst implantation rate [32, 33]. A more recent alternative to FBS is PL, an animal-free product, produced from human platelets, which are lysed several freezing and thawing cycles. PL contains HSA as a major protein component as well as different types of growth factors, such as fibroblast growth factor (FGF), endothelial growth factor (EGF), platelet-derived growth factors (PDGF), vascular endothelial growth factor (VEGF), transforming growth factor (TGF), insulin-like growth factor-1 (IGF-1), brain-derived neurotrophic factor (BDNF), and epidermal growth factor (EGF) originated from human plasma and platelet components [34, 35]. However, PL is also a donor-related product, and a decrease in the concentration of PDGF, TGF, FGF, or IGF with an increase in donor age has been shown [36]. Therefore, in order to decrease batch variation, PL is generally produced from multiple donors. Based on such differences in these supplement (HSA, FBS, PL, and KO) compositions, it is indeed expected that they can regulate cell behavior differently. For instance, mesenchymal stem cells proliferate faster in medium supplemented with PL than with FBS [37].
In vitro culture in medium supplemented with KO medium yielded a significantly higher proportion of CD326+ cells (epithelial-like cells) compared to D0 (25.19 ± 22.7% vs. 0.72 ± 0.38%; p < 0.05) (Fig. 1). On the other hand, other medium additives had no significant differences in the CD326+ population.
CD326- cells were further analyzed for the CD31 and CD34 (CD31-CD34+, CD31 + CD34+, CD31 + CD34-, and CD31-CD34-). Although CD31-CD34- cells in PL samples had no significant difference from other groups, other samples, except PL, indicated significant differences between CD31-CD34- and CD31-CD34+, CD31 + CD34+, and CD31 + CD34- (D0: vs. CD31-CD34+, CD31 + CD34+, and CD31 + CD34- p < 0.0001; KO: vs. CD31-CD34+, CD31 + CD34+, and CD31 + CD34- p < 0.0001; FBS: vs. CD31-CD34+ and CD31 + CD34+ p < 0.001, and vs. CD31 + CD34- p < 0.01). For HSA, CD31-CD34- had only a significant difference with CD31-CD34+ (p < 0.05) (Fig. 2).
Representative dot plots from the investigation of CD31 and CD34 stained cells in D0 (a), or cultured in HSA (b), PL (c), KO (d), and FBS (e). A graph represents the mean ± SD of main gates (CD31-CD34+, CD31 + CD34+, CD31 + CD34-, and CD31-CD34-) (f); black asterisks represent significant differences between main gates of each sample; blue, red, green, and purple asterisks represent significant differences between CD31-CD34+, CD31 + CD34+, CD31 + CD34-, and CD31-CD34- gates of all samples, respectively; n ≥ 3, mean ± SD; *p < 0.05; **p < 0.01; ***p < 0.001
The CD31-CD34- cells could be fibroblast or mesenchymal stem cells (MSCs). For further investigations, the expression of CD73, CD90, PDPN, CD146 and CD105 was assessed (Figs. 3, 4, and 5). Each sample had more than 5% cells in main gates (CD31-CD34+, CD31 + CD34+, CD31 + CD34-, and CD31-CD34-) considered for this analysis. One of the criteria for identifying MSCs is CD34-, CD73+, CD90+, and CD105+ [38]. Although fibroblasts express CD73, CD90, and CD105, as well [39], the PDPN could be another marker for stromal fibroblasts to be distinguished from MSCs [40, 41]. In addition, endothelial cells could be determined by the expression of CD31 and the perivascular marker CD146 [42].
Looking at CD31-CD34- cells, CD90 and CD73 gates (Fig. 3) reveals that the cells after culturing in different media significantly increased in CD90+ and CD73+ quantities (in HSA, PL, KO, and FBS were 35.38 ± 21.23%, 92.6 ± 3.19%, 86.45 ± 8.26%, and 99.40 ± 0.24% respectively) compared to D0 (16.31 ± 6.51%, vs. HSA, PL, KO, and FBS; p < 0.001). Regarding the majority of cell population in KO and FBS samples are in CD31-CD34- gate and, also, around 86% and 99% cells of CD31-CD34- gate in KO and FBS are CD90+ and CD73+, respectively, major cell types in KO and FBS supplemented samples could be characterized as MSCs, fibroblast, or pericytes, which are CD34-, CD73+, and CD90 + .
Furthermore, cell populations of CD31-CD34-CD90 + PDPN+ rose after culturing in PL (65.77 ± 23.36%; vs. D0; p < 0.01), KO (59.95 ± 22.18%; vs. D0; p < 0.01), and FBS (63.45 ± 13.39%; vs. D0; p < 0.001) (Fig. 4). The results show that around 60% of CD31-CD34- in PL, KO, and FBS could have fibroblast-like phenotype cells, which was around 7% on D0. The cells cultured in HSA had no significant difference with D0 in the number of CD31-CD34- gates cells expressing CD90 and PDPN. Besides, FBS, KO, and PL demonstrated decreasing cell percentage in CD31-CD34- identified CD90-CD73-, CD90-PDPN-, and CD105-CD146- compared to HSA and D0 samples (Figs. 3, 4, and 5).
A surge was also observed in the CD31-CD34- CD105 + CD146+ after culturing cells in different media from 4.13 ± 2.86% on D0 to 46.07 ± 28.03% in PL (vs. D0; p < 0.05), 73.23 ± 10.16% in KO (vs. D0; p < 0.001), and 74.68 ± 11.14% in FBS (vs. D0; p < 0.001) (Fig. 5). On the other hand, HSA had no significant difference in cell population characterized CD31-CD34-CD105+ CD146+ compared to D0.
While pericytes and MSCs express CD44, CD90, CD73, and CD105 [43] markers and pericytes and bone marrow-derived MSCs are CD146+ and CD34- [44, 45], as regards the cells in this experiment isolated from the ovarian cortex, not bone tissue, the CD31-CD34-CD105 + CD146+ could indicate pericytes (perivascular cells). These are fibroblast-like cells and around endothelial cells found in the endothelium basement [46, 47]. Therefore, the results could demonstrate that although a small number of pericytes characterized D0 samples, they could proliferate and increase their number, especially in KO- and FBS-supplemented media. On the other hand, cells in D0 and HSA were characterized by a higher number of cells in CD31-CD34-CD105-CD146- compared to KO and FBS (D0 vs. KO; p < 0.05, vs. FBS; p < 0.01, HSA vs. FBS; p < 0.05) (Fig. 5).
As CD34 is a marker of progenitor cells [48,49,50,51] and endothelial cells [52], CD31-CD34+ could be progenitor cells and CD31 + CD34+ could represent endothelial progenitor cells. Although cells cultured in different media showed no significant differences between cell populations in CD31-CD34+ and CD31 + CD34+ gates, these two gates on D0 had a significant difference in cell populations (p < 0.05; 26.75 ± 8.6% and 12.87 ± 7.34%, respectively) (Fig. 2). This may indicate differentiation of cells in CD31-CD34+ gate to other cell types when cells cultured in different media, which the average cell population in CD31-CD34+ gate decrease to 6.07 ± 7.34% in HSA (vs. D0; p < 0.001), 2.99 ± 2.92% in PL (vs. D0; p < 0.01), 4.85 ± 3.63% in KO (vs. D0; p < 0.01), and 6.1 ± 4.84% in FBS (vs. D0; p < 0.01) (Fig. 2). Moreover, HSA compared to KO and FBS in CD31 + CD34+ gate (p < 0.05) and PL compared to D0 in CD31 + CD34- gate (p < 0.05) had a higher cell number (Fig. 2), demonstrating differentiation of cells to the endothelial cells (CD31 + CD34-) in PL or endothelial progenitor cells (CD31 + CD34+) in HSA-based media.
The further evaluation of the cell population in CD31-CD34+ gates stained by extra antibodies (CD90 and CD73, CD90 and PDPN, and CD105 and CD146) reveals that considering the expression of CD90 and CD73 on D0, the majority of cells could be divided into two groups (Fig. 6): CD31-CD34 + CD90-CD73+ and CD31-CD34 + CD90 + CD73+ (45.33 ± 17.5% and 45.82 ± 14.82%, respectively). The further analysis of the CD31-CD34+ gate was not considered for HSA, PL, KO, and FBS, which had cell populations of less than 5%. As hematopoietic stem cells express CD34 and CD90 [53], around 45% of cells in the CD31-CD34+ gate could be identified as hematopoietic stem cells in D0 samples. Moreover, considering CD31-CD34 + CD90PDPN and CD31-CD34 + CD105CD146 gates on D0, the majority of cell populations belonged to CD31-CD34 + CD90-PDPN+ (42.55 ± 19.87%) and CD31-CD34 + CD105-CD146- (90.33 ± 4.22%) (Fig. 6). Ho et al. [54] demonstrated that maturate fibroblasts has a profile of CD34 + CD90-, so we can consider the CD31-CD34 + CD90-PDPN+ cells as maturate fibroblasts existing in the ovarian cortex.
Since CD31 + CD34+ gate of FBS and KO had a cell population of less than 5%, this gate was not considered for more evaluation in these media. Cells in culture in HSA- and PL-based media indicated increasing in CD31 + CD34 + CD90 + CD73+ cell populations (81.33 ± 12.57% and 98.12 ± 0.75%, respectively) compared to D0 (52.15 ± 20.52%; vs. HSA and vs. PL; p < 0.01) (Fig. 7). Moreover, when HSA or PL was used as media additives, most cell phenotypes changed from 35.75 ± 11.12% CD31 + CD34 + CD90 + PDPN- and 37.87 ± 20.17% CD31 + CD34 + CD90-PDPN- in D0 to 74.33 ± 19.59% and 97.4 ± 1.27% CD31 + CD34 + CD90 + PDPN+ in HSA and PL, respectively. Therefore, the main population of cells in CD31 + CD34+ changed their phenotype from PDPN- on D0 to the PDPN+ cells when cultured in HSA and PL. Considering that lymphatic endothelial cells are CD31 + CD34 + CD90 + PDPN+ [55, 56], around 74 and 97% of cells in the CD31 + CD34+ gate may be recognized as lymphatic endothelial cells in HSA and PL, respectively (vs D0 p < 0.01).
Furthermore, the phenotype change was observed in CD31 + CD34 + CD105CD146, which after culturing cells in media containing HSA and PL, the cell populations in CD31 + CD34+ CD105 + CD146+ reached 83.17 ± 25.65% and 93.6 ± 6.85% in HSA and PL, respectively, from 24.52 ± 14.56% in D0 (vs. HSA and PL; p < 0.001). On the other hand, CD31 + CD34+ CD105-CD146- cell populations were significantly decreased in HSA and PL (2.8 ± 4.77%; vs. D0; p < 0.01 and 0.10 ± 0.14% vs. D0; p < 0.05, respectively) in comparison to D0 (41.33 ± 12.17%). This surge of CD31 + CD34+ CD105+ CD146+ cells in PL and HSA showed the ability of these additives to increase the number of endothelial cells expressing CD31, CD34, CD105, and CD146.
CD31 + CD34- gates of samples, except D0, were also checked for other antibodies (Fig. 8). The results showed that the majority of cells in all culture conditions characterized as CD31 + CD34-CD90 + CD73+ (in HSA, PL, KO, and FBS were 75.28 ± 14.48%, 99.53 ± 0.19%, 92.53 ± 9.28%, and 96.58 ± 5.93%, respectively), CD31 + CD34-CD90 + PDPN+ (in HSA, PL, KO, and FBS were 69.27 ± 20.52, 99.27 ± 0.26%, 91.55 ± 8.94%, and 92.73 ± 7.47%, respectively), and CD31 + CD34-CD105 + CD146+ (in HSA, PL, KO, and FBS were 75.07 ± 20.24%, 85.13 ± 15.74%, 96.73 ± 3.13%, and 93.73 ± 6.98%, respectively) (Fig. 8). These results demonstrate that the most cell population of CD31 + CD34- in the different media could be endothelial cells, which may be positive for CD31, CD90, CD73, CD105, and CD146. However, blood vessel endothelial cells are PDPN- and lymphatic endothelial cells are PDPN+ [55]. Since more than 90% of cells in the CD31 + CD34- gate of PL, KO, and FBS are CD90 + PDPN+, the cells of these media in the CD31 + CD34- gate could demonstrate lymphatic endothelial-type cells. On the other hand, Gafaar et al. [57] compared endothelial cells derived from umbilical cord blood and differentiated endothelial cells from human adipose mesenchymal stem cells. They reported that the cell from the umbilical cord blood are CD31 + CD144 + CD146 + CD34 + CD73 + CD105 + CD90-CD45- whereas the differentiated endothelial cells are CD90 + CD73 + CD105 + CD34 + CD31+. Therefore, it seems that the CD31 + CD34- gate are differentiated endothelial cells which are positive for CD90, CD73, CD105, and CD31. As D0 had a negligible cells in CD31 + CD34-gate (2.84 ± 2.82%) this theory that these cells in other media’s CD31 + CD34- gate could be differentiated ones may be reinforced.
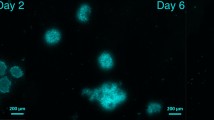
Light microscopy analysis of cells in different media
Images of the cells cultured in different media were taken during in vitro culture on days 5, 7, 9, and 15 by using a light microscope (Fig. 9). The microscopy analysis of cells indicated that while the seeding density was similar in all groups at day 0, the population of the cells revealed slight differences among the groups after 3 days of in vitro culture. Cells in PL showed the highest confluence, and those in KO, the lowest. However, when comparing cell growth from day 3 to day 5, 9, and 15, both PL and FBS groups displayed a marked increase in cell number over time with 100% confluence at day 15, while the cell number in the KO and HSA groups showed no notable increase in cells from day 5 to day 15. These differences between the various conditions indicate the potential presence of different cell types when culturing stromal cells by using various supplements.
The cells displayed high adhesion to the flask surface when media supplemented with FBS and PL, and low adhesion when media supplemented with HSA and KO. Cells within all four groups grew in a monolayer and had an elongated, bi- or multipolar cell type, similar to fibroblasts. Within this monolayer, various sizes of cells can be seen, especially in the PL, FBS, and KO-supplemented media. A difference in the HSA group relative to the other groups is the round cells, similar to lymphoblasts. These dissimilarities within the same condition indicate the possibility of more than one cell type in each supplemented medium (Fig. 9).
Conclusion
In conclusion, our findings show that isolated cells from the ovarian cortex have distinct characterization when cultured in media supplemented with HSA, PL, KO, or FBS. Furthermore, the cells were identified by different phenotypes when they were cultured in media using one of these four additives. Most cells in KO and FBS expressed CD31-CD34-CD73 + CD90+, indicating the possibility of cells being fibroblasts, mesenchymal stem cells, or pericytes in these media. Also, the cells in KO medium indicated a significant increase in cells expressed CD326+ (epithelial cells). PL and HSA groups contained more CD31 + CD34 + CD90 + PDPN+, lymphatic cells compared to the other group as well as PL demonstrated a significant increase in the CD31 + CD34-, endothelial cells compared to day 0.
While this initial study offers a novel strategy to obtain different cell populations for the bioengineered ovary, further studies, such as single-cell RNA-sequencing, would be instrumental in precisely identifying the different cell populations before and after in vitro culture. Identifying cells before their use for regenerative medicine is crucial as different cell types secret different growth factors and cytokines that can direct the fate of engineered tissue and the formation of extracellular matrix.
Availability of data and materials
Contact the authors for data requests.
Abbreviations
- DMEM/F12 :
-
Dulbecco’s modified Eagle’s medium F-12 nutrient mixture
- DPBS :
-
Dulbecco’s phosphate-buffered saline
- FBS :
-
Fetal bovine serum
- HSA :
-
Human serum albumin
- KO :
-
KnockOut serum replacement
- PL :
-
Platelet lysate
References
Dadashzadeh A, Moghassemi S, Shavandi A, Amorim CA. A review on biomaterials for ovarian tissue engineering. Acta Biomater. 2021;135:48-63.
Lliberos C, Liew SH, Zareie P, La Gruta NL, Mansell A, Hutt K. Evaluation of inflammation and follicle depletion during ovarian ageing in mice. Sci Rep. 2021;11(1):1–15.
Richardson SJ, Nelson JF. Follicular depletion during the menopausal transition. Ann N Y Acad Sci. 1990;592(1):13–20.
Stimpfel M, Skutella T, Cvjeticanin B, Meznaric M, Dovc P, Novakovic S, et al. Isolation, characterization and differentiation of cells expressing pluripotent/multipotent markers from adult human ovaries. Cell Tissue Res. 2013;354(2):593–607.
Parte S, Bhartiya D, Telang J, Daithankar V, Salvi V, Zaveri K, et al. Detection, characterization, and spontaneous differentiation in vitro of very small embryonic-like putative stem cells in adult mammalian ovary. Stem Cells Dev. 2011;20(8):1451–64.
Virant-Klun I, Zech N, Rožman P, Vogler A, Cvjetičanin B, Klemenc P, et al. Putative stem cells with an embryonic character isolated from the ovarian surface epithelium of women with no naturally present follicles and oocytes. Differentiation. 2008;76(8):843–56.
Szotek PP, Chang HL, Brennand K, Fujino A, Pieretti-Vanmarcke R, Celso CL, et al. Normal ovarian surface epithelial label-retaining cells exhibit stem/progenitor cell characteristics. Proc Natl Acad Sci. 2008;105(34):12469–73.
Kirsch M, Rach J, Handke W, Seltsam A, Pepelanova I, Strauß S, et al. Comparative analysis of mesenchymal stem cell cultivation in fetal calf serum, human serum, and platelet lysate in 2D and 3D systems. Front Bioeng Biotechnol. 2021;8:598389.
Fan X, Bialecka M, Moustakas I, Lam E, Torrens-Juaneda V, Borggreven N, et al. Single-cell reconstruction of follicular remodeling in the human adult ovary. Nat Commun. 2019;10(1):1–13.
Wagner M, Yoshihara M, Douagi I, Damdimopoulos A, Panula S, Petropoulos S, et al. Single-cell analysis of human ovarian cortex identifies distinct cell populations but no oogonial stem cells. Nat Commun. 2020;11(1):1–15.
Heath CA. Cells for tissue engineering. Trends Biotechnol. 2000;18(1):17–9.
Asiabi P, Dolmans M-M, Ambroise J, Camboni A, Amorim C. In vitro differentiation of theca cells from ovarian cells isolated from postmenopausal women. Hum Reprod. 2020;35(12):2793–807.
Soares M, Sahrari K, Chiti MC, Amorim C, Ambroise J, Donnez J, et al. The best source of isolated stromal cells for the artificial ovary: medulla or cortex, cryopreserved or fresh? Hum Reprod. 2015;30(7):1589–98.
Gallardo M, Paulini F, Corral A, Balcerzyk M, Lucci CM, Ambroise J, et al. Evaluation of a new freezing protocol containing 20% dimethyl sulphoxide concentration to cryopreserve human ovarian tissue. Reprod BioMed Online. 2018;37(6):653–65.
Dadashzadeh A, Moghassemi S, Amorim C. Evaluation of PEGylated fibrin as a three-dimensional biodegradable scaffold for ovarian tissue engineering. Mater Today Chem. 2021;22:100626.
Jafari H, Dadashzadeh A, Moghassemi S, Zahedi P, Amorim CA, Shavandi A. Ovarian cell encapsulation in an enzymatically Crosslinked silk-based hydrogel with tunable mechanical properties. Gels. 2021;7(3):138.
Moghassemi S, Dadashzadeh A, de Souza PEN, Azevedo RB, Amorim CA. AlPc/ZnPc-based oncological photodynamic therapy for a selective eradication of leukemic cells from ovarian tissue. Photodiagn Photodyn Ther. 2021;36:102555.
Feisst V, Brooks AE, Chen C-JJ, Dunbar PR. Characterization of mesenchymal progenitor cell populations directly derived from human dermis. Stem Cells Dev. 2014;23(6):631–42.
Zheng X, Baker H, Hancock WS, Fawaz F, McCaman M, Pungor E Jr. Proteomic analysis for the assessment of different lots of fetal bovine serum as a raw material for cell culture. Part IV. Application of proteomics to the manufacture of biological drugs. Biotechnol Prog. 2006;22(5):1294–300.
Lee DY, Lee SY, Yun SH, Jeong JW, Kim JH, Kim HW, et al. Review of the current research on fetal bovine serum and the development of cultured meat. Food Sci Anim Resour. 2022;42(5):775–99.
Van Der Valk J, Bieback K, Buta C, Cochrane B, Dirks W, Fu J, et al. Fetal bovine serum (FBS): past–present–future. Altex. 2018;35(1):1–20.
Zhang S, Liu Z, Su G, Wu H. Comparative analysis of KnockOut™ serum with fetal bovine serum for the in vitro long-term culture of human Limbal epithelial cells. J Ophthalmol. 2016;2016:7304812.
Tuschong L, Soenen SL, Blaese RM, Candotti F, Muul LM. Immune response to fetal calf serum by two adenosine deaminase-deficient patients after T cell gene therapy. Hum Gene Ther. 2002;13(13):1605–10.
Koivisto H, Hyvärinen M, Strömberg A-M, Inzunza J, Matilainen E, Mikkola M, et al. Cultures of human embryonic stem cells: serum replacement medium or serum-containing media and the effect of basic fibroblast growth factor. Reprod BioMed Online. 2004;9(3):330–7.
Inzunza J, Gertow K, Strömberg MA, Matilainen E, Blennow E, Skottman H, et al. Derivation of human embryonic stem cell lines in serum replacement medium using postnatal human fibroblasts as feeder cells. Stem Cells. 2005;23(4):544–9.
Jin JX, Lee S, Setyawan EMN, Taweechaipaisankul A, Kim GA, Han HJ, et al. A potential role of knockout serum replacement as a porcine follicular fluid substitute for in vitro maturation: lipid metabolism approach. J Cell Physiol. 2018;233(9):6984–95.
Ji J, Zhong B, Bhatia M. Genetic approaches in human embryonic stem cells and their derivatives. In: Atala A, Lanza R, Thomson JA, Nerem RM, editors. Principles of Regenerative Medicine. Cambridge, UK: Academic Press; 2008. p. 190–209.
Xu C, Carpenter MK. Chapter 30 - Feeder-Free Culture. In: Lanza R, Atala A, editors. Handbook of stem cells (second edition). San Diego: Academic Press; 2013. p. 365–73.
Yamazoe H, Uemura T, Tanabe T. Facile cell patterning on an albumin-coated surface. Langmuir. 2008;24(16):8402–4.
Yamazoe H, Tanabe T. Preparation of water-insoluble albumin film possessing nonadherent surface for cells and ligand binding ability. J Biomed Mater Res A. 2008;86(1):228–34.
Zoellner H, Hofler M, Beckmann R, Hufnagl P, Vanyek E, Bielek E, et al. Serum albumin is a specific inhibitor of apoptosis in human endothelial cells. J Cell Sci. 1996;109(10):2571–80.
Avgoustiniatos ES, Scott WE III, Suszynski TM, Schuurman H-J, Nelson RA, Rozak PR, et al. Supplements in human islet culture: human serum albumin is inferior to fetal bovine serum. Cell Transplant. 2012;21(12):2805–14.
Meintjes M, Chantilis SJ, Ward DC, Douglas JD, Rodriguez AJ, Guerami AR, et al. A randomized controlled study of human serum albumin and serum substitute supplement as protein supplements for IVF culture and the effect on live birth rates. Hum Reprod. 2009;24(4):782–9.
Cheng N-C, Tu Y-K, Lee N-H, Young T-H. Influence of human platelet lysate on extracellular matrix deposition and cellular characteristics in adipose-derived stem cell sheets. Front Cell Dev Biol. 2020;8:558354.
Burnouf T, Strunk D, Koh MB, Schallmoser K. Human platelet lysate: replacing fetal bovine serum as a gold standard for human cell propagation? Biomaterials. 2016;76:371–87.
Radtke S, Giebel B, Wagner W, Horn P. Platelet lysates and their role in cell therapy. ISBT Sci Ser. 2014;9(1):193–7.
Vogel JP, Szalay K, Geiger F, Kramer M, Richter W, Kasten P. Platelet-rich plasma improves expansion of human mesenchymal stem cells and retains differentiation capacity and in vivo bone formation in calcium phosphate ceramics. Platelets. 2006;17(7):462–9.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. Int Soc Cell Ther Position Statement Cytotherapy. 2006;8(4):315–7.
Lupatov AY, Vdovin A, Vakhrushev I, Poltavtseva R, Yarygin K. Comparative analysis of the expression of surface markers on fibroblasts and fibroblast-like cells isolated from different human tissues. Bull Exp Biol Med. 2015;158(4):537–43.
Hirayama K, Kono H, Nakata Y, Akazawa Y, Wakana H, Fukushima H, et al. Expression of podoplanin in stromal fibroblasts plays a pivotal role in the prognosis of patients with pancreatic cancer. Surg Today. 2018;48(1):110–8.
Aggoune D, Sorel N, Bonnet M-L, Goujon J-M, Tarte K, Hérault O, et al. Bone marrow mesenchymal stromal cell (MSC) gene profiling in chronic myeloid leukemia (CML) patients at diagnosis and in deep molecular response induced by tyrosine kinase inhibitors (TKIs). Leuk Res. 2017;60:94–102.
Li Q, Yu Y, Bischoff J, Mulliken JB, Olsen BR. Differential expression of CD146 in tissues and endothelial cells derived from infantile haemangioma and normal human skin. J Pathol. 2003;201(2):296–302.
Geevarghese A, Herman IM. Pericyte-endothelial crosstalk: implications and opportunities for advanced cellular therapies. Transl Res. 2014;163(4):296–306.
Baker N, Boyette LB, Tuan RS. Characterization of bone marrow-derived mesenchymal stem cells in aging. Bone. 2015;70:37–47.
Hörl S, Ejaz A, Ernst S, Mattesich M, Kaiser A, Jenewein B, et al. CD146 (MCAM) in human cs-DLK1−/cs-CD34+ adipose stromal/progenitor cells. Stem Cell Res. 2017;22:1–12.
Herndon J, Tome M, Davis T. Development and maintenance of the blood–brain barrier. In: Caplan LR, Biller J, Leary M, Lo E, Thomas A, Yenari M, Zhang J, editors. Primer on Cerebrovascular Diseases. Cambridge, UK: Academic Press; 2017. p. 51–6.
DeLisser H. Adhesion, cell-cell | Vascular. In: Laurent G, Shapiro S, editors. Encyclopedia of respiratory medicine. Cambridge, UK: Academic Press; 2006. p. 29–37.
Armitage S, Hargreaves R, Samson D, Brennan M, Kanfer E, Navarrete C. CD34 counts to predict the adequate collection of peripheral blood progenitor cells. Bone Marrow Transplant. 1997;20(7):587–91.
Jankowski RJ, Deasy BM, Cao B, Gates C, Huard J. The role of CD34 expression and cellular fusion in the regeneration capacity of myogenic progenitor cells. J Cell Sci. 2002;115(22):4361–74.
Henschler R, Brugger W, Luft T, Frey T, Mertelsmann R, Kanz L. Maintenance of transplantation potential in ex vivo expanded CD34 (+)-selected human peripheral blood progenitor cells; 1994.
Krause DS, Ito T, Fackler MJ, Smith OM, Collector MI, Sharkis SJ, et al. Characterization of murine CD34, a marker for hematopoietic progenitor and stem cells; 1994.
Lin G, Finger E, Gutierrez-Ramos JC. Expression of CD34 in endothelial cells, hematopoietic progenitors and nervous cells in fetal and adult mouse tissues. Eur J Immunol. 1995;25(6):1508–16.
Papa L, Djedaini M, Martin TC, Zangui M, Beaumont KG, Sebra R, et al. Limited mitochondrial activity coupled with strong expression of CD34, CD90 and EPCR determines the functional fitness of ex vivo expanded human hematopoietic stem cells. Front Cell Dev Biol. 2020;8:592348.
Ho JD, Chung HJ, Barron AM, Ho DA, Sahni D, Browning JL, et al. Extensive CD34-to-CD90 fibroblast transition defines regions of cutaneous reparative, hypertrophic, and keloidal scarring. Am J Dermatopathol. 2019;41(1):16–28.
Amatschek S, Kriehuber E, Bauer W, Reininger B, Meraner P, Wolpl A, et al. Blood and lymphatic endothelial cell-specific differentiation programs are stringently controlled by the tissue environment. Blood. 2007;109(11):4777–85.
Jurisic G, Iolyeva M, Proulx ST, Halin C, Detmar M. Thymus cell antigen 1 (Thy1, CD90) is expressed by lymphatic vessels and mediates cell adhesion to lymphatic endothelium. Exp Cell Res. 2010;316(17):2982–92.
Gaafar TM, Rahman HAA, Attia W, Hamza HS, Brockmeier K, El Hawary RE. Comparative characteristics of endothelial-like cells derived from human adipose mesenchymal stem cells and umbilical cord blood-derived endothelial cells. Clin Exp Med. 2014;14(2):177–84.
Acknowledgments
We deeply thank the Kidney and Pancreatic Transplantation Unit of UCLouvain’s Saint-Luc Hospital for donating ovaries for this study.
Funding
This study was supported by grants from the Fonds National de la Recherche Scientifique de Belgique (FNRS-PDR Convention grant number T.0004.20 awarded to C.A.A., Ph.D. scholarship awarded to H.V.) and Fondation Louvain (Ph.D. scholarship awarded to S.M., as part of a legacy from Mr. Frans Heyes, and Ph.D. scholarship awarded to A.D.).
Author information
Authors and Affiliations
Contributions
Arezoo Dadashzadeh: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing - Original Draft, Visualization; Saeid Moghassemi: Methodology, Validation, Formal analysis, Investigation, Writing - Original Draft, Visualization; Monika Grubliauskaité and Hanne Vlieghe: Methodology, Investigation; Davide Brusa: Conceptualization, Methodology, Validation, Formal analysis, Writing - Review & Editing; Christiani A. Amorim: Conceptualization, Resources, Writing - Review & Editing, Supervision, Project administration, Funding acquisition. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ovarian tissue biopsies were collected following approval from the Université Catholique de Louvain’s Institutional Review Board in May 2019 for the use of the human ovarian cortex on May 25, 2019 (IRB reference 2018/19DEC/475).
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dadashzadeh, A., Moghassemi, S., Grubliauskaité, M. et al. Medium supplementation can influence the human ovarian cells in vitro. J Ovarian Res 15, 137 (2022). https://doi.org/10.1186/s13048-022-01081-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13048-022-01081-2